The Eco-Bio-Social Factors That Modulate Aedes aegypti Abundance in South Texas Border Communities
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
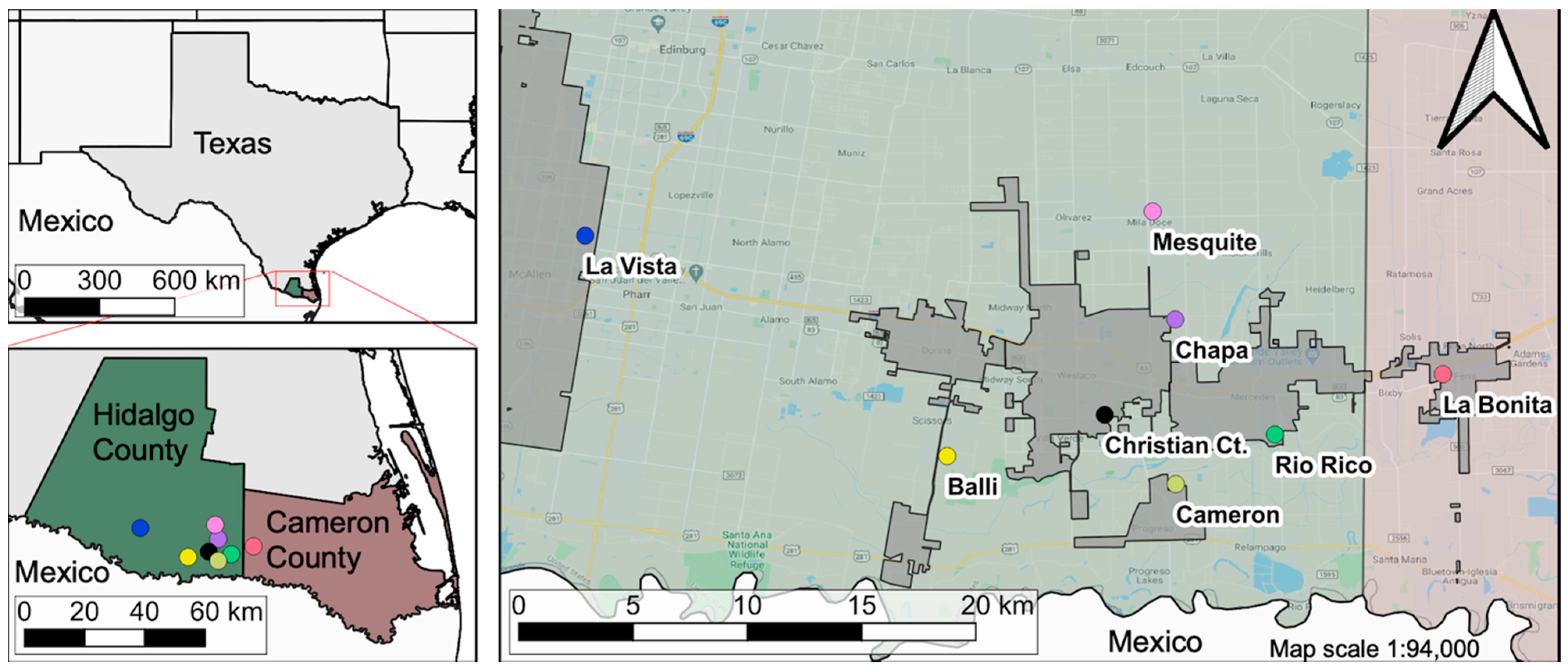
2.1. Study Area
2.2. Community Selection and Sample Size
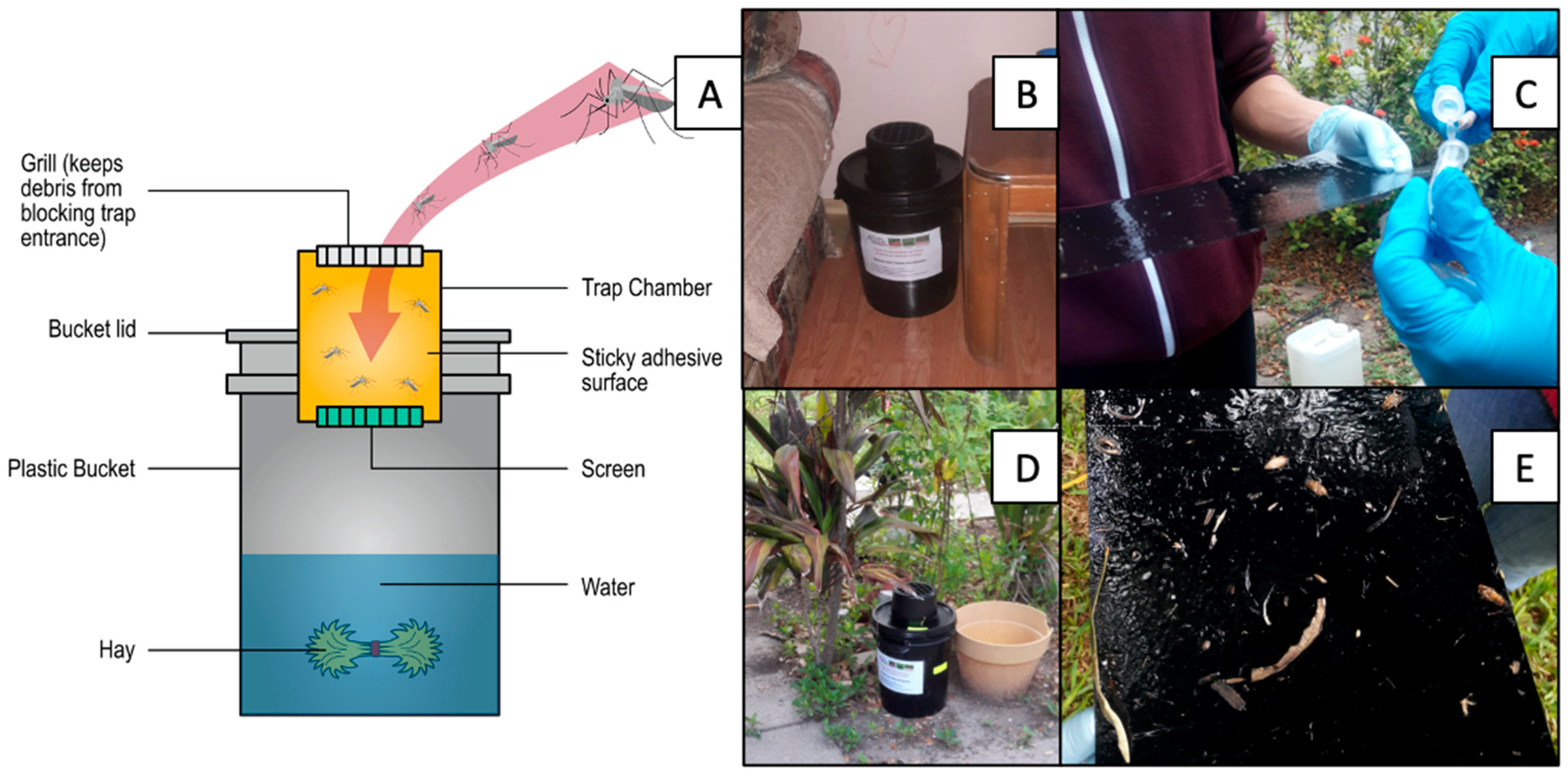
2.3. Entomological Surveillance
2.4. KAP and House Quality Surveys
2.5. Statistical Analysis
3. Results
3.1. KAP: Aedes aegypti and Zika
3.2. KAP: Prevention, Control, and Demographics
3.3. Housing Materials: Yard, Windows, and Doors
3.4. Factors Associated with Indoor and Outdoor Relative Ae. aegypti Abundance
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Global Vector Control Response 2017–2030; WHO: Geneva, Switzerland, 2017. [Google Scholar]
- Lounibos, L.P.; Kramer, L.D. Invasiveness of Aedes aegypti and Aedes albopictus and vectorial capacity for chikungunya virus. J. Infect. Dis. 2016, 214, S453–S458. [Google Scholar] [CrossRef]
- WHO. A Global Brief on Vector-Borne Diseases. Available online: www.who.int/about/licensing/copyright_form/en/ (accessed on 9 January 2020).
- PAHO. Epidemiological Alerts and Reports. Available online: https://www.paho.org/hq/index.php?option=com_topics&view=rdmore&cid=2217&item=dengue&type=alerts&Itemid=40734&lang=en (accessed on 7 January 2020).
- Fischer, M.; Erin Staples, J. Chikungunya virus spreads in the Americas—Caribbean and South America, 2013–2014. Morb. Mortal. Wkly. Rep. 2014, 63, 500–501. [Google Scholar]
- Yakob, L.; Walker, T. Zika virus outbreak in the Americas: The need for novel mosquito control methods. Lancet Glob. Health 2016, 4, e148–e149. [Google Scholar] [CrossRef]
- Fauci, A.S.; Morens, D.M. Zika Virus in the Americas—Yet Another Arbovirus Threat. N. Engl. J. Med. 2016, 374, 601–604. [Google Scholar] [CrossRef]
- Nagao, Y.; Thavara, U.; Chitnumsup, P.; Tawatsin, A.; Chansang, C.; Campbell-Lendrum, D. Climatic and social risk factors for Aedes infestation in rural Thailand. Trop. Med. Int. Health 2003, 8, 650–659. [Google Scholar] [CrossRef]
- Hiscox, A.; Banks, I.; Brey, P.T.; Hill, N.; Kaye, A.; Vongphayloth, K.; Khammanithong, P.; Lindsay, S.W.; Kaul, S.; Piffer, M.; et al. Risk Factors for the Presence of Aedes aegypti and Aedes albopictus in Domestic Water-Holding Containers in Areas Impacted by the Nam Theun 2 Hydroelectric Project, Laos. Am. J. Trop. Med. Hyg. 2013, 88, 1070–1078. [Google Scholar] [CrossRef] [PubMed]
- Vannavong, N.; Seidu, R.; Stenström, T.-A.; Dada, N.; Overgaard, H.J. Effects of socio-demographic characteristics and household water management on Aedes aegypti production in suburban and rural villages in Laos and Thailand. Parasit. Vectors 2017, 10, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Dhimal, M.; Gautam, I.; Joshi, H.D.; O’Hara, R.B.; Ahrens, B.; Kuch, U. Risk Factors for the Presence of Chikungunya and Dengue Vectors (Aedes aegypti and Aedes albopictus), Their Altitudinal Distribution and Climatic Determinants of Their Abundance in Central Nepal. PLoS Negl. Trop. Dis. 2015, 9, e0003545. [Google Scholar] [CrossRef] [PubMed]
- WHO. Global Strategy for Dengue Prevention and Control 2012–2020; WHO: Geneva, Switzerland, 2012. [Google Scholar]
- Gürtler, R.E.; Garelli, F.M.; Coto, H.D. Effects of a Five-Year Citywide Intervention Program To Control Aedes aegypti and Prevent Dengue Outbreaks in Northern Argentina. PLoS Neglected Trop. Dis. 2009, 3, e427. [Google Scholar] [CrossRef] [PubMed]
- Hahn, M.B.; Eisen, L.; McAllister, J.; Savage, H.M.; Mutebi, J.-P.; Eisen, R.J. Updated Reported Distribution of Aedes (Stegomyia) aegypti and Aedes (Stegomyia) albopictus (Diptera: Culicidae) in the United States, 1995–2016. J. Med. Entomol. 2017, 54, 1420–1424. [Google Scholar] [CrossRef]
- Monaghan, A.J.; Eisen, R.J.; Eisen, L.; McAllister, J.; Savage, H.M.; Mutebi, J.-P.; Johansson, M.A. Consensus and uncertainty in the geographic range of Aedes aegypti and Aedes albopictus in the contiguous United States: Multi-model assessment and synthesis. PLoS Comput. Biol. 2019, 15, e1007369. [Google Scholar] [CrossRef]
- CDC. ArboNET Disease Maps. Available online: https://wwwn.cdc.gov/arbonet/Maps/ADB_Diseases_Map/index.html (accessed on 9 January 2020).
- Martin, E.; Medeiros, M.C.; Carbajal, E.; Valdez, E.; Juarez, J.G.; Garcia-Luna, S.; Salazar, A.; Qualls, W.A.; Hinojosa, S.; Borucki, M.K.; et al. Surveillance of Aedes aegypti indoors and outdoors using Autocidal Gravid Ovitraps in South Texas during local transmission of Zika virus, 2016 to 2018. Acta Trop. 2019, 192, 129–137. [Google Scholar] [CrossRef] [PubMed]
- Monaghan, A.J.; Morin, C.W.; Steinhoff, D.F.; Wilhelmi, O.; Hayden, M.; Quattrochi, D.A.; Reiskind, M.; Lloyd, A.L.; Smith, K.; Schmidt, C.A.; et al. On the Seasonal Occurrence and Abundance of the Zika Virus Vector Mosquito Aedes aegypti in the Contiguous United States. PLoS Curr. Outbreaks 2016, 8, 31. [Google Scholar] [CrossRef] [PubMed]
- Butterworth, M.K.; Morin, C.W.; Comrie, A.C. An Analysis of the Potential Impact of Climate Change on Dengue Transmission in the Southeastern United States. Environ. Health Perspect. 2017, 125, 579–585. [Google Scholar] [CrossRef] [PubMed]
- Champion, S.R.; Vitek, C.J. Aedes aegypti and Aedes albopictus Habitat Preferences in South Texas, USA. Environ. Health Insights 2014, 8, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Uejio, C.K.; Hayden, M.H.; Zielinski-Gutierrez, E.; Lopez, J.L.R.; Barrera, R.; Amador, M.; Thompson, G.; Waterman, S.H. Biological Control of Mosquitoes in Scrap Tires in Brownsville, Texas, USA and Matamoros, Tamaulipas, Mexico. J. Am. Mosq. Control Assoc. 2014, 30, 130–135. [Google Scholar] [CrossRef] [PubMed]
- Adam, J.K.; Abeyta, R.; Smith, B.; Gaul, L.; Thomas, D.L.; Han, G.; Sharp, T.M.; Waterman, S.H.; Tomashek, K.M. Clinician Survey to Determine Knowledge of Dengue and Clinical Management Practices, Texas, 2014. Am. J. Trop. Med. Hyg. 2017, 96, 708–714. [Google Scholar] [CrossRef]
- Vitek, C.J.; Gutierrez, J.A.; Dirrigl, F.J. Dengue Vectors, Human Activity, and Dengue Virus Transmission Potential in the Lower Rio Grande Valley, Texas, United States. J. Med. Entomol. 2014, 51, 1019–1028. [Google Scholar] [CrossRef]
- Donnelly, M.A.P.; Kluh, S.; Snyder, R.E.; Barker, C.M. Quantifying sociodemographic heterogeneities in the distribution of Aedes aegypti among California households. PLoS Negl. Trop. Dis. 2020, 14, e0008408. [Google Scholar] [CrossRef]
- Hayden, M.H.; Uejio, C.K.; Walker, K.; Ramberg, F.; Moreno, R.; Rosales, C.; Gameros, M.; Mearns, L.O.; Zielinski-Gutierrez, E.; Janes, C.R. Microclimate and Human Factors in the Divergent Ecology of Aedes aegypti along the Arizona, U.S./Sonora, MX Border. EcoHealth 2010, 7, 64–77. [Google Scholar] [CrossRef]
- Hinojosa, S.; Alquiza, A.; Guerrero, C.; Vanegas, D.; Tapangan, N.; Cano, N.; Olivarez, E. Detection of a Locally-Acquired Zika Virus Outbreak in Hidalgo County, Texas through Increased Antenatal Testing in a High-Risk Area. Trop. Med. Infect. Dis. 2020, 5, 128. [Google Scholar] [CrossRef]
- U.S. Census Bureau Cameron County, Texas. Available online: https://www.census.gov/quickfacts/cameroncountytexas (accessed on 14 March 2019).
- U.S. Census Bureau Hidalgo County, Texas. Available online: https://www.census.gov/quickfacts/hidalgocountytexas (accessed on 14 March 2019).
- Hargrove, W.L.; Juárez-Carillo, P.M.; Korc, M. Healthy Vinton: A Health Impact Assessment Focused on Water and Sanitation in a Small Rural Town on the U.S.-Mexico Border. Int. J. Environ. Res. Public Health 2015, 12, 3864–3888. [Google Scholar] [CrossRef]
- Rivera, D.Z. The Forgotten Americans: A Visual Exploration of Lower Rio Grande Valley Colonias. Mich. J. Sustain. 2014, 2. [Google Scholar] [CrossRef][Green Version]
- HAC. Rural Research Report: Housing in the Border Colonias; HAC: Washigton, DC, USA, 2013. [Google Scholar]
- NOAA. National Weather Service: Climate Prediction Center. Available online: https://w2.weather.gov/climate/xmacis.php?wfo=bro (accessed on 29 January 2019).
- Darsie, R.; Ward, R. Identification and Geographical Distribution of the Mosquitoes of North America, North of Mexico; Walter Reed Army Inst of Research: Washington, DC, USA, 1981. [Google Scholar]
- Wilkerson, R.C.; Linton, Y.-M.; Fonseca, D.M.; Schultz, T.R.; Price, D.C.; Strickman, D.A. Making Mosquito Taxonomy Useful: A Stable Classification of Tribe Aedini that Balances Utility with Current Knowledge of Evolutionary Relationships. PLoS ONE 2015, 10, e0133602. [Google Scholar] [CrossRef]
- Acevedo, V.; Amador, M.; Félix, G.; Barrera, R. Operational Aspects of the Centers for Disease Control and Prevention Autocidal Gravid Ovitrap. J. Am. Mosq. Control Assoc. 2016, 32, 254–257. [Google Scholar] [CrossRef] [PubMed]
- WHO. Knowledge, Attitudes and Practice Surveys Zika Virus Disease and Potential Complications Resource Pack; WHO: Geneva, Switzerland, 2016. [Google Scholar]
- Ernst, K.C.; Haenchen, S.; Dickinson, K.; Doyle, M.S.; Walker, K.; Monaghan, A.J.; Hayden, M.H. Awareness and Support of Release of Genetically Modified “Sterile” Mosquitoes, Key West, Florida, USA. Emerg. Infect. Dis. 2015, 21, 320–324. [Google Scholar] [CrossRef] [PubMed]
- Juarez, J.G.; Garcia-Luna, S.; Chaves, L.F.; Carbajal, E.; Valdez, E.; Avila, C.; Tang, W.; Martin, E.; Barrera, R.; Hemme, R.R.; et al. Dispersal of female and male Aedes aegypti from discarded container habitats using a stable isotope mark-capture study design in South Texas. Sci. Rep. 2020, 10, 1–12. [Google Scholar] [CrossRef]
- Barrera, R.; Amador, M.; Acevedo, V.; Caban, B.; Felix, G.; Mackay, A.J. Use of the CDC Autocidal Gravid Ovitrap to Control and Prevent Outbreaks of Aedes aegypti (Diptera: Culicidae). J. Med. Entomol. 2014, 51, 145–154. [Google Scholar] [CrossRef] [PubMed]
- White, G.C.; Bennetts, R.E. Analysis of Frequency Count Data Using the Negative Binomial Distribution. Ecology 1996, 77, 2549–2557. [Google Scholar] [CrossRef]
- Sileshi, G. Selecting the right statistical model for analysis of insect count data by using information theoretic measures. Bull. Entomol. Res. 2006, 96, 479–488. [Google Scholar] [PubMed]
- Hardin, J.; Hilbe, J. Generalized Linear Models and Extensions; Stata Press: College Station, TX, USA, 2007. [Google Scholar]
- Hoef, J.M.V.; Boveng, P.L. Quasi-Poisson VS. Negative Binomial Regression: How Should We Model Overdispersed Count Data? Ecology 2007, 88, 2766–2772. [Google Scholar] [CrossRef]
- Lindén, A.; Mäntyniemi, S. Using the negative binomial distribution to model overdispersion in ecological count data. Ecology 2011, 92, 1414–1421. [Google Scholar] [CrossRef] [PubMed]
- SAS Institute Inc. PROC GLIMMIX: G-Side and R-Side Random Effects and Covariance Structures. Available online: https://support.sas.com/documentation/cdl/en/statug/63347/HTML/default/viewer.htm#statug_glimmix_a0000001405.htm (accessed on 15 May 2019).
- Bolker, B.M.; Brooks, M.E.; Clark, C.J.; Geange, S.W.; Poulsen, J.R.; Stevens, M.H.H.; White, J.-S.S. Generalized linear mixed models: A practical guide for ecology and evolution. Trends Ecol. Evol. 2009, 24, 127–135. [Google Scholar] [CrossRef]
- Bates, D.; Mächler, M.; Bolker, B.; Walker, S. Fitting Linear Mixed-Effects Models Usinglme4. J. Stat. Softw. 2015, 67, 1–48. [Google Scholar] [CrossRef]
- Brundson, C.; Comber, L. An Introduction to R for Spatial Analysis and Mapping; Sage Publications: London, UK, 2015. [Google Scholar]
- Kassambara, A. Practical Guide to Principal Component Methods in R; STHDA, 2017; Available online: http://www.sthda.com/english/articles/31-principal-component-methods-in-r-practical-guide/ (accessed on 20 February 2021).
- Chaves, L.F.; Calzada, J.E.; Rigg, C.; Valderrama, A.; Gottdenker, N.L.; Saldaña, A. Leishmaniasis sand fly vector density reduction is less marked in destitute housing after insecticide thermal fogging. Parasit. Vectors 2013, 6, 1–13. [Google Scholar] [CrossRef] [PubMed]
- McKenzie, D.J. Measuring inequality with asset indicators. J. Popul. Econ. 2005, 18, 229–260. [Google Scholar] [CrossRef]
- Vyas, S.; Kumaranayake, L. Constructing socio-economic status indices: How to use principal components analysis. Health Policy Plan. 2006, 21, 459–468. [Google Scholar] [CrossRef] [PubMed]
- Husson, F.; Josse, J.; Le, S.; Maintainer, J.M. Multivariate exploratory data analysis and data mining. CRAN 2020, 1, 1–130. [Google Scholar]
- Akinwande, M.O.; Dikko, H.G.; Samson, A. Variance Inflation Factor: As a Condition for the Inclusion of Suppressor Variable(s) in Regression Analysis. Open J. Stat. 2015, 5, 754–767. [Google Scholar] [CrossRef]
- Faraway, J.J. Linear Models with R; Chapman and Hall/CRC Texts in Statistical Science Series; CRC Press: Boca Raton, FL, USA, 2005; ISBN 1584881658. [Google Scholar]
- Burnham, K.P.; Anderson, D.R. Multimodel Inference: Understanding AIC and BIC in Model Selection. Sociol. Methods Res. 2004, 33, 261–304. [Google Scholar] [CrossRef]
- De Urioste-Stone, S.M.; Pennington, P.M.; Pellecer, E.; Aguilar, T.M.; Samayoa, G.; Perdomo, H.D.; Enríquez, H.; Juárez, J.G. Development of a community-based intervention for the control of Chagas disease based on peridomestic animal management: An eco-bio-social perspective. Trans. R. Soc. Trop. Med. Hyg. 2015, 109, 159–167. [Google Scholar] [CrossRef]
- Predescu, M.; Sirbu, G.; Levins, R.; Awerbuch-Friedlander, T. On the dynamics of a deterministic and stochastic model for mosquito control. Appl. Math. Lett. 2007, 20, 919–925. [Google Scholar] [CrossRef]
- Predescu, M.; Levins, R.; Awerbuch-Friedlander, T. Analysis of a nonlinear system for community intervention in mosquito control. Discret. Contin. Dyn. Syst. Ser. B 2006, 6, 605–622. [Google Scholar] [CrossRef]
- Reiter, P.; Lathrop, S.; Bunning, M.; Biggerstaff, B.; Singer, D.; Tiwari, T.; Baber, L.; Amador, M.; Thirion, J.; Hayes, J.; et al. Texas Lifestyle Limits Transmission of Dengue Virus. Emerg. Infect. Dis. 2003, 9, 86–89. [Google Scholar] [CrossRef] [PubMed]
- Ramos, M.M.; Waterman, S.H.; Zielinski-Gutierrez, E.; Anaya-Lopez, L.; Brunkard, J.M.; Smith, B.; Fournier, M.; Muñoz, J.L.; Trujillo, A.R.; Hayden, M.H.; et al. Epidemic Dengue and Dengue Hemorrhagic Fever at the Texas–Mexico Border: Results of a Household-based Seroepidemiologic Survey, December 2005. Am. J. Trop. Med. Hyg. 2008, 78, 364–369. [Google Scholar] [CrossRef]
- Brunkard, J.M.; López, J.L.R.; Ramirez, J.; Cifuentes, E.; Rothenberg, S.J.; Hunsperger, E.A.; Moore, C.G.; Brussolo, R.M.; Villarreal, N.A.; Haddad, B.M. Dengue Fever Seroprevalence and Risk Factors, Texas–Mexico Border, 2004. Emerg. Infect. Dis. 2007, 13, 1477–1483. [Google Scholar] [CrossRef] [PubMed]
- Lucero, D.E.; Morrissey, L.A.; Rizzo, D.M.; Rodas, A.; Garnica, R.; Stevens, L.; Bustamante, D.M.; Monroy, M.C. Ecohealth Interventions Limit Triatomine Reinfestation following Insecticide Spraying in La Brea, Guatemala. Am. J. Trop. Med. Hyg. 2013, 88, 630–637. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tusting, L.S.; Bottomley, C.; Gibson, H.; Kleinschmidt, I.; Tatem, A.J.; Lindsay, S.W.; Gething, P.W. Housing Improvements and Malaria Risk in Sub-Saharan Africa: A Multi-Country Analysis of Survey Data. PLoS Med. 2017, 14, e1002234. [Google Scholar] [CrossRef] [PubMed]
- Chaves, L.F.; Rojas, M.R.; Jiménez, S.D.; Prado, M.; Rodríguez, R.M. Housing quality improvement is associated with malaria transmission reduction in Costa Rica. Socio-Econ. Plan. Sci. 2020, 100951. [Google Scholar] [CrossRef]
- CDC 2018 Case Counts in the US. Available online: https://www.cdc.gov/zika/reporting/2018-case-counts.html (accessed on 4 January 2021).
- Thomas, D.L.; Santiago, G.A.; Abeyta, R.; Hinojosa, S.; Torres-Velasquez, B.; Adam, J.K.; Evert, N.; Caraballo, E.; Hunsperger, E.; Muñoz-Jordán, J.L.; et al. Reemergence of Dengue in Southern Texas, 2013. Emerg. Infect. Dis. 2016, 22, 1002–1007. [Google Scholar] [CrossRef]
- Ayi, I.; Nonaka, D.; Adjovu, J.K.; Hanafusa, S.; Jimba, M.; Bosompem, K.M.; Mizoue, T.; Takeuchi, T.; Boakye, D.A.; Kobayashi, J. School-based participatory health education for malaria control in Ghana: Engaging children as health messengers. Malar. J. 2010, 9, 1–12. [Google Scholar] [CrossRef] [PubMed]
| Income | Community | Total Households | AGO | KAP |
|---|---|---|---|---|
| Low | Balli | 45 | 7 | 4 |
| Cameron | 85 | 6 | 6 | |
| Chapa | 30 | 5 | 5 | |
| Mesquite | 39 | 5 | 5 | |
| Middle | Christian Ct. | 34 | 6 | 5 |
| Rio Rico | 20 | 5 | 5 | |
| La Vista | 63 | 6 | 4 | |
| La Bonita | 67 | 7 | 6 |
| Target | Offset | Fixed | Distribution (AIC) |
|---|---|---|---|
| Indoor female Ae. aegypti | logs (Weeks of Trapping) | TypeAC + OpenWindow + OpenDoor + WaterStorage + OtherContainers + Income + Outdoor female + AP2.1 + AP2.2 + Window1 + Window2 + Door2 | Poisson (156.4) Negative Binomial 1 (152.2) Negative Binomial 2 (145.8) |
| Outdoor female Ae. aegypti | logs (Weeks of Trapping) | Vegetation + MessyYard + OpenWindow + OpenDoor + WaterStorage + OtherContainers + Tires + Income + AP2.1 + AP2.2 + Window1 + Window2 + Door1 + Door2 | Poisson (804.1) Negative Binomial 1 (337.2) Negative Binomial 2 (340.8) |
| Knowledge, Attitudes and Practices | Response | No. Positive Responses/Total (%) |
|---|---|---|
| Mosquitoes and their diseases | Recognized a mosquito larva from picture | 17/39 (43.6) |
| Recognized an adult mosquito from picture | 38/39 (97.4) | |
| Believed mosquitoes are most abundant during the summer | 20/38 (52.6) | |
| Believed the canals are a source for mosquitoes in their community | 17/37 (45.9) | |
| Had seen a mosquito in the past few days | 27/38 (71.1) | |
| Believed mosquitoes had an impact on their life | 33/38 (86.8) | |
| Health risk | 24/33 (72.7) | |
| Nuisance | 12/33 (36.4) | |
| Considered mosquitoes a problem in their community | 33/39 (84.6) | |
| Small or moderate | 21/39 (53.8) | |
| Serious | 12/39 (30.7) | |
| Knew that mosquitoes can transmit diseases | 34/39 (87.2) | |
| Zika | 27/34 (79.4) | |
| Dengue | 19/34 (55.9) | |
| Chikungunya | 6/34 (17.6) | |
| Malaria | 5/34 (14.7) | |
| West Nile | 2/34 (5.6) | |
| Knew someone that had been infected with dengue, chikungunya and/or Zika | 8/39 (20.5) | |
| Zika virus | Had heard about Zika virus before this interview | 33/39 (84.6) |
| Knew that Zika causes fever symptoms | 22/33 (66.7) | |
| Knew that Zika may affect babies | 8/33 (24.2) | |
| Knew another mode of transmission for Zika besides mosquitoes | 13/33 (39.4) | |
| Sexual intercourse | 10/13 (76.9) | |
| Congenital | 1/13 (7.7) | |
| Considered Zika a problem in the LRGV | 22/39 (66.7) | |
| Somewhat or slightly | 14/39 (35.8) | |
| Very or extreme | 8/39 (29.4) | |
| Worried about Zika because of family and children | 12/22 (54.5) |
| Knowledge, Attitudes and Practices | Response | No. Positive Responses/Total (%) |
|---|---|---|
| Prevention and control of mosquitoes | Had been bitten by mosquitoes inside or outside the home in the past week | 22/39 (56.4) |
| Stored water on their property for plants and flowers | 7/10 (70.0) | |
| Left windows open for ventilation | 19/39 (48.2) | |
| Left door open for ventilation | 17/39 (43.9) | |
| Believed that they should do something if they had a mosquito problem in their property | 37/39 (94.9) | |
| Use insect repellent | 29/37 (78.4) | |
| Spray insecticide | 13/37 (35.1) | |
| Dump stagnant water | 6/37 (16.2) | |
| Call city or county | 5/37 (13.9) | |
| Limited outdoor activities because of mosquitoes | 25/39 (64.1) | |
| AGO intervention | Would support an AGO intervention in their community if the three traps were free and maintenance was provided | 37/39 (94.9) |
| Would support intervention if AGO traps were free, but household need to provide maintenance | 23/37 (62.2) | |
| Would support intervention if AGO traps were $15 each and household provided maintenance | 9/37 (25.0) |
| Question | Variable | No. Positive Responses/Total (%) |
|---|---|---|
| Size of lot (m2) | 262–600 | 9/39 (23.1) |
| 601–1000 | 19/39 (48.7) | |
| 1001–1204 | 11/39 (28.2) | |
| No. of bedrooms | 1–2 | 18/39 (46.1) |
| 3–4 | 19/39 (48.7) | |
| 5 | 2/39 (5.1) | |
| Length of vegetation in the yard | Short (< 5 cm) | 19/39 (48.7) |
| Medium (5–10 cm) | 17/39 (43.6) | |
| Long (>10 cm) | 3/39 (7.7) | |
| Houses with containers in peridomicile | Plant pots | 35/39 (89.7) |
| Tin cans | 18/39 (46.2) | |
| Tires | 17/39 (43.6) | |
| Drum water barrels | 2/39 (5.1) | |
| Wall material | Timber/Metal | 18/39 (46.1) |
| Cement | 3/39 (7.7) | |
| Brick | 18/39 (46.2) | |
| Type of roof and material | Flat and cement | 2/39 (5.1) |
| Pitched and asphalt shingles | 37/39 (94.9) | |
| Type of A/C unit | None | 1/39 (2.6) |
| Window mounted | 17/39 (43.6) | |
| Central system | 21/39 (53.9) | |
| Window | With mesh | 259/389 (66.6) |
| No holes | 232/259 (89.2) | |
| Holes < than 0.5cm | 15/259 (5.8) | |
| Holes ≥ than 0.5cm | 13/259 (5.0) | |
| Doors | Exterior door | 91/104 (87.5) |
| Exterior door with screen | 47/91 (51.6) | |
| Exterior door with gap in the frame | 20/91 (21.9) |
| Variable | Exp (Estimate) | Estimate | Std. Error | 95% CI |
|---|---|---|---|---|
| (Intercept) | −5.51 | 0.86 | −7.35–−3.87 | |
| Type AC (None) | 1.10 | 0.09 | 1.13 | −2.07–2.67 |
| Type AC (Window) | 4.68 | 1.54 | 0.57 | 0.39–2.74 * |
| OpenWindow (Yes) | 3.73 | 1.32 | 0.58 | 0.21–2.58 * |
| WaterStorage (Yes) | 2.83 | 1.04 | 0.53 | −0.05–2.10 |
| OtherContainers | 1.01 | 0.01 | 0.00 | 0.005–0.02 |
| AP2.1 | 0.49 | −0.71 | 0.22 | −1.16–−0.27 * |
| Window1 | 2.12 | 0.75 | 0.27 | 0.23–1.29 * |
| Door2 | 1.66 | 0.51 | 0.26 | 0.01–1.09 * |
| Outdoor female | 1.01 | 0.01 | 0.00 | 0.005–0.02 |
| Variable | Exp (Estimate) | Estimate | Std. Error | 95% CI |
|---|---|---|---|---|
| (Intercept) | 2.27 | 0.28 | 1.70–2.81 | |
| Vegetation (>51%) | 0.38 | −0.96 | 0.30 | −1.55–−0.36 * |
| OpenDoor | 0.30 | −1.19 | 0.27 | −1.74–−0.66 * |
| Tires | 0.92 | −0.08 | 0.02 | −0.12–−0.04 * |
| Income (>$75k) | 0.81 | −0.21 | 0.38 | −0.98–0.53 |
| Income ($25–$50k) | 5.01 | 1.61 | 0.31 | 0.99–2.23 * |
| AP2.1 | 1.65 | 0.50 | 0.11 | 0.27–0.72 * |
| AP2.2 | 1.40 | 0.34 | 0.15 | 0.01–0.64 * |
| Door1 | 1.23 | 0.20 | 0.07 | 0.01–0.34 * |
| Door2 | 0.70 | −0.35 | 0.09 | −0.54–−0.17 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Juarez, J.G.; Garcia-Luna, S.M.; Medeiros, M.C.I.; Dickinson, K.L.; Borucki, M.K.; Frank, M.; Badillo-Vargas, I.; Chaves, L.F.; Hamer, G.L. The Eco-Bio-Social Factors That Modulate Aedes aegypti Abundance in South Texas Border Communities. Insects 2021, 12, 183. https://doi.org/10.3390/insects12020183
Juarez JG, Garcia-Luna SM, Medeiros MCI, Dickinson KL, Borucki MK, Frank M, Badillo-Vargas I, Chaves LF, Hamer GL. The Eco-Bio-Social Factors That Modulate Aedes aegypti Abundance in South Texas Border Communities. Insects. 2021; 12(2):183. https://doi.org/10.3390/insects12020183
Chicago/Turabian StyleJuarez, Jose G., Selene M. Garcia-Luna, Matthew C. I. Medeiros, Katherine L. Dickinson, Monica K. Borucki, Matthias Frank, Ismael Badillo-Vargas, Luis F. Chaves, and Gabriel L. Hamer. 2021. "The Eco-Bio-Social Factors That Modulate Aedes aegypti Abundance in South Texas Border Communities" Insects 12, no. 2: 183. https://doi.org/10.3390/insects12020183
APA StyleJuarez, J. G., Garcia-Luna, S. M., Medeiros, M. C. I., Dickinson, K. L., Borucki, M. K., Frank, M., Badillo-Vargas, I., Chaves, L. F., & Hamer, G. L. (2021). The Eco-Bio-Social Factors That Modulate Aedes aegypti Abundance in South Texas Border Communities. Insects, 12(2), 183. https://doi.org/10.3390/insects12020183







