Playing Disability Rugby League with Charcot-Marie-Tooth Disease: A Case Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Case
2.2. Characteristics of Case Subject
2.3. Sport-Specific Fitness Tests
2.4. In-Game Physical Performance Analysis
3. Results
3.1. Case Subject Versus Aged-Matched CMT Participants
3.2. Sport-Specific Results—Case Subject Versus CP Rugby League Player
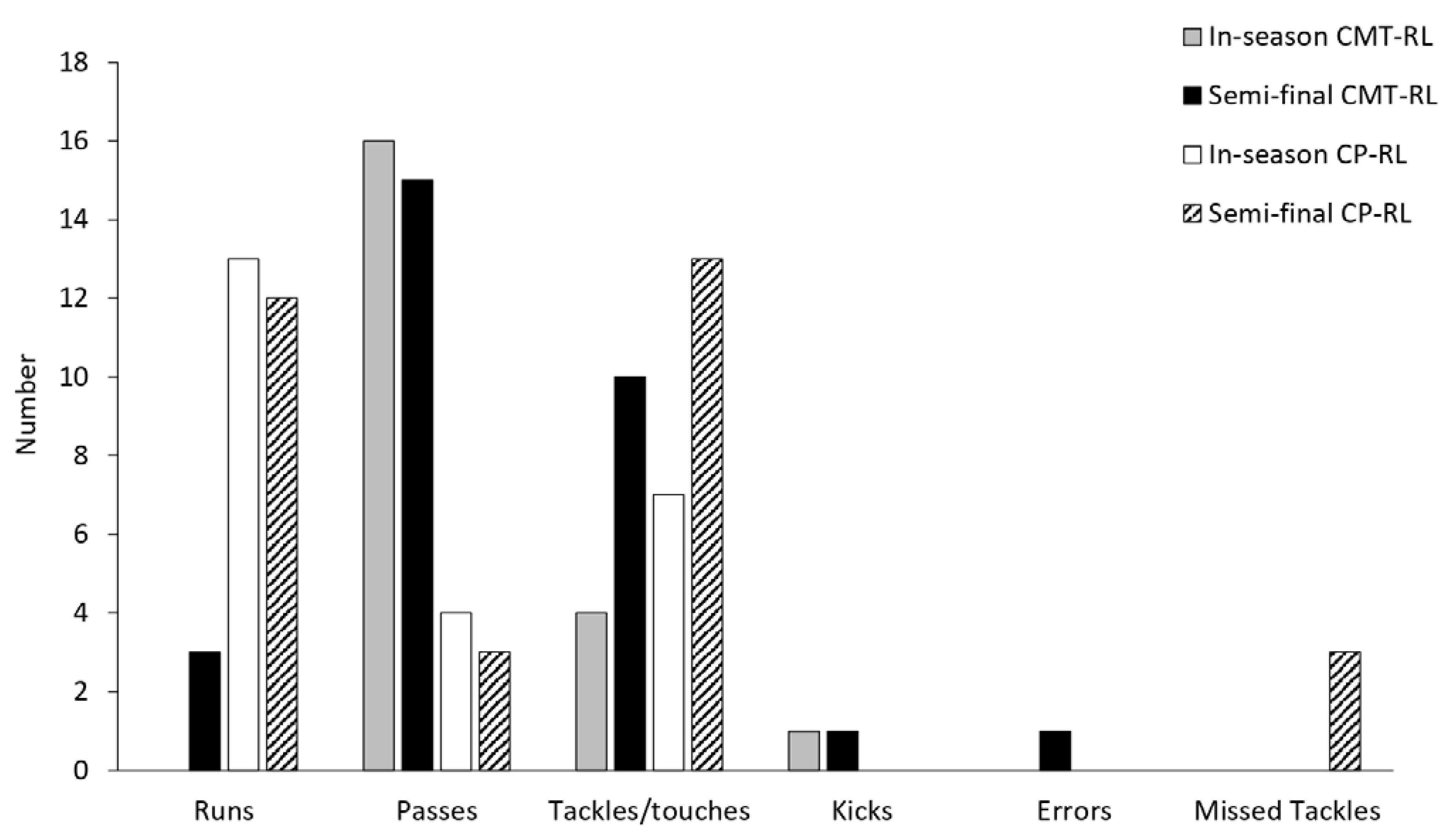
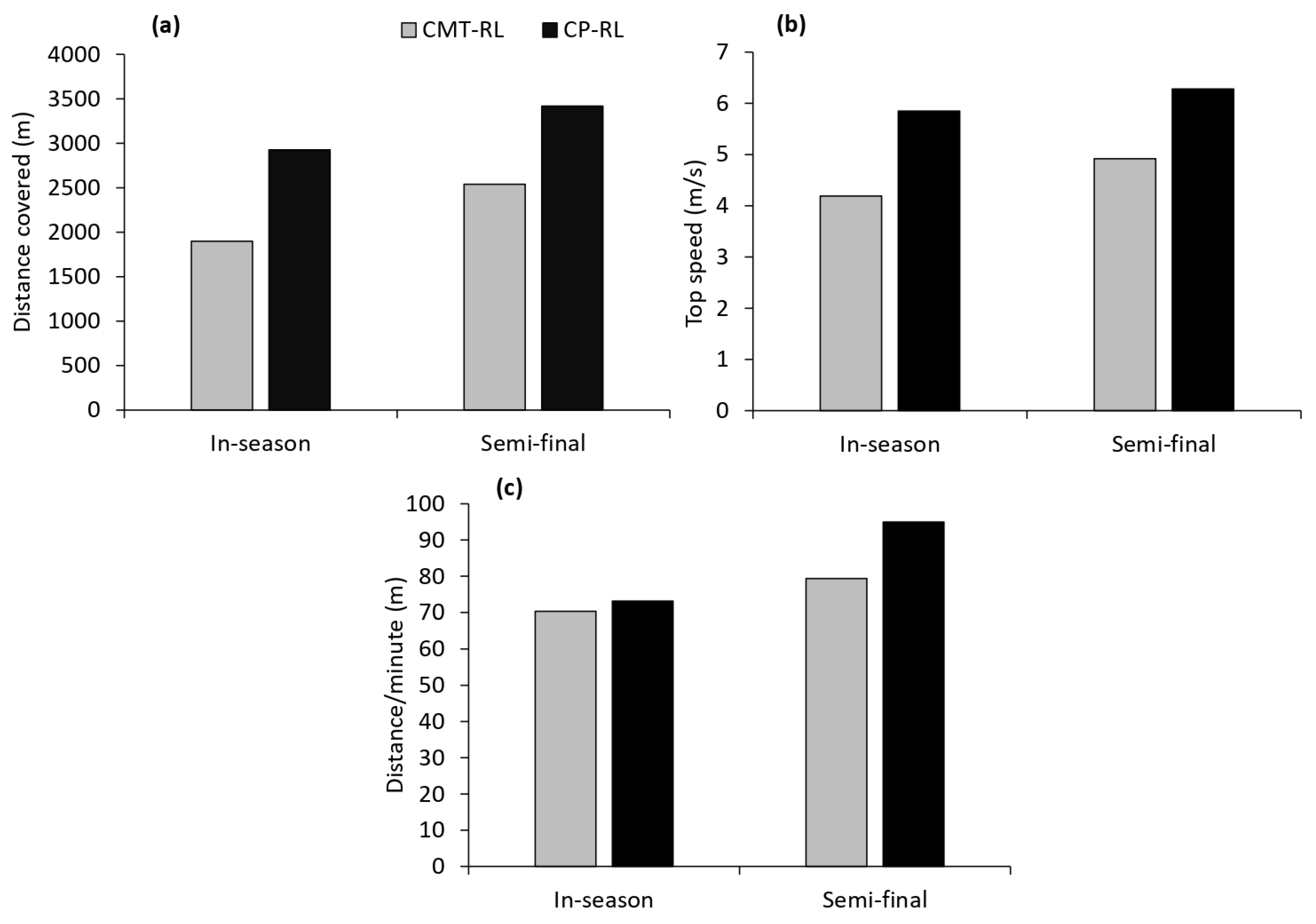
3.3. In-Game Analysis—Case Subject Versus CP Rugby League Player
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Szigeti, K.; Lupski, J.R. Charcot–marie–tooth disease. Eur. J. Hum. Genet. 2009, 17, 703–710. [Google Scholar] [CrossRef] [PubMed]
- Banchs, I.; Casasnovas, C.; Albertí, A.; De Jorge, L.; Povedano, M.; Mon, J.; Martínez-Matos, J.A.; Volpini, V. Diagnosis of charcot-marie-tooth disease. J. Biomed. Biotechnol. 2009, 2009, 985415. [Google Scholar] [CrossRef]
- Timmerman, V.; Strickland, A.V.; Züchner, S. Genetics of Charcot-Marie-Tooth (CMT) Disease within the Frame of the Human Genome Project Success. Genes 2014, 5, 13–32. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Yin, F. A Review of X-linked Charcot-Marie-Tooth Disease. J. Child Neurol. 2016, 31, 761–772. [Google Scholar] [CrossRef] [PubMed]
- Pareyson, D.; Marchesi, C. Diagnosis, natural history, and management of Charcot-Marie-Tooth disease. Lancet Neurol. 2009, 8, 654–667. [Google Scholar] [CrossRef] [PubMed]
- Maggi, G.; Monti Bragadin, M.; Padua, L.; Fiorina, E.; Bellone, E.; Grandis, M.; Reni, L.; Bennicelli, A.; Grosso, M.; Saporiti, R.; et al. Outcome measures and rehabilitation treatment in patients affected by Charcot-Marie-Tooth neuropathy: A pilot study. Am. J. Phys. Med. Rehabil. 2011, 90, 628–637. [Google Scholar] [CrossRef] [PubMed]
- Burns, J.; Ryan, M.M.; Ouvrier, R.A. Evolution of foot and ankle manifestations in children with CMT1A. Muscle Nerve 2009, 39, 158–166. [Google Scholar] [CrossRef] [PubMed]
- Pfeiffer, G.; Wicklein, E.M.; Ratusinski, T.; Schmitt, L.; Kunze, K. Disability and quality of life in Charcot-Marie-Tooth disease type 1. J. Neurol. Neurosurg. Psychiatry 2001, 70, 548–550. [Google Scholar] [CrossRef]
- Cordeiro, J.L.; Marques, W.; Hallak, J.E.; Osório, F.L. Charcot-Marie-Tooth disease, psychiatric indicators and quality of life: A systematic review. ASN Neuro 2014, 6, 185–192. [Google Scholar] [CrossRef]
- Zhao, M.; Veeranki, S.P.; Magnussen, C.G.; Xi, B. Recommended physical activity and all cause and cause specific mortality in US adults: Prospective cohort study. BMJ 2020, 370, m2031. [Google Scholar] [CrossRef]
- Alingh, R.A.; Hoekstra, F.; van der Schans, C.P.; Hettinga, F.J.; Dekker, R.; van der Woude, L.H.V. Protocol of a longitudinal cohort study on physical activity behaviour in physically disabled patients participating in a rehabilitation counselling programme: ReSpAct. BMJ Open 2015, 5, e007591. [Google Scholar] [CrossRef] [PubMed]
- van der Ploeg, H.P.; van der Beek, A.J.; van der Woude, L.H.; van Mechelen, W. Physical activity for people with a disability. Sports Med. 2004, 34, 639–649. [Google Scholar] [CrossRef] [PubMed]
- Sahlin, K.B.; Lexell, J. Impact of organized sports on activity, participation, and quality of life in people with neurologic disabilities. PM&R 2015, 7, 1081–1088. [Google Scholar]
- Vita, G.; La Foresta, S.; Russo, M.; Vita, G.L.; Messina, S.; Lunetta, C.; Mazzeo, A. Sport activity in Charcot–Marie–Tooth disease: A case study of a Paralympic swimmer. Neuromuscul. Disord. 2016, 26, 614–618. [Google Scholar] [CrossRef]
- Sman, A.D.; Hackett, D.; Fiatarone Singh, M.; Fornusek, C.; Menezes, M.P.; Burns, J. Systematic review of exercise for Charcot-Marie-Tooth disease. J. Peripher. Nerv. Syst. 2015, 20, 347–362. [Google Scholar] [CrossRef]
- Wallace, A.; Pietrusz, A.; Dewar, E.; Dudziec, M.; Jones, K.; Hennis, P.; Sterr, A.; Baio, G.; Machado, P.M.; Laurá, M.; et al. Community exercise is feasible for neuromuscular diseases and can improve aerobic capacity. Neurology 2019, 92, e1773–e1785. [Google Scholar] [CrossRef]
- Corrado, B.; Ciardi, G.; Bargigli, C. Rehabilitation management of the Charcot–Marie–tooth syndrome: A systematic review of the literature. Medicine 2016, 95, e3278. [Google Scholar] [CrossRef]
- Hackett, D.; Roberts-Clarke, D.; Halaki, M.; Burns, J.; Fiatatone Singh, M.; Fornusek, C. High intensity power training in middle-aged women with Charcot–Marie–Tooth disease: A case series. Int. J. Ther. Rehabil. 2021, 28, 1–12. [Google Scholar] [CrossRef]
- Anens, E.; Emtner, M.; Hellström, K. Exploratory study of physical activity in persons with Charcot-Marie-Tooth disease. Arch. Phys. Med. Rehabil. 2015, 96, 260–268. [Google Scholar] [CrossRef]
- NSWPDRLA. New South Wales Physical Disability Rugby League Association. About. 2021. Available online: https://nswpdrla.com.au/ (accessed on 28 November 2022).
- League, I.R. Playing Conditions, Physical Disability Rugby League. 2021. Available online: https://www.intrl.sport/media/ky0j0m5x/playing-conditions-physical-disability-rugby-league.pdf (accessed on 28 November 2022).
- Gabbett, T.J. Science of rugby league football: A review. J. Sports Sci. 2005, 23, 961–976. [Google Scholar] [CrossRef]
- Pisciotta, C.; Saveri, P.; Pareyson, D. Challenges in treating Charcot-Marie-Tooth disease and related neuropathies: Current management and future perspectives. Brain Sci. 2021, 11, 1447. [Google Scholar] [CrossRef] [PubMed]
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: Guidelines for the six-minute walk test. Am. J. Respir. Crit. Care Med. 2002, 166, 111–117. [Google Scholar] [CrossRef] [PubMed]
- Savva, C.; Giakas, G.; Efstathiou, M.; Karagiannis, C. Test-retest reliability of handgrip strength measurement using a hydraulic hand dynamometer in patients with cervical radiculopathy. J. Manip. Physiol. Ther. 2014, 37, 206–210. [Google Scholar] [CrossRef]
- Roberts-Clarke, D.; Fornusek, C.; Saigal, N.; Halaki, M.; Burns, J.; Nicholson, G.; Fiatarone Singh, M.; Hackett, D. Relationship between physical performance and quality of life in Charcot-Marie-Tooth disease: A pilot study. J. Peripher. Nerv. Syst. 2016, 21, 357–364. [Google Scholar] [CrossRef] [PubMed]
- Norkin, C.C.; White, D.J. Lower Extremity Testing. In Measurement of Joint Motion: A Guide to Goniometry; FA Davis: Philadelphia, PA, USA, 2016; pp. 253–408. [Google Scholar]
- Reina, R.; Iturricastillo, A.; Sabido, R.; Campayo-Piernas, M.; Yanci, J. Vertical and horizontal jump capacity in international cerebral palsy football players. Int. J. Sports Physiol. Perform. 2018, 13, 597–603. [Google Scholar] [CrossRef]
- Comfort, P.; Graham-Smith, P.; Matthews, M.J.; Bamber, C. Strength and power characteristics in English elite rugby league players. J. Strength Cond. Res. 2011, 25, 1374–1384. [Google Scholar] [CrossRef]
- Padua, L.; Pazzaglia, C.; Pareyson, D.; Schenone, A.; Aiello, A.; Fabrizi, G.M.; Cavallaro, T.; Santoro, L.; Manganelli, F.; Gemignani, F.; et al. Novel outcome measures for Charcot-Marie-Tooth disease: Validation and reliability of the 6-min walk test and StepWatch(™) Activity Monitor and identification of the walking features related to higher quality of life. Eur. J. Neurol. 2016, 23, 1343–1350. [Google Scholar] [CrossRef]
- Casanova, C.; Celli, B.R.; Barria, P.; Casas, A.; Cote, C.; de Torres, J.P.; Jardim, J.; Lopez, M.V.; Marin, J.M.; Montes de Oca, M.; et al. The 6-min walk distance in healthy subjects: Reference standards from seven countries. Eur. Respir. J. 2011, 37, 150–156. [Google Scholar] [CrossRef]
- Ferrarin, M.; Bovi, G.; Rabuffetti, M.; Mazzoleni, P.; Montesano, A.; Pagliano, E.; Marchi, A.; Magro, A.; Marchesi, C.; Pareyson, D.; et al. Gait pattern classification in children with Charcot-Marie-Tooth disease type 1A. Gait Posture 2012, 35, 131–137. [Google Scholar] [CrossRef][Green Version]
- Ramdharry, G.M.; Day, B.L.; Reilly, M.M.; Marsden, J.F. Hip flexor fatigue limits walking in Charcot-Marie-Tooth disease. Muscle Nerve 2009, 40, 103–111. [Google Scholar] [CrossRef]
- Kennedy, R.A.; Carroll, K.; McGinley, J.L. Gait in children and adolescents with Charcot-Marie-tooth disease: A systematic review. J. Peripher. Nerv. Syst. 2016, 21, 317–328. [Google Scholar] [CrossRef] [PubMed]
- Sikorska, I.; Gerc, K. Athletes with disability in the light of positive psychology. Balt. J. Health Phys. Act. 2018, 10, 64–76. [Google Scholar] [CrossRef]
- Downward, P.; Rasciute, S. Does sport make you happy? An analysis of the well-being derived from sports participation. Int. Rev. Appl. Econ. 2011, 25, 331–348. [Google Scholar] [CrossRef]
- Andersen, M.H.; Ottesen, L.; Thing, L.F. The social and psychological health outcomes of team sport participation in adults: An integrative review of research. Scand. J. Public Health 2019, 47, 832–850. [Google Scholar] [CrossRef] [PubMed]
- Lochbaum, M.; Sherburn, M.; Sisneros, C.; Cooper, S.; Lane, A.M.; Terry, P.C. Revisiting the Self-Confidence and Sport Performance Relationship: A Systematic Review with Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 6381. [Google Scholar] [CrossRef] [PubMed]
- Newman, C.J.; Walsh, M.; O’Sullivan, R.; Jenkinson, A.; Bennett, D.; Lynch, B.; O’Brien, T. The characteristics of gait in Charcot-Marie-Tooth disease types I and II. Gait Posture 2007, 26, 120–127. [Google Scholar] [CrossRef]
- El Mhandi, L.; Millet, G.Y.; Calmels, P.; Richard, A.; Oullion, R.; Gautheron, V.; Féasson, L. Benefits of interval-training on fatigue and functional capacities in Charcot-Marie-Tooth disease. Muscle Nerve 2008, 37, 601–610. [Google Scholar] [CrossRef]
| CMT-Active #1 | CMT-Active #2 | CMT-RL | Diff RL vs. Active #1 (%) | Diff RL vs. Active #2 (%) | |
|---|---|---|---|---|---|
| Age (y) | 57 | 54 | 50 | ||
| CMT type | CMTX | Unknown | CMTX3 | ||
| Age at diagnosis (y) | 18 | 29 | 8 | ||
| Duration of diagnosis (y) | 39 | 34 | 42 | ||
| BMI (kg/m2) | 24.1 | 27.2 | 25.7 | 6.2 | −5.8 |
| Waist circumference (cm) | 93.3 | 93.2 | 88.5 | −5.4 | −5.3 |
| Lean body mass (kg) a | 54.4 | 53.2 | 54.1 | −0.5 | 1.7 |
| Arm lean mass (kg) a | 6.8 | 7.5 | 7.2 | 5.6 | −4.2 |
| Leg lean mass (kg) a | 16.3 | 15.5 | 12.4 | −31.5 | −25.0 |
| % Body fat a | 22.6 | 28.8 | 32.0 | 29.4 | 10.0 |
| 6MWT (m) | 408.3 | 551.6 | 597 | 31.6 | 7.6 |
| Handgrip (kg)—right | 15 | 23 | 19 | 21.1 | −21.1 |
| Handgrip (kg)—left | 20 | 27 | 26 | 23.1 | −3.8 |
| 1 RM Chest press (N) | 452 | 640 | 650 | 30.5 | 1.5 |
| 1 RM Leg press (N) | 2500 | 3050 | 1550 | −61.3 | −96.8 |
| CP-RL | CMT-RL | Diff CMT-RL vs. CP-RL (%) | |
|---|---|---|---|
| 20 m sprint (sec) | 3.6 | 5.1 | 29.4 |
| Illinois agility (sec) | 20.9 | 26.5 | 21.1 |
| Vertical jump (cm) | 23 | 10.7 | −115 |
| Isometric mid-thigh pull (N) | 2358.8 | 1917.2 | −23.0 |
| Time to peak force (sec) | 1.6 | 2.4 | 33.3 |
| Joint range of motion (degrees) | |||
| Plantar flexion—right Plantar flexion—left | 39 38.5 | 25 25 | −56.0 −54.0 |
| Dorsi flexion—right Dorsi flexion—left | 20 16.5 | −15 a −14 a | −233.0 −218.0 |
| Knee flexion—right Knee flexion—left | 140 131.5 | 135.5 137.5 | −3.3 4.4 |
| Knee extension—right Knee extension—left | −3 a 0.5 | 1 4 | 400 87.5 |
| Hip flexion—right Hip flexion—left | 114 103 | 109 105 | −4.6 1.9 |
| Hip internal rotation—right Hip internal rotation—left | 43.5 42 | 26.5 28 | −64.2 −50.0 |
| Hip external rotation—right Hip external rotation—left | 40.5 36 | 48.5 36.5 | 16.5 1.4 |
| Hip abduction—right Hip abduction—left | 25.5 34.5 | 33 33.5 | 22.7 −3.0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Manny, L.; Wileman, T.; Fornusek, C.; Hackett, D.A. Playing Disability Rugby League with Charcot-Marie-Tooth Disease: A Case Study. Sports 2023, 11, 21. https://doi.org/10.3390/sports11020021
Manny L, Wileman T, Fornusek C, Hackett DA. Playing Disability Rugby League with Charcot-Marie-Tooth Disease: A Case Study. Sports. 2023; 11(2):21. https://doi.org/10.3390/sports11020021
Chicago/Turabian StyleManny, Luke, Taylor Wileman, Che Fornusek, and Daniel A. Hackett. 2023. "Playing Disability Rugby League with Charcot-Marie-Tooth Disease: A Case Study" Sports 11, no. 2: 21. https://doi.org/10.3390/sports11020021
APA StyleManny, L., Wileman, T., Fornusek, C., & Hackett, D. A. (2023). Playing Disability Rugby League with Charcot-Marie-Tooth Disease: A Case Study. Sports, 11(2), 21. https://doi.org/10.3390/sports11020021







