Enhancing the Tribological Properties of Bearing Surfaces in Hip Arthroplasty by Shot-Peening the Metal Surface
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.1.1. Cobalt–Chromium Alloy
- -
- A hardness of 400 HV;
- -
- A density of 8.3 g/cm3;
- -
- A melting point of 1300 degrees Celsius.
2.1.2. Highly Cross-Linked Polyethylene (HxPE)
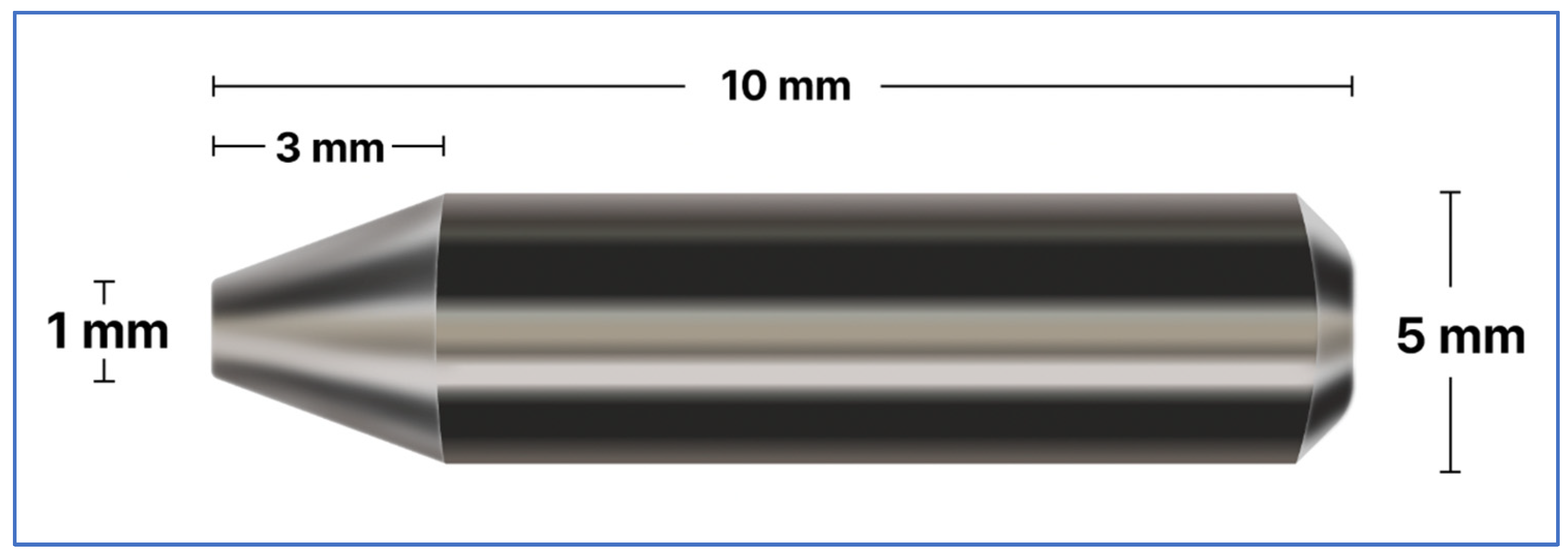
2.1.3. The Particles
2.2. Experimental Methods
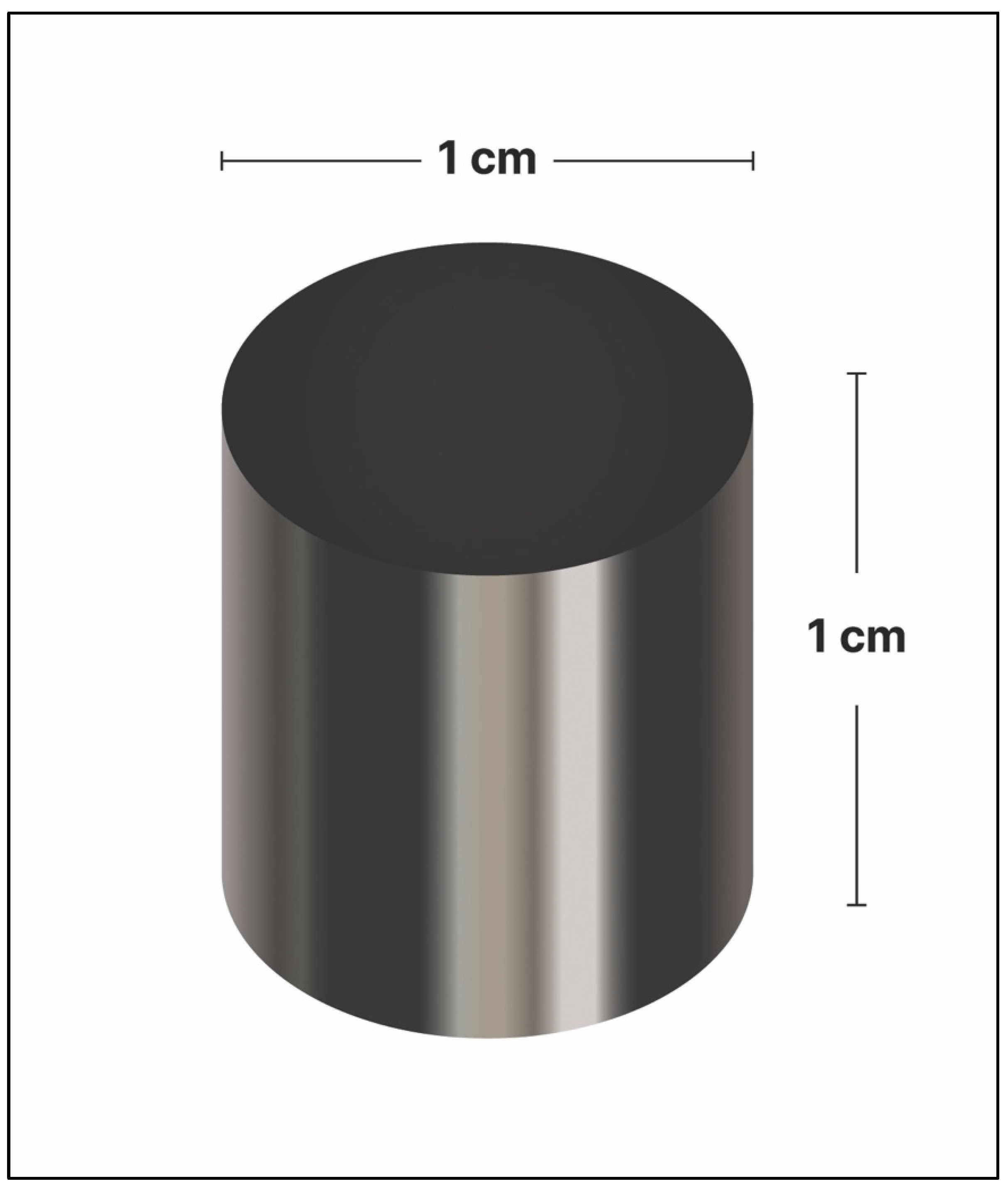
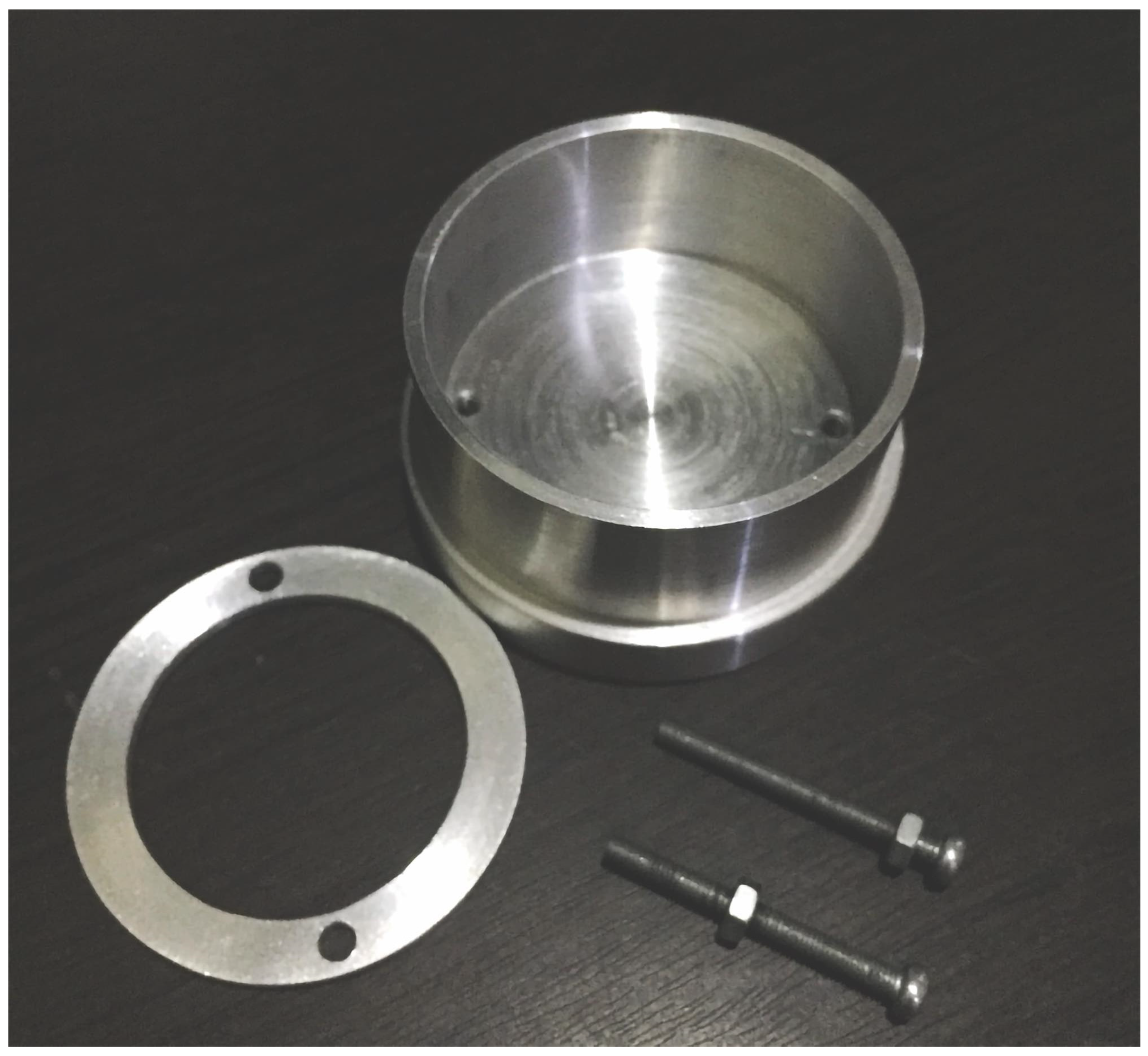
2.2.1. Workpiece Preparation
2.2.2. Surface Modification by Fine-Particle Shot Peening
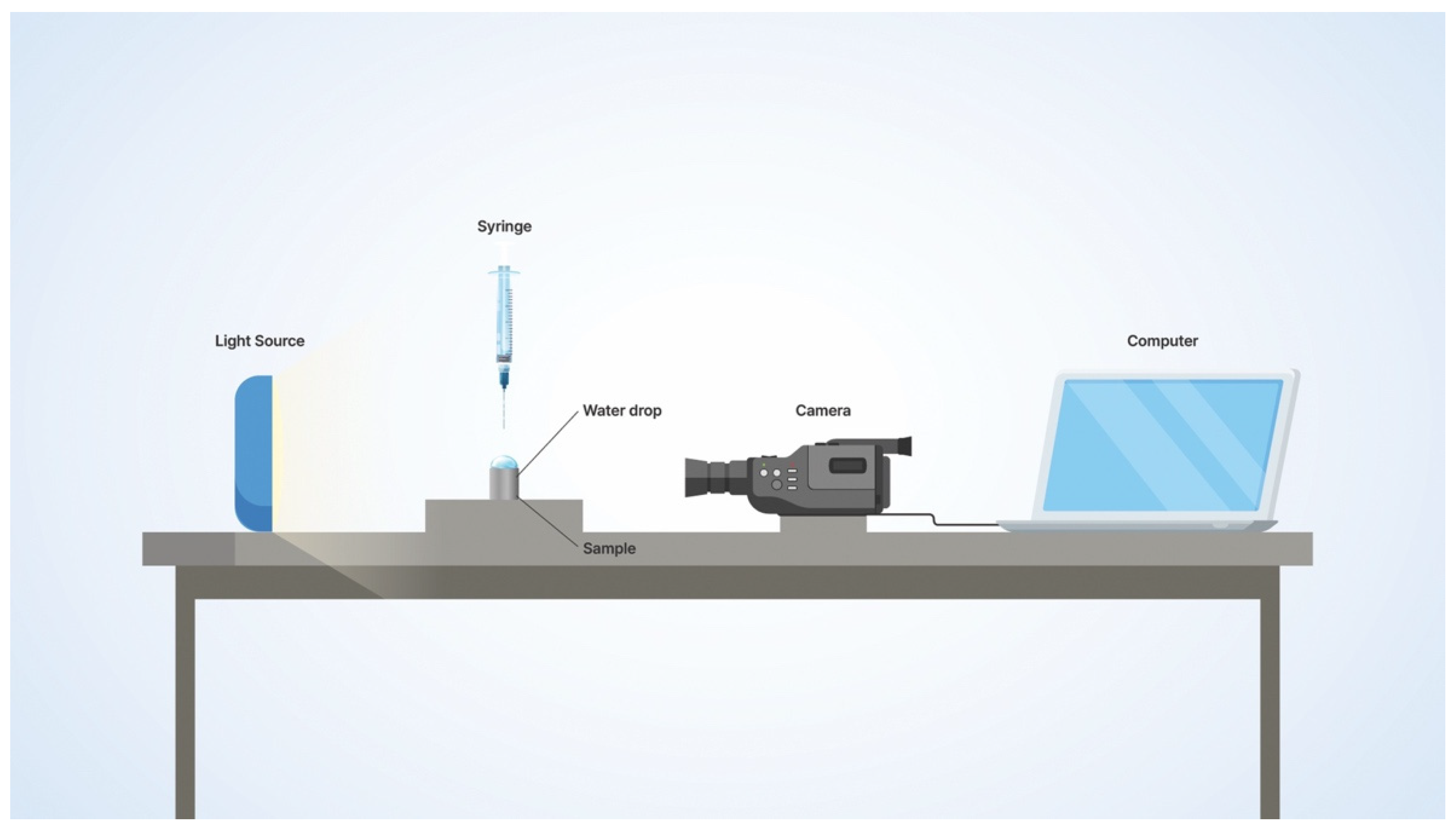
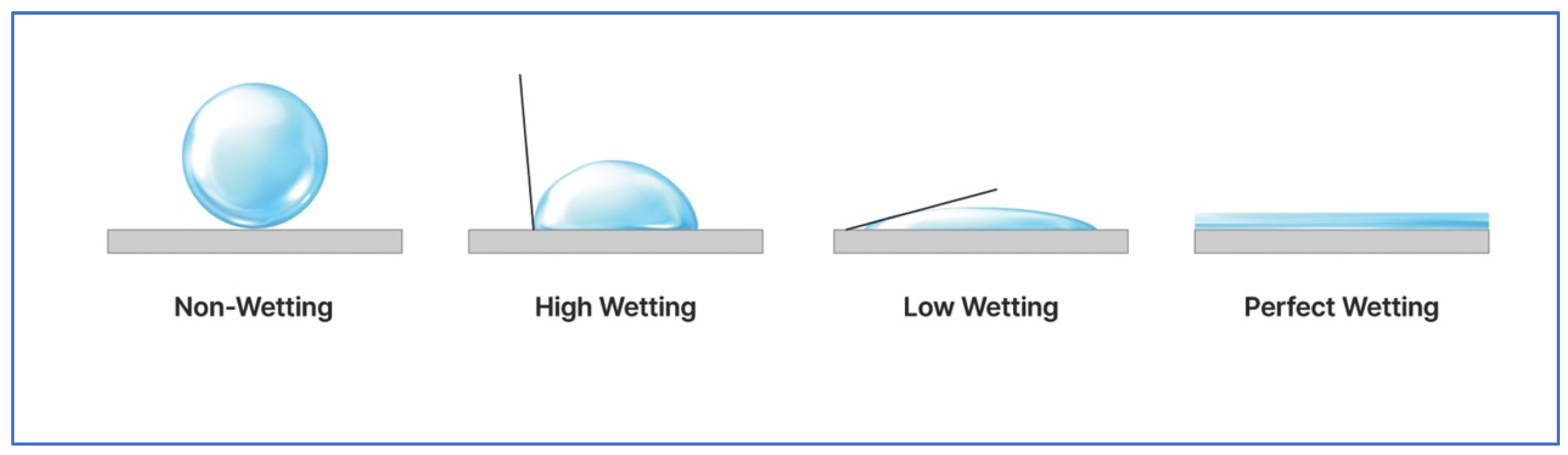
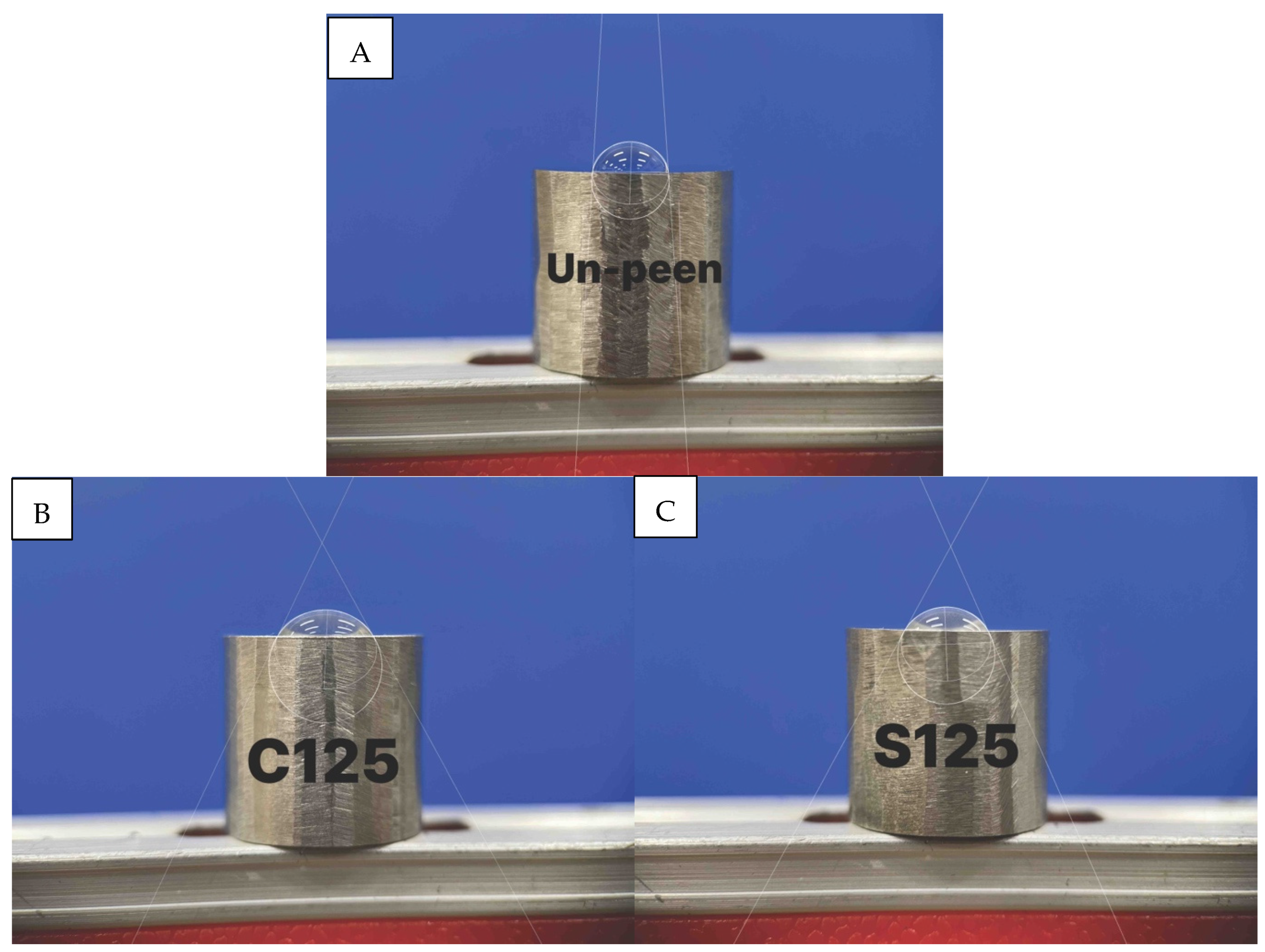
2.2.3. Wettability
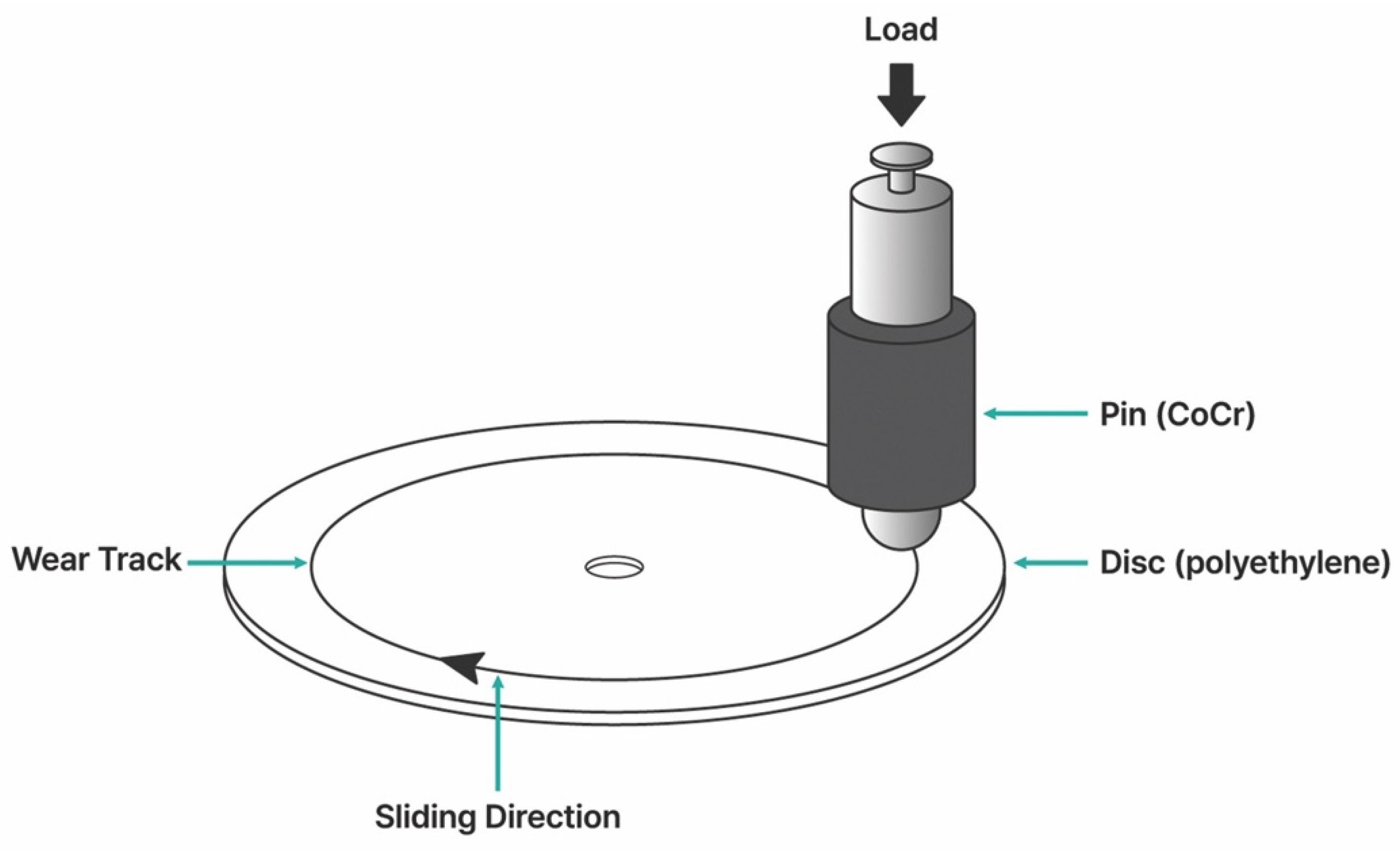
2.2.4. Tribology Test
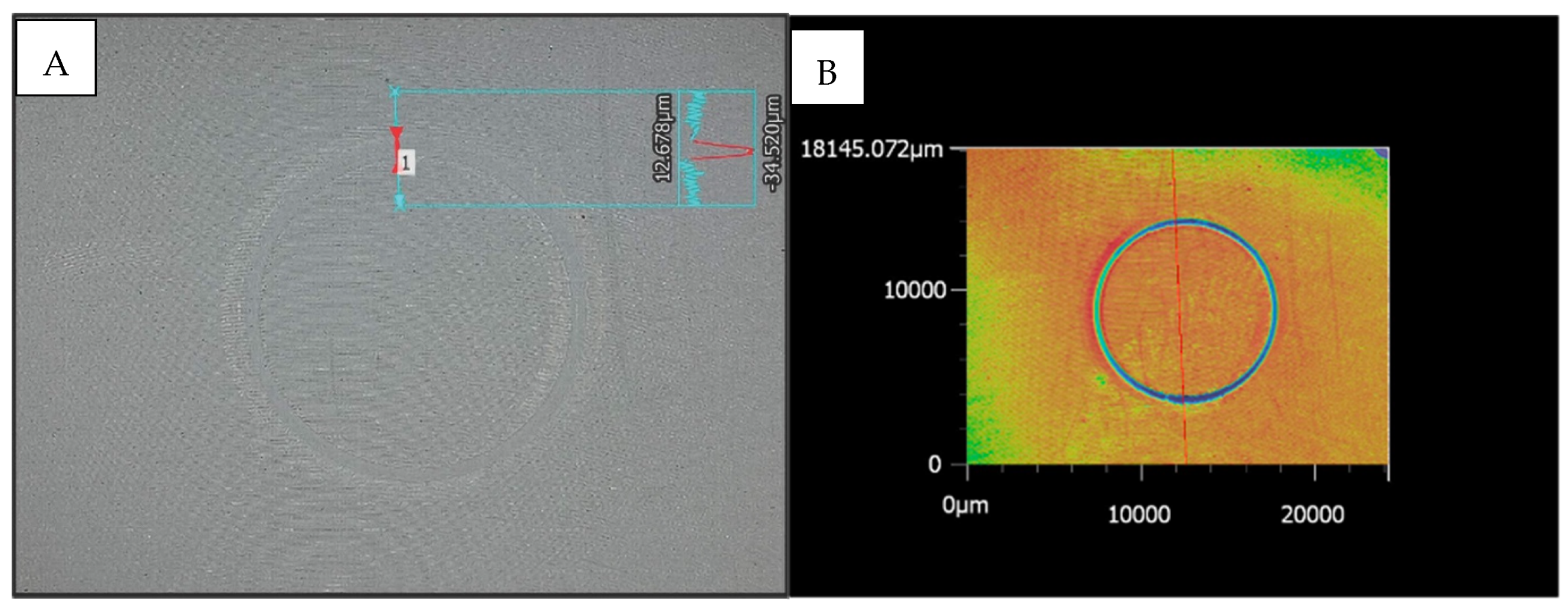
2.2.5. Wear Volume Measurement
3. Results and Discussion
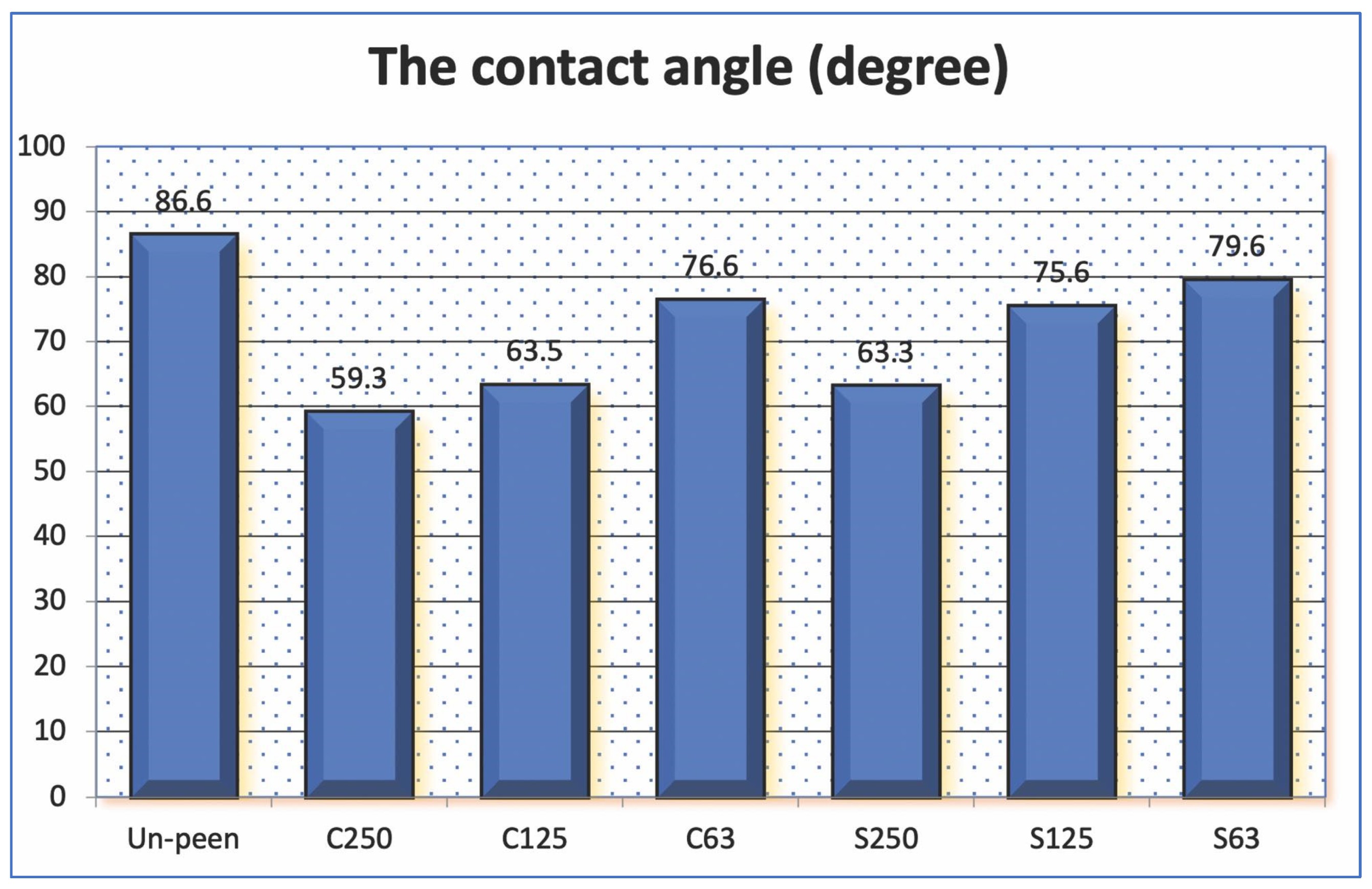
3.1. Wettability Test
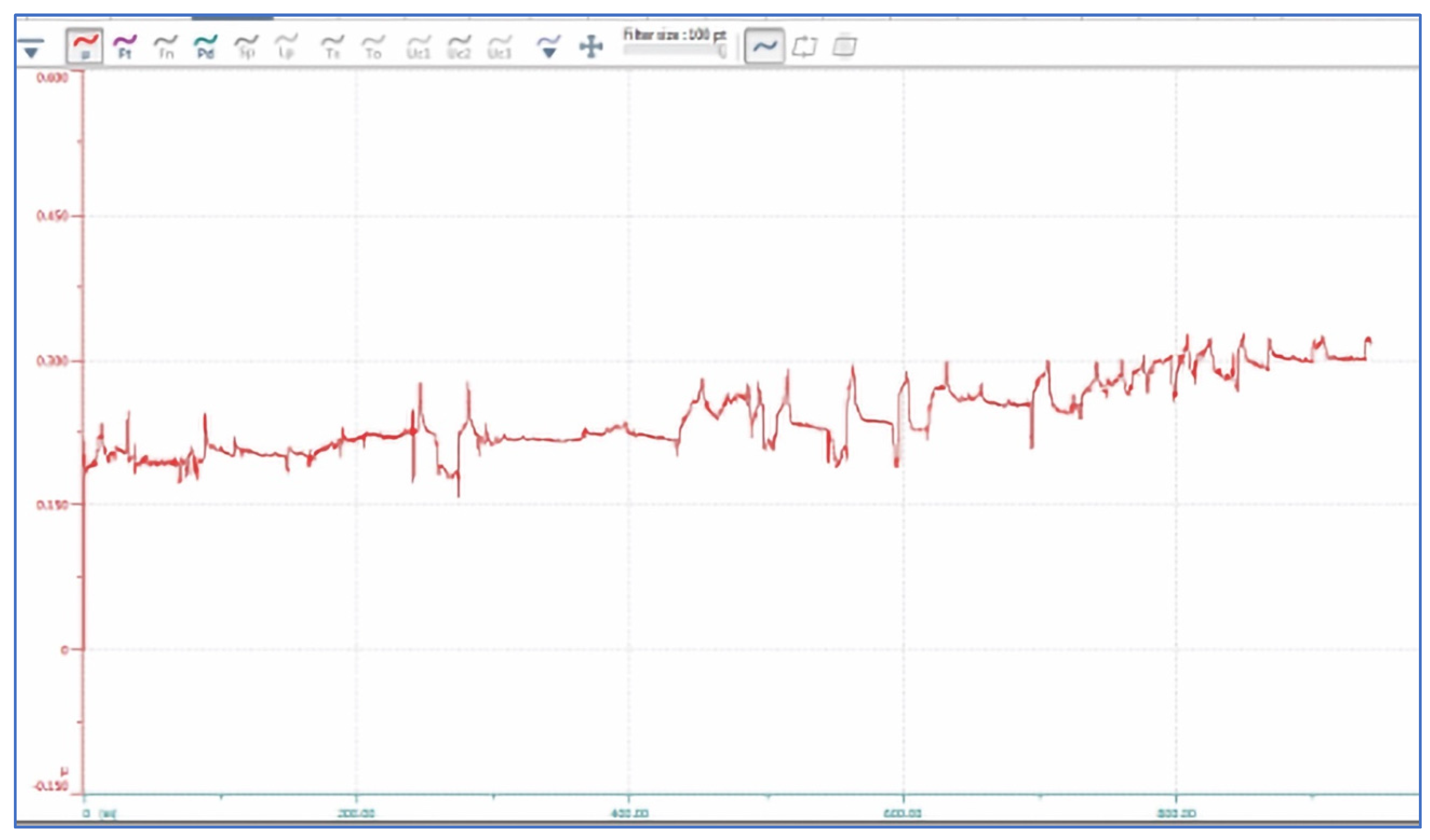
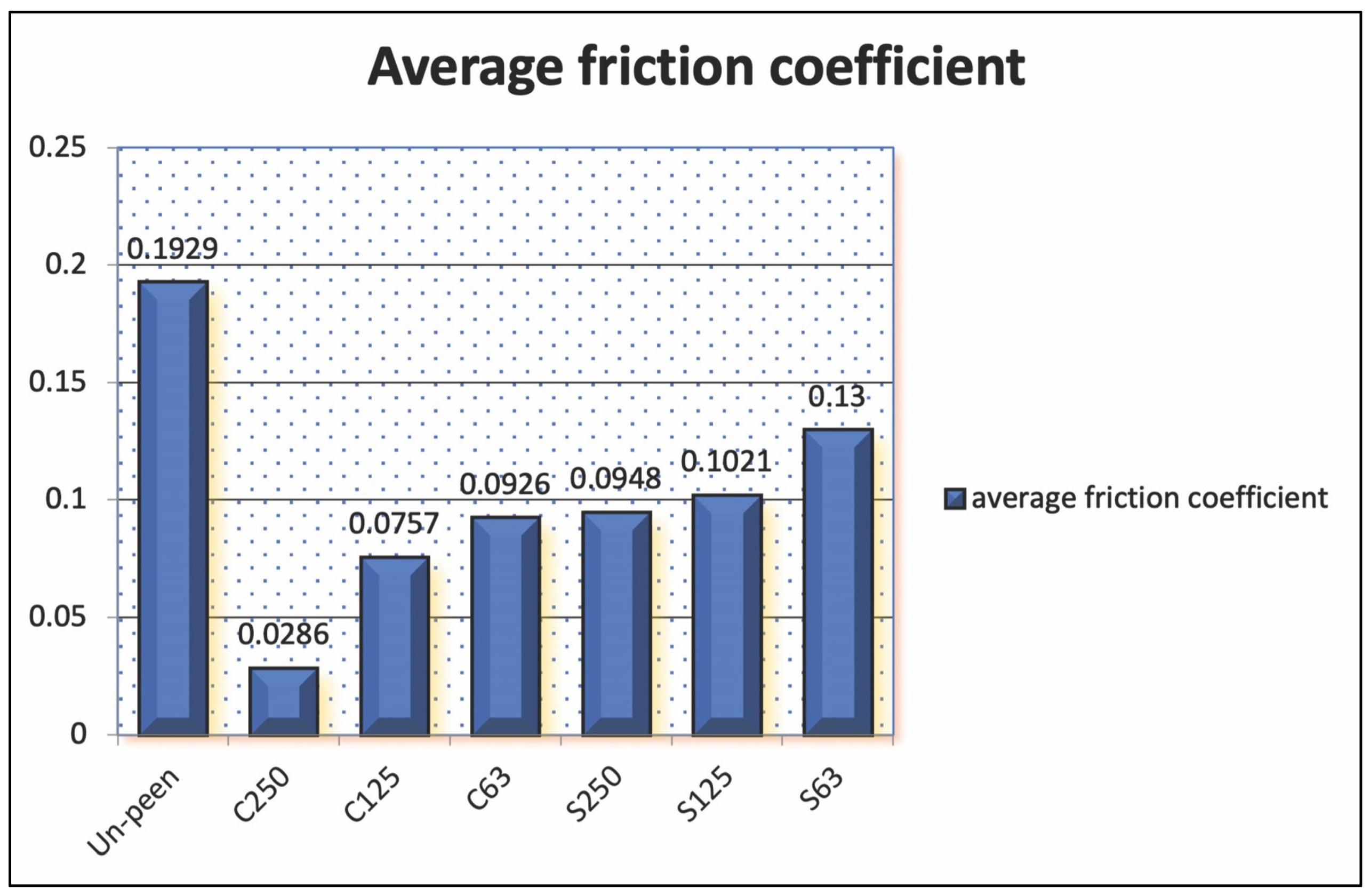
3.2. Tribology Test
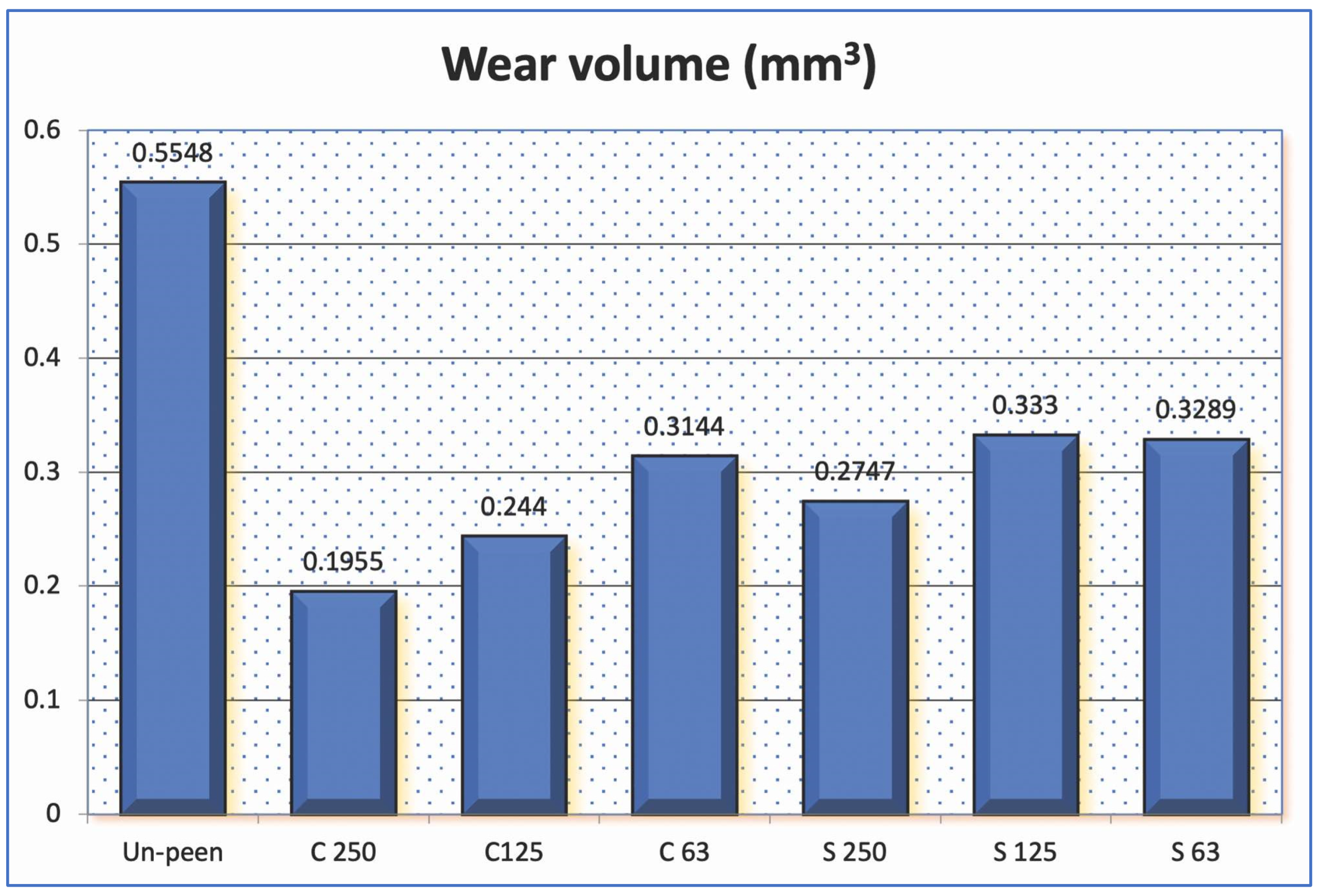
3.3. Wear Volume
4. Conclusions
- FSPS can increase the surface hardness in particles of any size [28], which may affect the tribological properties by enhancing the scratch resistance of the metal surface, thereby reducing the abrasive wear on the moving surface.
- FPSP can produce a smoother surface and reduce the sharpness of pits on the metal surface, thereby decreasing the coefficient of friction between the moving surfaces and reducing the wear process on polyethylene.
- FPSP can create small micro-dimples that act as pools of lubricant, enhancing the wettability of the metal surface and improving its lubrication properties.
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Bekker, S.; Bot, A.G.; Makarawung, D.; Neuhaus, V.; Ring, D. The National Hospital Discharge Survey and Nationwide Inpatient Sample: The databases used affect results in THA research. Clin. Orthop. Relat. 2014, 472, 3441–3449. [Google Scholar] [CrossRef] [PubMed]
- Marques, E.M.; Humphriss, R.; Welton, N.J.; Higgins, J.P.; Hollingworth, W.; Lopez, J.A.; Thom, H.; Hunt, L.P.; Blom, A.W.; Beswick, A.D. The choice between hip prosthetic bearing surfaces in total hip replacement: A protocol for a systematic review and network meta-analysis. Syst. Rev. 2016, 1, 5–19. [Google Scholar] [CrossRef] [PubMed]
- Karachalios, T.; Komnos, G.; Koutalos, A. Total hip arthroplasty: Survival and modes of failure. EFORT Open Rev. 2018, 3, 232–239. [Google Scholar] [CrossRef] [PubMed]
- Dreinhofer, K.E.; Dieppe, P.; Sturmer, T.; Grober-Gratz, D.; Floren, M.; Gunther, K.P.; Puhl, W.; Brenner, H. Indications for Total Hip Replacement: Comparison of Assessments of Orthopaedic Surgeons and Referring Physicians. Ann. Rheum. Dis. 2006, 65, 1346–1350. [Google Scholar] [CrossRef]
- Crawford, R.W.; Murray, D.W. Total Hip Replacement: Indications for Surgery and Risk Factors for Failure. Ann. Rheum. Dis. 1997, 56, 455–457. [Google Scholar] [CrossRef] [PubMed]
- Callaghan, J.; Forest, E.; Sporer, S.M.; Goetz, D.; Johnston, R.C. Total Hip Arthroplasty in the Young Adult. Clin. Orthop. 1997, 344, 257–262. [Google Scholar] [CrossRef]
- Kenney, C.; Dick, S.; Lea, J.; Liu, J.; Ebraheim, N.A. A Systematic Review of the Causes of Failure of Revision Total Hip Arthroplasty. J. Orthop. 2019, 16, 393–395. [Google Scholar] [CrossRef] [PubMed]
- Ulrich, S.D.; Seyler, T.M.; Bennett, D.; Delanois, R.E.; Saleh, K.J.; Thongtrangan, I.; Kuskowski, M.; Cheng, E.Y.; Sharkey, P.F.; Parvizi, J.; et al. Total Hip Arthroplasties: What Are the Reasons for Revision? Int. Orthop. 2008, 32, 597–604. [Google Scholar] [CrossRef]
- Sadoghi, P.; Liebensteiner, M.; Agreiter, M.; Leithner, A.; Bohler, N.; Labek, G. Revision Surgery After Total Joint Arthroplasty: A Complication-Based Analysis Using Worldwide Arthroplasty Registers. J. Arthroplast. 2003, 28, 1329–1332. [Google Scholar] [CrossRef]
- Zagra, L.; Gallazzi, E. Bearing Surfaces in Primary Total Hip Arthroplasty. EFORT Open Rev. 2018, 3, 217–224. [Google Scholar] [CrossRef]
- Heckmann, N.D.; Sivasundaram, L.; Stefl, M.D.; Kang, H.P.; Basler, E.T.; Lieberman, J.R. Total Hip Arthroplasty Bearing Surface Trends in the United States From 2007 to 2014: The Rise of Ceramic on Polyethylene. J. Arthroplast. 2014, 33, 1757–1763. [Google Scholar] [CrossRef] [PubMed]
- Kato, Y.; Omiya, M.; Hoshino, H. Modeling of particle behavior in Shot Peening Process. J. Mech. Eng. Autom. 2014, 4, 83–91. [Google Scholar]
- Zhi, J.; Jinjin, J. Influence Analysis of Shot Peening on Hot Forging Die. Int. J. Adv. Manuf. Technol. 2017, 90, 1779–1787. [Google Scholar]
- Kikuchi, S.; Nakamura, Y.; Nambu, K.; Ando, M. Effect of Shot Peening Using Ultra-Fine Particles on Fatigue Properties of 5056 Aluminum Alloy Under Rotating Bending. Mater. Sci. Eng. A 2016, 652, 279–286. [Google Scholar] [CrossRef]
- Choudhury, D.; Urban, F.; Vrbka, M.; Hartl, M.; Krupka, I. A Novel Tribological Study on DLC-Coated Micro-Dimpled Orthopedics Implant Interface. J. Mech. Behav. Biomed. Mater. 2015, 45, 121–131. [Google Scholar] [CrossRef] [PubMed]
- Choudhury, D.; Ay Ching, H.; Mamat, A.B.; Cizek, J.; Abu Osman, N.A.; Vrbka, M.; Hartl, H.; Krupka, I. Fabrication and Characterization of DLC Coated Microdimples on Hip Prosthesis Heads. J. Biomed. Mater. Res. Part B Appl. Biomater. 2015, 103, 1002–1012. [Google Scholar] [CrossRef] [PubMed]
- Choudhury, D.; Ghosh, S.; Ali, F.; Vrbka, M.; Hartl, M.; Krupka, I. The Influence of Surface Modification on Friction and Lubrication Mechanism Under a Bovine Serum– Lubricated Condition. Tribol. Trans. 2016, 59, 316–322. [Google Scholar] [CrossRef]
- Choudhury, D.; Vrbka, M.; Mamat, A.B.; Stavness, I.; Roy, C.K.; Mootanah, R.; Krupka, I. The Impact of Surface and Geometry on Coefficient of Friction of Artificial Hip Joints. J. Mech. Behav. Biomed. Mater. 2017, 72, 192–199. [Google Scholar] [CrossRef]
- Choudhury, D.; Rebenda, D.; Sasaki, S.; Hekrle, P.; Vrbka, M.; Zou, M. Enhanced Lubricant Film Formation Through Micro-Dimpled Hard-on-Hard Artificial Hip Joint: An In-Situ Observation of Dimple Shape Effects. J. Mech. Behav. Biomed. Mater. 2018, 81, 120–129. [Google Scholar] [CrossRef]
- Maryam, J.; David, P.F. Effects of shot peening parameters on gradient microstructure and mechanical properties of TRC AZ31. Mater. Charact. 2019, 148, 9–16. [Google Scholar]
- Ongtrakulkij, G.; Khantachawana, A.; Kondoh, K. Effects of media parameters on enhance ability of hardness and residual stress of Ti6Al4V by fine shot peening. Surf. Interfaces 2020, 18, 1004–1024. [Google Scholar] [CrossRef]
- Valkov, S.; Parshorov, S.; Andreeva, A.; Nikolova, M.; Petrov, P. Surface modification of CoCr-Mo alloys by electron-beam treatment. IOP Conf. Ser. Mater. Sci. Eng. 2021, 1056, 012008. [Google Scholar] [CrossRef]
- Jinxiong, H.; Wenwen, S.; Liwei, L.; Junwei, Q. Surface modification of plasma nitriding on AlxCoCrFeNi high-entropy alloys. J. Mater. Sci. Technol. 2020, 48, 140–145. [Google Scholar]
- Mertz, K.C.; Yang, J.; Chung, B.C.; Chen, X.; Mayfield, C.K.; Heckmann, N.D. Ceramic Femoral Heads Exhibit Lower Wear Rates Compared to Cobalt Chrome: A Meta-Analysis. J. Arthroplast. 2023, 38, 397–405. [Google Scholar] [CrossRef] [PubMed]
- Nho, J.H.; Park, J.S.; Song, U.S.; Kim, W.J.; Suh, Y.S. Ceramic head fracture in ceramic-on-polyethylene total hip arthroplasty. Yonsei Med. J. 2013, 54, 1550–1553. [Google Scholar] [CrossRef] [PubMed]
- Traina, F.; De Fine, M.; Di Martino, A.; Faldini, C. Fracture of ceramic bearing surfaces following total hip replacement: A systematic review. Biomed. Res. Int. 2013, 2013, 157247. [Google Scholar] [CrossRef] [PubMed]
- Sok, C.T.; Adrian, C.K.; Christopher, D.B.; James, L.; Howard, B.A. Tribocorrosion: Ceramic and Oxidized Zirconium vs Cobalt-Chromium Heads in Total Hip Arthroplasty. J. Arthroplast. 2016, 31, 2064–2071. [Google Scholar]
- Andrew, S.; Andrew, S.P.; Matthew, G.T.; Lyndsay, E.S.; Douglas, D.N.; Richard, W.M. A Ten-Year Radiostereometric Analysis of Polyethylene Wear Between Oxidized Zirconium and Cobalt Chrome Articulations in Total Hip Arthroplasty. J. Arthroplast. 2022, 37, 692–696. [Google Scholar]
- Malahias, M.A.; Atrey, A.; Gu, A.; Chytas, D.; Nikolaou, V.S.; Waddell, J.P. Is Oxidized Zirconium Femoral Head Superior to Other Bearing Types in Total Hip Arthroplasty? A Systematic Review and Meta-Analysis. J. Arthroplast. 2019, 34, 1844–1852. [Google Scholar] [CrossRef]
- Jarungvittayakon, C.; Khantachawana, A.; Sa-ngasoongsong, P. The Effect of Particle Type and Size on CoCr Surface Properties by Fine-Particle Shot Peening. Appl. Sci. 2023, 13, 5814. [Google Scholar] [CrossRef]
- Biemond, J.E.; Wolke, J.G. Cobalt-chromium alloys in fixed prosthodontics. Dent. Clin. 2017, 61, 797–814. [Google Scholar]
- Navarro, M.; Michiardi, A.; Castaño, O.; Planell, J.A. Biomaterials in orthopaedics. J. R. Soc. Interface 2008, 5, 1137–1158. [Google Scholar] [CrossRef]
- Hodgson, A.W.; Kurz, S.; Virtanen, S.; Fervel, V.; Olsson, C.O.; Mischler, S. Passive and transpassive behaviour of CoCrMo in simulated biological solutions. Electrochim. Acta 2014, 49, 2167–2178. [Google Scholar] [CrossRef]
- Xiang, D.D.; Wang, P.; Tan, X.P.; Chandra, S.; Wang, C.; Nai, M.L. Anisotropic microstructure and mechanical properties of additively manufactured Co–Cr–Mo alloy using selective electron beam melting for orthopedic implants. Mater. Sci. Eng. A Struct. Mater. 2019, 765, 138–270. [Google Scholar] [CrossRef]
- Igual, M.A.; Casabán, J.L. Influence of electrochemical potential on the tribocorrosion behaviour of high carbon CoCrMo biomedical alloy in simulated body fluids by electrochemical impedance spectroscopy. Electrochim. Acta 2010, 55, 5428–5439. [Google Scholar] [CrossRef]
- Fischer, A.; Shadanbaz, S.; Choudhury, N.R.; Dias, G.J. Wear and corrosion of cobalt and titanium alloys in orthopedic implant applications. J. Mech. Behav. Biomed. Mater. 2016, 63, 245–262. [Google Scholar]
- Young, T. An Essay on the Cohesion of Fluids. Philos. Trans. R. Soc. 1805, 95, 65–87. [Google Scholar] [CrossRef]
- Wang, S.; Liu, K.; Yao, X.; Jiang, L. Bioinspired Surfaces with Superwettability: New Insight on Theory, Design, and Applications. Chem. Rev. 2015, 115, 8230–8293. [Google Scholar] [CrossRef]
- Liu, K.; Yao, K.; Jiang, L. Recent Developments in Bio-Inspired Special Wettability. Chem. Soc. Rev. 2010, 39, 3240–3255. [Google Scholar] [CrossRef]
- Su, B.; Tian, Y.; Jiang, L. Bioinspired Interfaces with Superwettability: From Materials to Chemistry. J. Am. Chem. Soc. 2016, 138, 1727–1748. [Google Scholar] [CrossRef]
- Ranabothu, S.R.; Karnezis, C.; Dai, L.L. Dynamic Wetting: Hydrodynamic or Molecular-Kinetic? J. Colloid. Interface Sci. 2005, 288, 213–221. [Google Scholar] [CrossRef] [PubMed]
- Baykal, D.; Siskey, R.S.; Haider, H.; Saikko, V.; Ahlroos, T.; Kurtz, S.M. Advances in Tribological Testing of Artificial Joint Biomaterials Using Multidirectional Pin-on-Disk Testers. J. Mech. Behav. Biomed. Mater. 2014, 31, 117–134. [Google Scholar] [CrossRef] [PubMed]
- Borjali, A.; Monson, K.; Raeymaekers, B. Predicting the Polyethylene Wear Rate in Pin-on-Disc Experiments in the Context of Prosthetic Hip Implants: Deriving a Data-Driven Model Using Machine Learning Methods. Tribol. Int. 2019, 133, 101–110. [Google Scholar] [CrossRef] [PubMed]
- Kurtz, S.M.; Gawel, H.A.; Patel, J.D. History and Systematic Review of Wear and Osteolysis Outcomes for First-Generation Highly Crosslinked Polyethylene. Clin. Orthop. Relat. Res. 2011, 469, 2262–2277. [Google Scholar] [CrossRef] [PubMed]
- Aherwar, A.; Patnaik, A.; Bahraminasab, M.; Singh, A. Preliminary Evaluations on Development of New Materials for Hip Joint Femoral Head. Proc. Inst. Mech. Eng. L J. Mater. Des. Appl. 2019, 233, 885–899. [Google Scholar] [CrossRef]
- Fu, P.; Chu, R.; Xu, Z.; Ding, G.; Jiang, C. Relation of hardness with FWHM and residual stress of GCr15 steel after shot peening. Appl. Surf. Sci. 2018, 431, 165–169. [Google Scholar] [CrossRef]

| Cobalt (%) | Chromium (%) | Mo (%) | C (%) |
|---|---|---|---|
| 60–62 | 29–31 | 5–6 | 0.55–0.65 |
| Particle Code | Particle Type | Particle Size (μm) |
|---|---|---|
| S63 | Silica | 63–106 |
| S125 | Silica | 125–180 |
| S250 | Silica | 250–355 |
| C63 | Ceramic | 63–125 |
| C125 | Ceramic | 125–250 |
| C250 | Ceramic | 250–425 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jarungvittayakon, C.; Khantachawana, A.; Sa-ngasoongsong, P. Enhancing the Tribological Properties of Bearing Surfaces in Hip Arthroplasty by Shot-Peening the Metal Surface. Lubricants 2024, 12, 278. https://doi.org/10.3390/lubricants12080278
Jarungvittayakon C, Khantachawana A, Sa-ngasoongsong P. Enhancing the Tribological Properties of Bearing Surfaces in Hip Arthroplasty by Shot-Peening the Metal Surface. Lubricants. 2024; 12(8):278. https://doi.org/10.3390/lubricants12080278
Chicago/Turabian StyleJarungvittayakon, Chavarat, Anak Khantachawana, and Paphon Sa-ngasoongsong. 2024. "Enhancing the Tribological Properties of Bearing Surfaces in Hip Arthroplasty by Shot-Peening the Metal Surface" Lubricants 12, no. 8: 278. https://doi.org/10.3390/lubricants12080278
APA StyleJarungvittayakon, C., Khantachawana, A., & Sa-ngasoongsong, P. (2024). Enhancing the Tribological Properties of Bearing Surfaces in Hip Arthroplasty by Shot-Peening the Metal Surface. Lubricants, 12(8), 278. https://doi.org/10.3390/lubricants12080278





