Experimental Analysis of Catheter Push–Pull Forces: Effects of Vascular Curvature, Motion Speed, and Lumen Material
Abstract
1. Introduction
2. Experiment Design
2.1. Static Mechanics Experiment
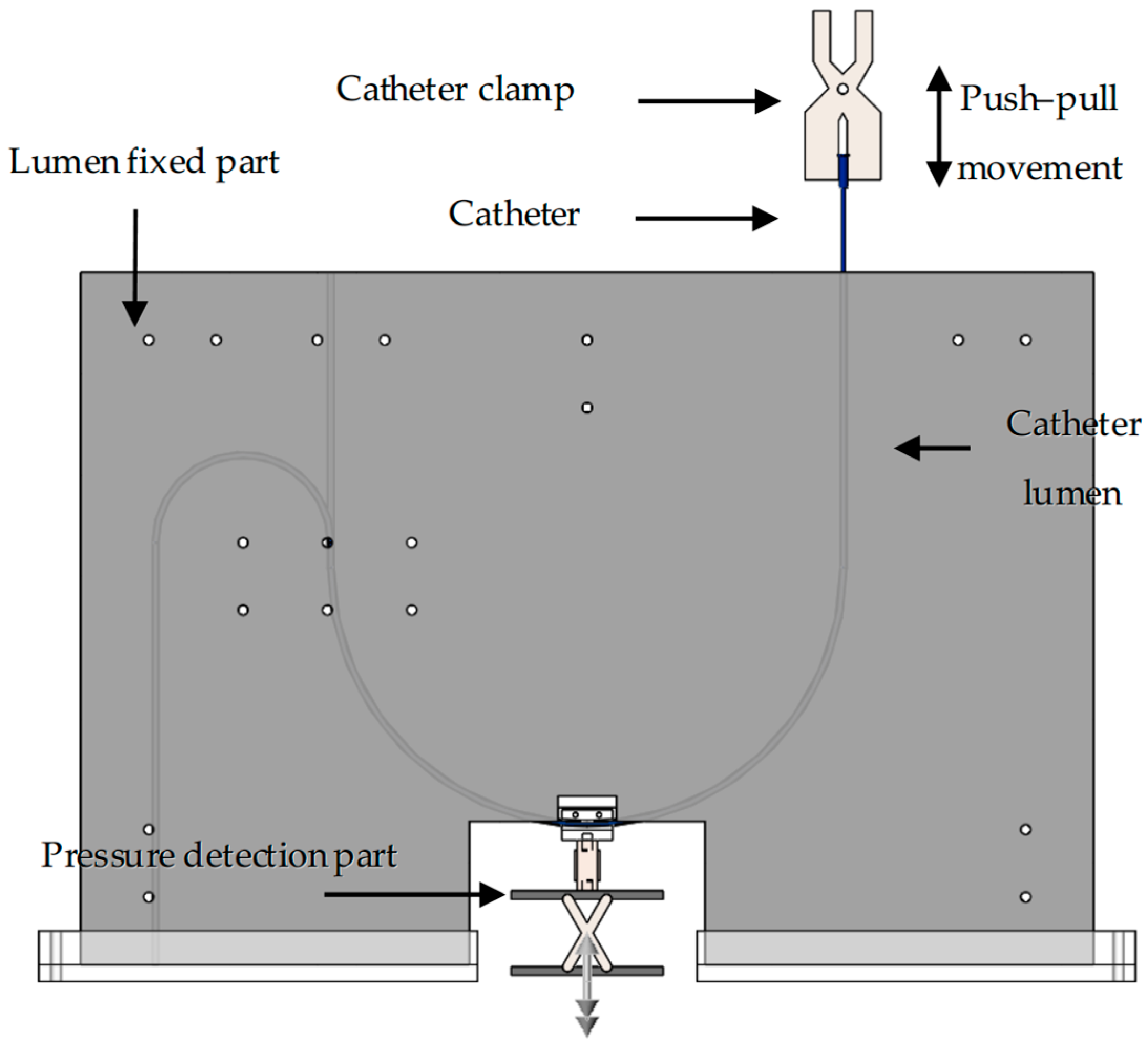
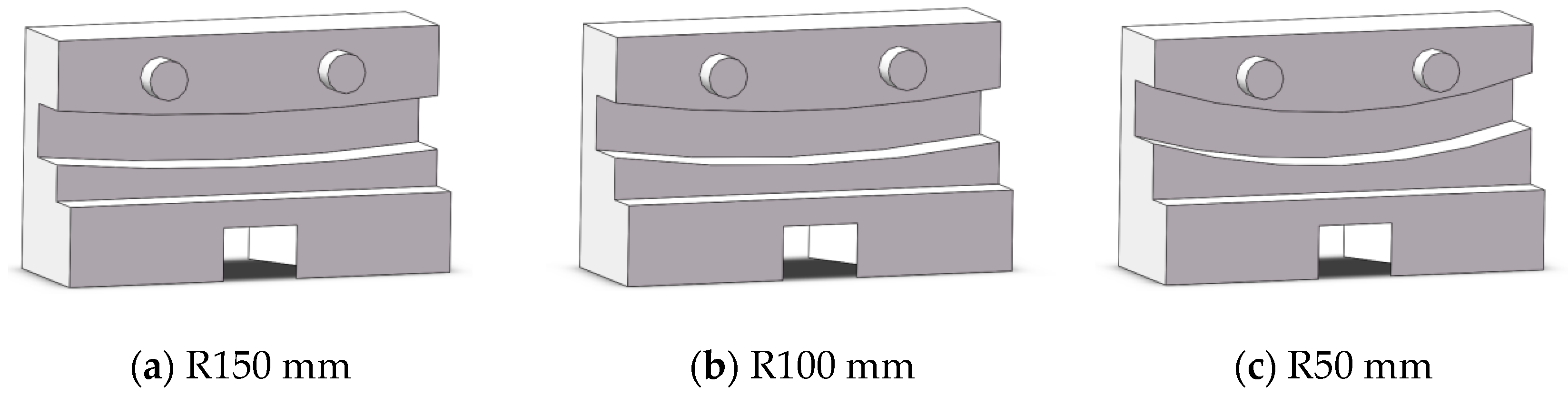
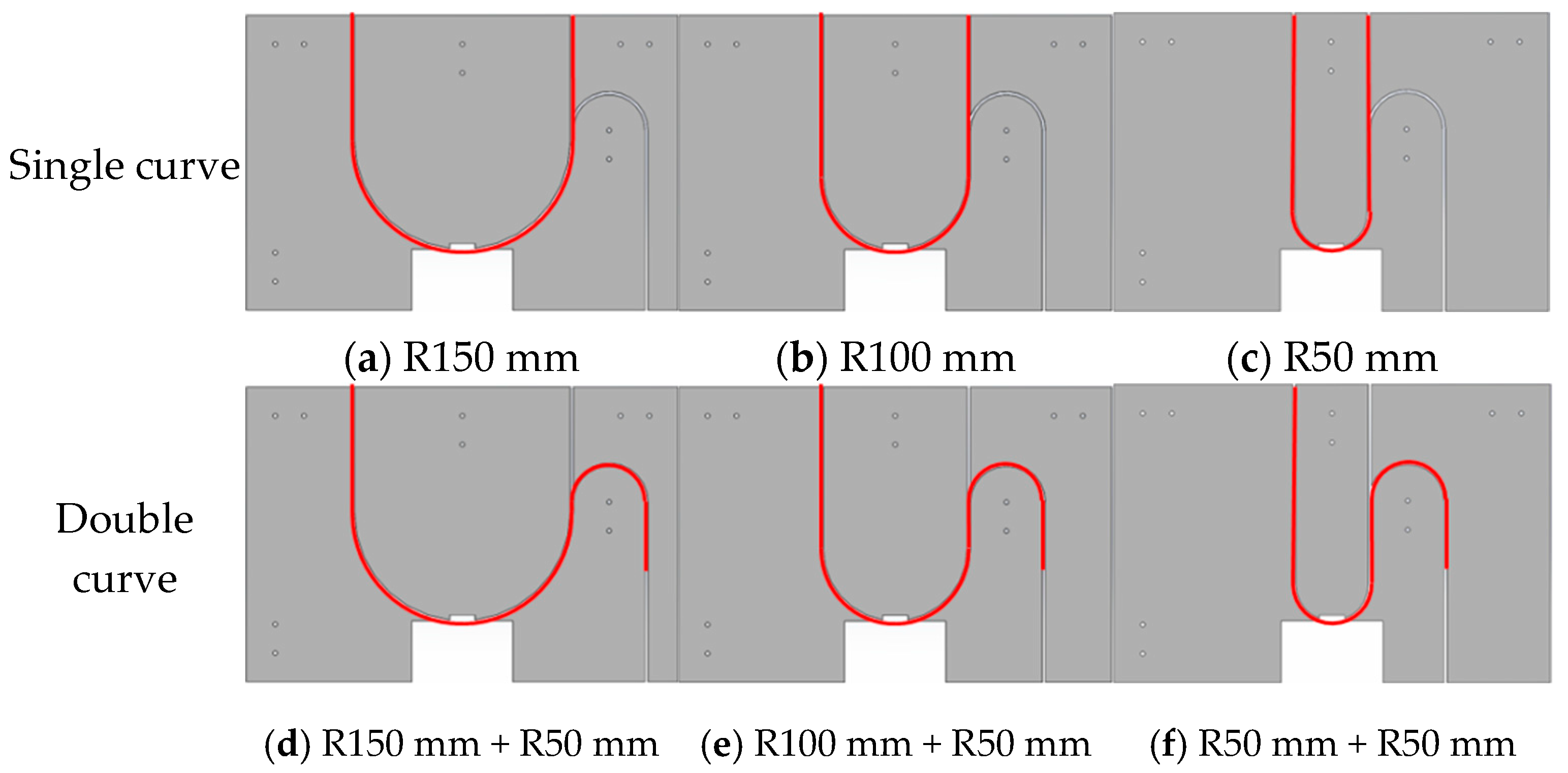
2.2. Catheter–Vessel Contact Experiment Platform
2.3. Catheter/Vessel Contact Experiment Protocol
2.4. Data Statistics
3. Results and Discussion
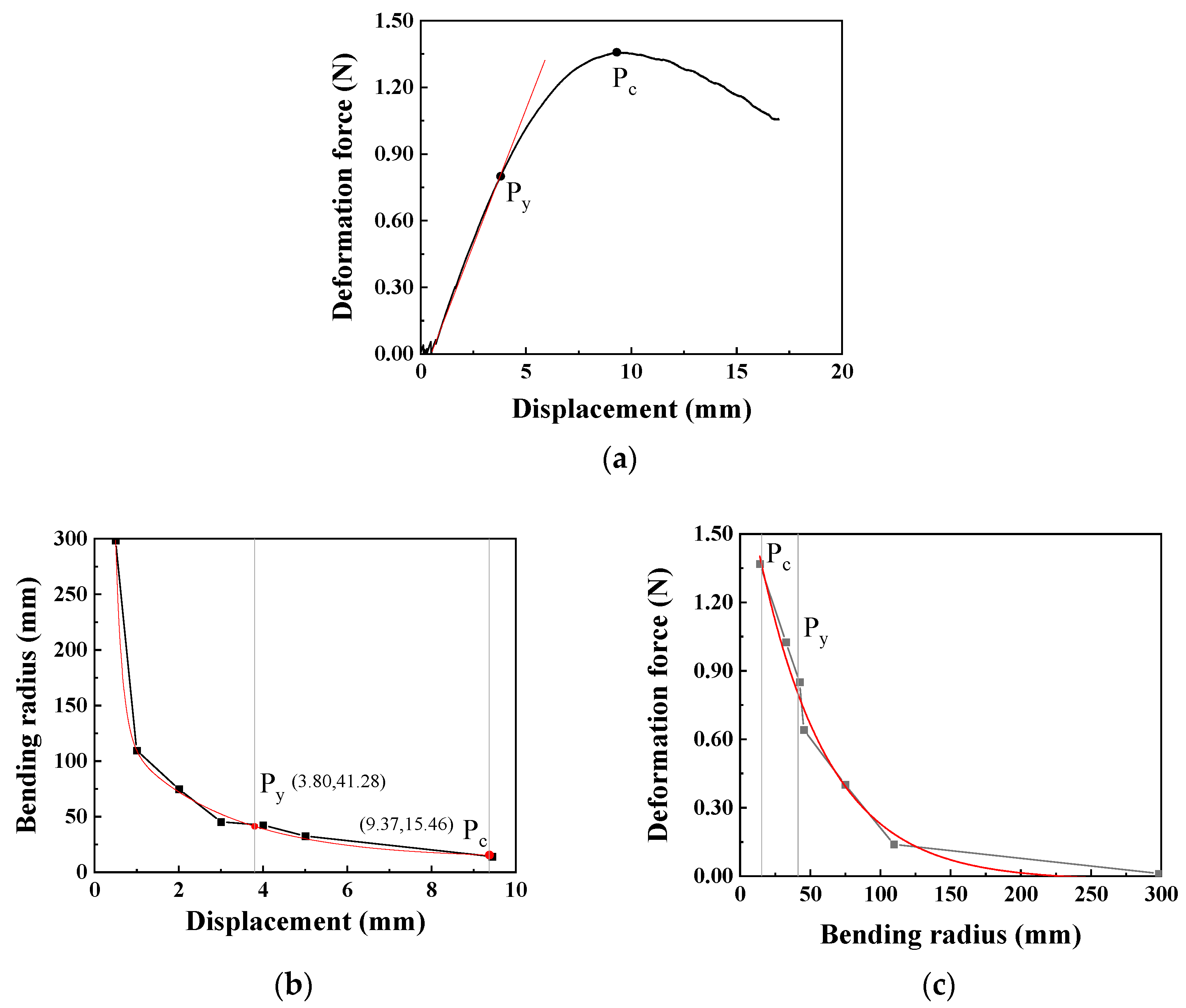
3.1. The Influence of Static Bending of Catheters on Contact
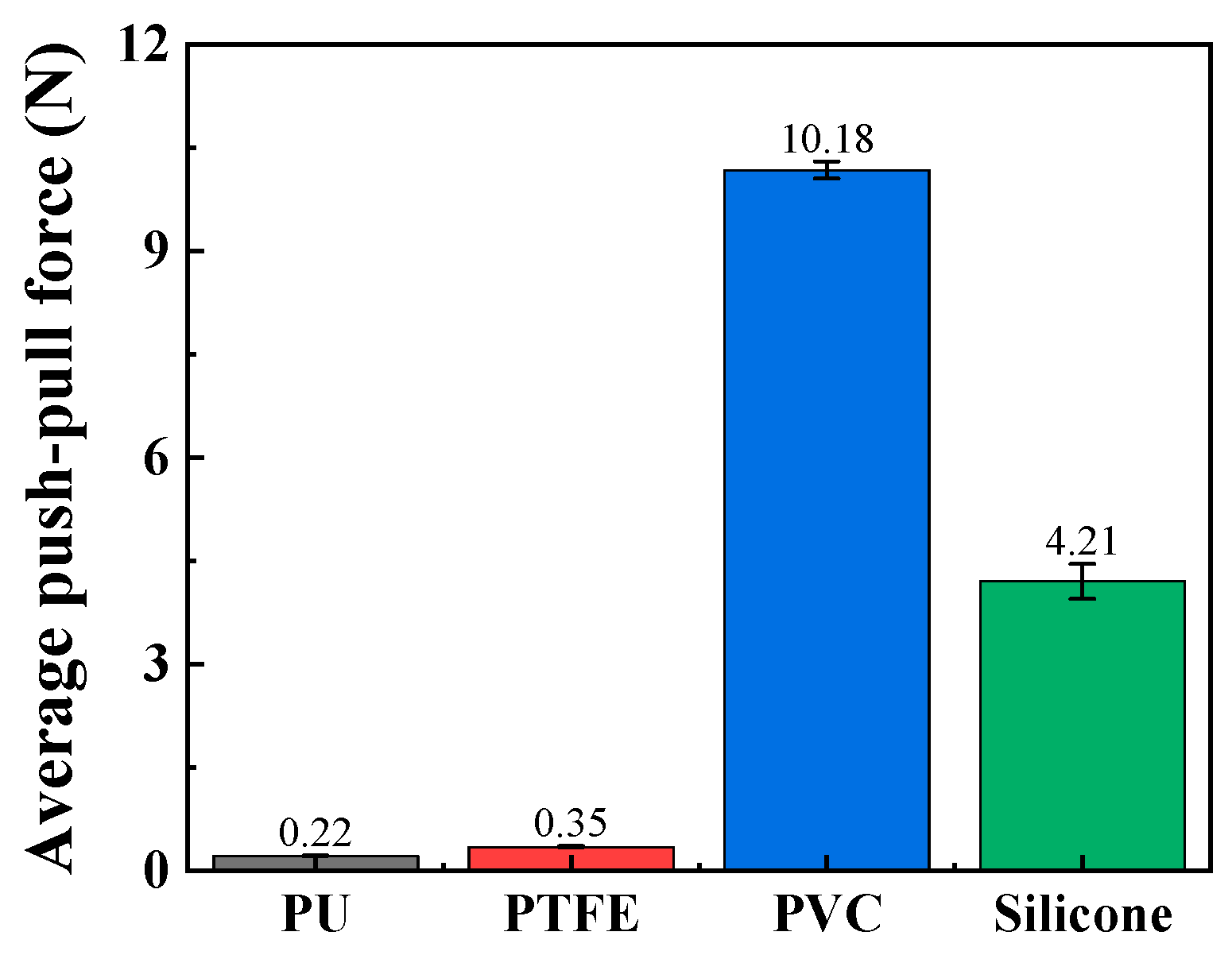
3.2. The Influence of Lumen Material on Contact
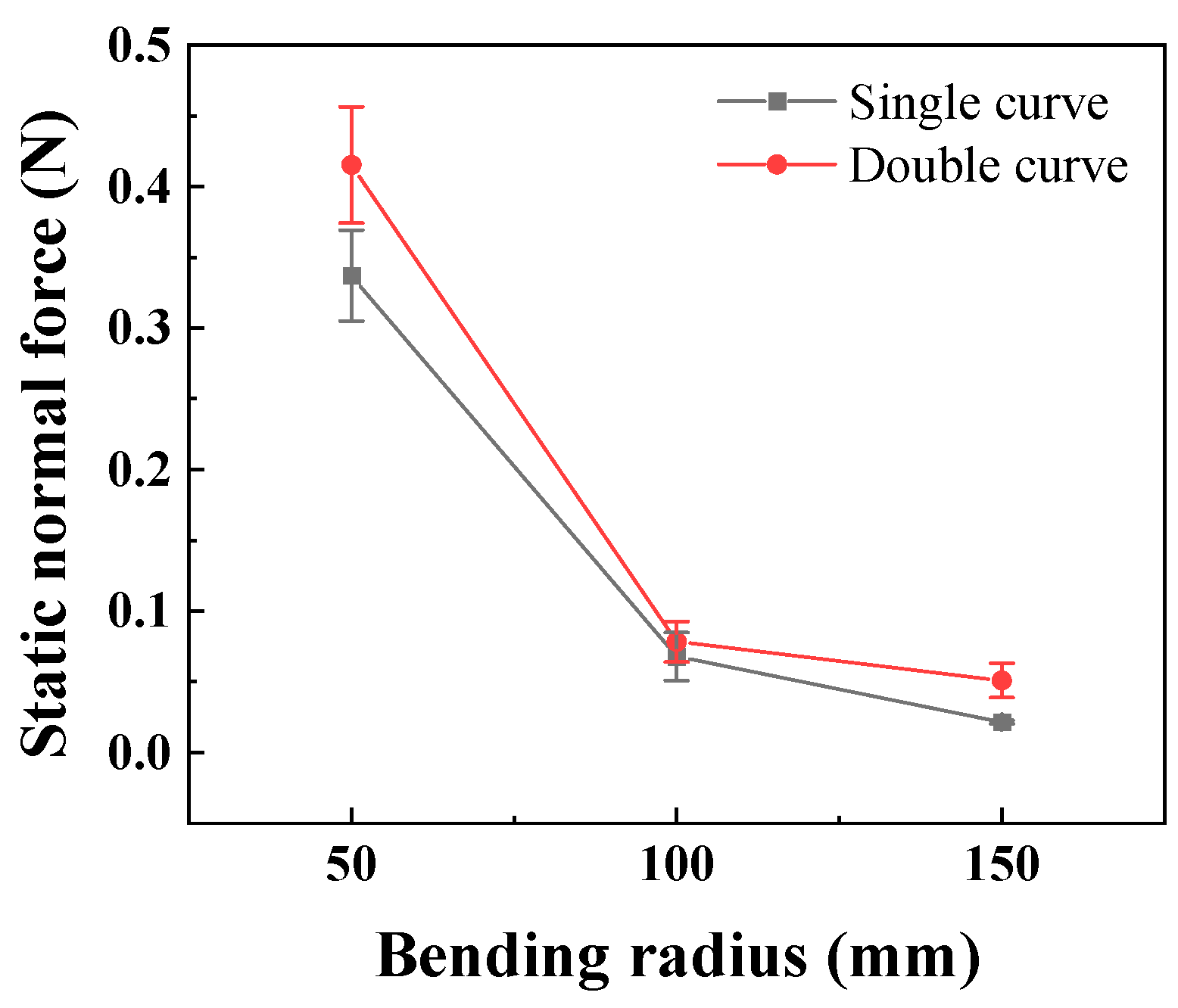
3.3. The Influence of the Lumen Curvature Degree on Contact
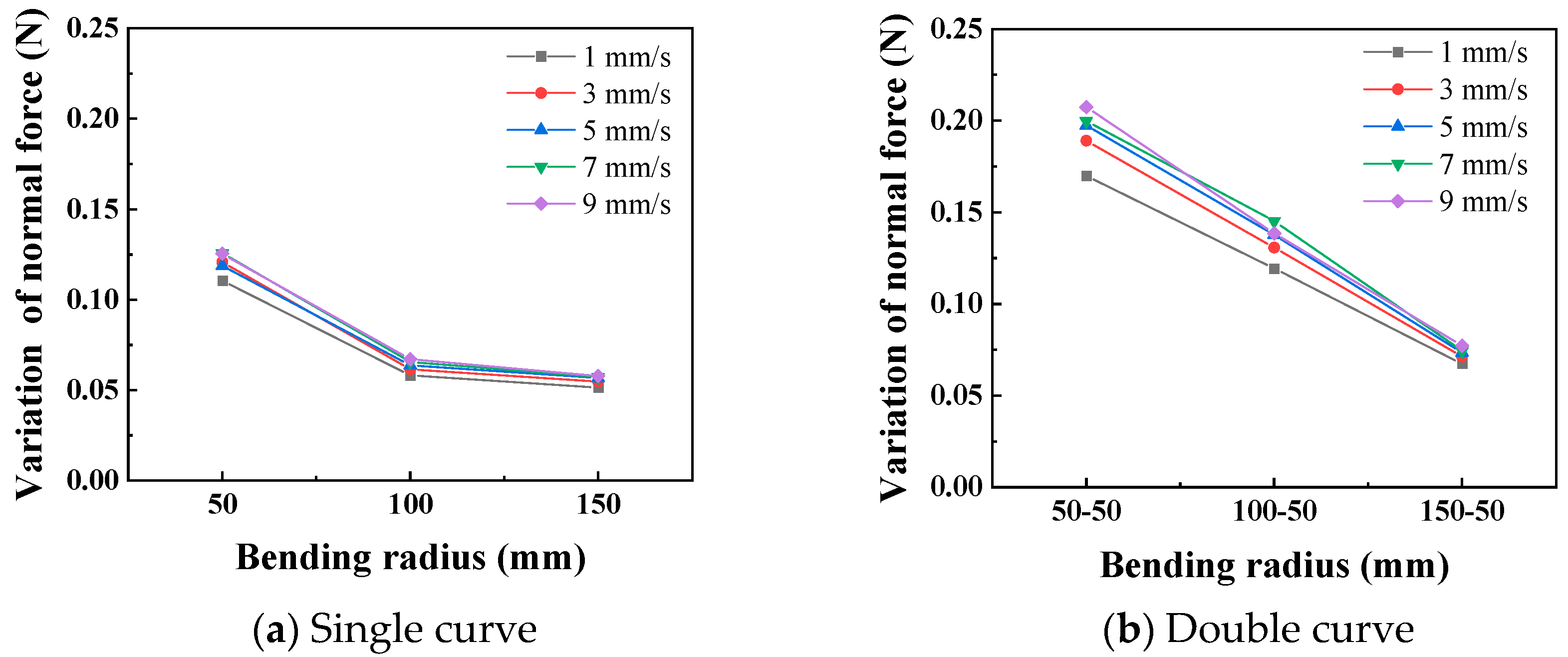
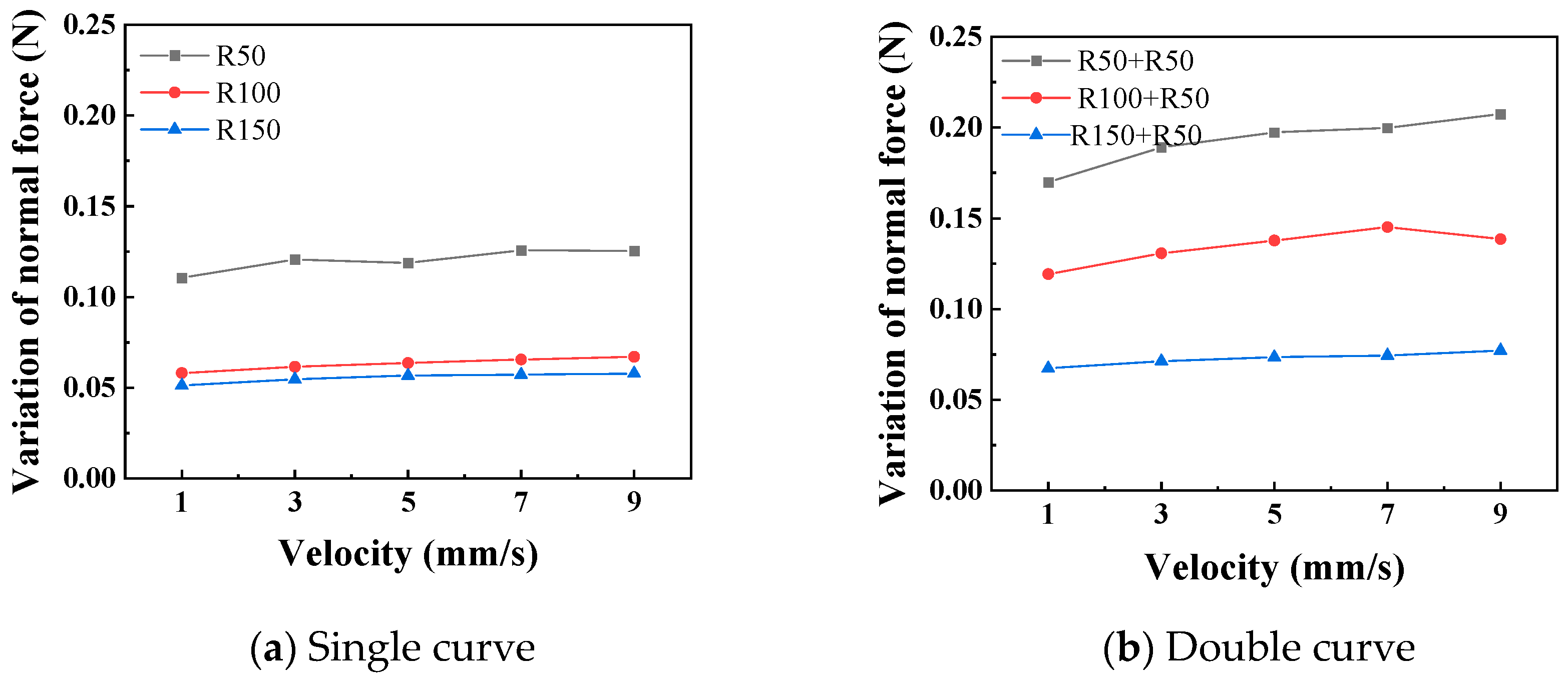
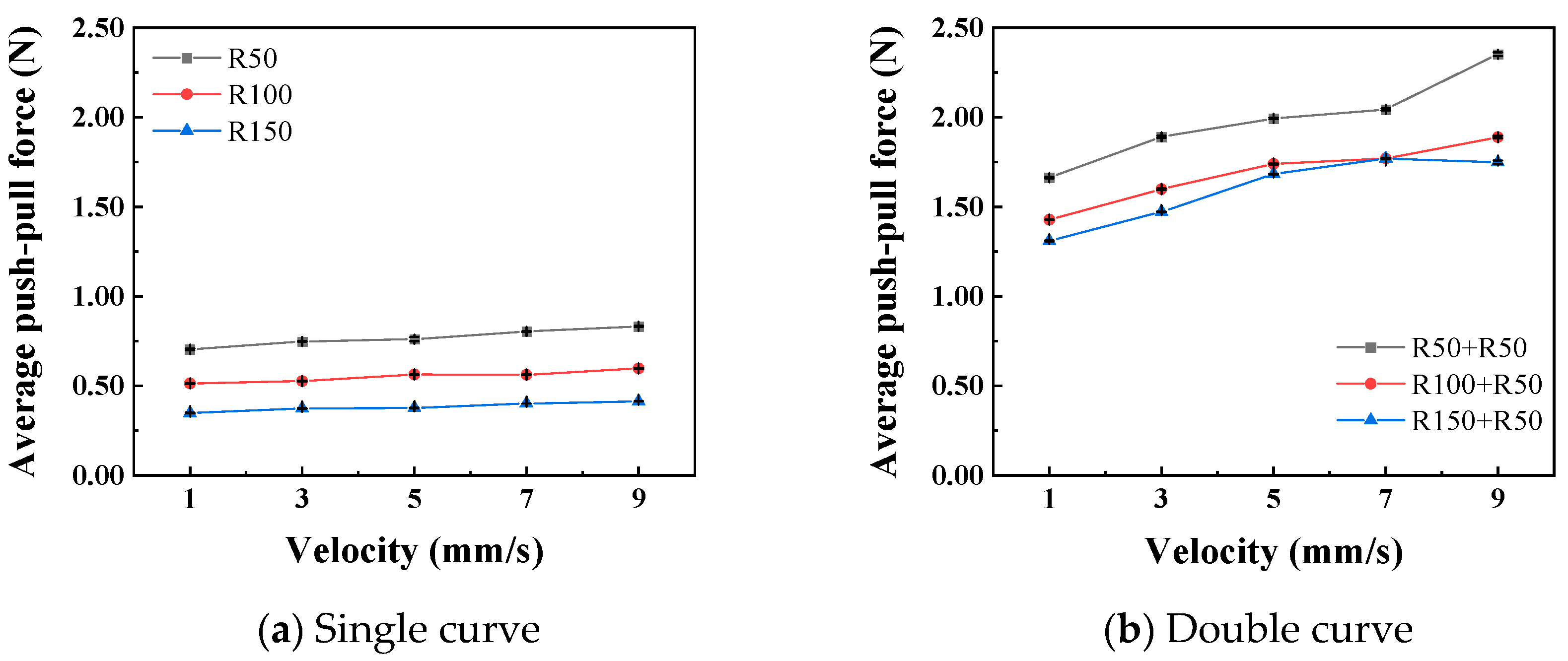
3.4. The Influence of the Push–Pull Speed on Contact
4. Discussion
5. Conclusions
- In the three-point bending test, the bending deformation force of the catheter increased as the radius decreased. It first reached the yield point at a bending radius of 41.28 mm, with a bending deformation force of 0.8 N; it reached the critical point at a bending radius of 15.46 mm, with a maximum bending deformation force of 1.36 N.
- PVC and silicone materials are not suitable for simulating the vascular lumen due to their excessive push–pull resistance. TPU and PTFE materials have relatively small and similar push–pull resistance.
- The normal force exerted by the catheter on the lumen in a static state increased as the curve radius decreased and increased with the increase in the number of curves. The curve radius and the curve number of the catheter lumen can be regarded as the degree of lumen curvature. The smaller the curve radius and the greater the curve number, the higher the degree of lumen curvature.
- When moving at a given speed within the lumen, the normal force exerted by the catheter on the lumen and the push–pull force at the catheter tip increased as the curve radius decreased and increased with the increase in the curve number. When the catheter moves in a lumen with a given curve radius, both the normal force exerted on the lumen and the average push–pull force at the catheter tip increase with increasing speed.
- When the catheter performed push–pull movements in the lumen, the degree of lumen curvature had a more significant impact on the push–pull force at the catheter tip and the push–pull force on the lumen compared to the push–pull speed. Therefore, in vascular interventional procedures, it is necessary to comprehensively consider the limitations of vascular curvature and the control of push–pull speed to select appropriate interventional devices for the operation.
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Rincón, I.D.; Williams, K.; Stern, M.P.; Freeman, G.L.; Escalante, A. High incidence of cardiovascular events in a rheumatoid arthritis cohort not explained by traditional cardiac risk factors. Arthritis Rheum. 2001, 44, 2737–2745. [Google Scholar] [CrossRef] [PubMed]
- Lagiou, P.; Sandin, S.; Lof, M.; Trichopoulos, D.; Adami, H.O.; Weiderpass, E. Low carbohydrate-high protein diet and incidence of cardiovascular diseases in Swedish women: Prospective cohort study. Bmj Br. Med. J. 2012, 345, 1759–2151. [Google Scholar] [CrossRef] [PubMed]
- Bulow, B. Hypopituitary females have a high incidence of cardiovascular morbidity and an increased prevalence of cardiovascular risk factors. J. Clin. Endocrinol. Metab. 2000, 85, 574–584. [Google Scholar] [CrossRef]
- Cheung, A.K.; Wu, L.L.; Kablitz, C.; Leypoldt, J.K. Atherogenic lipids and lipoproteins in hemodialysis patients. Am. J. Kidney Dis. 1993, 22, 271–276. [Google Scholar] [CrossRef]
- Avina-Zubieta, J.A.; Thomas, J.; Sadatsafavi, M.; Lehman, A.J.; Lacaille, D. Risk of incident cardiovascular events in patients with rheumatoid arthritis: A meta-analysis of observational studies. Ann. Rheum. Dis. 2012, 71, 1524–1529. [Google Scholar] [CrossRef]
- Ungprasert, P.; Charoenpong, P.; Ratanasrimetha, P.; Thongprayoon, C.; Suksaranjit, P. Risk of coronary artery disease in patients with systemic sclerosis: A systematic review and meta-analysis. Clin. Rheumatol. 2014, 33, 1099–1104. [Google Scholar] [CrossRef]
- Rat, N.; Muntean, I.; Opincariu, D.; Gozar, L.; Tognel, R.; Chiu, M. Cardiovascular Imaging for Guiding Interventional Therapy in Structural Heart Diseases. Curr. Med. Imaging 2020, 16, 111–122. [Google Scholar] [CrossRef]
- Shen, H.; Feng, X.X.; Guo, Q.Y.; Zhou, Y.J. Updates of developments in interventional therapy for elderly patients with cardiovascular diseases. J. Geriatr. Cardiol. 2024, 21, 1–3. [Google Scholar] [CrossRef]
- Guo, B.; Shi, S.; Guo, Y.; Xiong, J.; Wang, B.; Dong, Z.; Gao, D.; Tu, Y. Interventional therapies for chronic heart failure: An overview of recent developments. ESC Heart Fail. 2025, 12, 1081–1094. [Google Scholar] [CrossRef]
- Conradi, L.; Seiffert, M.; Franzen, O.; Baldus, S.; Schirmer, J.; Meinertz, T.; Reichenspurner, H.; Treede, H. First experience with transcatheter aortic valve implantation and concomitant percutaneous coronary intervention. Clin. Res. Cardiol. 2011, 100, 311–316. [Google Scholar] [CrossRef] [PubMed]
- Yuan, H.; Lin, C.; Wang, C. Research progress of the interaction between blood vessels and intervention catheters and its surface modification. Friction 2025, 13, 9441003. [Google Scholar] [CrossRef]
- Takashima, K.; Shimomura, R.; Kitou, T.; Terada, H.; Ikeuchi, K. Contact and friction between catheter and blood vessel. Tribol. Int. 2007, 40, 319–328. [Google Scholar] [CrossRef]
- Prokopovich, P.; Perni, S. Contact interactions of aorta against PVC catheters. Tribol. Int. 2013, 66, 157–164. [Google Scholar] [CrossRef]
- Wagner, R.M.F.; Maiti, R.; Carré, M.J.; Perrault, C.M.; Lewis, R. Bio-tribology of Vascular Devices: A Review of Tissue/Device Friction Research. Biotribology 2021, 25, 100169. [Google Scholar] [CrossRef]
- Song, W.; Liu, Z.; Li, Q.; Zhang, Y.; Lyu, Y.; Gao, Z.; Zhuang, J.; Lin, C. Research on the friction-damage mechanism between magnetic guide strip and tracheal tissue for magnetic navigation. Tribol. Int. 2025, 215, 111487. [Google Scholar] [CrossRef]
- Lin, C.; Yuan, H.; Wang, C. The study of quantitative friction-damage models at the interventional catheter-vascular tissues interface. Friction 2025. [Google Scholar] [CrossRef]
- Sobolewski, P.; El Fray, M. Cardiac catheterization: Consequences for the endothelium and potential for nanomedicine. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnology 2015, 7, 458–473. [Google Scholar] [CrossRef]
- Dellimore, K.H.; Franklin, S.E.; Helyer, A.R. A Review of Catheter Related Complications During Minimally Invasive Transcatheter Cardiovascular Intervention with Implications for Catheter Design. Cardiovasc. Eng. Technol. 2014, 5, 217–232. [Google Scholar] [CrossRef]
- Eklund, A.; Bergh, A.; Lindahl, O.A. A catheter tactile sensor for measuring hardness of soft tissue: Measurement in a silicone model and in an in vitro human prostate model. Med. Biol. Eng. Comput. 1999, 37, 618. [Google Scholar] [CrossRef]
- Wang, Y.; Guo, S.; Tamiya, T.; Hirata, H.; Ishihara, H. A Blood Vessel Deformation Model Based Virtual-reality Simulator for the Robotic Catheter Operating System. Neurosci. Biomed. Eng. 2014, 2, 126–131. [Google Scholar] [CrossRef]
- Chen, Z.; Zheng, Q.; Tong, Z.; Huang, X.; Yu, A. Numerical modelling of the interaction between dialysis catheter, vascular vessel and blood considering elastic structural deformation. Int. J. Numer. Methods Biomed. Eng. 2024, 40, e3811. [Google Scholar] [CrossRef]
- Bostan, L.E.; Noble, C.; Smulders, N.; Lewis, R.; Carré, M.J.; Franklin, S.; Green, N.H.; Macneil, S. Measurement of friction-induced changes in pig aorta fibre organization by non-invasive imaging as a model for detecting the tissue response to endovascular catheters. Biotribology 2017, 12, 24–32. [Google Scholar] [CrossRef]
- Gao, B.; Hu, K.; Guo, S.; Guo, P. Analysis of the haptic collision and deformation of the blood vessel model for the microsurgery training system. In Proceedings of the IEEE International Conference on Robotics & Biomimetics, Shenzhen, China, 12–14 December 2013. [Google Scholar] [CrossRef]
- Takagi, R.; Osada, K.; Hanafusa, A.; Takagi, M.; Mohamaddan, S.B.; Mitsui, K.; Anzai, H. Development of a remote-control system for catheterization capable of high-speed force feedback. Int. J. Comput. Assist. Radiol. Surg. 2023, 18, 763–773. [Google Scholar] [CrossRef]
- Lynn, S.; O’Malley, P.; Tanner, D.; Moore, S. Refining early stage interventional composite catheter design. Procedia Manuf. 2019, 38, 282–290. [Google Scholar] [CrossRef]
- White, E.; Bienemann, A.; Malone, J.; Megraw, L.; Bunnun, C.; Wyatt, M.; Gill, S. An evaluation of the relationships between catheter design and tissue mechanics in achieving high-flow convection-enhanced delivery. J. Neurosci. Methods 2011, 199, 87–97. [Google Scholar] [CrossRef]
- Kazmierska, K.; Szwast, M.; Ciach, T. Determination of urethral catheter surface lubricity. J. Mater. Sci. Mater. Med. 2008, 19, 2301–2306. [Google Scholar] [CrossRef]
- Shi, W.; Whittington, A.R.; Grant, D.C.; Boreyko, J.B. Reduced Sliding Friction of Lubricant-Impregnated Catheters. ACS Omega 2024, 10, 3635–3641. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.; Yuan, H.; Wang, C. Study on Lubricating Nano-coatings for Cardiovascular Catheters Based on Molecular Self-Assembly and Schiff Base Reaction. Friction 2025. [Google Scholar] [CrossRef]
- Lin, C.; Kaper, H.J.; Li, W.; Splinter, R.; Sharma, P.K. Role of endothelial glycocalyx in sliding friction at the catheter-blood vessel interface. Sci. Rep. 2020, 10, 11855. [Google Scholar] [CrossRef]
- Waseem, W.; Sherief, G.; Abdulaziz, A.-A.; David, F.K. Radial artery diameter: A comprehensive systematic review of anatomy. J. NeuroInterventional Surg. 2022, 14, 1274–1278. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Zhou, H.; Zhao, Y.; Zhang, J.; Zhang, T. Research on real-time detection system of catheter delivering force in vascular interventional robots. J. Biomed. Eng. 2022, 39, 359–369. [Google Scholar] [CrossRef]
- Adams, M.J.; Briscoe, B.J.; Johnson, S.A. Friction and lubrication of human skin. Tribol. Lett. 2007, 26, 239–253. [Google Scholar] [CrossRef]
- Tang, W.; Ge, S.R.; Zhu, H.; Cao, X.C.; Li, N. The Influence of Normal Load and Sliding Speed on Frictional Properties of Skin. J. Bionic Eng. 2008, 5, 33–38. [Google Scholar] [CrossRef]
- Hendriks, C.P.; Franklin, S.E. Influence of Surface Roughness, Material and Climate Conditions on the Friction of Human Skin. Tribol. Lett. 2010, 37, 361–373. [Google Scholar] [CrossRef]
- Ger, M.D.; Hou, K.H.; Wang, L.M.; Hwang, B.J. The friction and wear of Ni–P–PTFE composite deposits under water lubrication. Mater. Chem. Phys. 2003, 77, 755–764. [Google Scholar] [CrossRef]
- Greenwood, J.A.; Tabor, D. The Friction of Hard Sliders on Lubricated Rubber: The Importance of Deformation Losses. Proc. Phys. Soc. 2002, 71, 989. [Google Scholar] [CrossRef]
- Lincoln, B. Elastic Deformation and the Laws of Friction. Nature 1953, 172, 169–170. [Google Scholar] [CrossRef]
- Lin, C.; Ren, P.; Li, W.; Deng, H.; Zhou, Z. Finite-element modelling of frictional behaviour between oesophagus and endoscope. Biosurface Biotribology 2020, 6, 34. [Google Scholar] [CrossRef]
- Spilker, R.L.; Suh, J.K.; Mow, V.C. A finite element analysis of the indentation stress-relaxation response of linear biphasic articular cartilage. J. Biomech. Eng. 1992, 114, 191–201. [Google Scholar] [CrossRef]
- Mow, V.C.; Ateshian, G.A.; Lai, W.M.; Gu, W.Y. Effects of fixed charges on the stress-relaxation behavior of hydrated soft tissues in a confined compression problem. Int. J. Solids Struct. 1998, 35, 4945–4962. [Google Scholar] [CrossRef]
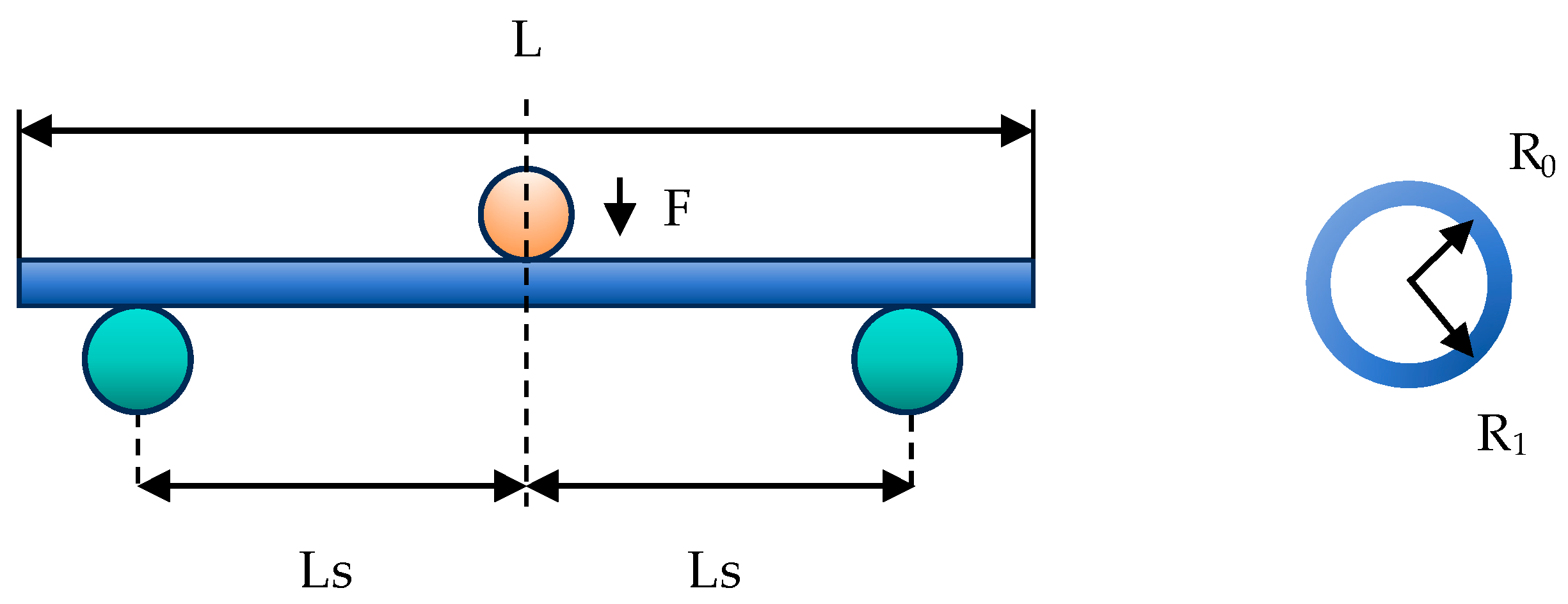


| Catheter Brand | Outer Diameter (Rl/mm) | Inter Diameter (Rl/mm) | Length (L/mm) | Span (Ls/mm) | Speed (mm/s) |
|---|---|---|---|---|---|
| Cordis@AL1 | 2 | 1.8 | 200 | 25 | 0.1 |
| Type | Parameter | Image |
|---|---|---|
| Model | DYLY-106 |  |
| Range | 0 kg~1 kg | |
| Output sensitivity | 1.2 mv-v | |
| Comprehensive error | 0.05% F.S | |
| Response frequency | 10 kHz |
| Group | Curve Radius (mm) | Speed (mm/s) | Materials |
|---|---|---|---|
| 1 | 50 | 1, 3, 5, 7, 9 | PTFE |
| 2 | 100 | ||
| 3 | 150 |
| Group | Curve 1 Radius (mm) | Curve 2 Radius (mm) | Speed (mm/s) | Materials |
|---|---|---|---|---|
| 1 | 50 | 50 | 1, 3, 5, 7, 9 | PTFE |
| 2 | 100 | 50 | ||
| 3 | 150 | 50 |
| Variation Source | Quadratic SUM | Degree of Freedom | Mean Square Error | p | Significance | |
|---|---|---|---|---|---|---|
| Curve radius | 2 | 7.41 | ||||
| Curve number | 1 | 8.06 | ||||
| Deviation | 2 | |||||
| Sum | 5 |
| Variation Source | Quadratic Sum | Degree of Freedom | Mean Square Error | p | Significance | |
|---|---|---|---|---|---|---|
| Curve radius | 0.12 | 2 | 0.06 | 29.17 | * | |
| Curve number | 2.30 | 1 | 2.30 | 1080.75 | ** | |
| Deviation | 2 | |||||
| Sum | 2.43 | 5 |
| Variation Source | Quadratic Sum | Degree of Freedom | Mean Square Error | p | Significance | |
|---|---|---|---|---|---|---|
| Curve radius | 2 | 1405.06 | ** | |||
| Velocity | 4 | 10.84 | ** | |||
| Deviation | 8 | |||||
| Sum | 14 |
| Variation Source | Quadratic Sum | Degree of Freedom | Mean Square Error | p | Significance | |
|---|---|---|---|---|---|---|
| Curve radius | 2 | 519.32 | ** | |||
| Velocity | 4 | 7.08 | ** | |||
| Deviation | 8 | |||||
| Sum | 14 |
| Variation Source | Quadratic Sum | Degree of Freedom | Mean Square Error | p | Significance | |
|---|---|---|---|---|---|---|
| Curve radius | 0.38 | 2 | 0.19 | 839.72 | ** | |
| Velocity | 0.02 | 4 | 17.10 | ** | ||
| Deviation | 8 | |||||
| Sum | 0.39 | 14 |
| Variation Source | Quadratic Sum | Degree of Freedom | Mean Square Error | p | Significance | |
|---|---|---|---|---|---|---|
| Curve radius | 0.42 | 2 | 0.21 | 44.05 | ** | |
| Velocity | 0.50 | 4 | 0.12 | 25.85 | ** | |
| Deviation | 0.04 | 8 | ||||
| Sum | 0.96 | 14 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hu, J.; Chen, X.; Jiang, X.; Zheng, Z.; Fang, Y.; Lin, C. Experimental Analysis of Catheter Push–Pull Forces: Effects of Vascular Curvature, Motion Speed, and Lumen Material. Lubricants 2025, 13, 552. https://doi.org/10.3390/lubricants13120552
Hu J, Chen X, Jiang X, Zheng Z, Fang Y, Lin C. Experimental Analysis of Catheter Push–Pull Forces: Effects of Vascular Curvature, Motion Speed, and Lumen Material. Lubricants. 2025; 13(12):552. https://doi.org/10.3390/lubricants13120552
Chicago/Turabian StyleHu, Jiafeng, Xiaojun Chen, Xianfeng Jiang, Zhaoxian Zheng, Yongkang Fang, and Chengxiong Lin. 2025. "Experimental Analysis of Catheter Push–Pull Forces: Effects of Vascular Curvature, Motion Speed, and Lumen Material" Lubricants 13, no. 12: 552. https://doi.org/10.3390/lubricants13120552
APA StyleHu, J., Chen, X., Jiang, X., Zheng, Z., Fang, Y., & Lin, C. (2025). Experimental Analysis of Catheter Push–Pull Forces: Effects of Vascular Curvature, Motion Speed, and Lumen Material. Lubricants, 13(12), 552. https://doi.org/10.3390/lubricants13120552






