Abstract
Fear is a factor contributing to poor return to sport after an anterior cruciate (ACL) injury, however the identification and assessment of fear is challenging. To improve understanding of fear, this study qualitatively and quantitatively assessed responses to videos depicting threat to knee stability in people who had experienced an ACL injury. ACL-injured participants who had above average fear on the Tampa Scale of Kinesiophobia and were at least 1-year post-injury/surgery were eligible. Participants were shown four videos depicting sequentially increasing threat to their knee stability (running, cut-and-pivot, feigned knee injury during cut-and-pivot, series of traumatic knee injuries). Qualitative interviews explored participants feeling related to viewing the videos. Participants quantitatively self-rated fear and distress in response to each video. Seventeen participants were included in this study (71% female, with an average time since last ACL injury of 5 ½ years). Five themes were identified: (1) Evoked physiological responses, (2) Deeper contextualisation of the meaning of an ACL injury influencing bodily confidence, (3) Recall of psychological difficulties, (4) Negative implications of a re-injury, and (5) Change to athletic identity. Quantitatively, direct proportionality was noticed between threat level and reported fear and distress. Specifically, participants reported increasing levels of fear and distress as the videos progressed in threat level, with the largest increase seen between a cut-and-pivot movement to a feigned injury during a cut and pivot. The results support the notion that in addition to being a physical injury, an ACL injury has more complex neurophysiological, psychological, and social characteristics which should be considered in management. Using video exposure in the clinic may assist identification of underlying psychological barriers to recovery following an ACL injury, facilitating person-centred care.
1. Introduction
The anterior cruciate ligament (ACL) provides proprioceptive feedback and mechanical stability within thef knee [1]. It is particularly important in supporting the knee during dynamic pivoting, acceleration, deceleration and change of direction movements, which are often performed in sports [1]. Injuries to the ACL are frequent [2], with almost 200,000 ACL reconstructions in Australia between July 2000 and June 2015 [3]. These injuries appear to be increasing [4], with many people not returning to their prior level of functioning. In a systematic review of 69 articles reporting on 7556 participants following a surgically managed ACL injury, only 55% of individuals returned to their competitive sport despite achieving successful surgical outcomes [5]. In another systematic review of 19 studies totalling 2175 participants after a surgically managed ACL injury, 37% did not return to any sport [6], with 65% citing psychological reasons, and 77% citing fear of re-injury as their main concern for failure to return to sport. This aligns with other research which identifies the significant role of psychological factors on return to sport, and recovery in general after an ACL injury [7,8,9].
The experience of an ACL injury can be traumatic and may lead to symptoms similar to post-traumatic stress disorder [10]. Behaviours such as avoidance, hesitation to attend therapy, guarding or protecting the knee during movement, and suboptimal performance may all be sequelae of underlying emotional and/or psychological distress [10,11,12]. Coupled with negative self-belief about knee function, this may increase an individual’s knee-related fear. Fear, which can be defined as “a basic, intense emotion aroused by the detection of imminent threat” [13]. Fear of re-injury is one of the most commonly reported reasons for not returning to sport in individuals who have suffered an ACL injury [7,8,14,15,16,17].
Fear may be heightened, or attenuated, through subconscious and conscious learning mechanisms [18]. Fear conditioning refers to the subconscious process wherein a previously non-fearful stimulus, such as playing sport, becomes associated with an unconditioned fearful stimulus, such as a traumatic injury event. The fear of the unconditioned injury, conditions the individual to also fear the previously non-fearful sport [18]. A conditioned fear response may also increase a person’s distress. Distress, defined as “a general term to describe a state of emotional suffering that interferes with the level of functioning” ([19], p. 877), may produce subconscious defensive or avoidance behaviours, such as a fight or flight response [20]. Distress and fear, whilst likely having some conceptual overlap [21], may differ in the context of an ACL injured individual. These individuals may be suffering emotionally and avoiding return to activities ([19], p. 877), but not necessarily fearful of an imminent threat [13]. Conscious thoughts and experiences can also contribute to fear [22].
Researchers who investigated lower back pain found that the conscious processing of a threat (to physical well-being) is complex and both physical and psychosocial factors can contribute to a heightening, or reduction, of fear [23,24,25]. In disorders such as chronic lower back pain, fear of movement has been assessed by exposing participants to potentially threatening stimuli, including pictures [26] and videos [27,28,29]. For example, participants with lower back pain exposed to four-second videos depicting potentially hazardous movements (e.g., shovelling soil with a bent back) demonstrated significantly greater brain activity, using Functional Magnetic Resonance Imaging, in regions of the brain that processes fear (e.g., amygdala and left anterior insula) compared to viewing harmless activities [29]. In a study of an ACL-injured cohort, nearly half (45.5%) identified cutting (i.e., planting the foot and changing direction by 90°) as the most feared movement [30]. Exposing people who have suffered an ACL injury to videos depicting potentially threatening stimuli may evoke a fear response that could offer clinical insight.
This study exposed people minimum 1-year after an ACL-injury/surgery to a series of videos depicting sequentially increasing threat to knee stability. The qualitative arm explored participants feelings related to viewing the videos, whilst the quantitative arm explored participants self-rated fear and distress levels in response to the videos. The overarching purpose of this study was to provide further insight into the nature of fear after an ACL injury. In addition, we aimed to provide some initial indication of the viability of using a video medium to assess fear in people who had experienced an ACL injury in the return to sport phase of their rehabilitation.
2. Materials and Methods
2.1. Study Design
A concurrent qualitative and quantitative design was selected, with both data types interpreted and merged during the Discussion phase [31,32]. Fear and distress responses were documented in participants during a series of videos depicting increasing threat to the knee, specifically: running, a cut-and-pivot action, a cut and pivot + a feigned knee injury, and a series of video clips of traumatic knee injuries. Qualitative data was gathered from individual participant experiences and feelings when viewing the series of threatening movements, to allow for a deeper understanding of the fear and distress associated with ACL injuries. The qualitative component of the study was aligned to the Consolidated Criteria for Reporting Qualitative Research (COREQ) guidelines, a 32 item checklist designed for explicit, comprehensive reporting of qualitative data [33]. Quantitative data was collected through self-reported ratings for fear and distress following each video. Data integration of the qualitative and quantitative components was conceived across the design and commented on in the Discussion [34]. Consumer engagement for feasibility, appropriateness and effectiveness of study [35] with three ACL-injured individuals (31-year-old male, 32-year-old female, 33-year-old male, not included in Table 1) occurred in the development of the study. This involvement included assistance in the generation of the research question and piloting of the videos depicting the sequentially threatening movements, with the aim to ensure the appropriateness and safety of the videos for this study. In addition, after 12 interviews these consumers were also given the opportunity to comment on the results. This feedback indicated that results were representative of the engagement group beliefs.

Table 1.
Participant Data.
2.2. Participants
Participant inclusion criteria were: aged 18–50, and either at least 1-year post injury without surgery or 1-year post ACL reconstruction surgery [36]. Surgically or conservatively managed participants were combined given similar long-term patient reported outcomes of knee function, activity levels, and quality of life [37,38,39,40,41,42,43]. Eligible participants had to report ‘above average’ fear through scoring more than 17 on a modified Tampa Scale Kinesiophobia (TSK). This scale has previously been used to identify fear of movement in an ACL reconstructed cohort, wherein the median score (average fear) equalled 17 [17] with those above considered to have above average fear. Potential participants were excluded for any of the following: non-English-speaking background, multiple pain sites, or low back pain with radicular signs.
2.3. Sampling and Power
The sample size was determined as the point where the qualitative data saturation occurred. This was determined by iteratively reviewing participant information to ensure the appropriateness and adequacy of collected data [44,45], with the depth and breadth of results determined to be deemed sufficient by the interdisciplinary team [45,46]. The nature of an iterative approach means there will be constant evolution of new themes. Saturation was reached after 16 interviews; one more interview was completed to ensure no new themes were discovered [45,46].
2.4. Measures
Participant profiling data included age, sex, year of the ACL injury(s), and if they had an ACL reconstruction. A modified TSK to include knee specific questions rather than pain was collected from participants as an indication of fear of movement [17]. The TSK was rated from 0–51, with a higher score indicating higher levels of fear. The Anterior Cruciate Ligament-Return to Sport Index (ACL-RSI) was used as an indication of psychological readiness to return to sport [47]. This scale is rated out of 100 with lower scores indicating higher impairment.
Participants were asked how much they had been ‘bothered’ by their knee in the last week across four constructs: (1) fear of movement, (2) distress/anxiety related to knee movements, (3) lack of confidence and (4) pain (rated from 0–10 where 0 was no bother at all and 10 was extremely bothered). The return to previous level of function was scored from 0 to 3 with: no return to any exercise = 0, return to basic exercise (gym, etc.) but no sport = 1, return to sport at a lower level than previous = 2, or return to previous level of sport = 3.
Standardised instructions, covering testing procedure and a safety caveat were provided prior to watching the first video, this included clear instructions that participants could stop testing at any time if they felt uncomfortable. Following the first video (running), quantitative data was collected by asking participants to self-rate their level of fear from 0 (no fear at all) to 10 (extreme fear). ‘Distress’ then replaced ‘fear’ in the question to attain a distress score. An 11-point scale was chosen to allow better discrimination between the participant scores [48]. Participants were then asked, ‘How do you feel about this video?’ to collect qualitative information.
The same procedure for quantitative and qualitative was followed after each subsequent video (a cut-and-pivot action, a cut and pivot + a feigned knee injury, and a series of video clips of traumatic knee injuries). After the four-video protocol was completed, participants were asked an open-ended question, “Did any of these videos make you feel any similar emotions or fear to what you experienced during your own ACL injury?” (referring to both the initial injury and the rehabilitation journey) with, a follow up question, “can you explain to me why/why not?”. The interviewer then allowed participant to guide the discussion and prompted any points requiring clarification.
At the cessation of testing, an informal discussion was undertaken for a minimum of 5 min, this was to ensure participants had not had any ongoing emotional effects as a result of watching the videos. During this time, participants were asked ‘how they were feeling’ and whether there was any ‘psychological aggravation’ as a result of the testing protocol. Participants were subsequently contacted within 24 h to ensure no aggravation had occurred. No participants had ongoing emotional effects after the testing.
2.5. Procedure
Participants were recruited between October and December 2020 using a social media advertisement shared via Facebook. The social media advertisement contained a link to an online questionnaire, which participants completed to determine their eligibility for the study. Key information on the study design was provided to allow participants to give informed consent. General principles of participant sampling were used to ensure the quality of the sample, including making the sampling feasible, affordable, and specific to the research question whilst acknowledging and minimising biases [49]. Non probabilistic purposive sampling was used to identify the participants, which consisted of ACL-injured individuals who could articulate their emotions. This technique identified information rich cases for the most effective use of resources [50]. No financial reward was offered to take part in the study.
Videos were created to assess participants’ fear and distress by exposing them to sequentially increasing threatening stimuli, with Video S1 being the least threatening, and Video S4 being the most threatening [30]. Each of the first three videos was looped twice and ran for 25 s in total, while Video S4 was not looped and ran for a similar time. Participants were shown the series of four videos, from least to most threatening. This was to ensure participant well-being, guided by pilot group testing and feedback, which had shown a potential for a significant negative reaction to the later injury videos. By keeping the videos sequential, we ensured that any adverse reactions were identified in the earlier videos and minimised.
- Video S1 ‘Running’: shows the video athletes running in a straight line at a low to moderate intensity for 10 s, followed by a gentle turn to leave the video frame -this was considered a baseline video showing a common, very lower-level activity
- Video S2 ‘Cut and Pivot’: shows the video athletes running forward at a low to moderate intensity for nine seconds, then completing a cut and pivot movement (i.e., planting one foot and turning sharply at a right angle) then continue off screen—this is the most commonly reported fearful movement for people following ACL injury [30].
- Video S3 ‘Cut & Pivot with feigned knee injury’: shows the video athletes running forward at a low to moderate intensity for nine seconds, then completing a sharp cut and pivot motion (as in Video 2) and then feigning a knee injury by holding the knee and falling down (reproducing an injury).
- Video S4 ‘Knee injury clips’: shows a series of video clips of traumatic knee injuries compiled from YouTube, representing a series of more graphic injuries (both male and female)
YouTube links to videos can be found in Supplementary Material (Videos S1–S4).
A guiding principle in the creation of the videos was to avoid bias that might affect participants’ responses. Potential biases affecting an individual’s fear/distress included (but were not limited to) the setting/location, the backdrop of the movements, and participant specific factors (e.g., age, gender, body type, and clothing). To minimise bias, filming of Videos S1, S2 and S3 was completed in a grassy location with an unremarkable backdrop of trees in the medium-far distance. This location was selected to not emulate a sports field, as a specific field may have resonated more with one participant over another. One male actor and one female actor, aged around 30 years, of average build, were selected for the videos. Both wore the same plain, unlabelled, unisex, neutral (blue and black) clothing (Figure 1). Videos were edited to show both the male and female simultaneously in a split-screen format. This was to allow the participants to watch/identify with either male or female actor.

Figure 1.
Video athletes.
2.6. Qualitative Data Analysis
All interviews were performed by CL, a titled physiotherapist with experience in patient centred interviewing and PhD candidate, who has experience in elite sport and ACL injuries both personally and professionally. Interviews were audio-recorded, transcribed verbatim, entered into NVIVO 12 (QSR International, Melbourne, Australia) and analysed using an interpretive descriptive framework [51]. Qualitative data from each video were pooled for analysis to allow for an overall presentation of the fear response. The methodological steps were closely followed throughout the analysis [52]. This involved two coders CL and CS, a titled physiotherapist and PhD candidate with experience in the clinical management and research of ACL injuries, independently coding the data. The coders used an inductive open coding method whereby codes were identified from the data and not preconceived. Inductive coding was first completed on 12 transcripts. Coders then discussed and synthesized their codes to create a single codebook and retrospectively applied this codebook to the first 12 transcripts, paying particular attention to any concepts that were not captured by the codebook. Once the coders were satisfied that the codebook accurately captured all relevant raw data, the codes were then presented to the broader research team for further discussion: DB, a specialist musculoskeletal physiotherapist and senior research fellow with expertise in the biopsychosocial nature of musculoskeletal disorders, CM, a Sport and Exercise Psychologist with over 20 years expertise in stress and anxiety in sport and exercise, and AL, a Senior researcher and lecturer in sports science. Through group discussion and negotiation, codes were further refined. Coders then completed coding of the remaining interviews to test, challenge, and refine the final themes.
2.7. Quantitative Data Analysis
Quantitative analyses were performed using Stata 16.1 [53]. Fear and distress were treated as separate dependent variables and modelled separately. Data was checked for normality with the Shapiro–Wilk test [54], with the majority of variables reaching the threshold for normality. Linear mixed models with random subject effects were used to analyse the relationship between both fear and distress for the four video conditions. Margins plots were created and post hoc pairwise comparisons (Tukey’s test) were used to compare the differences between the individual videos. Results were reported as the estimated mean difference, 95% Confidence Intervals (95% CI) and the associated p value.
3. Results
3.1. Participant Characteristics
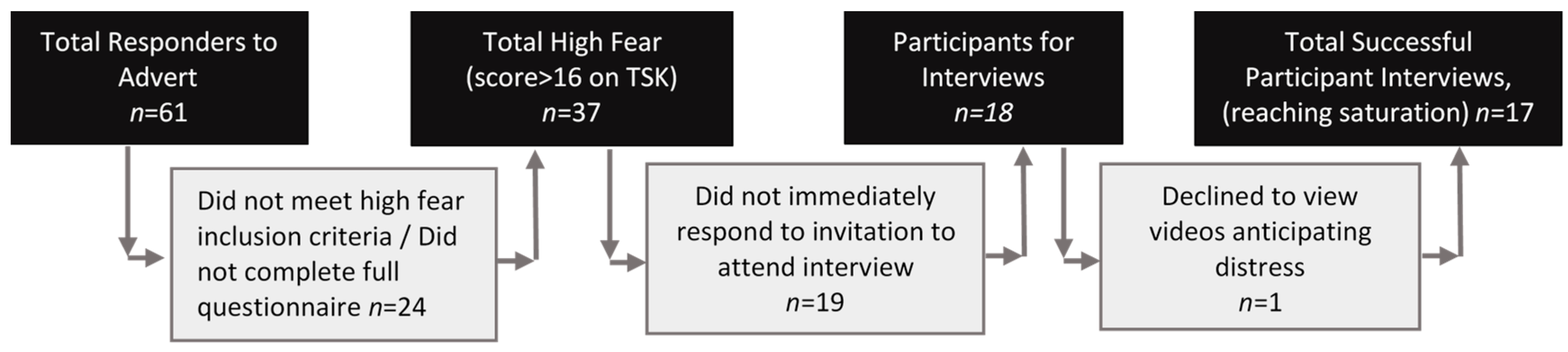
A total of seventeen participants 1-year post-ACL injury/surgery with high fear on the TSK were included (Figure 2, Table 1). The average age was 28 years, 71% were female, with an average time since their last ACL injury of 5.5 years. Sixteen of the seventeen participants had their injury managed surgically. Ten out of the seventeen participants returned to competitive sport at some level. Further demographics about the participants injury and sport is listed in Table S1.
Figure 2.
Flow diagram for participant recruitment.
3.2. Qualitative Results
Five themes were identified from the qualitative responses to the threatening stimuli (see Table 2 for supporting quotes—these are referenced in the relevant text, full transcripts are available in Supplementary Material Text S1).

Table 2.
Supporting quotes for Thematic Analysis.
3.2.1. Theme 1: Evoked Physiological Responses
Some participants reported physiological reactions (i.e., automatic, instinctive, unlearned responses) when watching the feigned injury (Video S3) and the knee injury videos (Video S4). These participants described a range of involuntary reactions, including a muscle ‘twitch’ (Quote 5, Q5) or a ‘tensing’ around the knee (Q2), as well as feeling ‘sick’(Q1). A few participants also reported feeling pain in the knee while viewing the videos, attributing this pain to psychological drivers such as ‘anxiety’ (Q3) or a ‘phantom pain’ (Q4). Participants reported wanting to physically reassure themselves (Q4) by ‘touching’ their knees (Q3–Q5).
3.2.2. Theme 2: Deeper Contextualisation of the meaning of an ACL Injury Influencing Body Confidence
Participants discussed beliefs about their own ACL injury in response to watching the threatening videos. They spoke of unhelpful extrinsic messages from those around them, such as those given by medical professionals, friends and/or societal/media messages, which shaped their evaluation of their knee stability and susceptibility to injury (Q6). These participants reported experiencing high levels of fear, which they attributed to beliefs of weakness and vulnerability of their own ACL-injured knee. For example, Participant 8 stated that any return to sport (after an ACL injury) involves risk of re-injury and there is an expectation that something will ‘go wrong’ (Q8), a message he gleaned from his rehabilitation team. Intrinsic messages of the perception of their knee and beliefs about knee function were shaped by personal experiences. Beliefs about weakness of the knee, and susceptibility of the knee to a re-injury (Q7), resulted in reduced confidence.
3.2.3. Theme 3: Recall of Psychological Difficulties
Most participants reported psychological effects experienced during the injury journey when viewing the videos. For some participants, the video exposure resulted in a personal recount of their own injury such as, bringing back ‘bad memories’ (Q9, Q13), or remembering the moment of their own ACL injury, the ‘exact feeling of it’ and the ‘noise’ (Q14). Others discussed how ‘confronting’ (Q10) and fearful the movements in the video (referring to the plant and cut movement) were to them in the present time (Q11, Q12).
3.2.4. Theme 4: Negative Implications of a Re-Injury
When watching the feigned injury and the series of traumatic knee injury videos, participants thought about what effects a re-injury would have on their own quality of life. Participants expanded on what the ACL injury had meant to them, not just from the pain and injury but from the wider psycho-social consequences (Q16, Q17). The negative consequences of a re-injury and factors that influenced fear appraisal included: rehabilitation (Q17, Q18), socio-economic implications (Q17), and changes to an individual’s function, life, and identity (Q20) ‘for the next few years’ (Q19).
In response to the feigned injury and the traumatic knee injury video, some participants reported how their previous ACL injury had changed their sporting lives (Q21–Q23). They reported a loss of athletic identity because they felt they were no longer capable of playing at their previous level. This had a negative impact on their sporting activities and overall physical confidence. For example, one participant indicated a perceptual shift from being the person who would ‘say yes to anything’ to becoming avoidant of physically challenging activities (Q22). These participants expressed increased fear and negative emotions related to not being able to play sport again; ‘yeah, I was crying in my bed some nights’ (Q21).
3.3. Quantitative Results
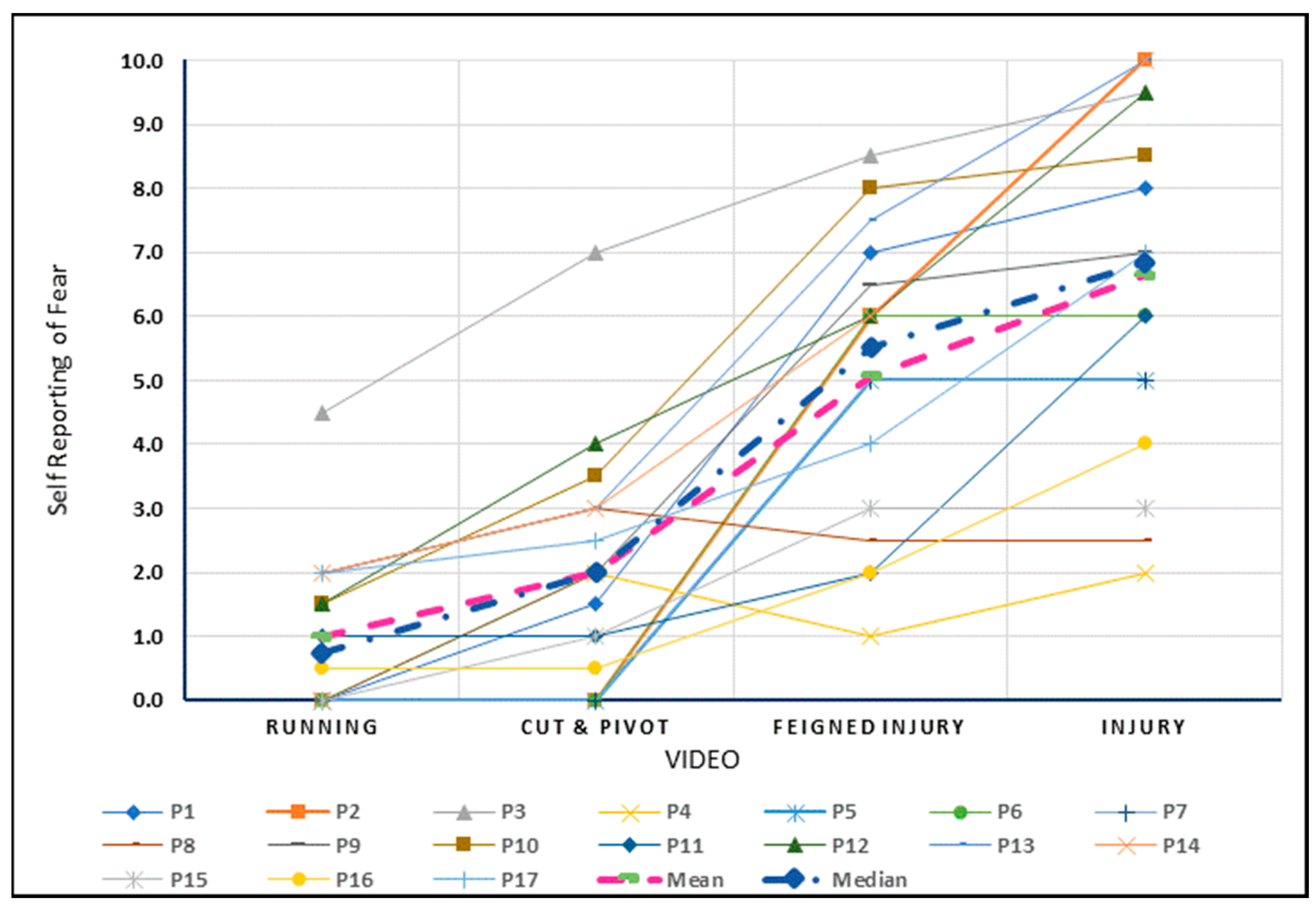
3.3.1. Self-Reported Fear
Figure 3 depicts the individual and group level changes for the rating of fear with exposure to the four levels of increasing threat. The quantitative results indicated a significant increase in the fear rating for each increment in the four videos. The largest increment between exposures for fear was found when participants moved from observing the cut and pivot (Video S2) to the feigned injury (Video S3) with an estimated mean difference of 3.1 on a scale of 0–10 (95% CI 2.1–4.0, p < 0.001). (Linear Mixed Models Analysis is provided in Table S2).
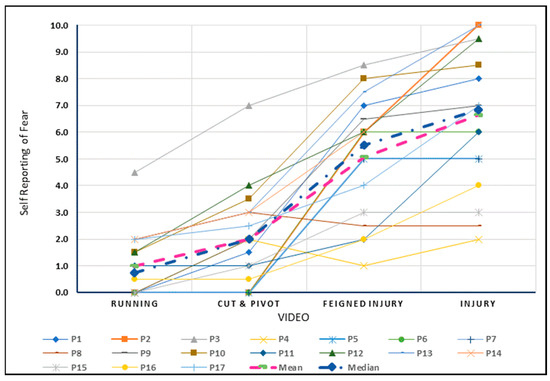
Figure 3.
Self-reported fear viewing videos depicting increasing threat to the knee.
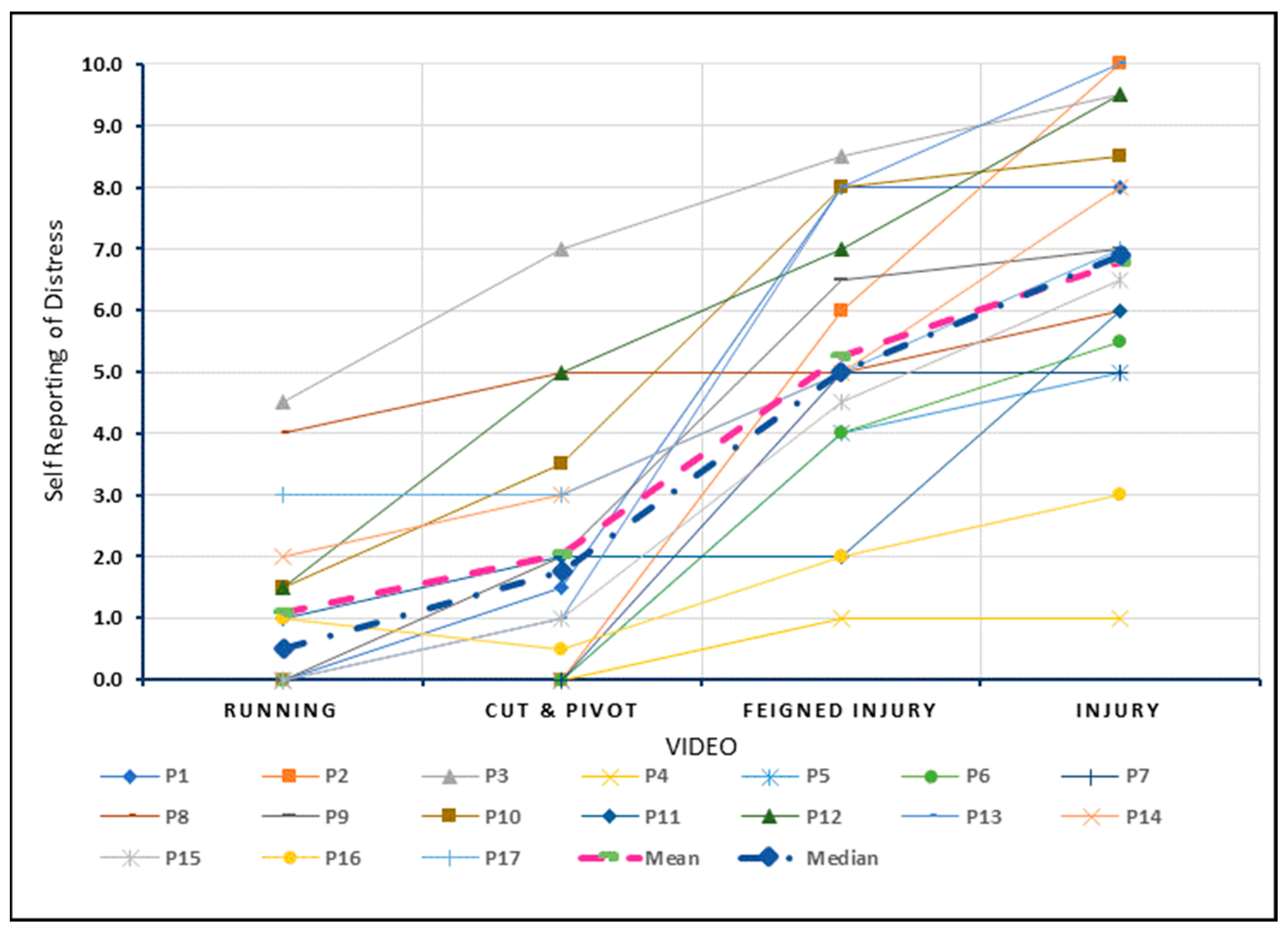
3.3.2. Self-Reported Distress
Figure 4 depicts the individual and group level changes for the rating of distress with exposure to the four levels of increasing threat. The linear mixed model results indicate a significant increase in distress for each increment. The largest increment between exposures for distress was also observed from cut and pivot (Video S2) to the feigned injury (Video S3) videos with an estimated mean difference of 3.2 (95% CI 2.3–4.2, p < 0.001). (Linear Mixed Models Analysis output is provided in Supplementary Material Table S2).
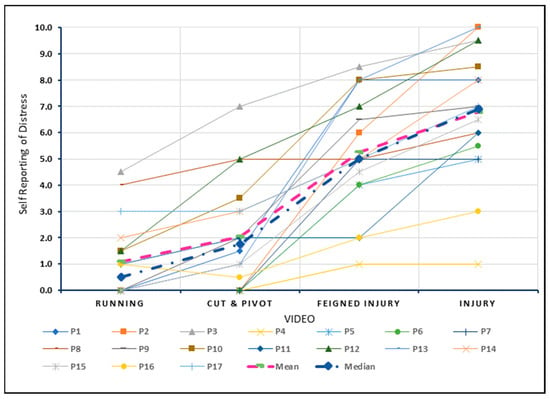
Figure 4.
Self-reported distress viewing videos depicting increasing threat to the knee.
4. Discussion
The purpose of the current study was to improve understanding of fear and distress, using qualitative and quantitative methodologies, within an ACL-injured cohort with above average fear during exposure to videos depicting sequentially increasing threat to knee stability. In doing so a range of responses (qualitative themes) were identified. The themes including physiological reactions to viewing the videos (such as participants rubbing their knee to soothe and protect themselves), contextual information affecting confidence, negative psychological associations, concerns about the ramifications of a re-injury and changes to their athletic identity. These themes were complementary [32] to quantitative ratings of fear and distress, in that with both the qualitative and quantitative outcomes, witnessing an injury (feigned or real) evoked the strongest responses, with the qualitative themes adding depth and breadth to the quantitative data.
4.1. Comparisons to the Literature
A number of studies using qualitative methodology to investigate the lived experience of an ACL-injury have touched on the concept of fear of re-injury [55,56,57,58,59]. These studies largely explored the practical consequences of the injury such as fear of surgery, the rehabilitation journey and socioeconomic considerations of a re-injury [56,57,58,59,60]. Unlike those prior studies, this study used videos to elicit a real-time response to a perceived threat, as opposed to asking people with an ACL-injured knee to recall their experience. Despite this difference in methodology similar constructs emerged in our data (Table 2) including fear of the rehabilitation process [56,58,59], social changes [56,57,58], and changing identity [57]. Similarities between the qualitative themes of this study and other non-qualitative research can also be identified. A range of factors such as fiscal position and time off work [61], the level of trauma associated with the initial injury [10], the duration and difficulty of the ACL recovery process [39,62] and rehabilitation [63] have been previously identified as factors which can affect return to previous level of function.
During testing, participants reported a range of psychological effects from viewing the videos including anxiety and rumination (Table 2). The substantial psychological effect of an ACL injury has also been identified in other research [61,63,64,65]. The combined importance of psychological, social factors and physiological changes seen in this cohort supports the notion in this broader literature that an ACL injury results in a wide range of effects which can drive fear and distress.
The quantitative results for fear and distress were broadly equivalent (Table S2, Figure 3 and Figure 4), suggesting it may be difficult to untangle fear from distress within an ACL injured cohort. Despite psychological effects being universally reported, only 2 out of 17 participants were asked by their healthcare professionals about their mental health during the rehabilitation process (Table 1). Those enquiries were in relation to return to sport performance, not related to the broader emotional and psychosocial health of the participants. Positive psychological support has been shown to be important in managing fear following an ACL-injury [66]. As fear of re-injury is a significant barrier for return to sport after an ACL injury [7,8,14,15,16,17], our findings support the notion that healthcare professionals can overly focus on the physical aspects of surgical repair and rehabilitation stages, while the issue of psychological support is often not considered.
There were indications of messaging from society and healthcare professionals that contributed to the beliefs underlying fear (Table 2). This is consistent with observations related to other musculoskeletal conditions such as persistent hip pain [67] and chronic low back pain [68]. Messages of damage, weakness and vulnerability, and messages reducing an individual’s control of their injury can all have a significant negative effect on functional outcomes [67,68]. There is a greater need to understand how messages from society, close contacts and healthcare professionals might contribute to fear after an ACL injury. Further, these messages seem to have a link to the individual’s athletic identity. Some individuals with stronger athletic identity report more emotional trauma following an ACL injury due to the increased challenge to their self-purpose [10,65], although this association is complex [69].
Perceived physiological reactions reported in this cohort may have been driven through activation of the sympathetic nervous system (SNS) in response to the perceived threats [70]. Similar responses (in the SNS) have been observed in people with other conditions and injuries when exposed to threatening stimuli, such as anxiety disorders [71] and chronic low back pain [72]. Within this cohort, increased heart rate, sweating, faster breathing and feeling ‘distressed/sick’ (e.g., Quote 1) could all be signs of a SNS reaction [20]. It should also be noted that these physiological responses could represent an empathic reaction of the participant towards the actors when viewing the videos [12]. Functional Magnetic Resonance Imaging studies have indicated that similar areas of the brain are involved during pain and pain empathy, and the latter can be activated when watching a painful scenario [73]. Further research comparing people with high and low fear after an ACL-injury exposed to a threatening video stimulus may provide further insight into the specific contribution of ‘pain empathy’ versus the heightening of fear from an ACL injury. Assessing biomarkers in the brain [74] may also assist in understanding the physiological sequelae of watching the threatening stimuli.
Fear in this cohort is likely to be complex and multifactorial. The participants often exhibited defensive, protective mechanisms in response to the videos, a behaviour that may be explainable through the concept of fear conditioning [75]. Responses within this cohort supporting fear conditioning [25] included behavioural (e.g., avoidance of an activity), perceived physiological (e.g., increased muscle tension) and cognitive responses (e.g., catastrophizing the injury or recalling the psychological difficulties). The Fear Avoidance Model (FAM) [76] may help to explain this cohort’s behavioural cycle. The FAM has been used to explain the cycle of fear, avoidance and disuse in conditions such as chronic low back pain [23]. In the FAM, a range of biological, psychological, and social factors following an injury may heighten pain and dysfunction, further reinforcing fear (and avoidance), thus creating a cycle of chronic disability and suffering [23,24]. Although pain, a driver in the FAM, was not a commonly reported issue within this cohort, a range of protective biopsychosocial factors, which heightened fear and avoidance could be seen [77,78].
4.2. Strengths
The use of videos represents a novel, low-risk method to assess fear of re-injury and distress in people who have experienced an ACL-injury. This was performed in real time, rather than relying on patient recall, with self-reported injury data being generally poor [79]. This may allow clinicians and patients to enter into a dialogue around a patient’s emotions and develop strategies if they are a barrier to function.
4.3. Limitations
Participants were included in this study via a designation of ‘above average fear’ dependent on their score on the TSK [17]. However, this questionnaire, despite being commonly utilised within the ACL literature, does not appear to have been fully validated in people following an ACL-injury. To the best of our knowledge there is no current psychometric scale that specifically assesses fear following ACL injuries. The multi-faceted nature of fear may not be adequately measured using a psychometric scale that is focused only on fear of painful movements (TSK), as evidenced by the broader variety of fear responses seen in this study. Within the development of the videos, we attempted to reduce any potential bias that would affect results. However, we acknowledge the likelihood of inherent biases which may impact different people (e.g., age, ethnicity and mechanism of injuries). Future studies with a wider diversity of participants would better help the generalisability of these videos for a broader cross-section of society.
The order of the videos may have been a limitation in the study. We considered the possibility of an ‘order effect’ of increased participant scores to the later videos due to the sequential nature of the videos. However, through consumer engagement we determined that participants may have strong adverse effects to watching the fearful stimuli. Keeping it ordered from least to most threatening allowed participants to exit the testing procedure at any point of time if required, improving participant safety. Future studies may use video randomisation to reduce order effects.
Our final sample included one person managed conservatively. While it was not the aim of this study to compare people managed surgically versus conservatively, given similar long-term outcomes for both groups [37,38,39,40,41,42,43] it is possible that the responses in these two groups might differ. We do not know if the responses provoked from the videos are specific to people with ACL injuries or are results that could be mirrored in the general population or in people following other lower limb injuries. Further work is needed to investigate the responses to the video stimuli in these alternate cohorts to determine the relevance of the results to an ACL injured cohort.
4.4. Clinical Significance
This study provides a novel way of assessing fear in people who have experienced an ACL injury. The video testing procedure is relatively quick to administer and provides a useful measure that could potentially be used for re-assessment purposes. This video procedure may be particularly useful in later stage rehabilitation. Showing a video in a clinical environment may provide additional insight compared to speaking about it in isolation. Further, if questioned in a clinical setting the person concerned may be guarded in their responses or not sufficiently self-aware of their psychological barriers to be able to answer effectively. The results of this study indicated that exposure to the videos initiated and promoted an open discussion, particularly in relation to the psychological barriers effecting return to activities. Clinically, this may lead to improved identification of these barriers and refinement of rehabilitation programs.
Of note was the identification of a number of subjects who had physiological reactions to the videos. To the best of our knowledge this has not been reported in other ACL and fear literature. Physiological responses may be a strong indicator of subconscious fear conditioning, the identification of which may further assist in fashioning effective clinical management strategies.
5. Conclusions
Fear is a significant barrier to optimal outcomes after an ACL injury. This study, using qualitative and quantitative methodology, has shown that people with an ACL injured knee can report significant fear and distress when shown videos depicting threat to their knee. This cohort reported a broad range of themes including (1) Evoked physiological responses, (2) Deeper contextualisation of the meaning of an ACL injury influencing bodily confidence, (3) Recall of psychological difficulties, (4) Negative implications of a re-injury, and (5) Change to athletic identity. Viewing a feigned or real injury appeared to evoke stronger responses than activities performed without an injury occurring. The fear narrative is participant-specific. The results support the notion that in addition to being a physical injury, an ACL injury has more complex neurophysiological, psychological, and social characteristics which should be considered in management. Using video exposure in the clinic may assist identification of underlying psychological barriers to recovery following an ACL injury, facilitating person-centred care.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/sports10110183/s1. Video S1: Running (https://youtu.be/zr6NpqrDpQk) accessed on 1 October 2022; Video S2: Cut and Pivot: (https://youtu.be/3zCg5ifP2dY) accessed on 1 October 2022; Video S3: Cut and Pivot + Feigned injury( https://youtu.be/LyTV9UqswMc) accessed on 1 October 2022; Video S4: Series of Traumatic injury videos: Available on request to main author. Table S1: Participant injury and sport; Table S2: Linear mixed models analysis; Text S1: Transcripts.
Author Contributions
Conceptualization, C.L. and D.B.; Formal analysis, C.S., C.M. and D.B.; Investigation, C.L., A.P.L., C.S., C.M., H.B. and D.B.; Methodology, C.L., T.M., R.W., H.B. and D.B.; Project administration, D.B.; Supervision, A.P.L., C.M., T.M., R.W. and D.B.; Writing—original draft, C.L. and D.B.; Writing—review and editing, C.L., A.P.L., C.S., C.M., T.M., R.W., H.B. and D.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding. The videos were paid for through a PhD stipend.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of Curtin University, the University Human Research Ethics Committee (HRE2020-0655) 2 November 2022 for studies involving humans.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy reasons.
Acknowledgments
Statistics assistance by Angela Jacques (Curtin University).
Conflicts of Interest
The authors declare no conflict of interest.
References
- Filbay, S.R.; Grindem, H. Evidence-based recommendations for the management of anterior cruciate ligament (ACL) rupture. Best Pract. Res. Clin. Rheumatol. 2019, 33, 33–47. [Google Scholar] [CrossRef] [PubMed]
- Ardern, C.L.; Taylor, N.F.; Feller, J.A.; Webster, K.E. Fear of re-injury in people who have returned to sport following anterior cruciate ligament reconstruction surgery. J. Sci. Med. Sport 2012, 15, 488–495. [Google Scholar] [CrossRef]
- Zbrojkiewicz, D.; Vertullo, C.; Grayson, J. Increasing rates of anterior cruciate ligament reconstruction in young Australians, 2000–2015. Med. J. Aust. 2018, 208, 354–358. [Google Scholar] [CrossRef] [PubMed]
- Maniar, N.; Verhagen, E.; Bryant, A.L.; Opar, D.A. Trends in Australian knee injury rates: An epidemiological analysis of 228,344 knee injuries over 20 years. Lancet Reg. Health-West. Pac. 2022, 21, 100409. [Google Scholar] [CrossRef] [PubMed]
- Ardern, C.L.; Taylor, N.F.; Feller, J.A.; Webster, K.E. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: An updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br. J. Sports Med. 2014, 48, 1543–1552. [Google Scholar] [CrossRef]
- Nwachukwu, B.; Adjei, J.; Rauck, R.; Chahla, J.; Okoroha, K.; Verma, N.; Allen, A.A.; Williams, I.R.J. How Much Do Psychological Factors Affect Lack of Return to Play After Anterior Cruciate Ligament Reconstruction? A Systematic Review. Orthop. J. Sports Med. 2019, 7, 2325967119845313. [Google Scholar] [CrossRef] [PubMed]
- Ardern, C.L.; Taylor, N.F.; Feller, J.A.; Whitehead, T.; Webster, K. Psychological responses matter in returning to pre-injury level of sport after anterior cruciate ligament reconstruction surgery. Am. J. Sports Med. 2013, 41, 1549–1555. [Google Scholar] [CrossRef]
- Flanigan, D.; Everhart, J.; Pedroza, A.; Smith, T.; Kaeding, C. Fear of reinjury (kinesiophobia) and persistent knee symptoms are common factors for lack of return to sport after anterior cruciate ligament reconstruction. Arthroscopy 2013, 29, 1322–1329. [Google Scholar] [CrossRef]
- Nwachukwu, B.U.; Voleti, P.B.; Berkanish, P.; Chang, B.; Cohn, M.R.; Williams, R.J.; Allen, A.A. Return to play and patient satisfaction after ACL reconstruction: Study with minimum 2-year follow-up. J. Bone Jt. Surg. 2017, 99, 720–725. [Google Scholar] [CrossRef] [PubMed]
- Padaki, A.S.; Noticewala, M.S.; Levine, W.N.; Ahmad, C.S.; Popkin, M.K.; Popkin, C.A. Prevalence of Posttraumatic Stress Disorder Symptoms Among Young Athletes After Anterior Cruciate Ligament Rupture. Orthop. J. Sports Med. 2018, 6, 2325967118787159. [Google Scholar] [CrossRef]
- Bateman, A.; Morgan, K.A.D. The Postinjury Psychological Sequelae of High-Level Jamaican Athletes: Exploration of a Posttraumatic Stress Disorder-Self-Efficacy Conceptualization. J. Sport Rehabil. 2019, 28, 144–152. [Google Scholar] [CrossRef] [PubMed]
- Aron, C.M.; Harvey, S.; Hainline, B.; Hitchcock, M.E.; Reardon, C.L. Post-traumatic stress disorder (PTSD) and other trauma-related mental disorders in elite athletes: A narrative review. Br. J. Sports Med. 2019, 53, 779–784. [Google Scholar] [CrossRef] [PubMed]
- VandenBos, G.R. Fear in APA Dictionary of Psychology, 2nd ed.; American Psychological Association: Washington, DC, USA, 2015. [Google Scholar]
- Ardern, C.L.; Osterberg, A.; Tagesson, S.; Gauffin, H.; Webster, K.E.; Kvist, J. The impact of psychological readiness to return to sport and recreational activities after anterior cruciate ligament reconstruction. Br. J. Sports Med. 2014, 48, 1613–1619. [Google Scholar] [CrossRef] [PubMed]
- Ardern, C.L.; Taylor, N.; Feller, J.; Webster, K. A systematic review of the psychological factors associated with returning to sport following injury. Br. J. Sports Med. 2012, 47, 1120–1126. [Google Scholar] [CrossRef]
- Ardern, C.L.; Webster, K.E.; Taylor, N.F.; Feller, J.A. Return to sport following anterior cruciate ligament reconstruction surgery: A systematic review and meta-analysis of the state of play. Br. J. Sports Med. 2011, 45, 596–606. [Google Scholar] [CrossRef]
- Kvist, J.; Ek, A.; Sporrstedt, K.; Good, L. Fear of re-injury: A hindrance for returning to sports after anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2005, 13, 393–397. [Google Scholar] [CrossRef]
- Lissek, S.; Powers, A.S.; McClure, E.B.; Phelps, E.A.; Woldehawariat, G.; Grillon, C.; Pine, D.S. Classical fear conditioning in the anxiety disorders: A meta-analysis. Behav. Res. Ther. 2005, 43, 1391–1424. [Google Scholar] [CrossRef]
- de Munter, L.; Polinder, S.; Haagsma, J.A.; Kruithof, N.; van de Ree, C.L.P.; Steyerberg, E.W.; de Jongh, M.A. Prevalence and Prognostic Factors for Psychological Distress After Trauma. Arch. Phys. Med. Rehabil. 2020, 101, 877. [Google Scholar] [CrossRef]
- McCarty, R. Chapter 4-The Fight-or-Flight Response: A Cornerstone of Stress Research. In Stress: Concepts, Cognition, Emotion, and Behavior; Fink, G., Ed.; Academic Press: San Diego, CA, USA, 2016; pp. 33–37. [Google Scholar]
- Campbell, P.; Bishop, A.; Dunn, K.; Main, J.C.; Thomas, E.; Foster, E.N. Conceptual overlap of psychological constructs in low back pain. Pain 2013, 154, 1783–1791. [Google Scholar] [CrossRef]
- LeDoux, J.E. Coming to terms with fear. Proc. Natl. Acad. Sci. USA 2014, 111, 2871–2878. [Google Scholar] [CrossRef]
- Bunzli, S.; Smith, A.; Schütze, R.; Lin, I.; O’Sullivan, P. Making Sense of Low Back Pain and Pain-Related Fear. J. Orthop. Sports Phys. Ther. 2017, 47, 628–636. [Google Scholar] [CrossRef] [PubMed]
- Crombez, G.; Eccleston, C.; Van Damme, S.; Vlaeyen, J.W.; Karoly, P. Fear-avoidance model of chronic pain: The next generation. Clin. J. Pain 2012, 28, 475–483. [Google Scholar] [CrossRef] [PubMed]
- Meulders, A. Fear in the context of pain: Lessons learned from 100 years of fear conditioning research. Behav. Res. Ther. 2020, 131, 103635. [Google Scholar] [CrossRef] [PubMed]
- Caneiro, J.P.; O’Sullivan, P.; Lipp, O.V.; Mitchinson, L.; Oeveraas, N.; Bhalvani, P.; Abrugiato, R.; Thorkildsen, S.; Smith, A. Evaluation of implicit associations between back posture and safety of bending and lifting in people without pain. Scand. J. Pain 2018, 18, 719–728. [Google Scholar] [CrossRef]
- Ellingsen, D.M.; Napadow, V.; Protsenko, E.; Mawla, I.; Kowalski, M.H.; Swensen, D.; O’Dwyer-Swensen, D.; Edwards, R.R.; Kettner, N.; Loggia, M.L. Brain Mechanisms of Anticipated Painful Movements and Their Modulation by Manual Therapy in Chronic Low Back Pain. J. Pain 2018, 19, 1352–1365. [Google Scholar] [CrossRef]
- Meier, M.L.; Stämpfli, P.; Vrana, A.; Humphreys, B.K.; Seifritz, E.; Hotz-Boendermaker, S. Fear avoidance beliefs in back pain-free subjects are reflected by amygdala-cingulate responses. Front. Hum. Neurosci. 2015, 9, 424. [Google Scholar] [CrossRef]
- Meier, M.L.; Stämpfli, P.; Vrana, A.; Humphreys, B.K.; Seifritz, E.; Hotz-Boendermaker, S. Neural Correlates of Fear of Movement in Patients with Chronic Low Back Pain vs. Pain-Free Individuals. Front. Hum. Neurosci. 2016, 10, 386. [Google Scholar] [CrossRef]
- Meierbachtol, A.; Obermeier, M.; Yungtum, W.; Bottoms, J.; Paur, E.; Nelson, B.J.; Tompkins, M.; Russell, H.C.; Chmielewski, T.L. Injury-Related Fears During the Return-to-Sport Phase of ACL Reconstruction Rehabilitation. Orthop. J. Sports Med. 2020, 8, 2325967120909385. [Google Scholar] [CrossRef]
- Farmer, T.; Robinson, K.; Elliott, S.J.; Eyles, J. Developing and Implementing a Triangulation Protocol for Qualitative Health Research. Qual. Health Res. 2006, 16, 377–394. [Google Scholar] [CrossRef]
- O’Cathain, A.; Murphy, E.; Nicholl, J. Three techniques for integrating data in mixed methods studies. BMJ 2010, 341, 4587. [Google Scholar] [CrossRef]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Fetters, M.D.; Curry, L.A.; Creswell, J.W. Achieving integration in mixed methods designs-principles and practices. Health Serv. Res. 2013, 48, 2134–2156. [Google Scholar] [CrossRef]
- Miller, C.L.; Mott, K.; Cousins, M.; Miller, S.; Johnson, A.; Lawson, T.; Wesselingh, S. Integrating consumer engagement in health and medical research–an Australian framework. Health Res. Policy Syst. 2017, 15, 9. [Google Scholar] [CrossRef] [PubMed]
- Burgi, C.R.; Peters, S.; Ardern, C.L.; Magill, J.R.; Gomez, C.D.; Sylvain, J.; Reiman, M.P. Which criteria are used to clear patients to return to sport after primary ACL reconstruction? A scoping review. Br. J. Sports Med. 2019, 53, 1154–1161. [Google Scholar] [CrossRef]
- Chalmers, P.N.; Mall, N.A.; Moric, M.; Sherman, S.L.; Paletta, G.P.; Cole, B.J. Does ACL reconstruction alter natural history? A systematic literature review of long-term outcomes. J. Bone Joint Surg. Am. 2014, 96, 292–300. [Google Scholar] [CrossRef] [PubMed]
- Delincé, P.; Ghafil, D. Anterior cruciate ligament tears: Conservative or surgical treatment? A critical review of the literature. Knee Surg. Sports Traumatol. Arthrosc. 2012, 20, 48–61. [Google Scholar] [CrossRef]
- Filbay, S.R.; Culvenor, A.G.; Ackerman, I.N.; Russell, T.G. Quality of life in anterior cruciate ligament-deficient individuals: A systematic review and meta-analysis. Br. J. Sports Med. 2015, 49, 1033–1041. [Google Scholar] [CrossRef]
- Harris, K.P.; Driban, J.B.; Sitler, M.R.; Cattano, N.M.; Balasubramanian, E.; Hootman, J.M. Tibiofemoral osteoarthritis after surgical or nonsurgical treatment of anterior cruciate ligament rupture: A systematic review. J. Athl. Train. 2015, 52, 507–517. [Google Scholar] [CrossRef]
- Smith, T.O.; Postle, K.; Penny, F.; McNamara, I.; Mann, C.J.V. Is reconstruction the best management strategy for anterior cruciate ligament rupture? A systematic review and meta-analysis comparing anterior cruciate ligament reconstruction versus non-operative treatment. Knee 2014, 21, 462–470. [Google Scholar] [CrossRef]
- Muaidi, Q.I.; Nicholson, L.L.; Refshauge, K.M.; Herbert, R.D.; Maher, C.G. Prognosis of conservatively managed anterior cruciate ligament injury: A systematic review. Sports Med. 2007, 37, 703–716. [Google Scholar] [CrossRef] [PubMed]
- Kovalak, E.; Atay, T.; Çetin, C.; Atay, İ.M.; Serbest, M.O. Is ACL reconstruction a prerequisite for the patients having recreational sporting activities? Acta Orthop. Traumatol. Turc. 2018, 52, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Morse, J.M.; Field, P.A. Qualitative Research Methods for Health Professional; SAGE Publications: Los Angeles, CA, USA, 1995. [Google Scholar]
- O’Reilly, M.; Parker, N. ‘Unsatisfactory Saturation’: A critical exploration of the notion of saturated sample sizes in qualitative research. Qual. Res. 2012, 13, 190–197. [Google Scholar] [CrossRef]
- Bowen, G.A. Naturalistic inquiry and the saturation concept: A research note. Qual Res. 2008, 8, 137–152. [Google Scholar] [CrossRef]
- Webster, K.E.; Feller, J.A.; Lambros, C. Development and preliminary validation of a scale to measure the psychological impact of returning to sport following anterior cruciate ligament reconstruction surgery. Phys. Ther. Sport 2008, 9, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Scherpenzeel, A. Why Use 11-Point Scales Research Gate. 2002. Available online: https://www.researchgate.net/publication/241262409_Why_Use_11-Point_Scales (accessed on 17 June 2022).
- Kemper, E.A.; Stringfield, S.; Teddlie, C. Mixed Methods Sampling Strategies in Social Science Research. In Handbook of Mixed Methods in Social and Behavioural Research; Tashakkori, A., Teddlie, C., Eds.; Sage Publications: Los Angeles, CA, USA, 2003; pp. 267–273. [Google Scholar]
- Palinkas, L.A.; Horwitz, S.M.; Green, C.A.; Wisdom, J.P.; Duan, N.; Hoagwood, K. Purposeful Sampling for Qualitative Data Collection and Analysis in Mixed Method Implementation Research. Adm. Policy Ment. Health 2015, 42, 533–544. [Google Scholar] [CrossRef] [PubMed]
- Thorne, S.; Reimer, K.S.; MacDonald-Emes, J. Interpretive description: A noncategorical qualitative alternative for developing nursing knowledge. Res. Nurs. Health 1997, 20, 169–177. [Google Scholar] [CrossRef]
- Thompson Burdine, J.; Thorne, S.; Sandhu, G. Interpretive description: A flexible qualitative methodology for medical education research. Med. Educ. 2021, 55, 336–343. [Google Scholar] [CrossRef]
- StataCorp. Stata Statistical Software; Release 17. 4905 Lakeway Drive; StataCorp LLC: College Station, TX, USA, 2021. [Google Scholar]
- Shapiro, S.S.; Wilk, M.B. An Analysis of Variance Test for Normality (Complete Samples). Biometrika 1965, 52, 591–611. [Google Scholar] [CrossRef]
- Burland, J.; Toonstra, J.; Werner, L.; Mattacola, G.C.; Howell, M.D.; Howard, S.J. Decision to Return to Sport After Anterior Cruciate Ligament Reconstruction, Part I: A Qualitative Investigation of Psychosocial Factors. J. Athl. Train. 2018, 53, 452–463. [Google Scholar] [CrossRef]
- Ross, A.C.; Clifford, A.; Louw, A.Q. Factors informing fear of reinjury after anterior cruciate ligament reconstruction. Physiother. Theory Pract. 2017, 33, 103–114. [Google Scholar] [CrossRef]
- Scott, M.S.; Perry, A.M.; Sole, G. “Not always a straight path”: Patients’ perspectives following anterior cruciate ligament rupture and reconstruction. Disabil. Rehabil. 2018, 40, 2311–2317. [Google Scholar] [CrossRef] [PubMed]
- Tjong, V.K.; Murnaghan, M.L.; Nyhof-Young, J.M.; Ogilvie-Harris, D.J. A qualitative investigation of the decision to return to sport after anterior cruciate ligament reconstruction: To play or not to play. American J. Sports Med. 2014, 42, 336–342. [Google Scholar] [CrossRef]
- DiSanti, J.; Lisee, C.; Erickson, K.; Bell, D.; Shingles, M.; Kuenze, C. Perceptions of Rehabilitation and Return to Sport Among High School Athletes with Anterior Cruciate Ligament Reconstruction: A Qualitative Research Study. J. Orthop. Sports Phys. Ther. 2018, 48, 951–959. [Google Scholar] [CrossRef] [PubMed]
- Ireland, M.L. The female ACL: Why is it more prone to injury? J. Orthop. 2016, 13, A1–A4. [Google Scholar]
- Noyes, F.R.; Barber-Westin, S. Return to Sport after ACL Reconstruction and Other Knee Operations: Limiting the Risk of Reinjury and Maximizing Athletic Performance; Springer: Cham, Switzerland, 2019. [Google Scholar]
- Filbay, S.R.; Crossley, K.M.; Ackerman, I.N. Activity preferences, lifestyle modifications and re-injury fears influence longer-term quality of life in people with knee symptoms following anterior cruciate ligament reconstruction: A qualitative study. J. Physiother. 2016, 62, 103–110. [Google Scholar] [CrossRef]
- Vutescu, E.S.; Orman, S.; Garcia-Lopez, E.; Lau, J.; Gage, A.; Cruz, A.I., Jr. Psychological and Social Components of Recovery Following Anterior Cruciate Ligament Reconstruction in Young Athletes: A Narrative Review. Int. J. Environ. Res. Public Health 2021, 18, 9267. [Google Scholar] [CrossRef]
- Sonesson, S.; Kvist, J.; Ardern, C.; Osterberg, A.; Silbernagel, K.G. Psychological factors are important to return to pre-injury sport activity after anterior cruciate ligament reconstruction: Expect and motivate to satisfy. Knee Surg. Sports Traumato. Arthrosc. 2017, 25, 1375–1384. [Google Scholar] [CrossRef]
- Truong, L.K.; Mosewich, A.D.; Holt, C.J.; Le, C.Y.; Miciak, M.; Whittaker, J.L. Psychological, social and contextual factors across recovery stages following a sport-related knee injury: A review. Br. J. Sports Med. 2020, 54, 1149–1156. [Google Scholar] [CrossRef]
- Mahood, C.; Perry, M.; Gallagher, P.; Sole, G. Chaos and confusion with confidence: Managing fear of Re-Injury after anterior cruciate ligament reconstruction. Phys. Ther. Sport. 2020, 45, 145–154. [Google Scholar] [CrossRef]
- de Oliveira, B.I.R.; Smith, A.J.; O’Sullivan, P.P.B.; Haebich, S.; Fick, D.; Khan, R.; Bunzli, S. ‘My hip is damaged’: A qualitative investigation of people seeking care for persistent hip pain. Br. J. Sports Med. 2020, 54, 858–865. [Google Scholar] [CrossRef]
- Darlow, B.; Dowell, A.; Baxter, G.D.; Mathieson, F.; Perry, M.; Dean, S. The enduring impact of what clinicians say to people with low back pain. Ann. Fam. Med. 2013, 11, 527–534. [Google Scholar] [CrossRef] [PubMed]
- Ohji, S.; Aizawa, J.; Hirohata, K.; Mitomo, S.; Ohmi, T.; Jinno, T.; Koga, H.; Yagishita, K. Athletic identity and sport commitment in athletes after anterior cruciate ligament reconstruction who have returned to sports at their pre-injury level of competition. BMC Sports Sci. Med. Rehabil. 2021, 13, 37. [Google Scholar] [CrossRef]
- Roelofs, K. Freeze for action: Neurobiological mechanisms in animal and human freezing. Philos. Trans. R Soc. Lond. B Biol. Sci. 2017, 372, 20160206. [Google Scholar] [CrossRef] [PubMed]
- Hoehn-Saric, R.; McLeod, D.R. The Peripheral Sympathetic Nervous System: Its Role in Normal and Pathologic Anxiety. Psychiatr. Clin. N. Am. 1988, 11, 375–386. [Google Scholar] [CrossRef]
- El-Badawy, M.A.; El Mikkawy, D.M. Sympathetic Dysfunction in Patients with Chronic Low Back Pain and Failed Back Surgery Syndrome. Clin. J. Pain 2016, 32, 226–231. [Google Scholar] [CrossRef] [PubMed]
- Oktem, E.O.; Cankaya, S. Empathy for Pain, Pain Management-Practices, Novel Therapies and Bioactives; IntechOpen: London, UK, 2021. [Google Scholar]
- Neto, T.; Sayer, T.; Theisen, D.; Mierau, A. Functional Brain Plasticity Associated with ACL Injury: A Scoping Review of Current Evidence. Neural Plast. 2019, 2019, 3480512. [Google Scholar] [CrossRef] [PubMed]
- Fanselow, M.S.; Sigmundi, R.A. Species-specific danger signals, endogenous opioid analgesia, and defensive behavior. J. Exp. Psychol. Anim. Behav. Process. 1986, 12, 301–309. [Google Scholar] [CrossRef]
- Lethem, J.; Slade, P.D.; Troup, J.D.; Bentley, G. Outline of a Fear-Avoidance Model of exaggerated pain perception--I. Behav. Res. Ther. 1983, 21, 401–408. [Google Scholar] [CrossRef]
- Moseley, L.; Butler, S.; Beames, B.T.; Giles, J.T. The Graded Motor Imagery Handbook, 1st ed.; Noigroup Publications: Adelaide, Australia, 2012. [Google Scholar]
- Pincus, T.; Henderson, J. Low back pain patients’ responses to videos of avoided movements. Eur. J. Pain 2013, 17, 271–278. [Google Scholar] [CrossRef]
- Lovalekar, M.; Abt, J.P.; Sell, T.C.; Lephart, S.M.; Pletcher, E.; Beals, K. Accuracy of recall of musculoskeletal injuries in elite military personnel: A cross-sectional study. BMJ Open 2017, 7, e017434. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).