Identifying Risk Groups in 73,000 Patients with Diabetes Receiving Total Hip Replacement: A Machine Learning Clustering Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Study Design and Population
2.3. Data Variables and Outcomes
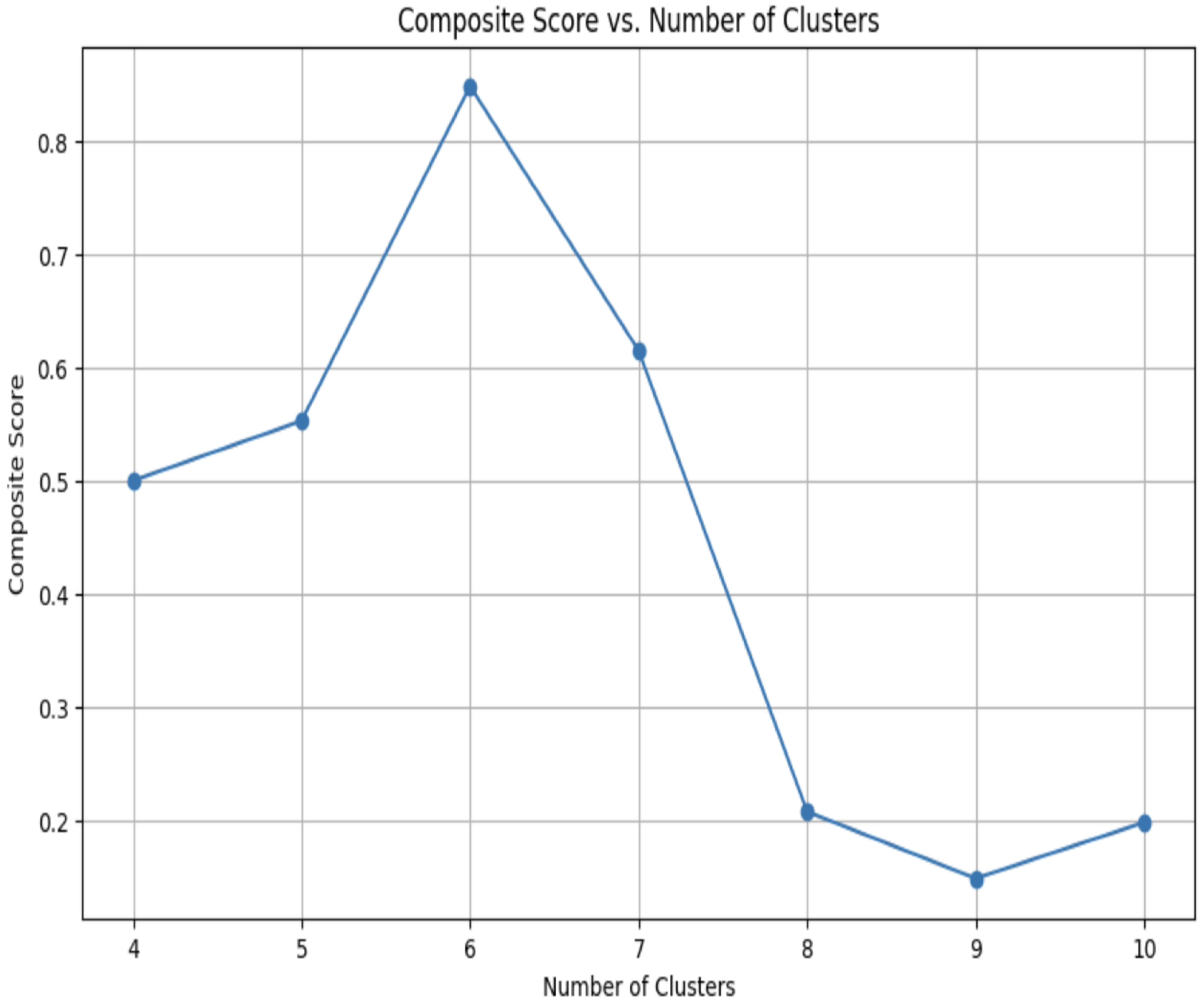
2.4. Clustering
2.5. Statistical Analysis
3. Results
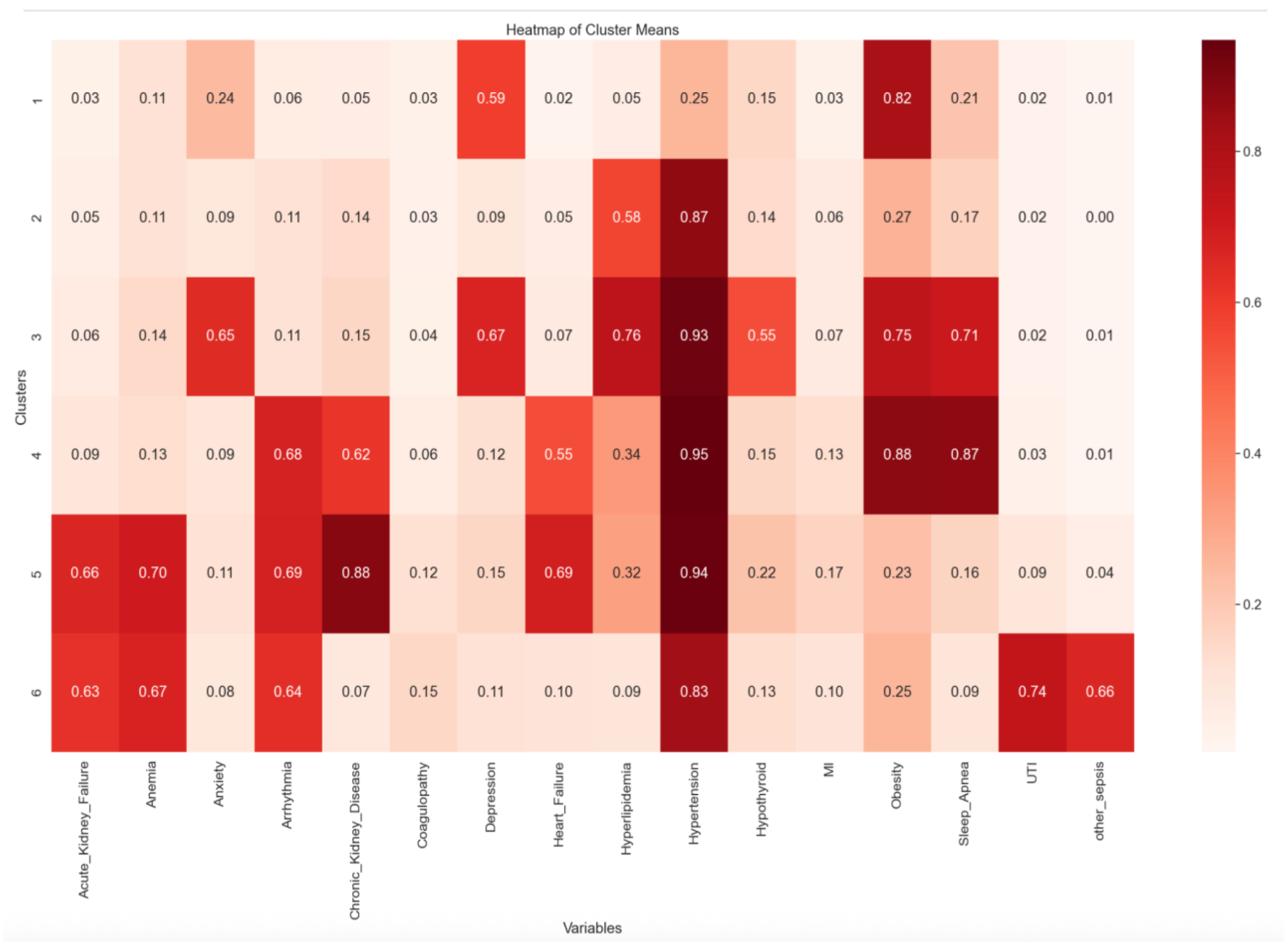
3.1. Clustering Comorbidities
3.2. Non-Routine Discharge
3.3. Length of Stay
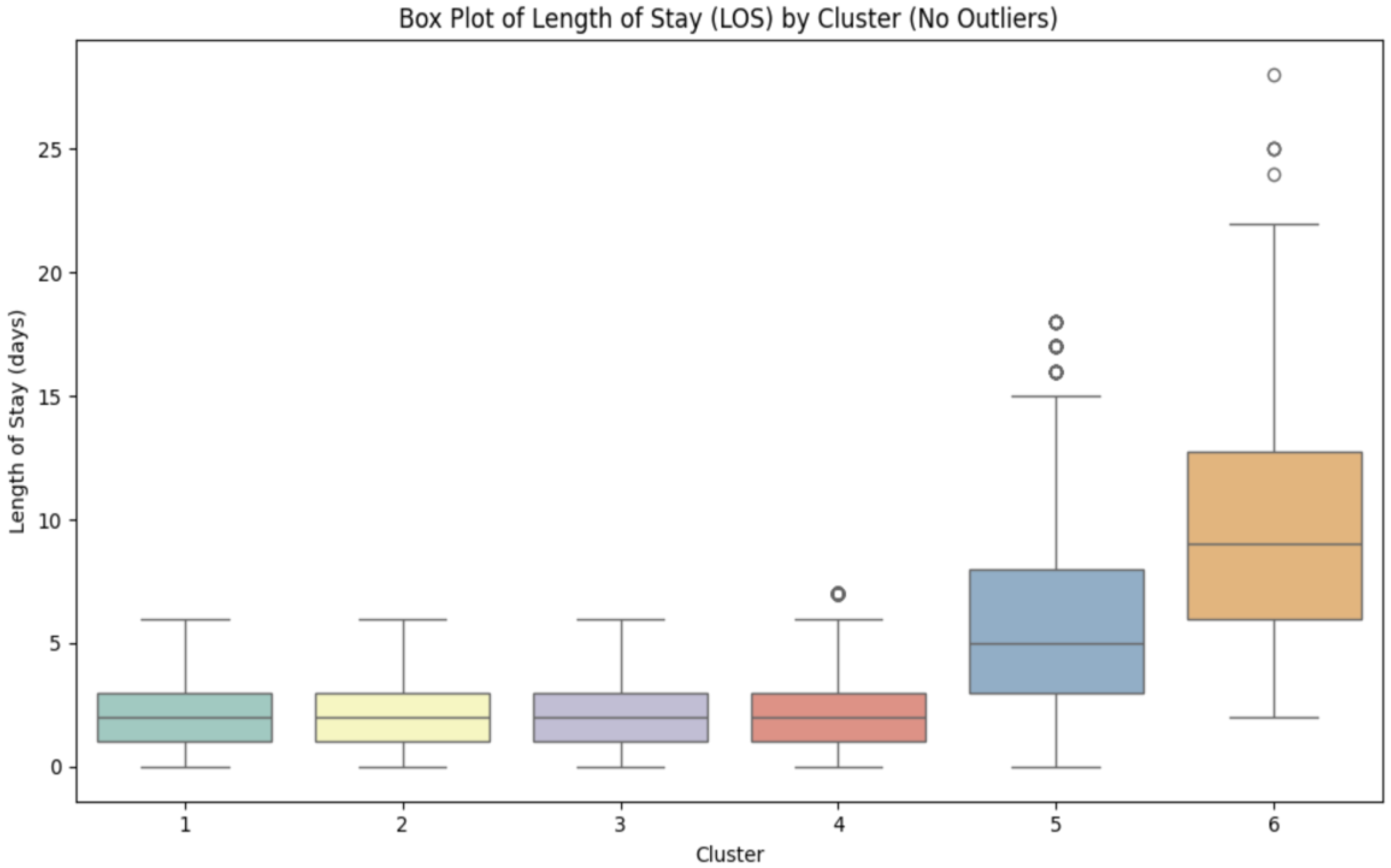
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Schuster, D.P.; Duvuuri, V. Diabetes mellitus. Clin. Podiatr. Med. Surg. 2002, 19, 79–107. [Google Scholar] [CrossRef]
- Skyler, J.S.; Oddo, C. Diabetes trends in the USA. Diabetes Metab. Res. Rev. 2002, 18 (Suppl. S3), S21–S26. [Google Scholar] [CrossRef]
- Ismail, L.; Materwala, H.; Al Kaabi, J. Association of risk factors with type 2 diabetes: A systematic review. Comput. Struct. Biotechnol. J. 2021, 19, 1759–1785. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Khalid, J.M.; Raluy-Callado, M.; Curtis, B.H. Rates and risk of hospitalisation among patients with type 2 diabetes. Int. J. Clin. Pract. 2014, 68, 40–48. [Google Scholar] [CrossRef]
- Varacallo, M.A.; Luo, T.D.; Johanson, N.A. Total Hip Arthroplasty Techniques; StatPearls: Treasure Island, FL, USA, 2025. [Google Scholar]
- López-de-Andrés, A.; Hernández-Barrera, V.; Martínez-Huedo, M.A. Type 2 diabetes and in-hospital complications after revision of total hip and knee arthroplasty. PLoS ONE 2017, 12, e0183796. [Google Scholar] [CrossRef] [PubMed]
- Habehh, H.; Gohel, S. Machine Learning in Healthcare. Curr. Genom. 2021, 22, 291–300. [Google Scholar] [CrossRef]
- Pean, C.A.; Buddhiraju, A.; Shimizu, M.R.; Chen, T.L.; Esposito, J.G.; Kwon, Y.M. Prediction of 30-Day Mortality Following Revision Total Hip and Knee Arthroplasty: Machine Learning Algorithms Outperform CARDE-B, 5-Item, and 6-Item Modified Frailty Index Risk Scores. J. Arthroplast. 2024, 39, 2824–2830. [Google Scholar] [CrossRef] [PubMed]
- Wang, J. Artificial intelligence in total knee arthroplasty: Current status and future directions. J. Orthop. Translat. 2020, 24, 76–81. [Google Scholar]
- Yoon, J.R. Machine learning in orthopaedics: Current use and future directions. Bone Jt. J. 2021, 103, 170–176. [Google Scholar]
- Granat, M.M.; Paź, A.; Mirowska-Guzel, D. Testing the Knowledge of Artificial Intelligence Chatbots in Pharmacology: Examples of Two Groups of Drugs. PeerJ Comput. Sci. 2025, 11, e2954. [Google Scholar] [CrossRef]
- Gupta, S.S.; Pandey, T.K.; Raju, V.P.; Shrivastava, R.; Pandey, R.; Nigam, A.; Roy, V. Diabetes Estimation Through Data Mining Using Optimization, Clustering, and Secure Cloud Storage Strategies. SN Comput. Sci. 2024, 5, 781. [Google Scholar] [CrossRef]
- Aminizadeh, S.; Heidari, A.; Dehghan, M.; Toumaj, S.; Rezaei, M.; Navimipour, N.J.; Stroppa, F.; Unal, M. Opportunities and challenges of artificial intelligence and distributed systems to improve the quality of healthcare service. Artif. Intell. Med. 2024, 149, 102779. [Google Scholar] [CrossRef] [PubMed]
- Ngiam, K.Y.; Khor, I.W. Big data and machine learning algorithms for health-care delivery. Lancet Oncol. 2019, 20, e262–e273. [Google Scholar] [CrossRef] [PubMed]
- Nagamine, T.; Gillette, B.; Pakhomov, A.; Kahoun, J.; Mayer, H.; Burghaus, R.; Lippert, J.; Saxena, M. Multiscale classification of heart failure phenotypes by unsupervised clustering of unstructured electronic medical record data. Sci. Rep. 2020, 10, 21340. [Google Scholar] [CrossRef]
- Ghassib, I.H.; Batarseh, F.A.; Wang, H.L.; Borgnakke, W.S. Clustering by periodontitis-associated factors: A novel application to NHANES data. J. Periodontol. 2021, 92, 1136–1150. [Google Scholar] [CrossRef]
- Chin, S. Clustering methods in rheumatic and musculoskeletal disease. J. Rheumatol. 2024, 51, 1160–1168. [Google Scholar] [CrossRef]
- Esteva, A.; Robicquet, A.; Ramsundar, B. A guide to deep learning in healthcare. Nat. Med. 2019, 25, 24–29. [Google Scholar] [CrossRef]
- Jiang, L. Disparities in surgical outcomes among patients with diabetes. Diabetes Care 2020, 43, e57–e58. [Google Scholar]
- Everhart, J.S.; Altneu, E.; Calhoun, J.H. Medical Comorbidities Are Independent Preoperative Risk Factors for Surgical Infection After Total Joint Arthroplasty. Clin. Orthop. Relat. Res. 2013, 471, 3112–3119. [Google Scholar] [CrossRef]
- Karlin, E.A.; Lin, C.C.; Meftah, M. The impact of machine learning on total joint arthroplasty patient outcomes: A systematic review. J. Arthroplast. 2023, 38, 2085–2095. [Google Scholar] [CrossRef]
- Zeng, C.; Kaur, M.N.; Malapati, S.H. Patterns of social needs predict quality-of-life and healthcare utilization outcomes in patients from a large hospital system. J. Gen. Intern. Med. 2024, 39, 2060–2068. [Google Scholar] [CrossRef]
- Axelrod, D.A.; Upchurch, G.R.; DeMonner, S. Perioperative cardiovascular risk stratification of patients with diabetes who undergo elective major vascular surgery. J. Vasc. Surg. 2002, 35, 894–901. [Google Scholar] [CrossRef]
- Stryker, L.S.; Abdel, M.P.; Morrey, M.E.; Morrow, M.M.; Kor, D.J.; Morrey, B.F. Elevated postoperative blood glucose and preoperative hemoglobin A1C are associated with increased wound complications following total joint arthroplasty. J. Bone Jt. Surg. Am. 2013, 95, 808–814. [Google Scholar] [CrossRef] [PubMed]
- Na, A.; Middleton, A.; Haas, A. Impact of diabetes on 90-day episodes of care after elective total joint arthroplasty among Medicare beneficiaries. J. Bone Jt. Surg. Am. 2020, 102, 2157–2165. [Google Scholar] [CrossRef]

| Sample Size | Age (Years) | Sex | n (%) | ||
|---|---|---|---|---|---|
| Total | 73,606 | Mean | 68.12 | Male | 35,800 (48.64) |
| St. Dev. | 10.003 | Female | 37,806 (51.36) | ||
| Income Quartile | n (%) | Payer Type | n (%) | Race | n (%) |
| 1st | 18,079 (24.56) | Medicare | 47,870 (65.04) | White | 58,854 (79.96) |
| 2nd | 20,001 (27.17) | Medicaid | 19,656 (26.70) | Black | 8559 (11.63) |
| 3rd | 19,326 (26.26) | Private insurance | 3628 (4.93) | Hispanic | 3575 (4.86) |
| 4th | 16,200 (22.01) | Self-pay | 1931 (2.62) | Asian or Pacific Islander | 935 (1.27) |
| No charge | 477 (0.65) | Native American | 340 (0.46) | ||
| Other | 44 (0.06) | Other | 1343 (1.82) | ||
| Cluster | Cluster Size | Odds Ratio (95% CI) | p-Value | Adjusted Odds Ratio (95% CI) | p-Value |
|---|---|---|---|---|---|
| 1 | 3372 | Ref. | Ref. | Ref. | Ref. |
| 2 | 61,505 | 1.10 (1.02–1.18) | 0.010 | 0.94 (0.87–1.02) | 0.128 |
| 3 | 5174 | 1.16 (1.06–1.27) | 0.002 | 1.06 (0.96–1.16) | 0.261 |
| 4 | 1916 | 1.51 (1.33–1.71) | <0.001 | 1.33 (1.16–1.53) | <0.001 |
| 5 | 1532 | 4.33 (3.63–5.16) | <0.001 | 3.18 (2.62–3.87) | <0.001 |
| 6 | 107 | 10.88 (4.42–26.78) | <0.001 | 7.83 (3.16–19.41) | <0.001 |
| Cluster Group | Median Days Spent Hospitalized Post-Surgery | Q1 | Q3 | IQR |
|---|---|---|---|---|
| 1 | 2.00 | 1.00 | 3.00 | 2.00 |
| 2 | 2.00 | 1.00 | 3.00 | 2.00 |
| 3 | 2.00 | 1.00 | 3.00 | 2.00 |
| 4 | 2.00 | 1.00 | 3.00 | 2.00 |
| 5 | 5.00 | 3.00 | 8.00 | 5.00 |
| 6 | 9.00 | 6.00 | 12.75 | 6.75 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahmadi, A.; Kaywood, A.J.; Chavarria, A.; Omobhude, O.F.; Kiss, A.; Faltyn, M.; Hoellwarth, J.S. Identifying Risk Groups in 73,000 Patients with Diabetes Receiving Total Hip Replacement: A Machine Learning Clustering Analysis. J. Pers. Med. 2025, 15, 537. https://doi.org/10.3390/jpm15110537
Ahmadi A, Kaywood AJ, Chavarria A, Omobhude OF, Kiss A, Faltyn M, Hoellwarth JS. Identifying Risk Groups in 73,000 Patients with Diabetes Receiving Total Hip Replacement: A Machine Learning Clustering Analysis. Journal of Personalized Medicine. 2025; 15(11):537. https://doi.org/10.3390/jpm15110537
Chicago/Turabian StyleAhmadi, Alishah, Anthony J. Kaywood, Alejandra Chavarria, Oserekpamen Favour Omobhude, Adam Kiss, Mateusz Faltyn, and Jason S. Hoellwarth. 2025. "Identifying Risk Groups in 73,000 Patients with Diabetes Receiving Total Hip Replacement: A Machine Learning Clustering Analysis" Journal of Personalized Medicine 15, no. 11: 537. https://doi.org/10.3390/jpm15110537
APA StyleAhmadi, A., Kaywood, A. J., Chavarria, A., Omobhude, O. F., Kiss, A., Faltyn, M., & Hoellwarth, J. S. (2025). Identifying Risk Groups in 73,000 Patients with Diabetes Receiving Total Hip Replacement: A Machine Learning Clustering Analysis. Journal of Personalized Medicine, 15(11), 537. https://doi.org/10.3390/jpm15110537






