Acute, Non-Specific Low Back Pain Does Not Impair Isometric Deadlift Force or Electromyographic Excitation: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Research Design
2.2. Participants
2.3. Subjective Assessment of LBP and Physical Disability
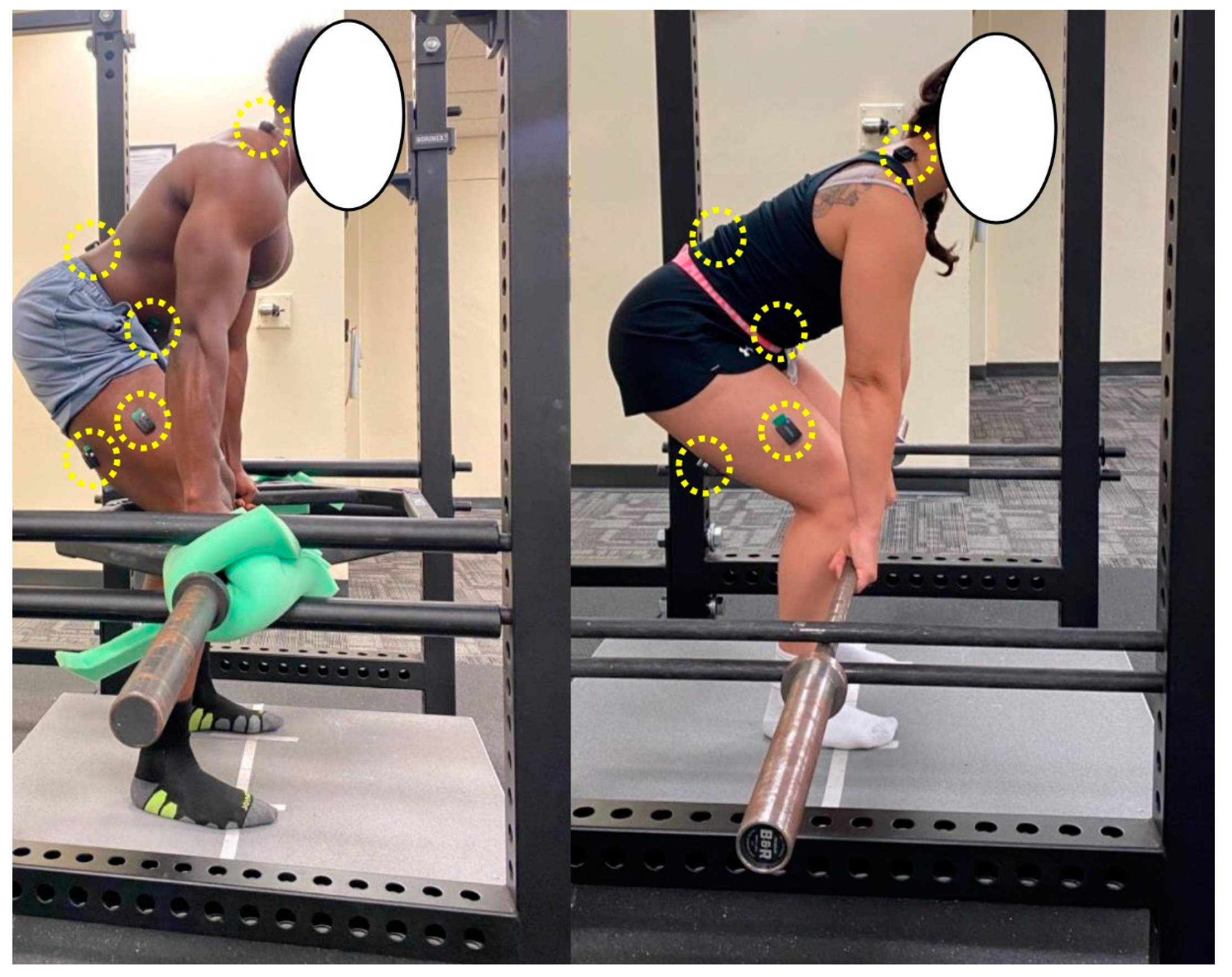
2.4. Maximal Isometric Deadlifts
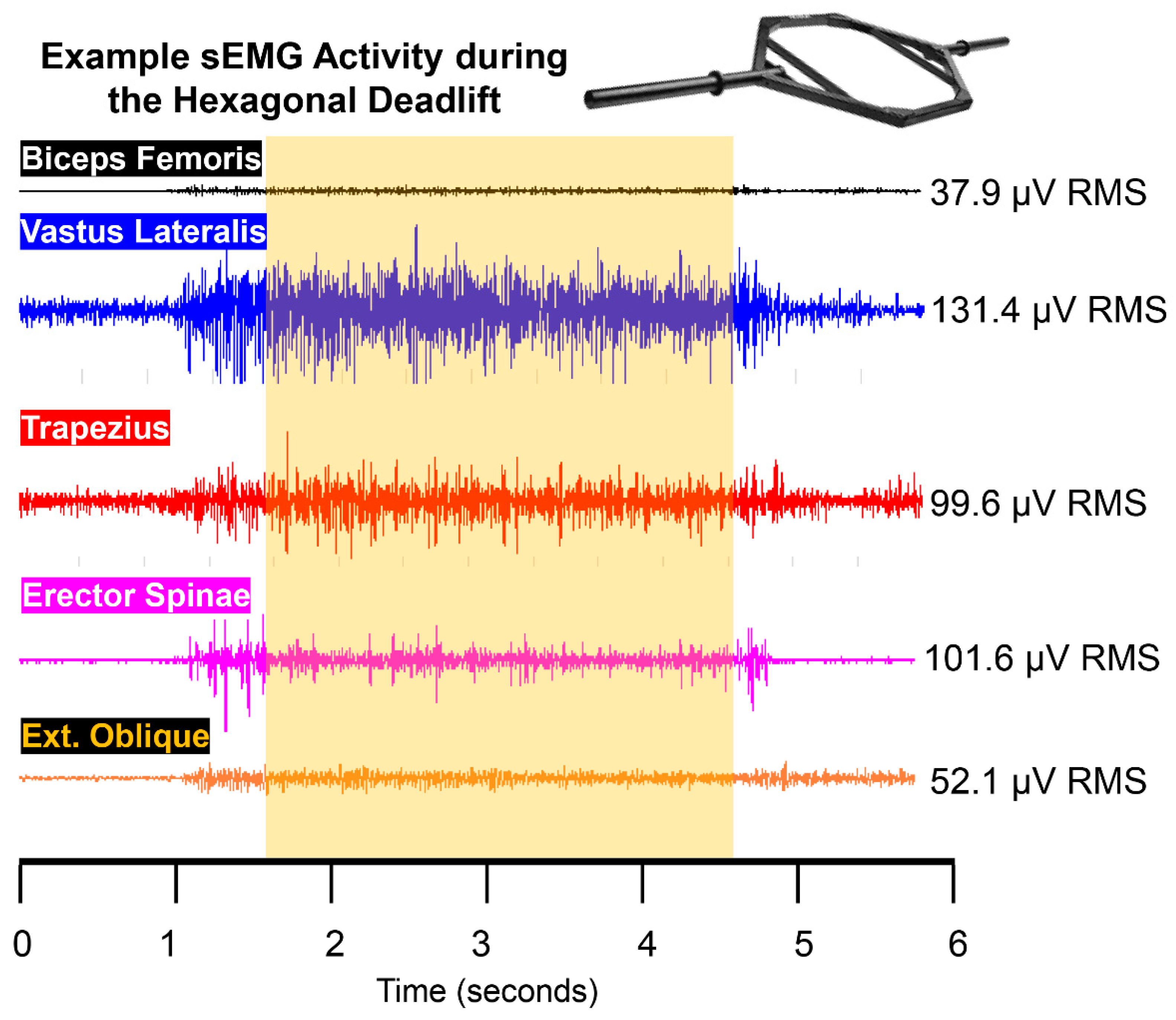
2.5. sEMG
2.6. Perceived Confidence, Safety, and Force
2.7. Statistical Analyses
3. Results
3.1. Description of Study Sample: NPRS, RMDQ, and FABQ
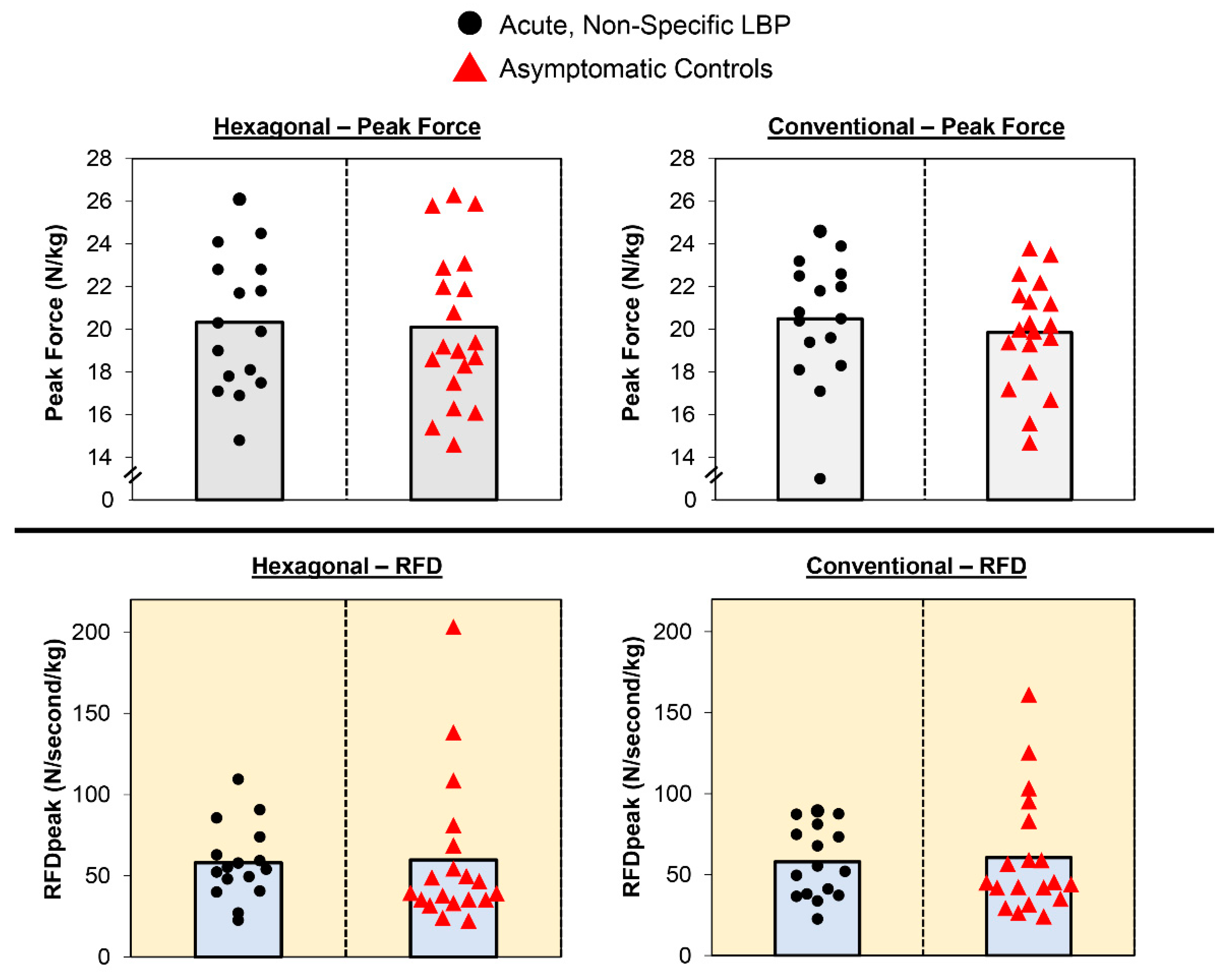
3.2. Normalized Peak Force and RFDpeak
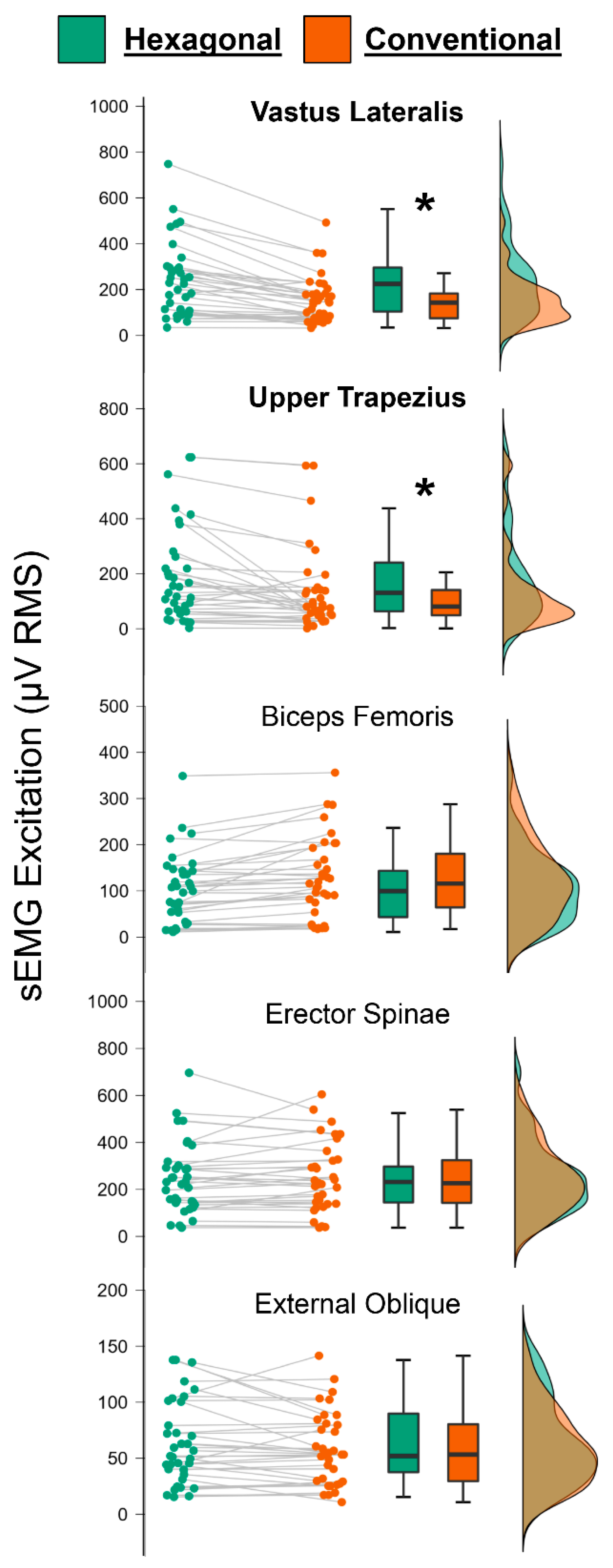
3.3. EMG Excitation
3.4. Perceived Confidence, Safety, and Force
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Traeger, A.C.; Buchbinder, R.; Elshaug, A.G.; Croft, P.R.; Maher, C.G. Care for low back pain: Can health systems deliver? Bull. World Health Organ. 2019, 97, 423–433. [Google Scholar] [CrossRef] [PubMed]
- Chou, R. Low back pain (chronic). BMJ Clin. Evid. 2010, 2010, 1116. [Google Scholar] [PubMed]
- National Institute of Neurological Disorders and Stroke. Low Back Pain Fact Sheet. Available online: https://www.ninds.nih.gov/low-back-pain-fact-sheet (accessed on 12 August 2022).
- Calvo-Lobo, C.; Vilar Fernández, J.M.; Becerro-de-Bengoa-Vallejo, R.; Losa-Iglesias, M.E.; Rodríguez-Sanz, D.; Palomo López, P.; López López, D. Relationship of depression in participants with nonspecific acute or subacute low back pain and no-pain by age distribution. J. Pain Res. 2017, 10, 129–135. [Google Scholar] [CrossRef]
- Lopez-Lopez, D.; Vilar-Fernandez, J.M.; Calvo-Lobo, C.; Losa-Iglesias, M.E.; Rodriguez-Sanz, D.; Becerro-de-Bengoa-Vallejo, R. Evaluation of depression in subacute low back pain: A case control study. Pain Physician 2017, 20, E499–E505. [Google Scholar] [CrossRef] [PubMed]
- Darzi, M.T.; Pourhadi, S.; Hosseinzadeh, S.; Ahmadi, M.H.; Dadian, M. Comparison of quality of life in low back pain patients and healthy subjects by using WHOQOL-BREF. J. Back Musculoskelet. Rehabil. 2014, 27, 507–512. [Google Scholar] [CrossRef]
- Pourahmadi, M.; Koes, B.W.; Nazemipour, M.; Mansournia, M.A. It is time to change our mindset and perform more high-quality research in low back pain. Spine 2021, 46, 69–71. [Google Scholar] [CrossRef] [PubMed]
- Holmberg, D.; Crantz, H.; Michaelson, P. Treating persistent low back pain with deadlift training—A single subject experimental design with a 15-month follow-up. Eur. J. Physiother. 2012, 14, 61–70. [Google Scholar] [CrossRef]
- Tataryn, N.; Simas, V.; Catterall, T.; Furness, J.; Keogh, J.W.L. Posterior-chain resistance training compared to general exercise and walking programmes for the treatment of chronic low back pain in the general population: A systematic review and meta-analysis. Sports Med. Open 2021, 7, 17. [Google Scholar] [CrossRef]
- Stock, M.S.; Olinghouse, K.D.; Drusch, A.S.; Mota, J.A.; Hernandez, J.M.; Akalonu, C.C.; Thompson, B.J. Evidence of muscular adaptations within four weeks of barbell training in women. Hum. Mov. Sci. 2016, 45, 7–22. [Google Scholar] [CrossRef]
- Thompson, B.J.; Stock, M.S.; Shields, J.E.; Luera, M.J.; Munayer, I.K.; Mota, J.A.; Carrillo, E.C.; Olinghouse, K.D. Barbell deadlift training increases the rate of torque development and vertical jump performance in novices. J. Strength Cond. Res. 2015, 29, 1–10. [Google Scholar] [CrossRef]
- Camara, K.D.; Coburn, J.W.; Dunnick, D.D.; Brown, L.E.; Galpin, A.J.; Costa, P.B. An examination of muscle activation and power characteristics while performing the deadlift exercise with straight and hexagonal barbells. J. Strength Cond. Res. 2016, 30, 1183–1188. [Google Scholar] [CrossRef]
- Swinton, P.A.; Stewart, A.; Agouris, I.; Keogh, J.W.L.; Lloyd, R. A Biomechanical analysis of straight and hexagonal barbell deadlifts using submaximal loads. J. Strength Cond. Res. 2011, 25, 2000–2009. [Google Scholar] [CrossRef]
- Fischer, S.C.; Calley, D.Q.; Hollman, J.H. Effect of an exercise program that includes deadlifts on low back pain. J. Sport Rehabil. 2021, 30, 672–675. [Google Scholar] [CrossRef]
- Andersen, V.; Fimland, M.S.; Mo, D.-A.; Iversen, V.M.; Vederhus, T.; Rockland Hellebø, L.R.; Nordaune, K.I.; Saeterbakken, A.H. Electromyographic comparison of barbell deadlift, hex bar deadlift, and hip thrust exercises: A cross-over study. J. Strength Cond. Res. 2018, 32, 587–593. [Google Scholar] [CrossRef]
- Waddell, G.; Newton, M.; Henderson, I.; Somerville, D.; Main, C.J. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain 1993, 52, 157–168. [Google Scholar] [CrossRef]
- Roland, M.; Morris, R. A study of the natural history of back pain. Part I: Development of a reliable and sensitive measure of disability in low-back pain. Spine 1983, 8, 141–144. [Google Scholar] [CrossRef]
- Childs, J.D.; Piva, S.R.; Fritz, J.M. Responsiveness of the Numeric Pain Rating Scale in patients with low back pain. Spine 2005, 30, 1331–1334. [Google Scholar] [CrossRef]
- Thompson, B.J. Influence of signal filtering and sample rate on isometric torque—Time parameters using a traditional Isokinetic Dynamometer. J. Biomech. 2019, 83, 235–242. [Google Scholar] [CrossRef]
- Hermens, H.J.; Freriks, B.; Disselhorst-Klug, C.; Rau, G. Development of recommendations for SEMG sensors and sensor placement procedures. J. Electromyogr. Kinesiol. Off. J. Int. Soc. Electrophysiol. Kinesiol. 2000, 10, 361–374. [Google Scholar] [CrossRef]
- JASP Team. JASP, version 0.16.3; University of Amsterdam: Amsterdam, The Netherlands, 2022. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; L. Erlbaum Associates: Hillsdale, NJ, USA, 1988; ISBN 978-0-8058-0283-2. [Google Scholar]
- Weissgerber, T.L.; Milic, N.M.; Winham, S.J.; Garovic, V.D. Beyond bar and line graphs: Time for a new data presentation paradigm. PLoS Biol. 2015, 13, e1002128. [Google Scholar] [CrossRef]
- Snyder, B.J.; Cauthen, C.P.; Senger, S.R. Comparison of muscle involvement and posture between the conventional deadlift and a “walk-in” style deadlift machine. J. Strength Cond. Res. 2017, 31, 2859–2865. [Google Scholar] [CrossRef]
- Martín-Fuentes, I.; Oliva-Lozano, J.M.; Muyor, J.M. Electromyographic activity in deadlift exercise and its variants. A systematic review. PLoS ONE 2020, 15, e0229507. [Google Scholar] [CrossRef]
| Acute, Non−Specific LBP | Asymptomatic Controls | ||||
| Mean ± SD (Range) | Mean Difference (95% CI) | p | d | ||
| Age (years) | 22 ± 3 (18–30) | 24 ± 4 (18–34) | −1.9 (−4.5–0.7) | 0.153 | 0.497 |
| Height (cm) | 172.1 ± 9.7 (152.7–186.2) | 171.2 ± 10.5 (148.5–188.0) | 0.78 (−6.20–7.73) | 0.823 | 0.077 |
| Mass (kg) | 76.4 ± 17.4 (53.2–127.5) | 70.6 ± 14.0 (51.2–96.5) | 5.81 (−4.99–16.60) | 0.309 | 0.371 |
| BMI (kg/m2) | 25.7 ± 4.3 (18.9–36.8) | 24.0 ± 3.2 (17.7–30.0) | 1.721 (−0.87–4.31) | 0.185 | 0.459 |
| Mean ± SD | Hodges−Lehmann Estimate (95% CI) | p | Rank biserial correlation | ||
| NPRS Current | 2.00 ± 0.97 (1–5) | 0 ± 0 | N/A | N/A | N/A |
| NPRS Best | 0.56 ± 0.96 (0–3) | 0 ± 0 | N/A | N/A | N/A |
| NPRS Worst | 3.44 ± 1.99 (1–9) | 0.53 ± 1.02 (0–3) | 3.0 (2.0–3.0) | <0.001 | 0.865 |
| RMDQ | 1.88 ± 2.09 (0–7) | 0.16 ± 0.37 (0–1) | 1.0 (0.0–2.0) | 0.002 | 0.546 |
| FABQ Physical Activity | 7.44 ± 3.72 (1–13) | 0.79 ± 1.81 (0–6) | 6.8 (4.0–9.0) | <0.001 | 0.914 |
| FABQ Work | 4.38 ± 5.45 (0–14) | 1.16 ± 3.45 (0–16) | 0.0 (0.0–8.0) | 0.017 | 0.381 |
| Acute, Non-Specific LBP | Asymptomatic Controls | p | Rank Biserial Correlation | |
|---|---|---|---|---|
| “Did you feel safe pulling with the hexagonal barbell?” | 9.5 ± 1.1 (5–10) | 9.7 ± 0.5 (9–10) | 0.914 | 0.020 |
| “Did you feel safe pulling with the conventional barbell?” | 9.1 ± 1.6 (4–10) | 9.6 ± 0.8 (7–10) | 0.443 | 0.128 |
| “Did you feel confident pulling with the hexagonal barbell?” | 8.3 ± 1.5 (5–10) | 8.7 ± 1.4 (5–10) | 0.428 | 0.155 |
| “Did you feel confident pulling with the conventional barbell?” | 8.3 ± 1.7 (6–10) | 9.2 ± 1.0 (6–10) | 0.120 | 0.296 |
| “Which barbell do you believe you pulled with more force?” 0 = hexagonal, 1 = conventional | 0.63 ± 0.50 | 0.53 ± 0.51 | 0.576 | 0.099 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stock, M.S.; Bodden, M.E.; Bloch, J.M.; Starnes, K.L.; Rodriguez, G.; Girts, R.M. Acute, Non-Specific Low Back Pain Does Not Impair Isometric Deadlift Force or Electromyographic Excitation: A Cross-Sectional Study. Sports 2022, 10, 168. https://doi.org/10.3390/sports10110168
Stock MS, Bodden ME, Bloch JM, Starnes KL, Rodriguez G, Girts RM. Acute, Non-Specific Low Back Pain Does Not Impair Isometric Deadlift Force or Electromyographic Excitation: A Cross-Sectional Study. Sports. 2022; 10(11):168. https://doi.org/10.3390/sports10110168
Chicago/Turabian StyleStock, Matt S., Megan E. Bodden, Jenna M. Bloch, Karen L. Starnes, Gabriela Rodriguez, and Ryan M. Girts. 2022. "Acute, Non-Specific Low Back Pain Does Not Impair Isometric Deadlift Force or Electromyographic Excitation: A Cross-Sectional Study" Sports 10, no. 11: 168. https://doi.org/10.3390/sports10110168
APA StyleStock, M. S., Bodden, M. E., Bloch, J. M., Starnes, K. L., Rodriguez, G., & Girts, R. M. (2022). Acute, Non-Specific Low Back Pain Does Not Impair Isometric Deadlift Force or Electromyographic Excitation: A Cross-Sectional Study. Sports, 10(11), 168. https://doi.org/10.3390/sports10110168









