Measuring Nasal Airway Resistance to Personalize Surgery for Nasal Obstruction in OSA Patients
Abstract
1. Introduction
2. Materials and Methods
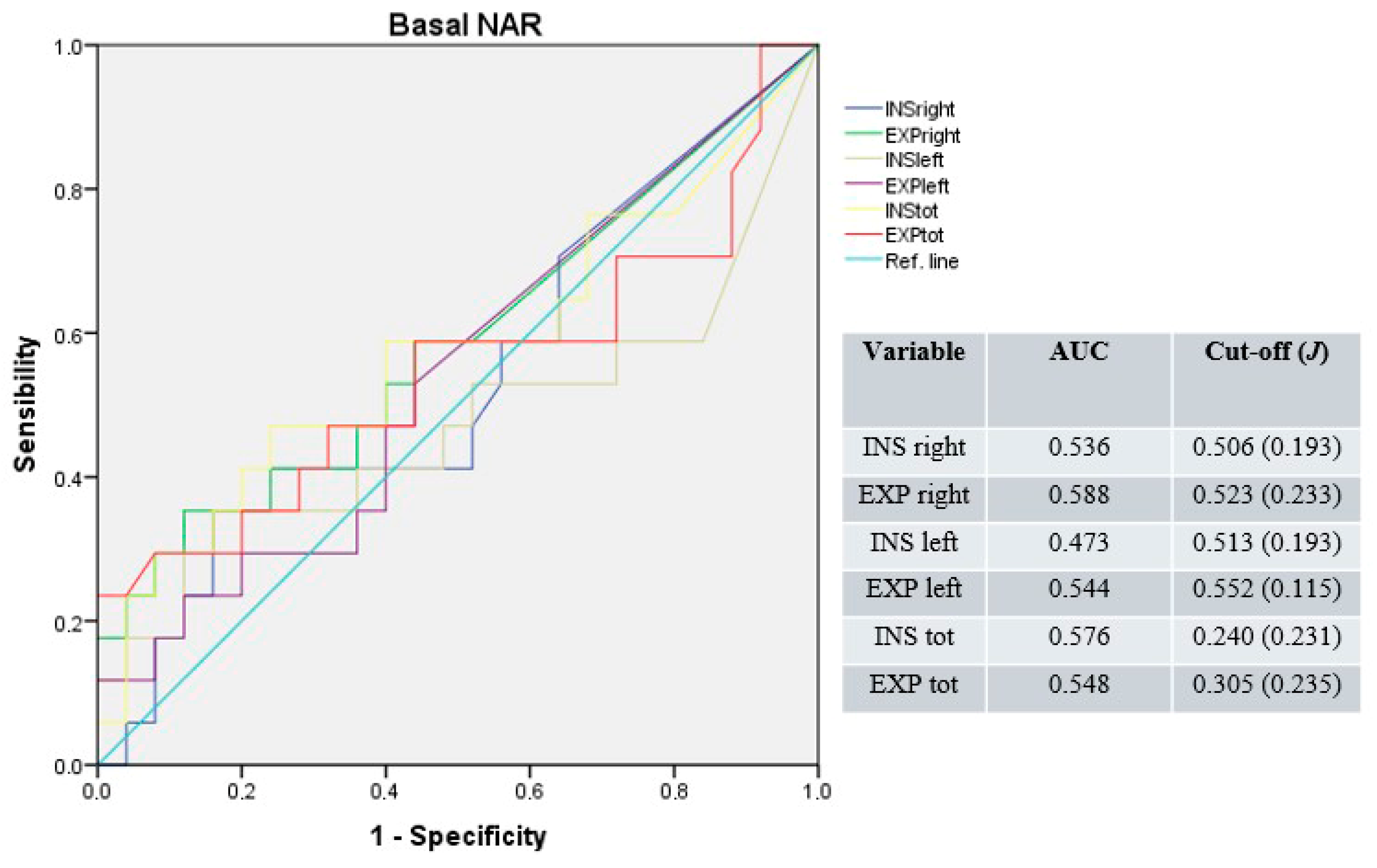
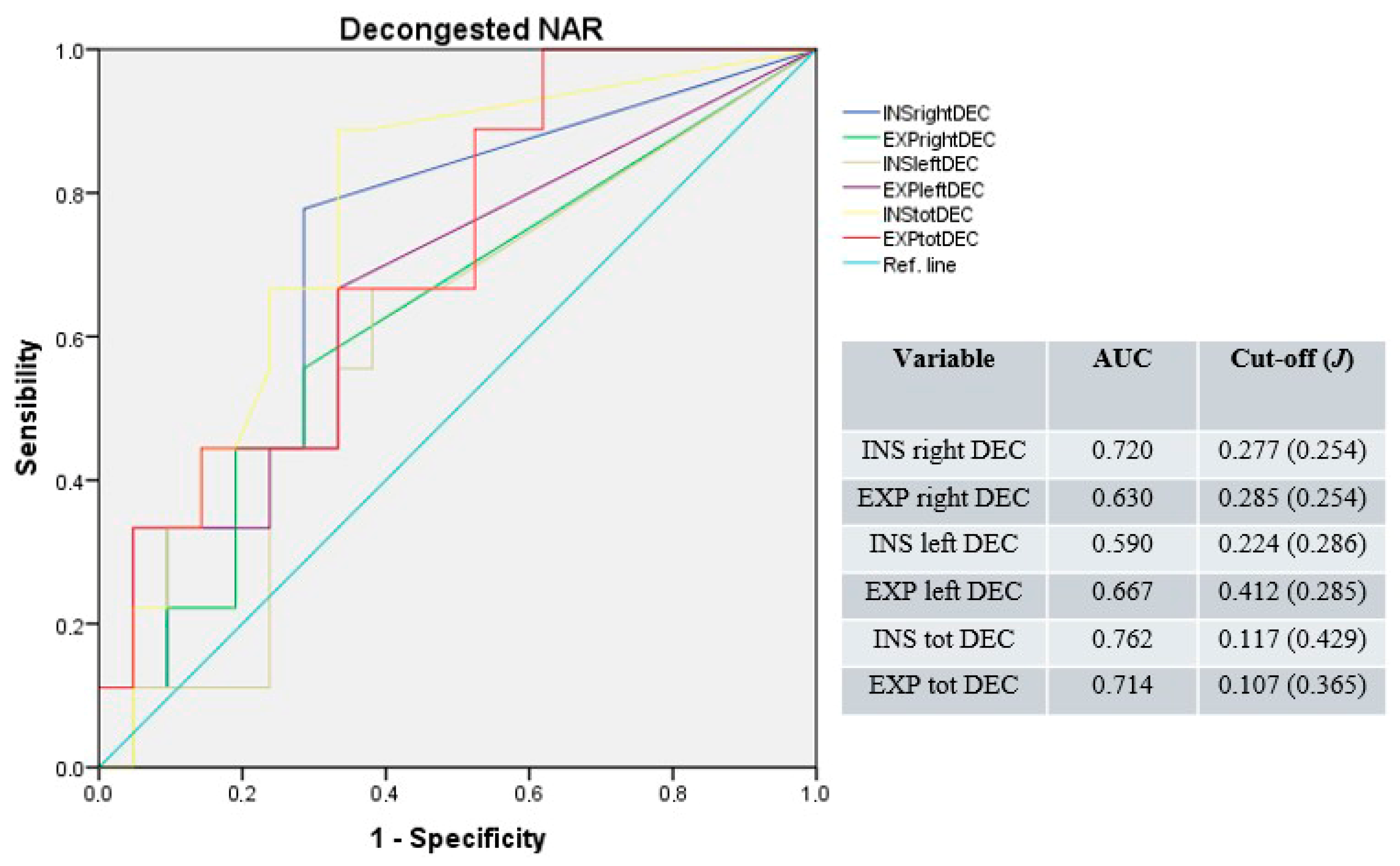
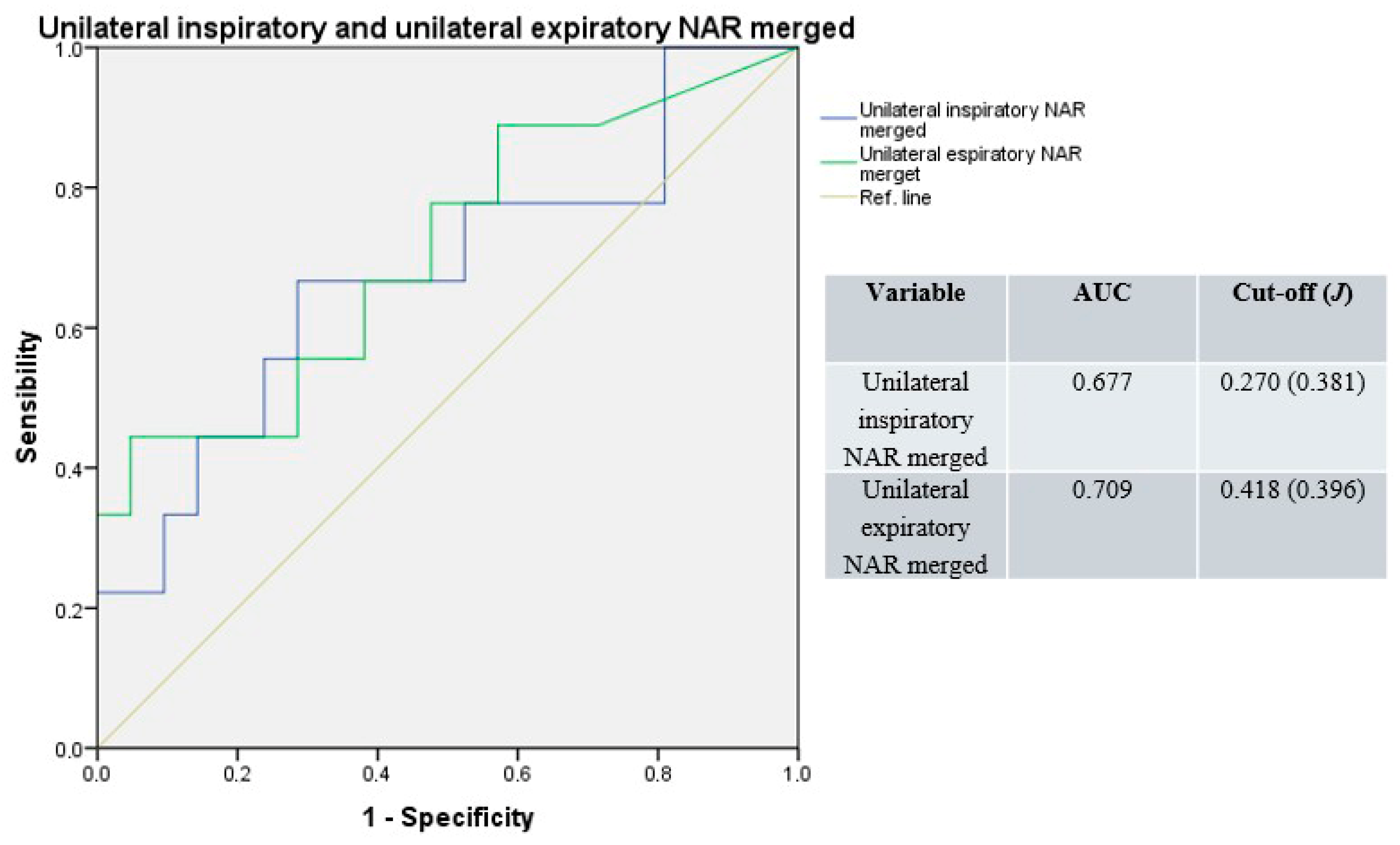
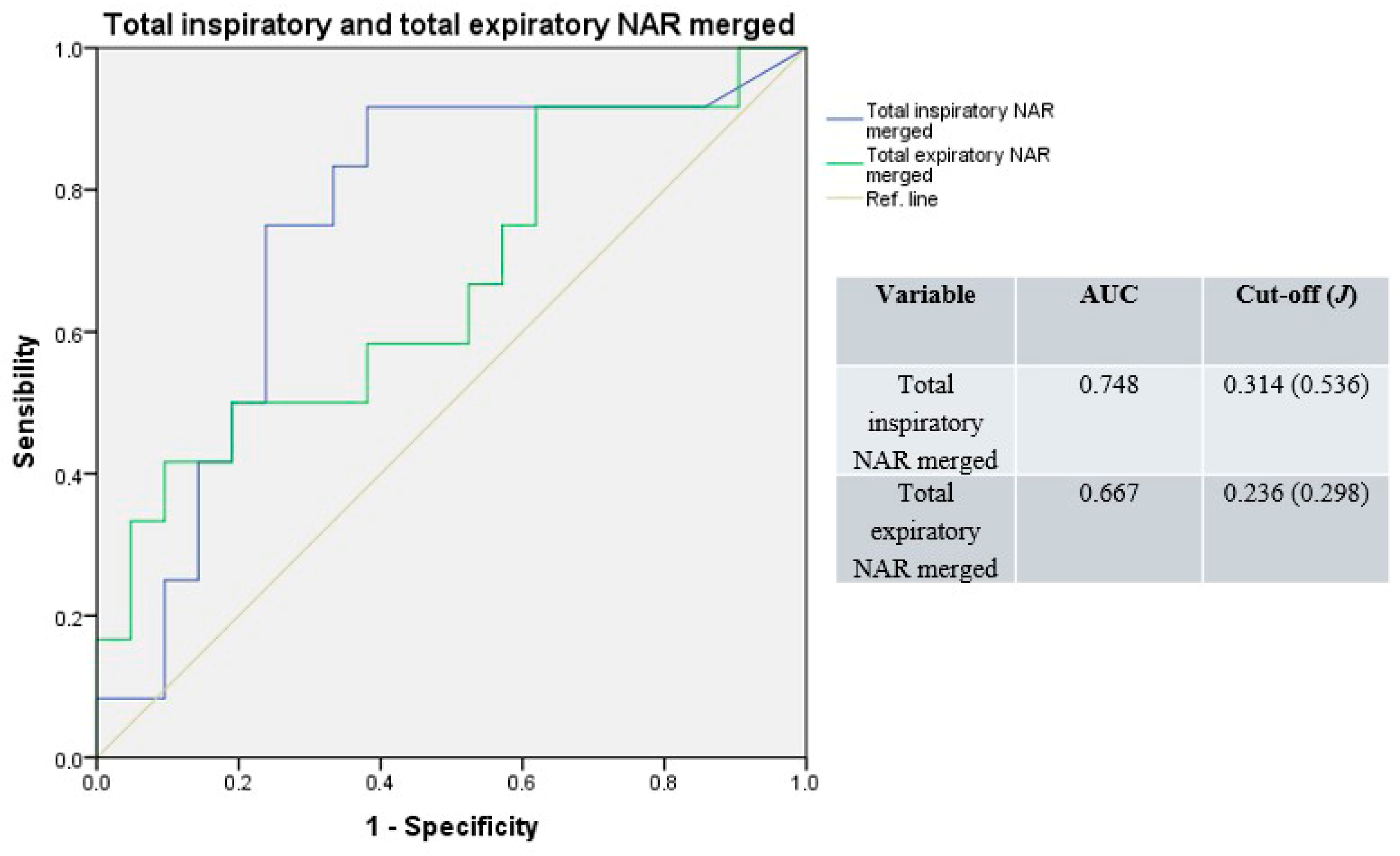
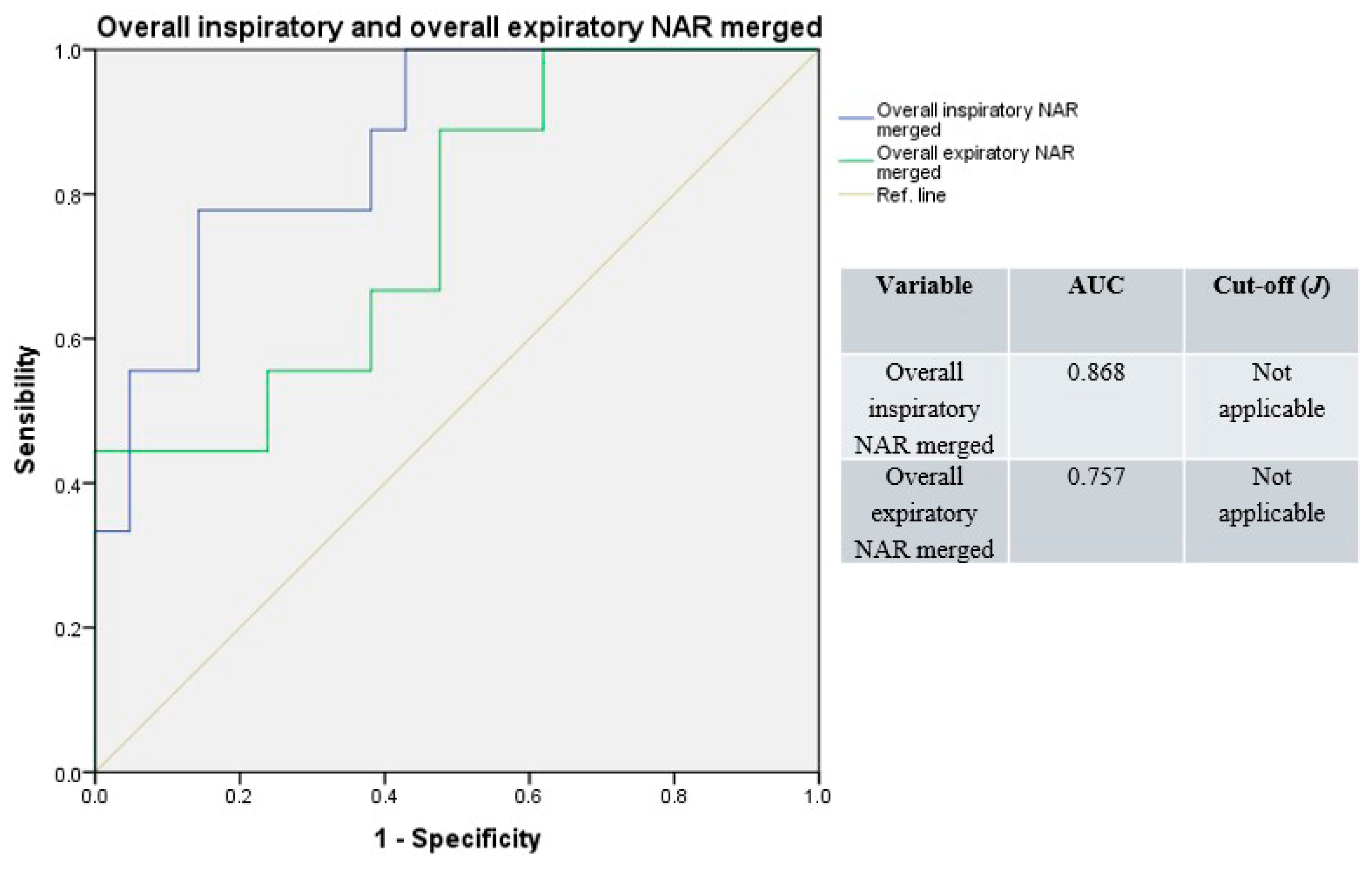
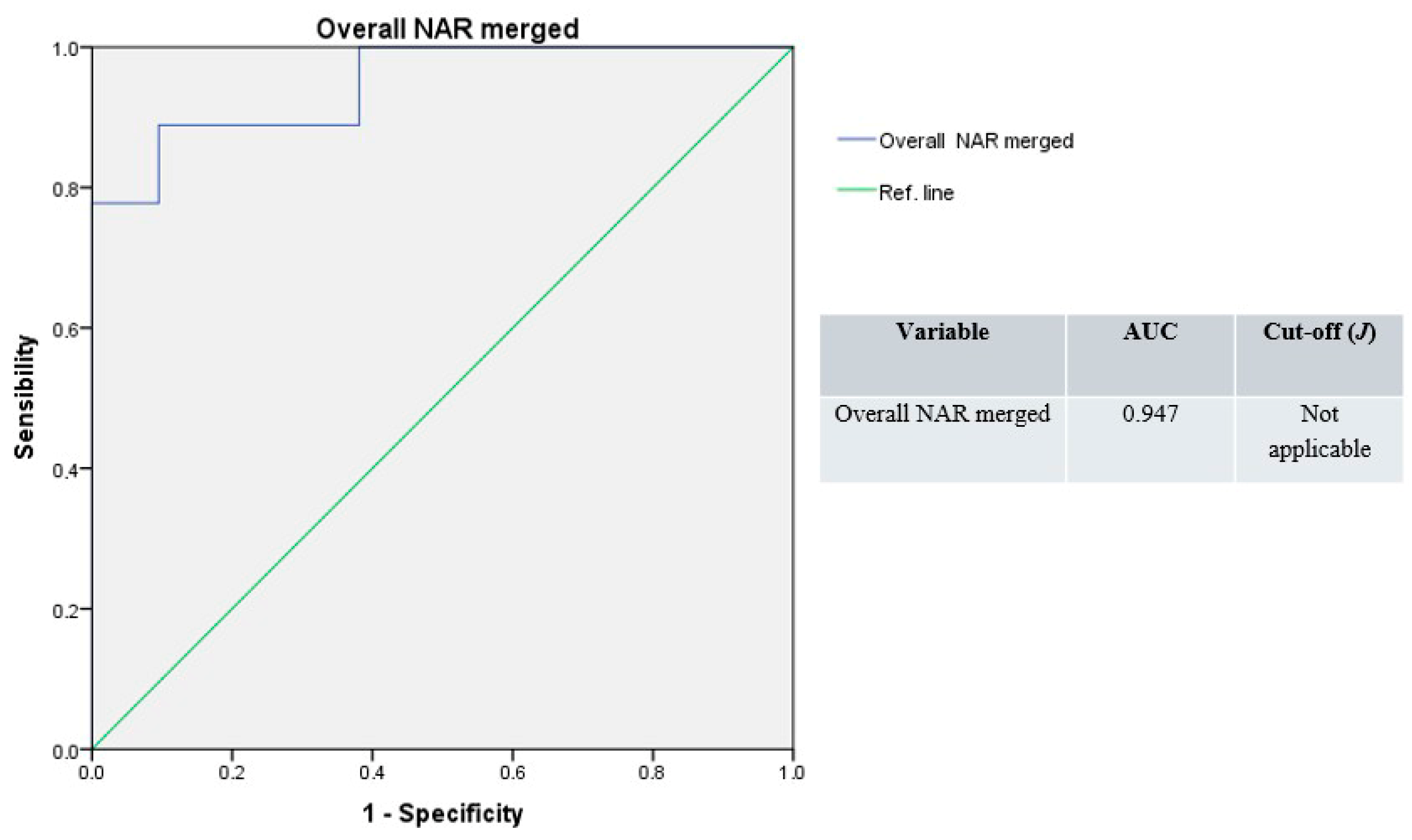
- AUC = 0.5: The test provides no diagnostic information;
- 0.5 < AUC ≤ 0.7: The test has low accuracy;
- 0.7 < AUC ≤ 0.9: The test has moderate accuracy;
- 0.9 < AUC < 1.0: The test has high accuracy;
- AUC = 1.0: The test is considered perfect.
3. Results
3.1. General Characteristics
3.2. Nasal Airflow Resistances
3.3. ROC Analysis
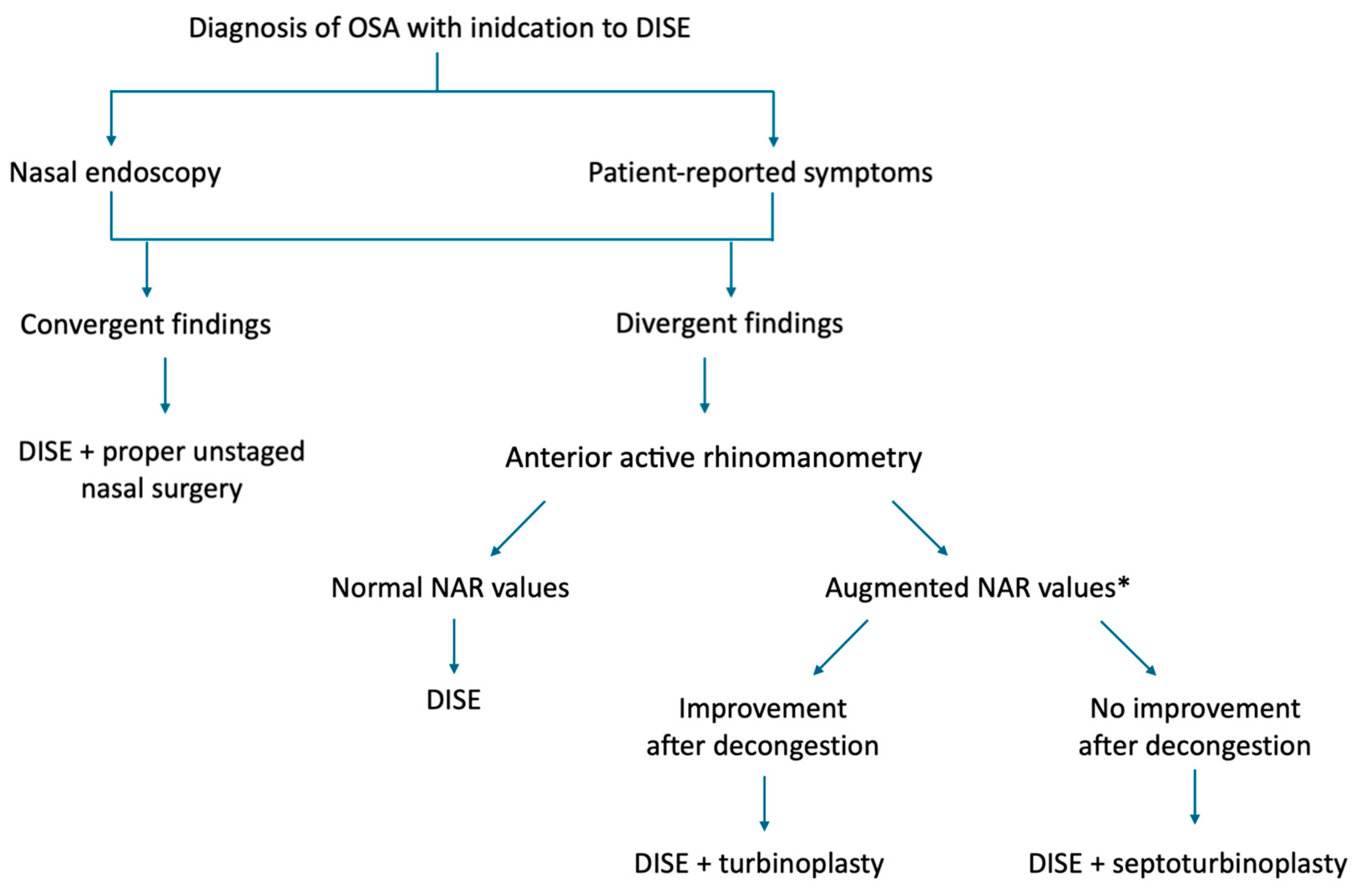
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hsu, D.W.; Suh, J.D. Anatomy and Physiology of Nasal Obstruction. Otolaryngol. Clin. N. Am. 2018, 51, 853–865. [Google Scholar] [CrossRef]
- García-Chabur, M.A.; Castellanos, J.; Corredor-Rojas, G.; Salgar, M.; Moreno, S.; Pinzón, M.; Peñaranda, A. Improvement in Nasal Obstruction and Quality of Life after Nasal Septoplasty with Turbinoplasty: A Pre- and Post-study. Int. Arch. Otorhinolaryngol. 2023, 27, e266–e273. [Google Scholar] [CrossRef] [PubMed]
- Stewart, M.; Ferguson, B.; Fromer, L. Epidemiology and burden of nasal congestion. Int. J. Gen. Med. 2010, 3, 37–45. [Google Scholar] [CrossRef] [PubMed]
- Hartfield, P.J.; Janczy, J.; Sharma, A.; Newsome, H.A.; Sparapani, R.A.; Rhee, J.S.; Woodson, B.T.; Garcia, G.J.M. Anatomical determinants of upper airway collapsibility in obstructive sleep apnea: A systematic review and meta-analysis. Sleep Med. Rev. 2023, 68, 101741. [Google Scholar] [CrossRef] [PubMed]
- Valero, A.; Navarro, A.M.; Del Cuvillo, A.; Alobid, I.; Benito, J.R.; Colás, C.; de Los Santos, G.; Fernández Liesa, R.; García-Lliberós, A.; González-Pérez, R.; et al. SEAIC Rhinoconjunctivitis Committee & SEORL Rhinology, Allergy, and Skull Base Committee. Position paper on nasal obstruction: Evaluation and treatment. J. Investig. Allergol. Clin. Immunol. 2018, 28, 67–90. [Google Scholar] [CrossRef]
- Giombi, F.; Pace, G.M.; Pirola, F.; Cerasuolo, M.; Ferreli, F.; Mercante, G.; Spriano, G.; Canonica, G.W.; Heffler, E.; Ferri, S.; et al. Airways Type-2 Related Disorders: Multiorgan, Systemic or Syndemic Disease? Int. J. Mol. Sci. 2024, 25, 730. [Google Scholar] [CrossRef]
- Magliulo, G.; Iannella, G.; Ciofalo, A.; Polimeni, A.; De Vincentiis, M.; Pasquariello, B.; Montevecchi, F.; Vicini, C. Nasal pathologies in patients with obstructive sleep apnoea. Acta Otorhinolaryngol. Ital. 2019, 39, 250–256. [Google Scholar] [CrossRef]
- Takahashi, R.; Ohbuchi, T.; Hohchi, N.; Takehuci, S.; Ohkubo, J.; Ikazaki, S.; Suzuki, H. Effect of septoplasty and turbinectomy on obstructive sleep apnea syndrome. Nippon. Jibiinkoka Gakkai Kaiho 2013, 116, 789–792. [Google Scholar] [CrossRef][Green Version]
- Zasadzińska-Stempniak, K.; Zajączkiewicz, H.; Kukwa, A. Prevalence of Obstructive Sleep Apnea in the Young Adult Population: A Systematic Review. J. Clin. Med. 2024, 13, 1386. [Google Scholar] [CrossRef]
- Di Bari, M.; Colombo, G.; Giombi, F.; Leone, F.; Bianchi, A.; Colombo, S.; Salamanca, F.; Cerasuolo, M. The effect of drug-induced sleep endoscopy on surgical outcomes for obstructive sleep apnea: A systematic review. Sleep Breath. 2024, 28, 859–867. [Google Scholar] [CrossRef]
- Fiorita, A.; Scarano, E.; Mastrapasqua, R.; Picciotti, P.M.; Loperfido, A.; Rizzotto, G.; Paludetti, G. Moderate OSAS and turbinate decongestion: Surgical efficacy in improving the quality of life and compliance of CPAP using Epworth score and SNOT-20 score. Acta Otorhinolaryngol. Ital. 2018, 38, 214–221. [Google Scholar] [CrossRef] [PubMed]
- Patil, N.; Jain, S. Rhinomanometry: A Comprehensive Review of Its Applications and Advancements in Rhinology Practice. Cureus 2024, 16, e61370. [Google Scholar] [CrossRef] [PubMed]
- Naito, K.; Horibe, S.; Tanaito, Y.; Kato, H.; Yoshioka, S.; Tateya, I. Objective assessment of nasal obstruction. Fujita Med. 2022, 9, 53–64. [Google Scholar] [CrossRef]
- Merkle, J.; Kohlhas, L.; Zadoyan, G.; Mösges, R.; Hellmich, M. Rhinomanometric reference intervals for normal total nasal airflow resistanxce. Rhinol. J. 2014, 4, 292–299. [Google Scholar] [CrossRef]
- Ohki, M.; Naito, K.; Cole, P. Dimensions and resistances of the human nose: Racial differences. Laryngoscope 1991, 101, 276–278. [Google Scholar] [CrossRef]
- Morgan, N.J.; MacGregor, F.B.; Birchall, M.A.; Lund, V.J.; Sittampalam, Y. Racial differences in nasal fossa dimensions determined by acoustic rhinometry. Rhinology 1995, 33, 224–228. [Google Scholar]
- Pshennikov, D.; Angotoeva, I.; Kosiakov, S. Piriform aperture as a cause of nasal obstruction. Part I. Anthropometric characteristics in different populations (systematic review). Vestn. Otorinolaringol. 2022, 87, 81–85. [Google Scholar] [CrossRef]
- Bolger, E.W.; Butzin, C.A.; Parsons, D.S. Paranasal sinus bony anatomic variations and mucosal abnormalities: CT analysis for endoscopic sinus surgery. Laryngoscope 1991, 101, 56–64. [Google Scholar] [CrossRef]
- Malhotra, R.K. AASM Scoring Manual 3: A step forward for advancing sleep care for patients with obstructive sleep apnea. J. Clin. Sleep Med. 2024, 20, 835–836. [Google Scholar] [CrossRef]
- Eccles, R. A guide to practical aspects of measurement of human nasal airflow by rhinomanometry. Rhinol. J. 2011, 49, 2–10. [Google Scholar] [CrossRef]
- Swoboda, S.; Thulesius, H.L.; Jessen, M. Paradoxical increase in nasal airway resistance after topical nasal decongestion—does it really exist? A retro- and prospective study. Clin. Otolaryngol. 2016, 41, 689–693. [Google Scholar] [CrossRef]
- Vogt, K.; Parker-Davidson, K. Measurement of Nasal Obstruction: Rhinomanometry as Basic Method in Functional Rhinology. Facial Plast. Surg. 2024, 40, 314–322. [Google Scholar] [CrossRef]
- Atkins, M.; Taskar, V.; Clayton, N.; Stone, P.; Woodcock, A. Nasal resistance in obstructive sleep apnea. Chest 1994, 105, 1133–1135. [Google Scholar] [CrossRef]
- Swets, J.A. Measuring the accuracy of diagnostic systems. Science 1998, 240, 1285–1293. [Google Scholar] [CrossRef]
- Sunnergren, O.; Ahonen, H.; Holmström, M.; Broström, A. Active anterior rhinomanometry: A study on nasal airway resistance, paradoxical reactions to decongestion, and repeatability in healthy subjects. Laryngoscope Investig. Otolaryngol. 2023, 8, 1136–1145. [Google Scholar] [CrossRef]
- Giunta, G.; Pirola, F.; Giombi, F.; Muci, G.; Pace, G.M.; Heffler, E.; Paoletti, G.; Puggioni, F.; Cerasuolo, M.; Ferreli, F.; et al. Care for Patients with Type-2 Chronic Rhinosinusitis. J. Pers. Med. 2023, 13, 618. [Google Scholar] [CrossRef]
- Yi-Fong Su, V.; Chou, K.T.; Tseng, C.H.; Kuo, C.Y.; Su, K.C.; Perng, D.W.; Chen, Y.M.; Chang, S.C. Mouth opening/breathing is common in sleep apnea and linked to more nocturnal water loss. Biomed. J. 2023, 46, 100536. [Google Scholar] [CrossRef]
- Suzuki, M.; Tanuma, T. The effect of nasal and oral breathing on airway collapsibility in patients with obstructive sleep apnea: Computational fluid dynamics analyses. PLoS ONE 2020, 15, e0231262. [Google Scholar] [CrossRef]
- Michels, D.d.S.; Rodrigues, A.d.M.; Nakanishi, M.; Sampaio, A.L.; Venosa, A.R. Nasal involvement in obstructive sleep apnea syndrome. Int. J. Otolaryngol. 2014, 2014, 717419. [Google Scholar] [CrossRef]
- Dang-Thi-Mai, K.; Le-Dong, N.N.; Le-Thuong, V.; Tran-Van, N.; Duong-Quy, S. Exhaled Nitric Oxide as a Surrogate Marker for Obstructive Sleep Apnea Severity Grading: An In-Hospital Population Study. Nat. Sci. Sleep 2021, 13, 763–773. [Google Scholar] [CrossRef]
- Miyamura, K.; Nakashima, D.; Nakayama, T.; Wada, K.; Capasso, R.; Chiba, S. Morphology of Nasal Septal Deviation in Obstructive Sleep Apnea Patients and its Treatment Method. Laryngoscope 2025, 135, 1520–1524. [Google Scholar] [CrossRef]
- Bican, A.; Kahraman, A.; Bora, I.; Kahveci, R.; Hakyemez, B. What is the efficacy of nasal surgery in patients with obstructive sleep apnea syndrome? J. Craniofacial Surg. 2010, 21, 1801–1806. [Google Scholar] [CrossRef]
- Wu, J.; Zhao, G.; Li, Y.; Zang, H.; Wang, T.; Wang, D.; Han, D. Apnea-hypopnea index decreased significantly after nasal surgery for obstructive sleep apnea: A meta-analysis. Medicine 2017, 96, e6008. [Google Scholar] [CrossRef]
- Brimioulle, M.; Chaidas, K. Nasal function and CPAP use in patients with obstructive sleep apnoea: A systematic review. Sleep Breath. 2022, 26, 1321–1332. [Google Scholar] [CrossRef]
- Holmstrom, M. The use of objective measures in selecting patients for septal surgery. Rhinol. J. 2010, 48, 387–393. [Google Scholar] [CrossRef]
- Giombi, F.; Pace, G.M.; Mari, G.; Cerasuolo, M.; Sandri, G.; Cerri, L.; Heffler, E.; Paoletti, G.; Puggioni, F.; Mercante, G.; et al. Assessing Nasal Obstruction Improvement in Dupilumab-Treated Patients with Active Anterior Rhinomanometry: A Preliminary Study. Ear. Nose Throat. J. 2025. Advance online publication. [Google Scholar] [CrossRef]
| Gender (%) | Male | 35 (73) |
| Female | 13 (27) | |
| Age (mean ± sd) | 53 ± 11 | |
| Surgery (%) | DISE with turbinoplasty | 27 (56) |
| DISE with septoturbinoplasty | 21 (44) | |
| HSAT parameters (mean ± sd) | AHI | 21.7/h ± 15 |
| ODI | 21.8/h ± 15 | |
| Mean SpO2 | 93.5% ± 2 | |
| Minimum SpO2 | 81.0% ± 7 | |
| CT90 | 8.9% ± 11 | |
| Upper airway comorbidities (%) | Non-allergic rhinitis | 34 (67) |
| Allergic rhinitis | 13 (26) | |
| Asthma | 2 (4) | |
| Chronic rhinosinusitis | 11 (23) | |
| With nasal polyps | 2 (4) | |
| Without nasal polyps | 9 (19) |
| Basal | Right | Inspiratory | 0.456 ± 0.680 |
| Expiratory | 0.270 ± 0.310 | ||
| Left | Inspiratory | 0.346 ± 0.329 | |
| Expiratory | 0.458 ± 1.493 | ||
| Total | Inspiratory | 0.183 ± 0.154 | |
| Expiratory | 0.178 ± 0.130 | ||
| Decongestion | Right | Inspiratory | 0.229 ± 0.395 |
| Expiratory | 0.158 ± 0.242 | ||
| Left | Inspiratory | 0.227 ± 0.258 | |
| Expiratory | 0.340 ± 1.011 | ||
| Total | Inspiratory | 0.103 ± 0.128 | |
| Expiratory | 0.134 ± 0.108 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lunardi, G.; Giombi, F.; Pace, G.M.; Cerasuolo, M.; Spriano, G.; Malvezzi, L. Measuring Nasal Airway Resistance to Personalize Surgery for Nasal Obstruction in OSA Patients. J. Pers. Med. 2025, 15, 608. https://doi.org/10.3390/jpm15120608
Lunardi G, Giombi F, Pace GM, Cerasuolo M, Spriano G, Malvezzi L. Measuring Nasal Airway Resistance to Personalize Surgery for Nasal Obstruction in OSA Patients. Journal of Personalized Medicine. 2025; 15(12):608. https://doi.org/10.3390/jpm15120608
Chicago/Turabian StyleLunardi, Giuseppe, Francesco Giombi, Gian Marco Pace, Michele Cerasuolo, Giuseppe Spriano, and Luca Malvezzi. 2025. "Measuring Nasal Airway Resistance to Personalize Surgery for Nasal Obstruction in OSA Patients" Journal of Personalized Medicine 15, no. 12: 608. https://doi.org/10.3390/jpm15120608
APA StyleLunardi, G., Giombi, F., Pace, G. M., Cerasuolo, M., Spriano, G., & Malvezzi, L. (2025). Measuring Nasal Airway Resistance to Personalize Surgery for Nasal Obstruction in OSA Patients. Journal of Personalized Medicine, 15(12), 608. https://doi.org/10.3390/jpm15120608








