How Elite Athletes with a Spinal Cord Injury Sweat during Exercise—An Exploratory Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Data Collection
2.3. Data Preparation
2.4. Data Analysis
3. Results
4. Discussion
5. Strengths and Limitations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cheuvront, S.N.; Kenefick, R.W. Personalized fluid and fuel intake for performance optimization in the heat. J. Sci. Med. Sport 2021, 24, 735–738. [Google Scholar] [CrossRef]
- Griggs, K.E.; Leicht, C.A.; Price, M.J.; Goosey-Tolfrey, V.L. Thermoregulation during intermittent exercise in athletes with a spinal-cord injury. Int. J. Sport. Physiol. Perform. 2015, 10, 469–475. [Google Scholar] [CrossRef] [PubMed]
- Hopman, M.T.; Oeseburg, B.; Binkhorst, R.A. Cardiovascular responses in persons with paraplegia to prolonged arm exercise and thermal stress. Med. Sci. Sports Exerc. 1993, 25, 577–583. [Google Scholar] [CrossRef]
- Grossmann, F.; Flueck, J.L.; Perret, C.; Meeusen, R.; Roelands, B. The Thermoregulatory and Thermal Responses of Individuals with a Spinal Cord Injury during Exercise, Acclimation and by Using Cooling Strategies—A Systematic Review. Front. Physiol. 2021, 12, 636997. [Google Scholar] [CrossRef]
- Price, M.J. Thermoregulation during exercise in individuals with spinal cord injuries. Sports Med. 2006, 36, 863–879. [Google Scholar] [CrossRef] [PubMed]
- Pritchett, K.; Broad, E.; Scaramella, J.; Baumann, S. Hydration and Cooling Strategies for Paralympic Athletes: Applied Focus: Challenges Athletes May Face at the Upcoming Tokyo Paralympics. Curr. Nutr. Rep. 2020, 9, 137–146. [Google Scholar] [CrossRef]
- Flueck, J.L. Nutritional Considerations for Para-Cycling Athletes: A Narrative Review. Sports 2021, 9, 154. [Google Scholar] [CrossRef] [PubMed]
- Dietz, V.A.; Roberts, N.; Knox, K.; Moore, S.; Pitonak, M.; Barr, C.; Centeno, J.; Leininger, S.; New, K.C.; Nowell, P.; et al. Fighting for recovery on multiple fronts: The past, present, and future of clinical trials for spinal cord injury. Front. Cell. Neurosci. 2022, 16, 977679. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. BMJ 2007, 335, 806–808. [Google Scholar] [CrossRef]
- Baker, L.B.; Ungaro, C.T.; Sopeña, B.C.; Nuccio, R.P.; Reimel, A.J.; Carter, J.M.; Stofan, J.R.; Barnes, K.A. Body map of regional vs. whole body sweating rate and sweat electrolyte concentrations in men and women during moderate exercise-heat stress. J. Appl. Physiol. 2018, 124, 1304–1318. [Google Scholar] [CrossRef]
- Au, J.S.; Kamijo, Y.-I.; Goosey-Tolfrey, V.L.; Leicht, C.A.; MacDonald, M.J.; Mukai, Y.; Tajima, F. Comparison between esophageal and intestinal temperature responses to upper-limb exercise in individuals with spinal cord injury. Spinal Cord 2019, 57, 586–593. [Google Scholar] [CrossRef]
- Grossmann, F.; Perret, C.; Roelands, B.; Meeusen, R.; Flueck, J.L. Fluid Balance and Thermoregulatory Responses during Wheelchair Basketball Games in Hot vs. Temperate Conditions. Nutrients 2022, 14, 2930. [Google Scholar] [CrossRef] [PubMed]
- Borg, G.A. Psychophysical bases of perceived exertion. Med. Sci. Sports Exerc. 1982, 14, 377–381. [Google Scholar] [CrossRef]
- Kirshblum, S.C.; Burns, S.P.; Biering-Sorensen, F.; Donovan, W.; Graves, D.E.; Jha, A.; Johansen, M.; Jones, L.; Krassioukov, A.; Mulcahey, M.J.; et al. International standards for neurological classification of spinal cord injury (revised 2011). J. Spinal Cord Med. 2011, 34, 535–546. [Google Scholar] [CrossRef] [PubMed]
- Sawka, M.N.; Burke, L.M.; Eichner, E.R.; Maughan, R.J.; Montain, S.J.; Stachenfeld, N.S. American College of Sports Medicine position stand. Exercise and fluid replacement. Med. Sci. Sports Exerc. 2007, 39, 377–390. [Google Scholar] [CrossRef]
- Baker, L.B. Sweating Rate and Sweat Sodium Concentration in Athletes: A Review of Methodology and Intra/Interindividual Variability. Sports Med. 2017, 47 (Suppl. 1), 111–128. [Google Scholar] [CrossRef]
- Fritz, C.O.; Morris, P.E.; Richler, J.J. Effect size estimates: Current use, calculations, and interpretation. J. Exp. Psychol. Gen. 2012, 141, 2–18. [Google Scholar] [CrossRef]
- Pritchett, R.C.; Al-Nawaiseh, A.M.; Pritchett, K.K.; Nethery, V.; Bishop, P.A.; Green, J.M. Sweat gland density and response during high-intensity exercise in athletes with spinal cord injuries. Biol. Sport 2015, 32, 249–254. [Google Scholar] [CrossRef]
- Grossmann, F.; Flueck, J.L.; Roelands, B.; Meeusen, R.; Perret, C. Validity of a Wheelchair Rugby Field Test to Simulate Physiological and Thermoregulatory Match Outcomes. Sports 2022, 10, 144. [Google Scholar] [CrossRef] [PubMed]
- Griggs, K.E.; Havenith, G.; Price, M.J.; Mason, B.S.; Goosey-Tolfrey, V.L. Thermoregulatory Responses during Competitive Wheelchair Rugby Match Play. Int. J. Sports Med. 2017, 38, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Trbovich, M.; Ortega, C.; Schroeder, J.; Fredrickson, M. Effect of a cooling vest on core temperature in athletes with and without spinal cord injury. Top. Spinal Cord Inj. Rehabil. 2014, 20, 70–80. [Google Scholar] [CrossRef]
- Moore, A.; Pritchett, K.L.; Pritchett, R.C.; Broad, E. Effects of Pre-Exercise Ice Slurry Ingestion on Physiological and Perceptual Measures in Athletes with Spinal Cord Injuries. Int. J. Exerc. Sci. 2021, 14, 19–32. [Google Scholar]
- Sanchez-Jimenez, J.L.; Aparicio, I.; Romero-Avila, J.L.; Bellot-Arcís, C.; Cibrián Ortiz de Anda, R.M.; Priego-Quesada, J.I. Skin temperature measurement in individuals with spinal cord injury during and after exercise: Systematic review. J. Therm. Biol. 2022, 105, 103146. [Google Scholar] [CrossRef] [PubMed]
- Forsyth, P.; Miller, J.; Pumpa, K.; Thompson, K.G.; Jay, O. Independent Influence of Spinal Cord Injury Level on Thermoregulation during Exercise. Med. Sci. Sports Exerc. 2019, 51, 1710–1719. [Google Scholar] [CrossRef] [PubMed]
- Price, M.J.; Campbell, I.G. Effects of spinal cord lesion level upon thermoregulation during exercise in the heat. Med. Sci. Sports Exerc. 2003, 35, 1100–1107. [Google Scholar] [CrossRef]
- Trbovich, M.B.; Kiratli, J.B.; Price, M.J. The effects of a heat acclimation protocol in persons with spinal cord injury. J. Therm. Biol. 2016, 62 Pt A, 56–62. [Google Scholar] [CrossRef]
- Burke, L.M. Nutritional approaches to counter performance constraints in high-level sports competition. Exp. Physiol. 2021, 106, 2304–2323. [Google Scholar] [CrossRef]
- Thomas, D.T.; Erdman, K.A.; Burke, L.M. American College of Sports Medicine Joint Position Statement. Nutrition and Athletic Performance. Med. Sci. Sports Exerc. 2016, 48, 543–568. [Google Scholar] [CrossRef]
- Janse Van Rensburg, D.C.; Schwellnus, M.; Derman, W.; Webborn, N. Illness among Paralympic Athletes: Epidemiology, Risk Markers, and Preventative Strategies. Phys. Med. Rehabil. Clin. N. Am. 2018, 29, 185–203. [Google Scholar] [CrossRef] [PubMed]
- Compton, S.; Trease, L.; Cunningham, C.; Hughes, D. Australian Institute of Sport and the Australian Paralympic Committee position statement: Urinary tract infection in spinal cord injured athletes. Br. J. Sports Med. 2015, 49, 1236–1240. [Google Scholar] [CrossRef]
- Armstrong, L.E. Rehydration during Endurance Exercise: Challenges, Research, Options, Methods. Nutrients 2021, 13, 887. [Google Scholar] [CrossRef]
- Black, K.E.; Huxford, J.; Perry, T.; Brown, R.C. Fluid and sodium balance of elite wheelchair rugby players. Int. J. Sport Nutr. Exerc. Metab. 2013, 23, 110–118. [Google Scholar] [CrossRef] [PubMed]
- Trbovich, M.; Ford, A.; Wu, Y.; Koek, W.; Wecht, J.; Kellogg, D., Jr. Correlation of neurological level and sweating level of injury in persons with spinal cord injury. J. Spinal Cord Med. 2021, 44, 902–909. [Google Scholar] [CrossRef] [PubMed]
- Baker, L.B. Physiology of sweat gland function: The roles of sweating and sweat composition in human health. Temperature 2019, 6, 211–259. [Google Scholar] [CrossRef] [PubMed]
- Maughan, R.J.; Shirreffs, S.M.; Leiper, J.B. Errors in the estimation of hydration status from changes in body mass. J. Sports Sci. 2007, 25, 797–804. [Google Scholar] [CrossRef]
- Gee, C.M.; West, C.R.; Krassioukov, A.V. Boosting in Elite Athletes with Spinal Cord Injury: A Critical Review of Physiology and Testing Procedures. Sports Med. 2015, 45, 1133–1142. [Google Scholar] [CrossRef]
- Blauwet, C.A.; Benjamin-Laing, H.; Stomphorst, J.; Van de Vliet, P.; Pit-Grosheide, P.; Willick, S.E. Testing for boosting at the Paralympic games: Policies, results and future directions. Br. J. Sports Med. 2013, 47, 832–837. [Google Scholar] [CrossRef]
| Overall (n = 15) | Females (n = 3) | Males (n = 12) | |
|---|---|---|---|
| Age (years) | 30 (28–36) | 36 (25–37) | 30 (28–35) |
| Height (cm) | 174 (160–183) | 170 (150–171) | 175 (163–185) |
| Body mass (kg) | 66 (56–74) | 48 (47–49) | 69 (62–76) |
| BMI (kg/m2) | 22 (20–24) | 17 (16–21) | 23 (21–24) |
| Lesion cause (n (%)) | |||
| Traumatic SCI | 10 (67) | 2 (67) | 8 (67) |
| Spina bifida | 5 (33) | 1 (33) | 4 (33) |
| Lesion duration (years) | 22 (6–28) | 23 (8–25) | 16 (6–30) |
| Lesion level (n (%)) | |||
| Tetraplegia | 3 (20) | 0 | 3 (25) |
| Paraplegia | 12 (80) | 3 (100) | 9 (75) |
| Motor impairment (n (%)) | |||
| Complete | 11 (73) | 2 (67) | 9 (75) |
| Incomplete | 4 (27) | 1 (33) | 3 (25) |
| Time active at elite athlete level (years) | 3 (1–8) | 3 (1–6) | 4 (1–9) |
| Sport type (n (%)) | |||
| Cycling | 9 (60) | 2 (67) | 7 (58) |
| Wheelchair racing | 1 (7) | 1 (33) | 0 |
| Basketball | 2 (13) | 0 | 2 (17) |
| Rugby | 2 (13) | 0 | 2 (17) |
| Alpine skiing | 1 (7) | 0 | 1 (7) |
| Average weekly training | |||
| Duration (hours) | 11 (9–12) | 11 (10–20) | 11 (9–12) |
| Frequency (sessions) | 6 (5–7) | 7 (6–12) | 6 (5–7) |
| (A) | ||||
| Overall | Sport Type | |||
| Endurance (n = 10) | Team/Skill (n = 5) | |||
| Core temperature (°C) | ||||
| Average | 37.7 (37.3–37.8) | 37.7 (37.6–37.8) | 37.3 (37.0–38.1) | |
| Minimum | 37.1 (36.9–37.1) | 37.1 (37.0–37.1) | 36.6 (36.1–37.2) | |
| Maximum | 38.1 (37.9–38.6) | 38.2 (38.1–38.6) | 37.8 (37.4–38.9) | |
| Heart rate (bpm) | ||||
| Average | 126 (100–146) | 134 (125–148) | 100 (96–104) | |
| Relative to max heart rate (%) * | 73 (69–76) | 74 (71–76) | 71 (62–74) | |
| Minimum | 68 (61–74) | 69 (63–83) | 62 (61–72) | |
| Maximum | 178 (133–195) | 190 (178–195) | 133 (119–149) | |
| Urine specific gravity (g/mL) | ||||
| Pre-exercise | 1.020 (1.015–1.027) | 1.017 (1.015–1.022) | 1.028 (1.024–1.030) | |
| Post-exercise | 1.018 (1.014–1.026) | 1.018 (1.014–1.026) | 1.019 (1.016–1.029) | |
| Body mass difference | ||||
| Absolute (kg) | 0.20 (0.10–0.30) | 0.30 (0.20–0.40) | −0.45 (−0.55–0.15) | |
| Relative (%) | 0.37 (0.12–0.61) | 0.48 (0.34–0.63) | −0.63 (−0.82–0.19) | |
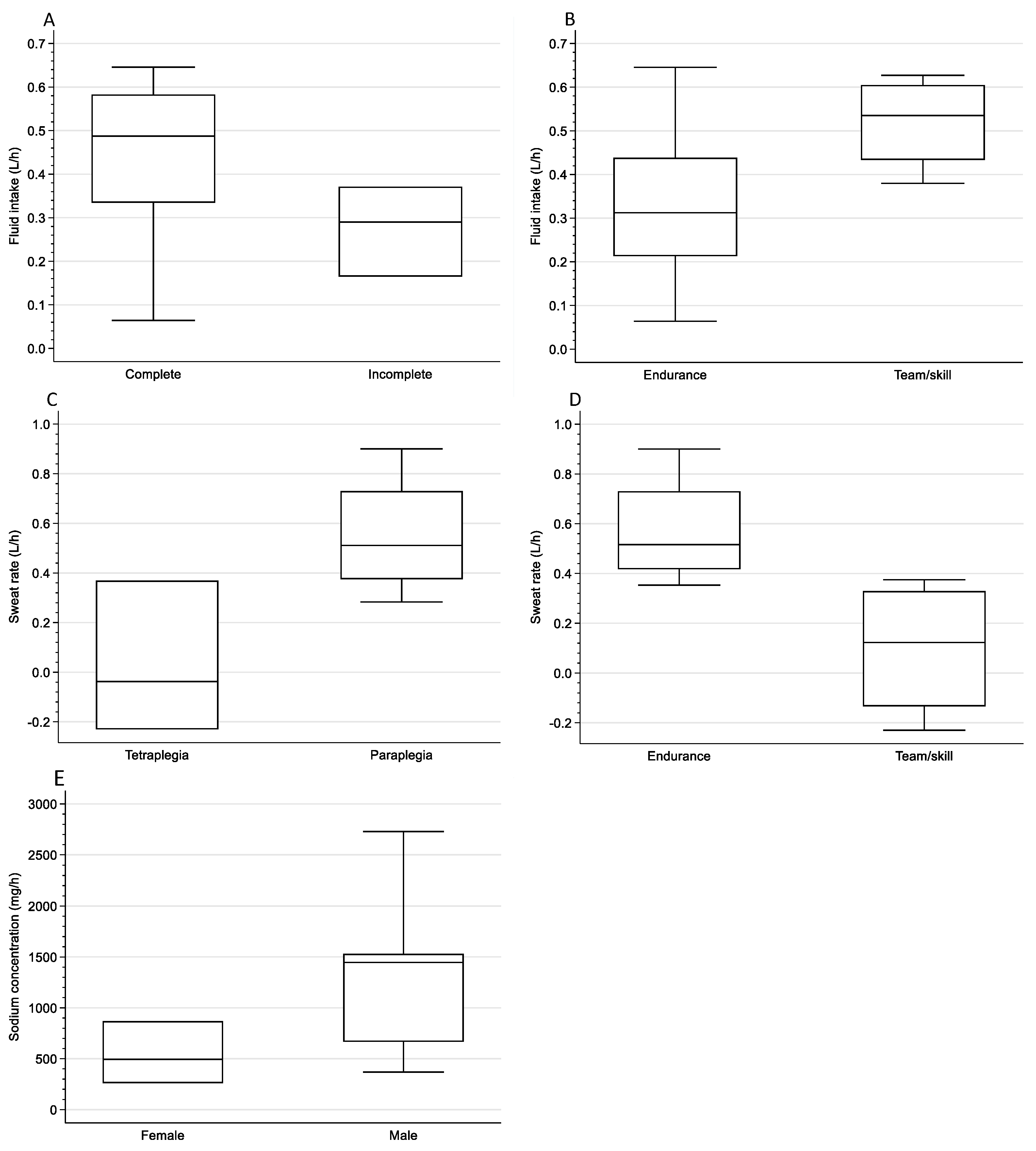
| Fluid intake (L/h) | 0.38 (0.28–0.54) | 0.31 (0.21–0.44) | 0.54 (0.43–0.61) | |
| Sweat rate (L/h) | 0.44 (0.35–0.63) | 0.52 (0.42–0.73) | 0.12 (−0.13–0.33) | |
| (B) | ||||
| Sodium Concentration (mg/L) | Sodium Loss (mg/h) | Potassium Concentration (mg/L) | Potassium Loss (mg/h) | |
| Head (n = 9) | 2100 (1300–2400) | 1256 (584–1752) | 210 (200–265) | 121 (104–145) |
| Scapula (n = 11) | 1700 (1400–2000) | 876 (494–1460) | 200 (160–220) | 98 (74–131) |
| Forearm (n = 10) | 1350 (1200–1800) | 817 (424–1241) | 240 (190–290) | 107 (102–117) |
| Shin (n = 5) | 1400 (770–1800) | 920 (401–1022) | 260 (180–300) | 129 (101–153) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hertig-Godeschalk, A.; Perret, C. How Elite Athletes with a Spinal Cord Injury Sweat during Exercise—An Exploratory Study. Sports 2024, 12, 81. https://doi.org/10.3390/sports12030081
Hertig-Godeschalk A, Perret C. How Elite Athletes with a Spinal Cord Injury Sweat during Exercise—An Exploratory Study. Sports. 2024; 12(3):81. https://doi.org/10.3390/sports12030081
Chicago/Turabian StyleHertig-Godeschalk, Anneke, and Claudio Perret. 2024. "How Elite Athletes with a Spinal Cord Injury Sweat during Exercise—An Exploratory Study" Sports 12, no. 3: 81. https://doi.org/10.3390/sports12030081
APA StyleHertig-Godeschalk, A., & Perret, C. (2024). How Elite Athletes with a Spinal Cord Injury Sweat during Exercise—An Exploratory Study. Sports, 12(3), 81. https://doi.org/10.3390/sports12030081






