From Consultation to Collaboration: A Patient-Centered Approach to Shingles Pain and Postherpetic Neuralgia Management
Abstract
1. Introduction
2. Methods
2.1. Development of the Shared Decision-Making (SDM) Forms
- Introduction to acute neuralgia from herpes zoster and postherpetic neuralgia–providing essential information about the conditions.
- Introduction and comparison of relevant interventional treatments—covering options such as local steroid injection, pulsed radiofrequency, paravertebral block, and peripheral nerve stimulation.
- Patient considerations—addressing factors such as cost, potential complications, and the possibility of hospitalization.
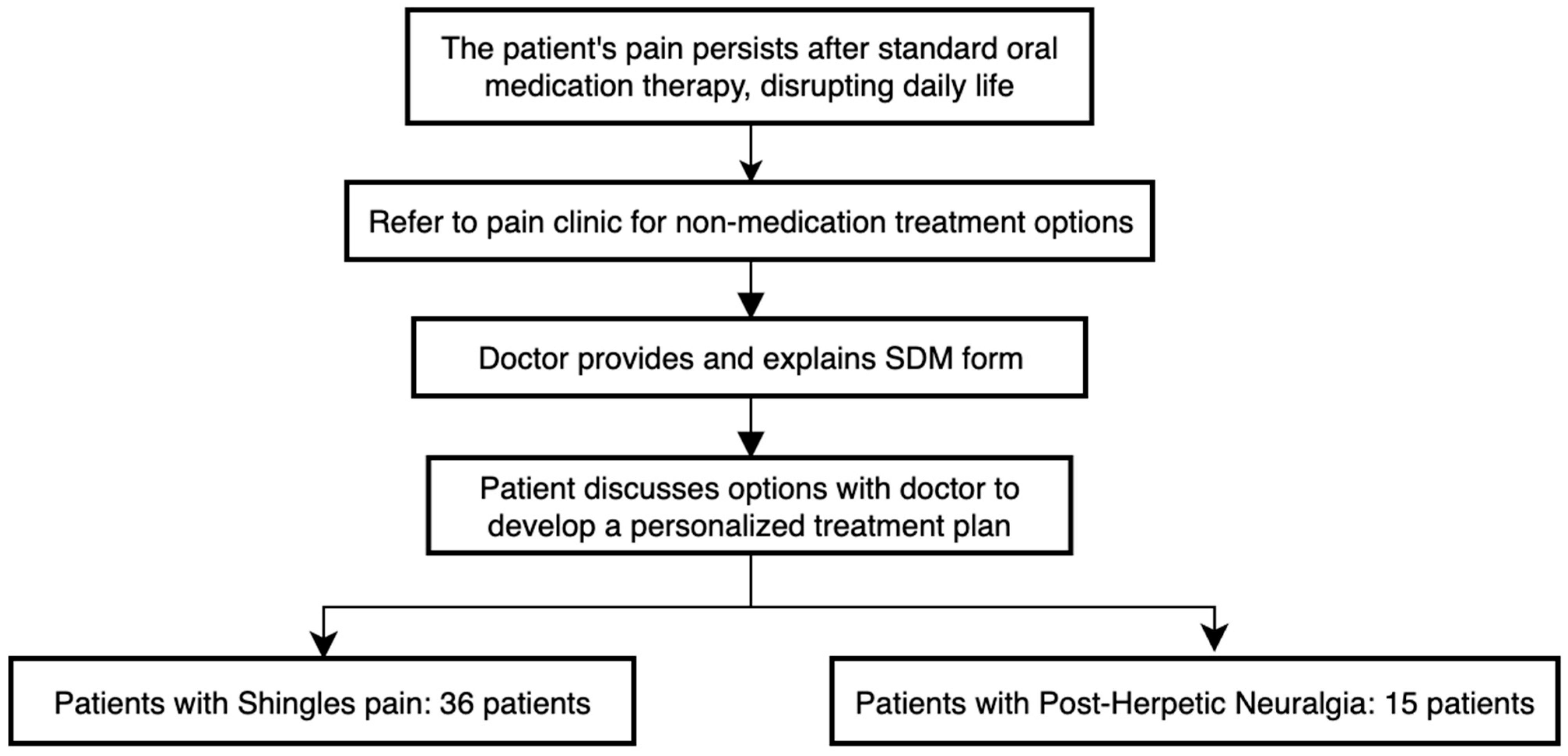
2.2. Enrollment
2.3. Consistency Among Staff
2.4. Outcome Measures
2.5. Assessment
2.6. Statistical Analysis
3. Results
3.1. Demographic Data of the Patients
3.2. Patients with Shingles Pain
3.3. Patients with Postherpetic Neuralgia
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| PHN | postherpetic neuralgia |
| SDM | shared decision making |
| NRS | numerical rating scale |
References
- Saguil, A.; Kane, S.; Mercado, M.; Lauters, R. Herpes Zoster and Postherpetic Neuralgia: Prevention and Management. Am. Fam. Physician 2017, 96, 656–663. [Google Scholar] [PubMed]
- Lin, K.Y.; Wang, C.H.; Su, L.Y.; Lin, I.F.; Liu, C.W.; Wu, P.F.; Tsai, W.C.; Chang, C.N.; Hung, M.C.; Huang, C.H.; et al. Recommendations and guidance for herpes zoster vaccination for adults in Taiwan. J. Microbiol. Immunol. Infect. 2024, 57, 669–684. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.H.; Huang, L.M.; Chang, I.S.; Tsai, F.Y.; Lu, C.Y.; Shao, P.L.; Chang, L.Y. Disease burden and epidemiology of herpes zoster in pre-vaccine Taiwan. Vaccine 2010, 28, 1217–1220. [Google Scholar] [CrossRef] [PubMed]
- John, A.R.; Canaday, D.H. Herpes Zoster in the Older Adult. Infect. Dis. Clin. North Am. 2017, 31, 811–826. [Google Scholar] [CrossRef]
- Johnson, R.W.; Rice, A.S. Clinical practice. Postherpetic neuralgia. N. Engl. J. Med. 2014, 371, 1526–1533. [Google Scholar] [CrossRef]
- Nahm, F.S.; Kim, S.H.; Kim, H.S.; Shin, J.W.; Yoo, S.H.; Yoon, M.H.; Lee, D.I.; Lee, Y.W.; Lee, J.H.; Jeon, Y.H.; et al. Survey on the treatment of postherpetic neuralgia in Korea; multicenter study of 1414 patients. Korean J. Pain 2013, 26, 21–26. [Google Scholar] [CrossRef]
- Lin, C.S.; Lin, Y.C.; Lao, H.C.; Chen, C.C. Interventional Treatments for Postherpetic Neuralgia: A Systematic Review. Pain Physician 2019, 22, 209–228. [Google Scholar] [CrossRef]
- Wendler, D. The Theory and Practice of Surrogate Decision-Making. Hastings Cent. Rep. 2017, 47, 29–31. [Google Scholar] [CrossRef]
- Kunneman, M.; Montori, V.M.; Castaneda-Guarderas, A.; Hess, E.P. What Is Shared Decision Making? (and What It Is Not). Acad. Emerg. Med. 2016, 23, 1320–1324. [Google Scholar] [CrossRef]
- Marcum, Z.A.; Jain, P.; Embry, A.; Arakaki, B.; Estevez, I.; Viscidi, E. Incidence of Herpes Zoster and Postherpetic Neuralgia and Herpes Zoster Vaccination Uptake in a US Administrative Claims Database. Open Forum Infect. Dis. 2024, 11, ofae211. [Google Scholar] [CrossRef]
- Kawai, K.; Yawn, B.P.; Wollan, P.; Harpaz, R. Increasing Incidence of Herpes Zoster Over a 60-year Period From a Population-based Study. Clin. Infect. Dis. 2016, 63, 221–226. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J.I. Herpes Zoster. N. Engl. J. Med. 2013, 369, 255–263. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Abrahamson, P.E.; Ke, Y.; Ong, C.R.; Parikh, R.; Shantakumar, S. A systematic literature review of the epidemiology and burden of herpes zoster in selected locales in Asia Pacific. Hum. Vaccines Immunother. 2024, 20, 2344983. [Google Scholar] [CrossRef] [PubMed]
- Chiu, H.H.; Chang, S.L.; Cheng, H.M.; Chao, T.F.; Lin, Y.J.; Lo, L.W.; Hu, Y.F.; Chung, F.P.; Liao, J.N.; Tuan, T.C.; et al. Shared decision making for anticoagulation reduces anxiety and improves adherence in patients with atrial fibrillation. BMC Med. Inform. Decis. Mak. 2023, 23, 163. [Google Scholar] [CrossRef]
- Cheng, H.-M.; Chang, H.-D.; Huang, H.-C.; Hsu, H.-F.; Lee, C.-Y.; Sheu, M.-J.; Chiu, H.-h. Clinical efficiency analysis of share decision making in the atrial fibrillation patients. Int. J. Stud. Nurs. 2020, 5, 17. [Google Scholar] [CrossRef]
- Bolson, R.; Lalka, A.; Korrell, H.; Sibbel, S.E.; Bartels, K. Shared Decision-Making Tool for Opioid Prescribing After Ambulatory Orthopedic Surgery in Veterans: A Randomized Controlled Clinical Trial. J. Hand Surg. Glob. Online 2022, 4, 196–200. [Google Scholar] [CrossRef]
- An, K.; Wu, Z.; Qiu, Y.; Pan, M.; Zhang, L.; An, Z.; Li, S. Shared decision making in sarcopenia treatment. Front. Public Health 2023, 11, 1296112. [Google Scholar] [CrossRef]
- Faiman, B.; Tariman, J.D. Shared Decision Making: Improving Patient Outcomes by Understanding the Benefits of and Barriers to Effective Communication. Clin. J. Oncol. Nurs. 2019, 23, 540–542. [Google Scholar] [CrossRef]
- Von Korff, M.; Katon, W.; Rutter, C.; Ludman, E.; Simon, G.; Lin, E.; Bush, T. Effect on disability outcomes of a depression relapse prevention program. Psychosom. Med. 2003, 65, 938–943. [Google Scholar] [CrossRef]
- Ludman, E.; Katon, W.; Bush, T.; Rutter, C.; Lin, E.; Simon, G.; Von Korff, M.; Walker, E. Behavioural factors associated with symptom outcomes in a primary care-based depression prevention intervention trial. Psychol. Med. 2003, 33, 1061–1070. [Google Scholar] [CrossRef]
- van Roosmalen, M.S.; Stalmeier, P.F.; Verhoef, L.C.; Hoekstra-Weebers, J.E.; Oosterwijk, J.C.; Hoogerbrugge, N.; Moog, U.; van Daal, W.A. Randomized trial of a shared decision-making intervention consisting of trade-offs and individualized treatment information for BRCA1/2 mutation carriers. J. Clin. Oncol. 2004, 22, 3293–3301. [Google Scholar] [CrossRef] [PubMed]
- Brown, T.T.; Lee, J.; Markarian, S. The causal impact of shared decision making on pain outcomes: Gender matters. Soc. Sci. Med. 2024, 355, 117132. [Google Scholar] [CrossRef] [PubMed]
- Smith, S.K.; Dixon, A.; Trevena, L.; Nutbeam, D.; McCaffery, K.J. Exploring patient involvement in healthcare decision making across different education and functional health literacy groups. Soc. Sci. Med. 2009, 69, 1805–1812. [Google Scholar] [CrossRef]
- Kikuchi, R.; Kingston, P.; Hao, A.; Sadrolashrafi, K.; Yamamoto, R.K.; Tolson, H.; Bilimoria, S.N.; Guo, L.; Yee, D.; Ochoa, M.T.; et al. Shared decision-making in psoriasis care: Evaluation of how patients’ perception of clinicians’ delivery of care changes by age and sex. PLoS ONE 2024, 19, e0303058. [Google Scholar] [CrossRef]
| Characteristic | SHINGLES PAIN | PHN |
|---|---|---|
| (N = 36) | (N = 15) | |
| Age, median (QD) | 71.5 (59.5–75.0) | 75.0 (70.5–81.0) |
| Sex, n (%) | 36 | 15 |
| Male | 17 (47.2) | 8 (53.3) |
| Female | 19 (52.8) | 7 (46.7) |
| Race, n (%) | ||
| Asian | 36(100) | 15 (100) |
| Duration of pain, median (QD) | 55.5 (35.0–76.0, days) | 22.0 (14.0–40.0, months) |
| The distribution of lesions, n (%) | ||
| C spine | 11 (28.2) | 1 (5.8) |
| T spine | 22 (56.4) | 11 (64.7) |
| L spine | 3 (7.6) | 2 (11.7) |
| S spine | 3 (7.6) | 3 (17.6) |
| Comorbidities, n (%) | ||
| Type 2 diabetes mellitus | 5 (13.9) | 3 (20.0) |
| Hypertension | 9 (25.0) | 2 (13.3) |
| Chronic kidney disease | 2 (5.6) | 2 (13.3) |
| Hyperlipidemia | 7 (19.4) | 4 (26.7) |
| Cardiovascular disease | 3 (8.3) | 2 (13.3) |
| Cancer | 7 (19.4) | 2 (13.3) |
| Group | Shingles Pain | PHN |
|---|---|---|
| (N = 36) | (N = 15) | |
| Treatment received after SDM completion number (%) | ||
| Oral medications/local lidocaine patch | 17 (47.2) | 11 (73.3) |
| Subcutaneous steroid injection | 11 (30.6) | 2 (13.3) |
| Nerve block | 6 (16.7) | 2 (13.3) |
| Pulsed radiofrequency | 1 (2.8) | 0 (0.0) |
| Treatment received after SDM number (%) | ||
| Oral medications/local lidocaine patch ¶ | 36 (100.0) | 15 (100.0) |
| Subcutaneous steroid injection | 13 (36.1) | 2 (13.0) |
| Nerve block | 12 (33.3) | 6 (40.0) |
| Pulsed radiofrequency | 3 (8.3) | 5 (33.3) |
| Receiving more than one intervention therapy | 10 (27.8) | 3 (20.0) |
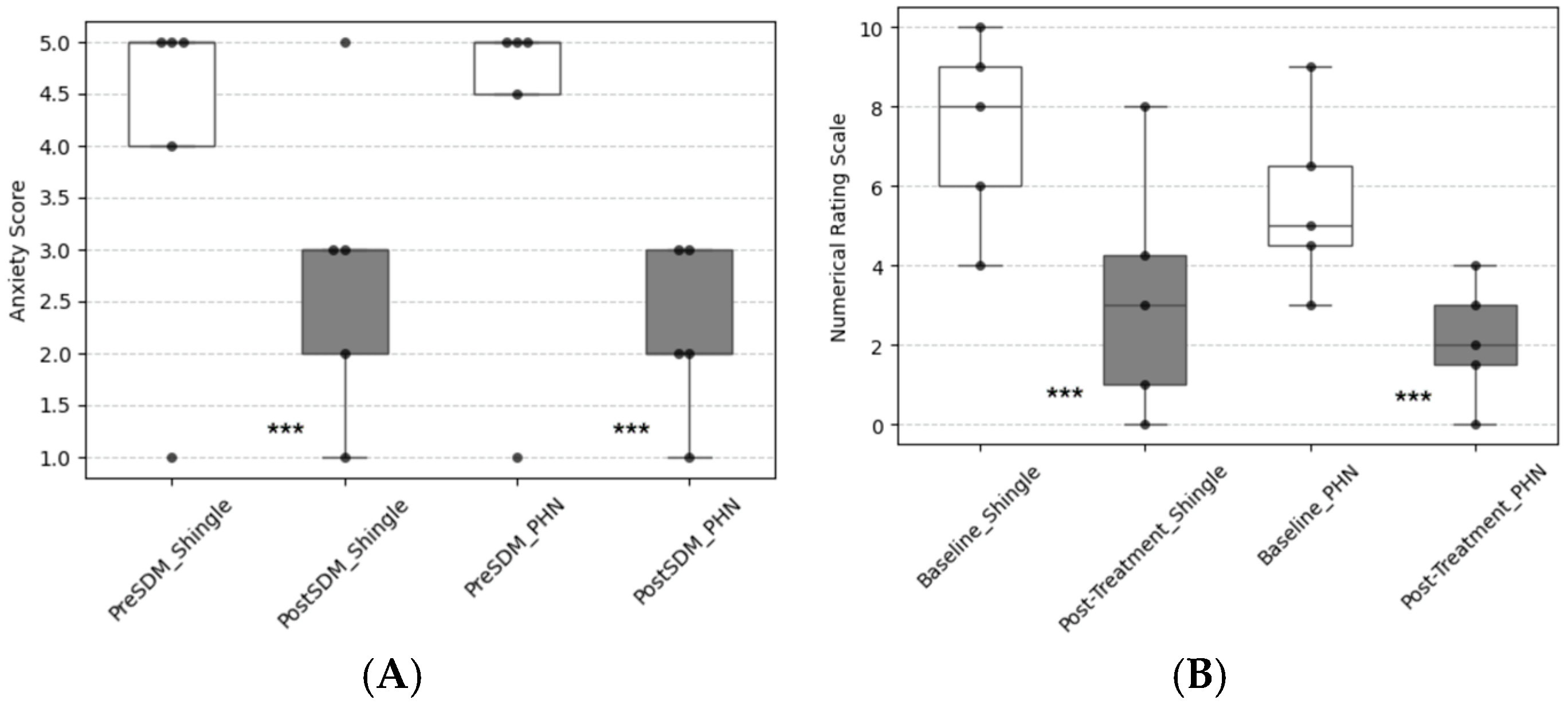
| Primary outcome, median(QD) | ||
| Anxiety level (before) | 5.0 (3.5–5.0) | 5.0 (4.0–5.0) |
| Anxiety level (after) | 3.0 (2.0–3.0) | 2.0 (2.0–3.0) |
| Secondary outcomes, median(QD) | ||
| NRS (before) | 8.0 (6.0–9.0) | 5.0 (4.0–8.0) |
| NRS (after) | 3.0 (1.0–6.5) | 2.0 (1.0–3.0) |
| Patient considerations | ||
| Waiting time | 5.0 (3.0–5.0) | 5.0 (3.0–5.0) |
| Cost | 5.0 (3.0–5.0) | 5.0 (4.5–5.0) |
| Complication rate | 5.0 (5.0–5.0) | 5.0 (4.5–5.0) |
| Number and frequency of treatments | 2.0 (5.0–5.0) | 5.0 (4.5–5.0) |
| Hospitalization | 3.0 (5.0–5.0) | 5.0 (4.5–5.0) |
| Continuity of treatment | None | 5.0 (4.5–5.0) |
| The helpfulness scores for participation | 5.0 (4.0–5.0) | 5.0 (4.5–5.0) |
| The helpfulness scores for knowing | 5.0 (4.0–5.0) | 5.0 (4.0–5.0) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, Y.-T.; Lao, H.-C.; Kao, S.-C.; Lin, Y.-C.; Yang, Y.-W.; Li, Y.-H.; Chen, Y.-J. From Consultation to Collaboration: A Patient-Centered Approach to Shingles Pain and Postherpetic Neuralgia Management. J. Pers. Med. 2025, 15, 191. https://doi.org/10.3390/jpm15050191
Wu Y-T, Lao H-C, Kao S-C, Lin Y-C, Yang Y-W, Li Y-H, Chen Y-J. From Consultation to Collaboration: A Patient-Centered Approach to Shingles Pain and Postherpetic Neuralgia Management. Journal of Personalized Medicine. 2025; 15(5):191. https://doi.org/10.3390/jpm15050191
Chicago/Turabian StyleWu, Yin-Tse, Hsuan-Chih Lao, Sheng-Chin Kao, Ying-Chun Lin, Ying-Wei Yang, Ying-Hsin Li, and Yi-Jun Chen. 2025. "From Consultation to Collaboration: A Patient-Centered Approach to Shingles Pain and Postherpetic Neuralgia Management" Journal of Personalized Medicine 15, no. 5: 191. https://doi.org/10.3390/jpm15050191
APA StyleWu, Y.-T., Lao, H.-C., Kao, S.-C., Lin, Y.-C., Yang, Y.-W., Li, Y.-H., & Chen, Y.-J. (2025). From Consultation to Collaboration: A Patient-Centered Approach to Shingles Pain and Postherpetic Neuralgia Management. Journal of Personalized Medicine, 15(5), 191. https://doi.org/10.3390/jpm15050191







