An Investigation of the Nature of Fear within ACL-Injured Subjects When Exposed to Provocative Videos: A Concurrent Qualitative and Quantitative Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
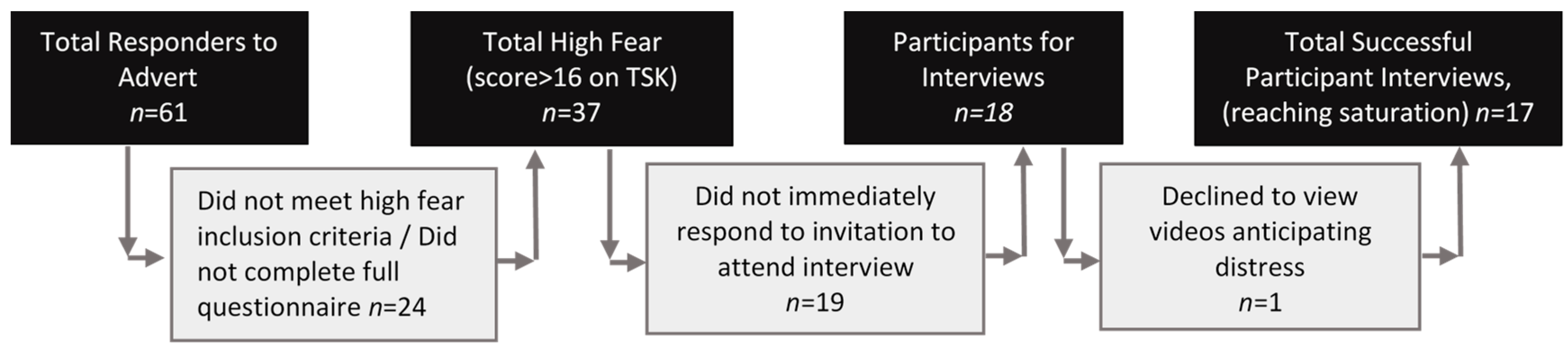
2.2. Participants
2.3. Sampling and Power
2.4. Measures
2.5. Procedure
- Video S1 ‘Running’: shows the video athletes running in a straight line at a low to moderate intensity for 10 s, followed by a gentle turn to leave the video frame -this was considered a baseline video showing a common, very lower-level activity
- Video S2 ‘Cut and Pivot’: shows the video athletes running forward at a low to moderate intensity for nine seconds, then completing a cut and pivot movement (i.e., planting one foot and turning sharply at a right angle) then continue off screen—this is the most commonly reported fearful movement for people following ACL injury [30].
- Video S3 ‘Cut & Pivot with feigned knee injury’: shows the video athletes running forward at a low to moderate intensity for nine seconds, then completing a sharp cut and pivot motion (as in Video 2) and then feigning a knee injury by holding the knee and falling down (reproducing an injury).
- Video S4 ‘Knee injury clips’: shows a series of video clips of traumatic knee injuries compiled from YouTube, representing a series of more graphic injuries (both male and female)
2.6. Qualitative Data Analysis
2.7. Quantitative Data Analysis
3. Results
3.1. Participant Characteristics
3.2. Qualitative Results
3.2.1. Theme 1: Evoked Physiological Responses
3.2.2. Theme 2: Deeper Contextualisation of the meaning of an ACL Injury Influencing Body Confidence
3.2.3. Theme 3: Recall of Psychological Difficulties
3.2.4. Theme 4: Negative Implications of a Re-Injury
3.3. Quantitative Results
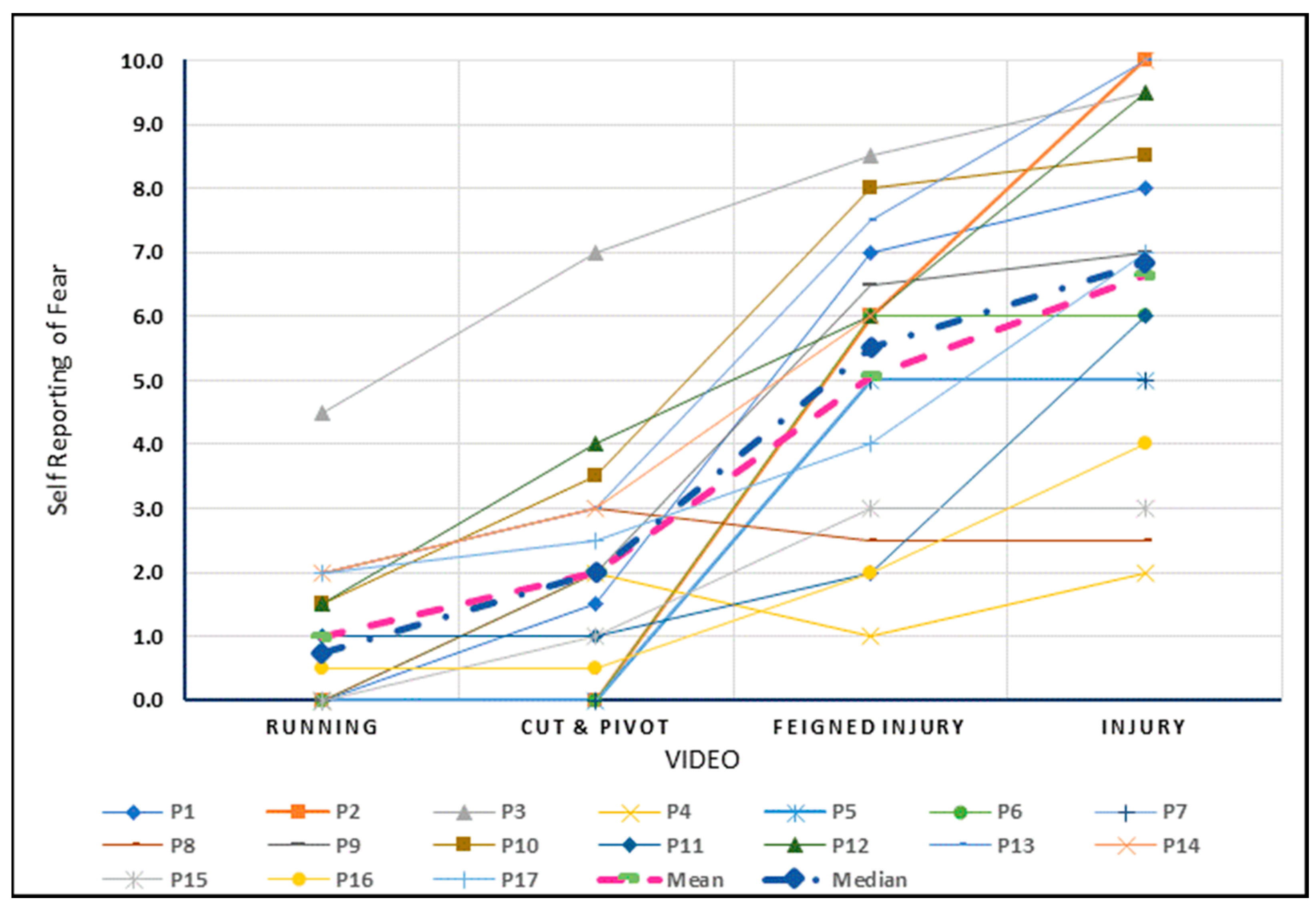
3.3.1. Self-Reported Fear
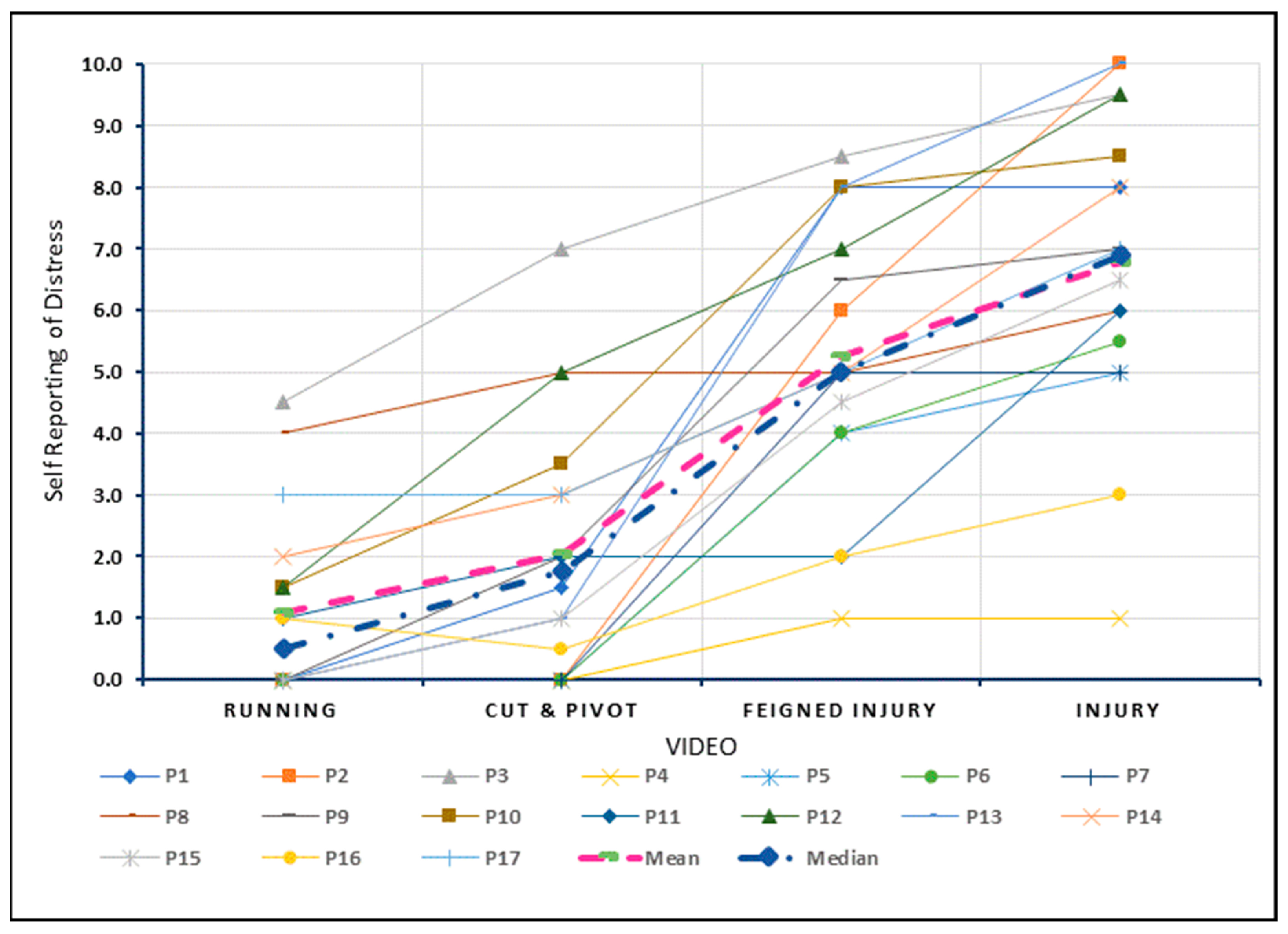
3.3.2. Self-Reported Distress
4. Discussion
4.1. Comparisons to the Literature
4.2. Strengths
4.3. Limitations
4.4. Clinical Significance
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Filbay, S.R.; Grindem, H. Evidence-based recommendations for the management of anterior cruciate ligament (ACL) rupture. Best Pract. Res. Clin. Rheumatol. 2019, 33, 33–47. [Google Scholar] [CrossRef] [PubMed]
- Ardern, C.L.; Taylor, N.F.; Feller, J.A.; Webster, K.E. Fear of re-injury in people who have returned to sport following anterior cruciate ligament reconstruction surgery. J. Sci. Med. Sport 2012, 15, 488–495. [Google Scholar] [CrossRef]
- Zbrojkiewicz, D.; Vertullo, C.; Grayson, J. Increasing rates of anterior cruciate ligament reconstruction in young Australians, 2000–2015. Med. J. Aust. 2018, 208, 354–358. [Google Scholar] [CrossRef] [PubMed]
- Maniar, N.; Verhagen, E.; Bryant, A.L.; Opar, D.A. Trends in Australian knee injury rates: An epidemiological analysis of 228,344 knee injuries over 20 years. Lancet Reg. Health-West. Pac. 2022, 21, 100409. [Google Scholar] [CrossRef] [PubMed]
- Ardern, C.L.; Taylor, N.F.; Feller, J.A.; Webster, K.E. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: An updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br. J. Sports Med. 2014, 48, 1543–1552. [Google Scholar] [CrossRef]
- Nwachukwu, B.; Adjei, J.; Rauck, R.; Chahla, J.; Okoroha, K.; Verma, N.; Allen, A.A.; Williams, I.R.J. How Much Do Psychological Factors Affect Lack of Return to Play After Anterior Cruciate Ligament Reconstruction? A Systematic Review. Orthop. J. Sports Med. 2019, 7, 2325967119845313. [Google Scholar] [CrossRef] [PubMed]
- Ardern, C.L.; Taylor, N.F.; Feller, J.A.; Whitehead, T.; Webster, K. Psychological responses matter in returning to pre-injury level of sport after anterior cruciate ligament reconstruction surgery. Am. J. Sports Med. 2013, 41, 1549–1555. [Google Scholar] [CrossRef]
- Flanigan, D.; Everhart, J.; Pedroza, A.; Smith, T.; Kaeding, C. Fear of reinjury (kinesiophobia) and persistent knee symptoms are common factors for lack of return to sport after anterior cruciate ligament reconstruction. Arthroscopy 2013, 29, 1322–1329. [Google Scholar] [CrossRef]
- Nwachukwu, B.U.; Voleti, P.B.; Berkanish, P.; Chang, B.; Cohn, M.R.; Williams, R.J.; Allen, A.A. Return to play and patient satisfaction after ACL reconstruction: Study with minimum 2-year follow-up. J. Bone Jt. Surg. 2017, 99, 720–725. [Google Scholar] [CrossRef] [PubMed]
- Padaki, A.S.; Noticewala, M.S.; Levine, W.N.; Ahmad, C.S.; Popkin, M.K.; Popkin, C.A. Prevalence of Posttraumatic Stress Disorder Symptoms Among Young Athletes After Anterior Cruciate Ligament Rupture. Orthop. J. Sports Med. 2018, 6, 2325967118787159. [Google Scholar] [CrossRef]
- Bateman, A.; Morgan, K.A.D. The Postinjury Psychological Sequelae of High-Level Jamaican Athletes: Exploration of a Posttraumatic Stress Disorder-Self-Efficacy Conceptualization. J. Sport Rehabil. 2019, 28, 144–152. [Google Scholar] [CrossRef] [PubMed]
- Aron, C.M.; Harvey, S.; Hainline, B.; Hitchcock, M.E.; Reardon, C.L. Post-traumatic stress disorder (PTSD) and other trauma-related mental disorders in elite athletes: A narrative review. Br. J. Sports Med. 2019, 53, 779–784. [Google Scholar] [CrossRef] [PubMed]
- VandenBos, G.R. Fear in APA Dictionary of Psychology, 2nd ed.; American Psychological Association: Washington, DC, USA, 2015. [Google Scholar]
- Ardern, C.L.; Osterberg, A.; Tagesson, S.; Gauffin, H.; Webster, K.E.; Kvist, J. The impact of psychological readiness to return to sport and recreational activities after anterior cruciate ligament reconstruction. Br. J. Sports Med. 2014, 48, 1613–1619. [Google Scholar] [CrossRef] [PubMed]
- Ardern, C.L.; Taylor, N.; Feller, J.; Webster, K. A systematic review of the psychological factors associated with returning to sport following injury. Br. J. Sports Med. 2012, 47, 1120–1126. [Google Scholar] [CrossRef]
- Ardern, C.L.; Webster, K.E.; Taylor, N.F.; Feller, J.A. Return to sport following anterior cruciate ligament reconstruction surgery: A systematic review and meta-analysis of the state of play. Br. J. Sports Med. 2011, 45, 596–606. [Google Scholar] [CrossRef]
- Kvist, J.; Ek, A.; Sporrstedt, K.; Good, L. Fear of re-injury: A hindrance for returning to sports after anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2005, 13, 393–397. [Google Scholar] [CrossRef]
- Lissek, S.; Powers, A.S.; McClure, E.B.; Phelps, E.A.; Woldehawariat, G.; Grillon, C.; Pine, D.S. Classical fear conditioning in the anxiety disorders: A meta-analysis. Behav. Res. Ther. 2005, 43, 1391–1424. [Google Scholar] [CrossRef]
- de Munter, L.; Polinder, S.; Haagsma, J.A.; Kruithof, N.; van de Ree, C.L.P.; Steyerberg, E.W.; de Jongh, M.A. Prevalence and Prognostic Factors for Psychological Distress After Trauma. Arch. Phys. Med. Rehabil. 2020, 101, 877. [Google Scholar] [CrossRef]
- McCarty, R. Chapter 4-The Fight-or-Flight Response: A Cornerstone of Stress Research. In Stress: Concepts, Cognition, Emotion, and Behavior; Fink, G., Ed.; Academic Press: San Diego, CA, USA, 2016; pp. 33–37. [Google Scholar]
- Campbell, P.; Bishop, A.; Dunn, K.; Main, J.C.; Thomas, E.; Foster, E.N. Conceptual overlap of psychological constructs in low back pain. Pain 2013, 154, 1783–1791. [Google Scholar] [CrossRef]
- LeDoux, J.E. Coming to terms with fear. Proc. Natl. Acad. Sci. USA 2014, 111, 2871–2878. [Google Scholar] [CrossRef]
- Bunzli, S.; Smith, A.; Schütze, R.; Lin, I.; O’Sullivan, P. Making Sense of Low Back Pain and Pain-Related Fear. J. Orthop. Sports Phys. Ther. 2017, 47, 628–636. [Google Scholar] [CrossRef] [PubMed]
- Crombez, G.; Eccleston, C.; Van Damme, S.; Vlaeyen, J.W.; Karoly, P. Fear-avoidance model of chronic pain: The next generation. Clin. J. Pain 2012, 28, 475–483. [Google Scholar] [CrossRef] [PubMed]
- Meulders, A. Fear in the context of pain: Lessons learned from 100 years of fear conditioning research. Behav. Res. Ther. 2020, 131, 103635. [Google Scholar] [CrossRef] [PubMed]
- Caneiro, J.P.; O’Sullivan, P.; Lipp, O.V.; Mitchinson, L.; Oeveraas, N.; Bhalvani, P.; Abrugiato, R.; Thorkildsen, S.; Smith, A. Evaluation of implicit associations between back posture and safety of bending and lifting in people without pain. Scand. J. Pain 2018, 18, 719–728. [Google Scholar] [CrossRef]
- Ellingsen, D.M.; Napadow, V.; Protsenko, E.; Mawla, I.; Kowalski, M.H.; Swensen, D.; O’Dwyer-Swensen, D.; Edwards, R.R.; Kettner, N.; Loggia, M.L. Brain Mechanisms of Anticipated Painful Movements and Their Modulation by Manual Therapy in Chronic Low Back Pain. J. Pain 2018, 19, 1352–1365. [Google Scholar] [CrossRef]
- Meier, M.L.; Stämpfli, P.; Vrana, A.; Humphreys, B.K.; Seifritz, E.; Hotz-Boendermaker, S. Fear avoidance beliefs in back pain-free subjects are reflected by amygdala-cingulate responses. Front. Hum. Neurosci. 2015, 9, 424. [Google Scholar] [CrossRef]
- Meier, M.L.; Stämpfli, P.; Vrana, A.; Humphreys, B.K.; Seifritz, E.; Hotz-Boendermaker, S. Neural Correlates of Fear of Movement in Patients with Chronic Low Back Pain vs. Pain-Free Individuals. Front. Hum. Neurosci. 2016, 10, 386. [Google Scholar] [CrossRef]
- Meierbachtol, A.; Obermeier, M.; Yungtum, W.; Bottoms, J.; Paur, E.; Nelson, B.J.; Tompkins, M.; Russell, H.C.; Chmielewski, T.L. Injury-Related Fears During the Return-to-Sport Phase of ACL Reconstruction Rehabilitation. Orthop. J. Sports Med. 2020, 8, 2325967120909385. [Google Scholar] [CrossRef]
- Farmer, T.; Robinson, K.; Elliott, S.J.; Eyles, J. Developing and Implementing a Triangulation Protocol for Qualitative Health Research. Qual. Health Res. 2006, 16, 377–394. [Google Scholar] [CrossRef]
- O’Cathain, A.; Murphy, E.; Nicholl, J. Three techniques for integrating data in mixed methods studies. BMJ 2010, 341, 4587. [Google Scholar] [CrossRef]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Fetters, M.D.; Curry, L.A.; Creswell, J.W. Achieving integration in mixed methods designs-principles and practices. Health Serv. Res. 2013, 48, 2134–2156. [Google Scholar] [CrossRef]
- Miller, C.L.; Mott, K.; Cousins, M.; Miller, S.; Johnson, A.; Lawson, T.; Wesselingh, S. Integrating consumer engagement in health and medical research–an Australian framework. Health Res. Policy Syst. 2017, 15, 9. [Google Scholar] [CrossRef] [PubMed]
- Burgi, C.R.; Peters, S.; Ardern, C.L.; Magill, J.R.; Gomez, C.D.; Sylvain, J.; Reiman, M.P. Which criteria are used to clear patients to return to sport after primary ACL reconstruction? A scoping review. Br. J. Sports Med. 2019, 53, 1154–1161. [Google Scholar] [CrossRef]
- Chalmers, P.N.; Mall, N.A.; Moric, M.; Sherman, S.L.; Paletta, G.P.; Cole, B.J. Does ACL reconstruction alter natural history? A systematic literature review of long-term outcomes. J. Bone Joint Surg. Am. 2014, 96, 292–300. [Google Scholar] [CrossRef] [PubMed]
- Delincé, P.; Ghafil, D. Anterior cruciate ligament tears: Conservative or surgical treatment? A critical review of the literature. Knee Surg. Sports Traumatol. Arthrosc. 2012, 20, 48–61. [Google Scholar] [CrossRef]
- Filbay, S.R.; Culvenor, A.G.; Ackerman, I.N.; Russell, T.G. Quality of life in anterior cruciate ligament-deficient individuals: A systematic review and meta-analysis. Br. J. Sports Med. 2015, 49, 1033–1041. [Google Scholar] [CrossRef]
- Harris, K.P.; Driban, J.B.; Sitler, M.R.; Cattano, N.M.; Balasubramanian, E.; Hootman, J.M. Tibiofemoral osteoarthritis after surgical or nonsurgical treatment of anterior cruciate ligament rupture: A systematic review. J. Athl. Train. 2015, 52, 507–517. [Google Scholar] [CrossRef]
- Smith, T.O.; Postle, K.; Penny, F.; McNamara, I.; Mann, C.J.V. Is reconstruction the best management strategy for anterior cruciate ligament rupture? A systematic review and meta-analysis comparing anterior cruciate ligament reconstruction versus non-operative treatment. Knee 2014, 21, 462–470. [Google Scholar] [CrossRef]
- Muaidi, Q.I.; Nicholson, L.L.; Refshauge, K.M.; Herbert, R.D.; Maher, C.G. Prognosis of conservatively managed anterior cruciate ligament injury: A systematic review. Sports Med. 2007, 37, 703–716. [Google Scholar] [CrossRef] [PubMed]
- Kovalak, E.; Atay, T.; Çetin, C.; Atay, İ.M.; Serbest, M.O. Is ACL reconstruction a prerequisite for the patients having recreational sporting activities? Acta Orthop. Traumatol. Turc. 2018, 52, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Morse, J.M.; Field, P.A. Qualitative Research Methods for Health Professional; SAGE Publications: Los Angeles, CA, USA, 1995. [Google Scholar]
- O’Reilly, M.; Parker, N. ‘Unsatisfactory Saturation’: A critical exploration of the notion of saturated sample sizes in qualitative research. Qual. Res. 2012, 13, 190–197. [Google Scholar] [CrossRef]
- Bowen, G.A. Naturalistic inquiry and the saturation concept: A research note. Qual Res. 2008, 8, 137–152. [Google Scholar] [CrossRef]
- Webster, K.E.; Feller, J.A.; Lambros, C. Development and preliminary validation of a scale to measure the psychological impact of returning to sport following anterior cruciate ligament reconstruction surgery. Phys. Ther. Sport 2008, 9, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Scherpenzeel, A. Why Use 11-Point Scales Research Gate. 2002. Available online: https://www.researchgate.net/publication/241262409_Why_Use_11-Point_Scales (accessed on 17 June 2022).
- Kemper, E.A.; Stringfield, S.; Teddlie, C. Mixed Methods Sampling Strategies in Social Science Research. In Handbook of Mixed Methods in Social and Behavioural Research; Tashakkori, A., Teddlie, C., Eds.; Sage Publications: Los Angeles, CA, USA, 2003; pp. 267–273. [Google Scholar]
- Palinkas, L.A.; Horwitz, S.M.; Green, C.A.; Wisdom, J.P.; Duan, N.; Hoagwood, K. Purposeful Sampling for Qualitative Data Collection and Analysis in Mixed Method Implementation Research. Adm. Policy Ment. Health 2015, 42, 533–544. [Google Scholar] [CrossRef] [PubMed]
- Thorne, S.; Reimer, K.S.; MacDonald-Emes, J. Interpretive description: A noncategorical qualitative alternative for developing nursing knowledge. Res. Nurs. Health 1997, 20, 169–177. [Google Scholar] [CrossRef]
- Thompson Burdine, J.; Thorne, S.; Sandhu, G. Interpretive description: A flexible qualitative methodology for medical education research. Med. Educ. 2021, 55, 336–343. [Google Scholar] [CrossRef]
- StataCorp. Stata Statistical Software; Release 17. 4905 Lakeway Drive; StataCorp LLC: College Station, TX, USA, 2021. [Google Scholar]
- Shapiro, S.S.; Wilk, M.B. An Analysis of Variance Test for Normality (Complete Samples). Biometrika 1965, 52, 591–611. [Google Scholar] [CrossRef]
- Burland, J.; Toonstra, J.; Werner, L.; Mattacola, G.C.; Howell, M.D.; Howard, S.J. Decision to Return to Sport After Anterior Cruciate Ligament Reconstruction, Part I: A Qualitative Investigation of Psychosocial Factors. J. Athl. Train. 2018, 53, 452–463. [Google Scholar] [CrossRef]
- Ross, A.C.; Clifford, A.; Louw, A.Q. Factors informing fear of reinjury after anterior cruciate ligament reconstruction. Physiother. Theory Pract. 2017, 33, 103–114. [Google Scholar] [CrossRef]
- Scott, M.S.; Perry, A.M.; Sole, G. “Not always a straight path”: Patients’ perspectives following anterior cruciate ligament rupture and reconstruction. Disabil. Rehabil. 2018, 40, 2311–2317. [Google Scholar] [CrossRef] [PubMed]
- Tjong, V.K.; Murnaghan, M.L.; Nyhof-Young, J.M.; Ogilvie-Harris, D.J. A qualitative investigation of the decision to return to sport after anterior cruciate ligament reconstruction: To play or not to play. American J. Sports Med. 2014, 42, 336–342. [Google Scholar] [CrossRef]
- DiSanti, J.; Lisee, C.; Erickson, K.; Bell, D.; Shingles, M.; Kuenze, C. Perceptions of Rehabilitation and Return to Sport Among High School Athletes with Anterior Cruciate Ligament Reconstruction: A Qualitative Research Study. J. Orthop. Sports Phys. Ther. 2018, 48, 951–959. [Google Scholar] [CrossRef] [PubMed]
- Ireland, M.L. The female ACL: Why is it more prone to injury? J. Orthop. 2016, 13, A1–A4. [Google Scholar]
- Noyes, F.R.; Barber-Westin, S. Return to Sport after ACL Reconstruction and Other Knee Operations: Limiting the Risk of Reinjury and Maximizing Athletic Performance; Springer: Cham, Switzerland, 2019. [Google Scholar]
- Filbay, S.R.; Crossley, K.M.; Ackerman, I.N. Activity preferences, lifestyle modifications and re-injury fears influence longer-term quality of life in people with knee symptoms following anterior cruciate ligament reconstruction: A qualitative study. J. Physiother. 2016, 62, 103–110. [Google Scholar] [CrossRef]
- Vutescu, E.S.; Orman, S.; Garcia-Lopez, E.; Lau, J.; Gage, A.; Cruz, A.I., Jr. Psychological and Social Components of Recovery Following Anterior Cruciate Ligament Reconstruction in Young Athletes: A Narrative Review. Int. J. Environ. Res. Public Health 2021, 18, 9267. [Google Scholar] [CrossRef]
- Sonesson, S.; Kvist, J.; Ardern, C.; Osterberg, A.; Silbernagel, K.G. Psychological factors are important to return to pre-injury sport activity after anterior cruciate ligament reconstruction: Expect and motivate to satisfy. Knee Surg. Sports Traumato. Arthrosc. 2017, 25, 1375–1384. [Google Scholar] [CrossRef]
- Truong, L.K.; Mosewich, A.D.; Holt, C.J.; Le, C.Y.; Miciak, M.; Whittaker, J.L. Psychological, social and contextual factors across recovery stages following a sport-related knee injury: A review. Br. J. Sports Med. 2020, 54, 1149–1156. [Google Scholar] [CrossRef]
- Mahood, C.; Perry, M.; Gallagher, P.; Sole, G. Chaos and confusion with confidence: Managing fear of Re-Injury after anterior cruciate ligament reconstruction. Phys. Ther. Sport. 2020, 45, 145–154. [Google Scholar] [CrossRef]
- de Oliveira, B.I.R.; Smith, A.J.; O’Sullivan, P.P.B.; Haebich, S.; Fick, D.; Khan, R.; Bunzli, S. ‘My hip is damaged’: A qualitative investigation of people seeking care for persistent hip pain. Br. J. Sports Med. 2020, 54, 858–865. [Google Scholar] [CrossRef]
- Darlow, B.; Dowell, A.; Baxter, G.D.; Mathieson, F.; Perry, M.; Dean, S. The enduring impact of what clinicians say to people with low back pain. Ann. Fam. Med. 2013, 11, 527–534. [Google Scholar] [CrossRef] [PubMed]
- Ohji, S.; Aizawa, J.; Hirohata, K.; Mitomo, S.; Ohmi, T.; Jinno, T.; Koga, H.; Yagishita, K. Athletic identity and sport commitment in athletes after anterior cruciate ligament reconstruction who have returned to sports at their pre-injury level of competition. BMC Sports Sci. Med. Rehabil. 2021, 13, 37. [Google Scholar] [CrossRef]
- Roelofs, K. Freeze for action: Neurobiological mechanisms in animal and human freezing. Philos. Trans. R Soc. Lond. B Biol. Sci. 2017, 372, 20160206. [Google Scholar] [CrossRef] [PubMed]
- Hoehn-Saric, R.; McLeod, D.R. The Peripheral Sympathetic Nervous System: Its Role in Normal and Pathologic Anxiety. Psychiatr. Clin. N. Am. 1988, 11, 375–386. [Google Scholar] [CrossRef]
- El-Badawy, M.A.; El Mikkawy, D.M. Sympathetic Dysfunction in Patients with Chronic Low Back Pain and Failed Back Surgery Syndrome. Clin. J. Pain 2016, 32, 226–231. [Google Scholar] [CrossRef] [PubMed]
- Oktem, E.O.; Cankaya, S. Empathy for Pain, Pain Management-Practices, Novel Therapies and Bioactives; IntechOpen: London, UK, 2021. [Google Scholar]
- Neto, T.; Sayer, T.; Theisen, D.; Mierau, A. Functional Brain Plasticity Associated with ACL Injury: A Scoping Review of Current Evidence. Neural Plast. 2019, 2019, 3480512. [Google Scholar] [CrossRef] [PubMed]
- Fanselow, M.S.; Sigmundi, R.A. Species-specific danger signals, endogenous opioid analgesia, and defensive behavior. J. Exp. Psychol. Anim. Behav. Process. 1986, 12, 301–309. [Google Scholar] [CrossRef]
- Lethem, J.; Slade, P.D.; Troup, J.D.; Bentley, G. Outline of a Fear-Avoidance Model of exaggerated pain perception--I. Behav. Res. Ther. 1983, 21, 401–408. [Google Scholar] [CrossRef]
- Moseley, L.; Butler, S.; Beames, B.T.; Giles, J.T. The Graded Motor Imagery Handbook, 1st ed.; Noigroup Publications: Adelaide, Australia, 2012. [Google Scholar]
- Pincus, T.; Henderson, J. Low back pain patients’ responses to videos of avoided movements. Eur. J. Pain 2013, 17, 271–278. [Google Scholar] [CrossRef]
- Lovalekar, M.; Abt, J.P.; Sell, T.C.; Lephart, S.M.; Pletcher, E.; Beals, K. Accuracy of recall of musculoskeletal injuries in elite military personnel: A cross-sectional study. BMJ Open 2017, 7, e017434. [Google Scholar] [CrossRef]

| ID | P1 | P2 | P3 | P4 | P5 | P6 | P7 | P8 | P9 | P10 | P11 | P12 | P13 | P14 | P15 | P16 | P17 | Mean (SD) | Median (IQR) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | 22 | 25 | 33 | 28 | 24 | 22 | 28 | 32 | 23 | 31 | 33 | 32 | 31 | 24 | 23 | 36 | 25 | 27.70 (4.58) | 28 (23.5, 32) |
| Sex | F | F | M | F | F | F | M | M | F | F | F | F | F | M | M | F | F | M:5, F:12 | |
| Tampa Scale of Kinesiophobia 1 | 19 | 17 | 33 | 23 | 23 | 18 | 21 | 17 | 17 | 31 | 25 | 17 | 22 | 25 | 30 | 18 | 30 | 22.71 (5.5) | 22 (17.5, 27.5) |
| ACL-Return to Sport Index (ACL-RSI) 2 | 39.4 | 34.2 | 25.8 | 41.7 | 52.5 | 28.3 | 53.3 | 63.3 | 66.7 | 20 | 16.7 | 65.8 | 18.3 | 31.7 | 47.5 | 41.7 | 15.8 | 38.98 (17.21) | 39.4 (22.9, 52.9) |
| Fear of movement 3 | 1 | 4 | 3 | 0 | 4 | 2 | 0 | 0 | 0 | 10 | 0 | 0 | 6 | 3 | 8 | 2 | 2 | 2.65 (3) | 2 (0, 4) |
| Distress/Anxiety related to knee movements 3 | 1 | 1 | 5 | 1 | 4 | 0 | 0 | 0 | 0 | 8 | 5 | 0 | 6 | 4 | 7 | 3 | 1 | 2.71 (2.73) | 1 (0, 5) |
| Lack of Confidence in Knee movements 3 | 0 | 8 | 7 | 2 | 5 | 2 | 0 | 0 | 0 | 10 | 5 | 0 | 6 | 4 | 6 | 5 | 4 | 3.76 (3.15) | 4 (0, 6) |
| Pain 3 | 1 | 7 | 2 | 1 | 6 | 0 | 2 | 0 | 0 | 3 | 0 | 0 | 6 | 1 | 2 | 3 | 1 | 2.06 (2.28) | 1 (0, 3) |
| Surgical reconstruction | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | Y:16, N:1 | |
| HCP Provided Psychological Support 4 | N | Y | N | N | N | N | N | Y | N | N | N | N | N | N | N | N | N | Y:2, N:15 | |
| Return to Previous level of function 5 | 2 | 2 | 0 | 3 | 3 | 2 | 3 | 3 | 3 | 2 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 0: 1, 1: 6, 2: 5, 3: 5 | |
| Year of ACL injury | ‘16 | ‘17‘18 | ‘16 | ‘16 | ’17 | ‘11‘16 | ‘17 | ‘11‘12 | ‘15 | ‘15 | ‘08 | ‘08 | ‘06‘09‘13 | ‘19 | ‘19 | ‘06 | ‘19 | ||
| Theme 1: Evoked Physiological Responses | |
| Quote 1 (Q1) | “I honestly stopped watching after the first rebound, it made me feel sick …”. (Participant 2; P2) |
| Q2 | “Like my body tenses and I sort of imagine that that’s your knee, and then your muscles will kind of tense up unconsciously to protect it. (P6)” |
| Q3 | “I get anxious when I see someone go down screaming in agonizing pain holding their knee knowing that it may be an ACL. I feel that pain but that’s only in terms of that stress and anxiety… I do grab at it (my knee) if I see someone lunging and grabbing at their knee. It’s weird.” (P14) |
| Q4 | “The immediate reaction that I have sometimes when you see other people tear their ACL is you want to go, “Oh, shit.” You physically check, “Is my knee still intact?” [laughs]. … It’s a phantom pain that you remember because it’s not that I’ve experienced that many super painful things in my life.” (P15) |
| Q5 | “Every time I see someone go down with a knee (injury), it doesn’t even have to be an ACL but I feel my knee twitch. If I see someone go down holding their knee, I will sometimes hold my knee, as well.” (P15) |
| Theme 2: Deeper Contextualisation of the Meaning of an ACL Injury Influencing Body Confidence | |
| Q6 | I think with the distress or how worried I am or was when I did it, a lot of that was already built up. If that makes sense. If I didn’t know nothing about it, or hadn’t seen it happen (referring to messages and clips in the media around snow sports), or had people that I knew do it, it probably wouldn’t have been as bad for me. I think about that a fair bit then I just worry about it more than I should. Does that make sense? (P3) |
| Q7 | I guess that (cut and pivot movement) made me feel like he should be careful doing that because that’s how you can get ACL injuries, changing directions really fast. (P12) |
| Q8 | If you want to play sports and push it hard you have got to expect that at some point something is going to go wrong…there is a fear that you are going to hurt yourself I think everyone has that. (P8) |
| Theme 3: Recall of Psychological Difficulties | |
| Q9 | It (series of traumatic knee injuries video) gives you bad memories and makes you not want to play sport again I reckon. Watching a compilation of ACL injuries especially the way that you did your one makes you think maybe you shouldn’t go back to playing netball again because that’s what’s going to happen, or that’s what could happen. (P12) |
| Q10 | It’s quite confronting because that’s probably what I looked like (when getting injured). (P13) |
| Q11 | I feel like I’m cautious watching them. I’m fearful of thinking of myself doing that (plant and cut action). (P17) |
| Q12 | I used to watch people change direction, it would give me that like, ‘uh, can’t imagine doing that’. (P9) |
| Q13 | “Ooh”. It was distressing to watch them because it looks so painful (referring to the cut and pivot + feigned injury and a series of traumatic knee injuries). A couple of times, while playing, I’ve ended up in something similar, so it’s more like a little bit anxiety as well, just feeling anxious about it because it brings back—I don’t know, bad memories. I distinctively remember falling on the ground and just touching my knee in pain in a similar situation. (P10) |
| Q14 | I feel like I just remember the exact feeling of it. The classic empathy kind of thing. I remember the exact feeling. How terrible it was. When I see those videos, I actually think more of the noise, (referring to the noise when sustaining ACL injury), I distinctly remember the noise. When I see those videos, I almost see the noise. (P17) |
| Q15 | I find that they (thoughts of injuries) just pop into my brain randomly and it makes me really uncomfortable because you’ve got to try and get it out (from your head) and think about something else which is why I really hate watching them because I don’t need … I just don’t want new fresh ones (thoughts) that decide they want to come in every now and again. (P5) |
| Theme 4: Negative Implications of a Re-Injury | |
| Q16 | I just feel bad for them knowing what they now have to go through (after watching cut and pivot with feigned injury). (P7) |
| Q17 | Already being on edge as I am, doing that and then just knowing that, “All right, well, should I try and give up competitive sports?” That’s the way I think, I just don’t want to do it. From the pain associated with it, the rehab and the time it takes and, like I’ve touched on, the financial implications of it as well. I always sympathize with the athletes when I see someone go down … you just see that (traumatic injury video), and you say, “Well there goes the next year of your career.” It’s the trauma, the injury, but also how it affects you, how it affects your livelihood, and whatnot. (P14) |
| Q18 | I guess, elite athletes when they do an injury, I know it’s their entire life, but that, they do have an entire team of people straight away onto it, doing everything for them to help them out. When its someone, a poor old pleb, they don’t realize how much of an impact it might have. (P4) |
| Q19 | You don’t want to see anyone’s knee bend that weird … that second of them thinking, “Oh, shit, my life is going to change considerably after this one second for the next few years. My life choices have changed, and my options are limited.” (P15) |
| Q20 | Feeling my joint absolutely just give way. It’s pretty messy, it’s not fun. You’re like, “That person’s really good,” and then being injured, and it’s like, “Oh, shit. That person’s life is going to change forever now.” It’s a pretty big deal. (P15) |
| Theme 5: Change to Athletic Identity | |
| Q21 | I do remember some nights just crying in bed, like not too many … because as I said before playing sport every day doing it because I love it so much and not being able to do it. Yeah, I definitely was crying in my bed some nights. (P1) |
| Q22 | I used to be the person that would say yes to anything. Anything sports-related, I would just say, “Yes, let’s do it, give it a try”. Now I don’t. (P11) |
| Q23 | But, on the court, I was mostly slower and less agile. I think that was just fear…I’ve convinced myself that I never will play as well, and that’s why I’m not doing it. (P2) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Little, C.; Lavender, A.P.; Starcevich, C.; Mesagno, C.; Mitchell, T.; Whiteley, R.; Bakhshayesh, H.; Beales, D. An Investigation of the Nature of Fear within ACL-Injured Subjects When Exposed to Provocative Videos: A Concurrent Qualitative and Quantitative Study. Sports 2022, 10, 183. https://doi.org/10.3390/sports10110183
Little C, Lavender AP, Starcevich C, Mesagno C, Mitchell T, Whiteley R, Bakhshayesh H, Beales D. An Investigation of the Nature of Fear within ACL-Injured Subjects When Exposed to Provocative Videos: A Concurrent Qualitative and Quantitative Study. Sports. 2022; 10(11):183. https://doi.org/10.3390/sports10110183
Chicago/Turabian StyleLittle, Cameron, Andrew P. Lavender, Cobie Starcevich, Christopher Mesagno, Tim Mitchell, Rodney Whiteley, Hanieh Bakhshayesh, and Darren Beales. 2022. "An Investigation of the Nature of Fear within ACL-Injured Subjects When Exposed to Provocative Videos: A Concurrent Qualitative and Quantitative Study" Sports 10, no. 11: 183. https://doi.org/10.3390/sports10110183
APA StyleLittle, C., Lavender, A. P., Starcevich, C., Mesagno, C., Mitchell, T., Whiteley, R., Bakhshayesh, H., & Beales, D. (2022). An Investigation of the Nature of Fear within ACL-Injured Subjects When Exposed to Provocative Videos: A Concurrent Qualitative and Quantitative Study. Sports, 10(11), 183. https://doi.org/10.3390/sports10110183







