Total Knee Arthroplasty and the Evolution of Coronal Alignment: From Mechanical to Personalized Strategies
Abstract
1. Introduction
2. Mechanical Alignment
3. Anatomical Alignment
4. Adjusted Mechanical Alignment
5. Kinematic Alignment
6. Restricted Kinematic Alignment
7. Inverse Kinematic Alignment
8. Functional Alignment
9. Discussion
10. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hsu, H.; Siwiec, R. Knee Osteoarthritis. [Updated 26 June 2023]; In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar]
- Picchi, A.; Rovere, G.; Fulchignoni, C.; Bosco, F.; Venosa, M.; Andriollo, L.; De Vitis, R.; Smakaj, A.; Fidanza, A. Dual Mobility Arthroplasty Versus Suspension Tenoplasty for Treatment of Trapezio–Metacarpal Joint Arthritis: A Clinical Trial. Appl. Sci. 2025, 15, 3967. [Google Scholar] [CrossRef]
- Clark, G.P. Treatment options for symptomatic knee osteoarthritis in adults. JAAPA 2023, 36, 1–6. [Google Scholar] [CrossRef]
- Matassi, F.; Pettinari, F.; Frasconà, F.; Innocenti, M.; Civinini, R. Coronal alignment in total knee arthroplasty: A review. J. Orthop. Traumatol. 2023, 24, 24. [Google Scholar] [CrossRef] [PubMed]
- Insall, J.N.; Binazzi, R.; Soudry, M.; Mestriner, L.A. Total knee arthroplasty. Clin. Orthop. Relat. Res. 1985, 192, 13–22. [Google Scholar] [CrossRef]
- Rodriguez, J.A.; Bhende, H.; Ranawat, C.S. Total condylar knee replacement: A 20-year followup study. Clin. Orthop. Relat. Res. 2001, 388, 10–17. [Google Scholar] [CrossRef]
- Dhungana, H.; Jangid, S.; Goyal, M.; Department of Orthopedics, Fortis Hospital, Gurgaon, Haryana, India. Alignment Techniques in Total Knee Arthroplasty: Where do We Stand Today? Chin. Med. Sci. J. 2024, 39, 217–225. [Google Scholar] [CrossRef]
- Boonen, B.; Schotanus, M.; Kerens, B.; Van der Weegen, W.; van Drumpt, R.; Kort, N. Intra-operative results and radiological outcome of conventional and patient-specific surgery in total knee arthroplasty: A multicentre, randomised controlled trial. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 2206–2212. [Google Scholar] [CrossRef]
- Nisar, S.; Palan, J.; Rivière, C.; Emerton, M.; Pandit, H. Kinematic alignment in total knee arthroplasty. EFORT Open Rev. 2020, 5, 380–390. [Google Scholar] [CrossRef]
- Ritter, M.A.; Faris, P.M.; Keating, E.M.; Meding, J.B. Postoperative Alignment of Total Knee Replacement Its Effect on Survival. Clin. Orthop. Relat. Res. 1994, 299, 153–156. [Google Scholar] [CrossRef]
- Zhang, G.; Chen, J.; Chai, W.; Liu, M.; Wang, Y. Comparison between computer-assisted-navigation and conventional total knee arthroplasties in patients undergoing simultaneous bilateral procedures: A randomized clinical trial. JBJS 2011, 93, 1190–1196. [Google Scholar] [CrossRef]
- Rossi, S.M.P.; Sangaletti, R.; Andriollo, L.; Matascioli, L.; Benazzo, F. The use of a modern robotic system for the treatment of severe knee deformities. Technol. Health Care 2024, 32, 3737–3746. [Google Scholar] [CrossRef]
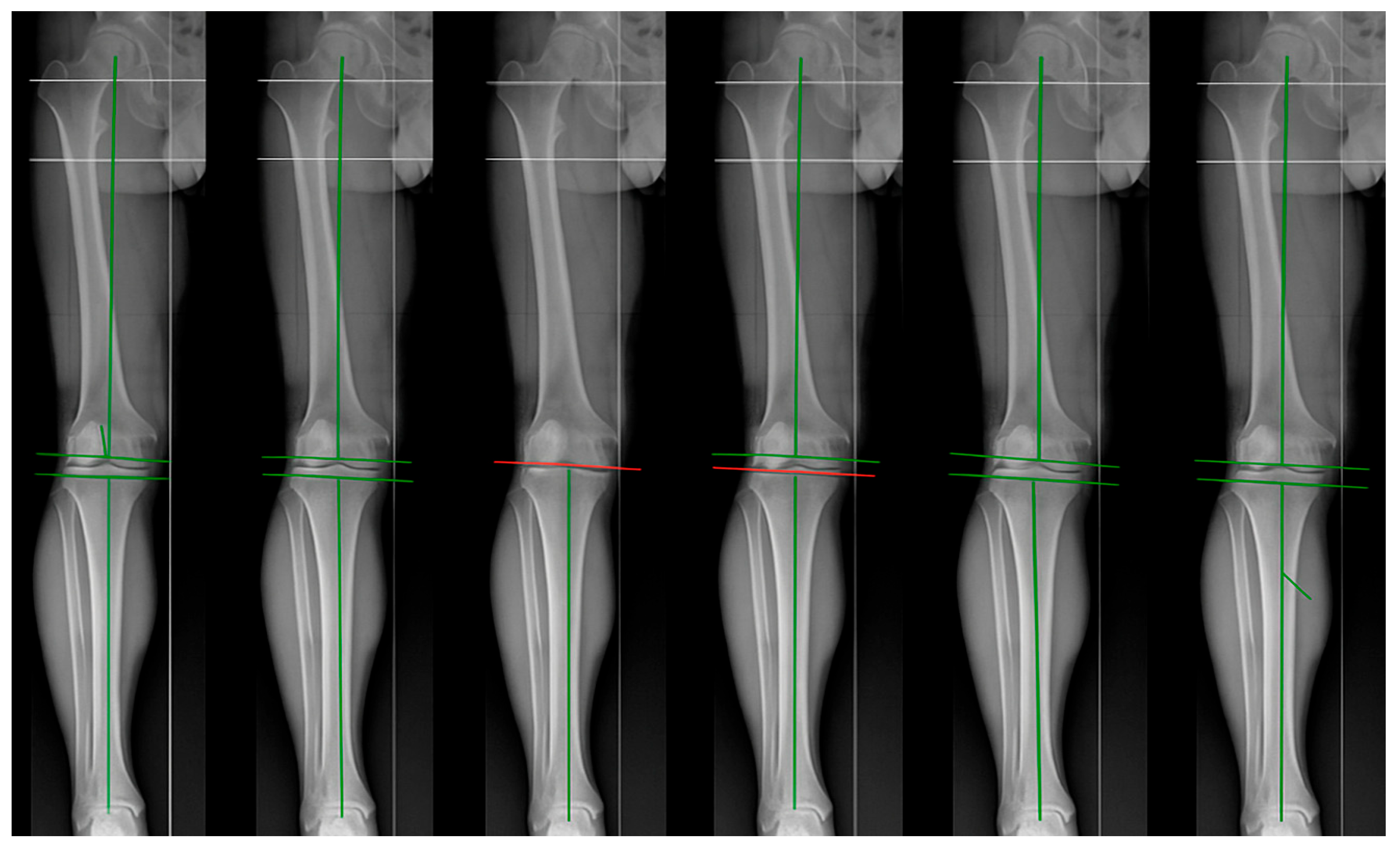
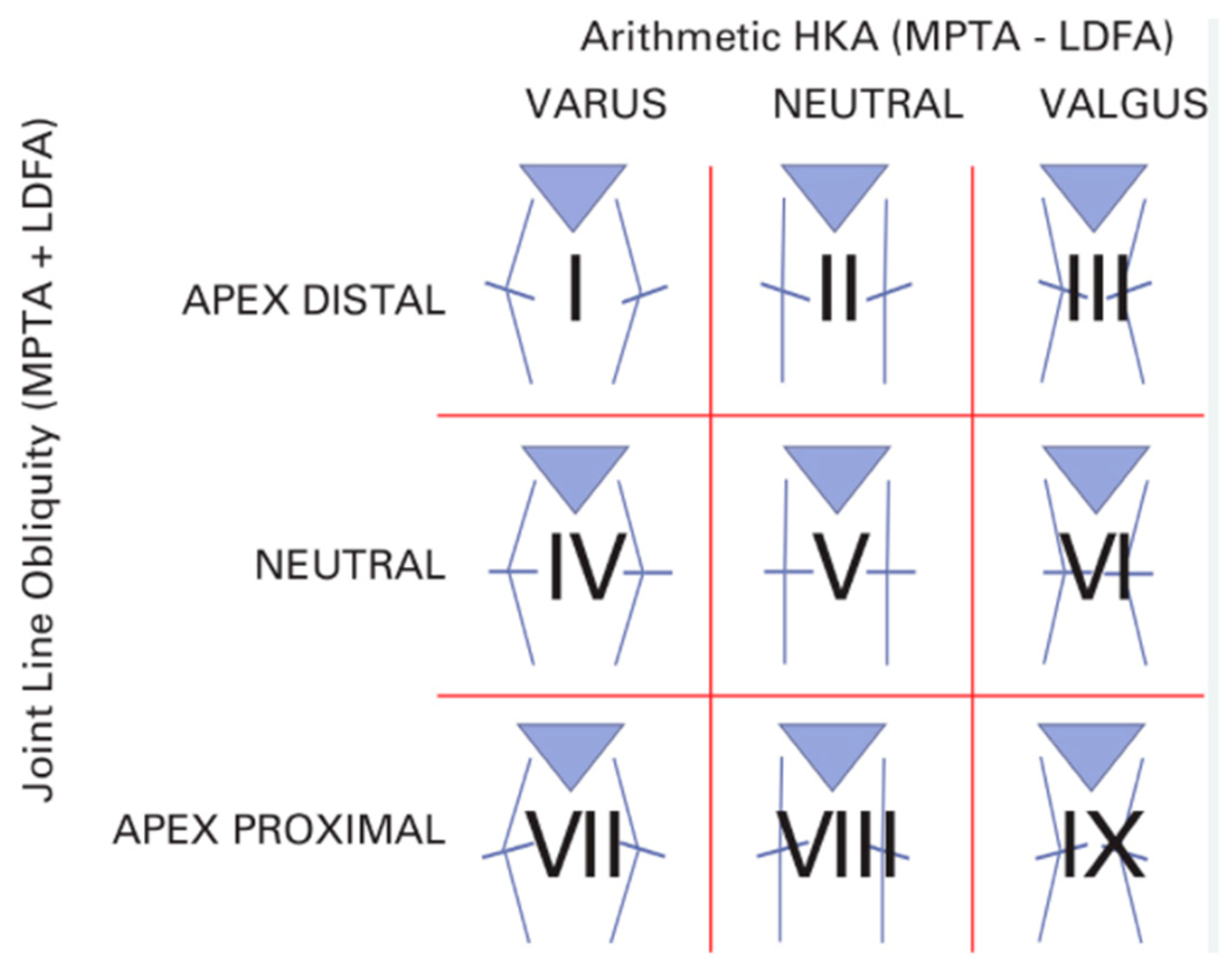
- MacDessi, S.J.; Griffiths-Jones, W.; Harris, I.A.; Bellemans, J.; Chen, D.B. Coronal Plane Alignment of the Knee (CPAK) classification: A new system for describing knee phenotypes. Bone Jt. J. 2021, 103-B, 329–337. [Google Scholar] [CrossRef]
- Bellemans, J.; Colyn, W.; Vandenneucker, H.; Victor, J. The Chitranjan Ranawat Award: Is neutral mechanical alignment normal for all patients?: The concept of constitutional varus. Clin. Orthop. Relat. Res. 2012, 470, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Karasavvidis, T.; Moldenhauer, C.A.P.; Haddad, F.S.; Hirschmann, M.T.; Pagnano, M.W.; Vigdorchik, J.M. Current concepts in alignment in total knee arthroplasty. J. Arthroplast. 2023, 38, S29–S37. [Google Scholar] [CrossRef] [PubMed]
- Park, A.; Stambough, J.B.; Nunley, R.M.; Barrack, R.L.; Nam, D. The inadequacy of short knee radiographs in evaluating coronal alignment after total knee arthroplasty. J. Arthroplast. 2016, 31, 878–882. [Google Scholar] [CrossRef]
- Hungerford, D.S.; Krackow, K.A. Total joint arthroplasty of the knee. Clin. Orthop. Relat. Res. 1985, 192, 23–33. [Google Scholar] [CrossRef]
- Rivière, C.; Iranpour, F.; Auvinet, E.; Howell, S.; Vendittoli, P.-A.; Cobb, J.; Parratte, S. Alignment options for total knee arthroplasty: A systematic review. Orthop. Traumatol. Surg. Res. 2017, 103, 1047–1056. [Google Scholar] [CrossRef]
- Yeo, J.H.; Seon, J.K.; Lee, D.H.; Song, E.K. No difference in outcomes and gait analysis between mechanical and kinematic knee alignment methods using robotic total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 1142–1147. [Google Scholar] [CrossRef] [PubMed]
- Manjunath, K.; Gopalakrishna, K.; Vineeth, G. Evaluation of alignment in total knee arthroplasty: A prospective study. Eur. J. Orthop. Surg. Traumatol. 2015, 25, 895–903. [Google Scholar] [CrossRef]
- Zheng, K.; Sun, H.; Zhang, W.; Zhu, F.; Zhou, J.; Li, R.; Geng, D.; Xu, Y. Mid-Term Outcomes of Navigation-Assisted Primary Total Knee Arthroplasty Using Adjusted Mechanical Alignment. Orthop. Surg. 2023, 15, 230–238. [Google Scholar] [CrossRef]
- Graichen, H.; Luderer, V.; Strauch, M.; Hirschmann, M.T.; Scior, W. Navigated, gap-balanced, adjusted mechanical alignment achieves alignment and balancing goals in a very high percentage but with partially non-anatomical resections. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 768–776. [Google Scholar] [CrossRef]
- Luderer, V.; Strauch, M.; Hirschmann, M.T.; Graichen, H. Independent of the preoperative coronal deformity, adjusted mechanical alignment leads in a high percentage to non-anatomical tibial and femoral bone cuts. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 3784–3791. [Google Scholar] [CrossRef] [PubMed]
- Hollister, A.M.; Jatana, S.; Singh, A.K.; Sullivan, W.W.; Lupichuk, A.G. The axes of rotation of the knee. Clin. Orthop. Relat. Res. 1993, 290, 259–268. [Google Scholar] [CrossRef]
- Howell, S.M.; Kuznik, K.; Hull, M.L.; Siston, R.A. Results of an initial experience with custom-fit positioning total knee arthroplasty in a series of 48 patients. Orthopedics 2008, 31, 857–863. [Google Scholar] [CrossRef]
- Dossett, H.G.; Swartz, G.J.; Estrada, N.A.; LeFevre, G.W.; Kwasman, B.G. Kinematically versus mechanically aligned total knee arthroplasty. Orthopedics 2012, 35, e160–e169. [Google Scholar] [CrossRef]
- Tuecking, L.R.; Savov, P.; Windhagen, H.; Ettinger, M. Current evidence base for kinematic alignment. Orthopade 2020, 49, 584–592. [Google Scholar] [CrossRef]
- Calliess, T.; Ettinger, M.; Stukenborg-Colsmann, C.; Windhagen, H. Kinematic alignment in total knee arthroplasty: Concept, evidence base and limitations. Orthopade 2015, 44, 282–289. [Google Scholar] [CrossRef]
- Howell, S.M.; Howell, S.J.; Kuznik, K.T.; Cohen, J.; Hull, M.L. Does a kinematically aligned total knee arthroplasty restore function without failure regardless of alignment category? Clin. Orthop. Relat. Res. 2013, 471, 1000–1007. [Google Scholar] [CrossRef] [PubMed]
- Brar, A.S.; Howell, S.M.; Hull, M.L.; Mahfouz, M.R. Does kinematic alignment and flexion of a femoral component designed for mechanical alignment reduce the proximal and lateral reach of the trochlea? J. Arthroplast. 2016, 31, 1808–1813. [Google Scholar] [CrossRef] [PubMed]
- Courtney, P.M.; Lee, G.C. Early outcomes of kinematic alignment in primary total knee arthroplasty: A meta-analysis of the literature. J. Arthroplast. 2017, 32, 2028–2032. [Google Scholar] [CrossRef]
- Howell, S.M.; Shelton, T.J.; Hull, M.L. Implant survival and function ten years after kinematically aligned total knee arthroplasty. J. Arthroplast. 2018, 33, 3678–3684. [Google Scholar] [CrossRef]
- Shelton, T.J.; Gill, M.; Athwal, G.; Howell, S.M.; Hull, M.L. Outcomes in patients with a calipered kinematically aligned TKA that already had a contralateral mechanically aligned TKA. J. Knee Surg. 2021, 34, 087–093. [Google Scholar] [CrossRef]
- Becker, R.; Tandogan, R.; Violante, B. Alignment in total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 2393–2394. [Google Scholar] [CrossRef]
- Blakeney, W.G.; Vendittoli, P.A. Restricted kinematic alignment: The ideal compromise? In Personalized Hip and Knee Joint Replacement; Springer: Cham, Switzerland, 2020; pp. 197–206. [Google Scholar]
- Minoda, Y. Alignment techniques in total knee arthroplasty. J. Jt. Surg. Res. 2023, 1, 108–116. [Google Scholar] [CrossRef]
- Abhari, S.; Hsing, T.; Malkani, M.; Smith, A.F.; Smith, L.S.; Mont, M.A.; Malkani, A.L. Patient Satisfaction Following Total Knee Arthroplasty Using Restricted Kinematic Alignment. Bone Jt. J. 2021, 103-B, 59–66. [Google Scholar] [CrossRef] [PubMed]
- Shichman, I.; Hadad, A.; Brandstetter, A.S.; Ashkenazi, I.; Warschwaski, Y.; Gold, A.; Snir, N. Better restoration of joint line obliquity in tibia first restricted kinematic alignment versus mechanical alignment TKA. Arch. Orthop. Trauma. Surg. 2024, 144, 4475–4481. [Google Scholar] [CrossRef]
- de Grave, P.W.; Kellens, J.; Luyckx, T.; Tampere, T.; Lacaze, F.; Claeys, K. Inverse kinematic alignment for total knee arthroplasty. Orthop. Traumatol. Surg. Res. 2022, 108, 103305. [Google Scholar] [CrossRef]
- Genestoux, V.; Vermorel, P.H.; Neri, T.; Farizon, F.; Philippot, R. Does inverse kinematic alignment coupled with robot-assisted TKA optimize patellofemoral clinical and radiological results? Orthop. Traumatol. Surg. Res. 2024, 110, 103880. [Google Scholar] [CrossRef] [PubMed]
- Keyes, S.; Russell, S.P.; Bertalan, Z.; Harty, J.A. Inverse kinematic total knee arthroplasty using conventional instrumentation restores constitutional coronal alignment. Knee Surg. Sports Traumatol. Arthrosc. 2024, 32, 3210–3219. [Google Scholar] [CrossRef] [PubMed]
- Winnock de Grave, P.; Luyckx, T.; Van Criekinge, T.; Müller, J.H.; Ollivier, B.; Van Eecke, E.; LiArno, S.; Faizan, A.; Claeys, K. Inverse kinematic alignment accommodates native coronal knee alignment better in comparison to adjusted mechanical alignment and restricted kinematic alignment. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 3765–3774. [Google Scholar] [CrossRef]
- Lustig, S.; Sappey-Marinier, E.; Fary, C.; Servien, E.; Parratte, S.; Batailler, C. Personalized alignment in total knee arthroplasty: Current concepts. SICOT-J. 2021, 7, 19. [Google Scholar] [CrossRef]
- Hiranaka, T. Current concept: Personalized alignment total knee arthroplasty as a contrast to classical mechanical alignment total knee arthroplasty. Arthroplasty 2024, 6, 23. [Google Scholar] [CrossRef]
- Rossi, S.M.P.; Benazzo, F. Individualized alignment and ligament balancing technique with the ROSA® robotic system for total knee arthroplasty. Int. Orthop. 2023, 47, 755–762. [Google Scholar] [CrossRef] [PubMed]
- Benazzo, F.; Ghiara, M.; Rossi, S.M.P.; Pruneri, E.; Tiwari, V.; Perelli, S. Clinical and radiological analysis of a personalized total knee arthroplasty system design. Int. Orthop. 2019, 43, 1113–1121. [Google Scholar] [CrossRef]
- Clark, G.W.; Steer, R.A.; Khan, R.N.; Collopy, D.M.; Wood, D. Maintaining joint line obliquity optimizes outcomes of functional alignment in total knee arthroplasty in patients with constitutionally varus knees. J. Arthroplast. 2023, 38, S239–S244. [Google Scholar] [CrossRef] [PubMed]
- Jeffrey, M.; Marchand, P.; Kouyoumdjian, P.; Coulomb, R. Short-term functional outcomes of robotic-assisted TKA are better with functional alignment compared to adjusted mechanical alignment. SICOT-J. 2024, 10, 2. [Google Scholar] [CrossRef] [PubMed]
- Parratte, S.; Van Overschelde, P.; Bandi, M.; Ozturk, B.Y.; Batailler, C. An anatomo-functional implant positioning technique with robotic assistance for primary TKA allows the restoration of the native knee alignment and a natural functional ligament pattern, with a faster recovery at 6 months compared to an adjusted mechanical technique. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 1334–1346. [Google Scholar]
- Arai, N.; Toyooka, S.; Masuda, H.; Kawano, H.; Nakagawa, T. Kinematic Alignment Achieves a More Balanced Total Knee Arthroplasty Than Mechanical Alignment among CPAK Type I Patients: A Simulation Study. J. Clin. Med. 2024, 13, 3596. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sosio, C.; Rossi, N.; Sirtori, P.; Ciliberto, R.; Lombardo, M.D.M.; Peretti, G.M.; Mangiavini, L. Clinical and Functional Outcomes of Kinematic Aligned Total Knee Arthroplasty with a Medial Pivot Design: Two-Year Follow-Up. J. Clin. Med. 2023, 12, 7258. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Corban, L.E.; van de Graaf, V.A.; Chen, D.B.; Wood, J.A.; Diwan, A.D.; MacDessi, S.J. How often do we alter constitutional limb alignment, joint line obliquity, and Coronal Plane Alignment of the Knee (CPAK) phenotype when performing mechanically aligned TKA?: A large single-institution retrospective radiological analysis. Bone Jt. Open 2024, 5, 109. [Google Scholar] [CrossRef]
- An, V.V.; Twiggs, J.; Leie, M.; Fritsch, B.A. Kinematic alignment is bone and soft tissue preserving compared to mechanical alignment in total knee arthroplasty. Knee 2019, 26, 466–476. [Google Scholar] [CrossRef]
- Agarwal, S.; Ayeni, F.E.; Sorial, R. Impact of change in coronal plane alignment of knee (CPAK) classification on outcomes of robotic-assisted TKA. Arthroplasty 2024, 6, 15. [Google Scholar] [CrossRef]
- Hirschmann, M.T.; Moser, L.B.; Amsler, F.; Behrend, H.; Leclercq, V.; Hess, S. Phenotyping the knee in young non-osteoarthritic knees shows a wide distribution of femoral and tibial coronal alignment. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 1385–1393. [Google Scholar] [CrossRef]
- Hess, S.; Moser, L.B.; Amsler, F.; Behrend, H.; Hirschmann, M.T. Highly variable coronal tibial and femoral alignment in osteoarthritic knees: A systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 1368–1377. [Google Scholar] [CrossRef]
- Nedopil, A.J.; Howell, S.M.; Hull, M.L. What clinical characteristics and radiographic parameters are associated with patellofemoral instability after kinematically aligned total knee arthroplasty? Int. Orthop. 2017, 41, 283–291. [Google Scholar] [CrossRef]
- Brown, W.; Gallagher, N.; Roberts, D.; Napier, R.; Barrett, D.; Beverland, D. The third gap–The forgotten space in total knee arthroplasty. Knee 2025, 52, 164–170. [Google Scholar] [CrossRef] [PubMed]
- Koutserimpas, C.; Andriollo, L.; Gregori, P.; Zambianchi, F.; Tsiridis, E.; Catani, F.; Lustig, S. Revisiting Terminology: The Transition from “functional Alignment” to “Functional Knee Positioning”. Knee Surg. Sports Traumatol. Arthrosc. Off. J. ESSKA 2025, 33, 1948–1953. [Google Scholar] [CrossRef] [PubMed]
- Andriollo, L.; Mazzella, G.G.; Koutserimpas, C.; Gregori, P.; Servien, E.; Batailler, C.; Lustig, S. Functional Positioning in Robotic Medial Unicompartmental Knee Arthroplasty: A Step-by-Step Technique. SICOT-J. 2025, 11, 34. [Google Scholar] [CrossRef] [PubMed]
- Andriollo, L.; Koutserimpas, C.; Gregori, P.; Baltzer, J.; Servien, E.; Batailler, C.; Lustig, S. Functional Positioning in Robotic Patello-Femoral Arthroplasty: A Step-by-Step Technique. SICOT-J. 2025, 11, 35. [Google Scholar] [CrossRef]
- Andriollo, L.; Koutserimpas, C.; Gregori, P.; Servien, E.; Batailler, C.; Lustig, S. Beyond the Coronal Plane in Robotic Total Knee Arthroplasty-Part 1: Variations in Tibial Slope and Distal Femoral Flexion Do Not Affect Outcomes. Knee Surg. Sports Traumatol. Arthrosc. Off. J. ESSKA 2025, 33, 2928–2938. [Google Scholar] [CrossRef]
- Andriollo, L.; Gregori, P.; Koutserimpas, C.; Servien, E.; Batailler, C.; Lustig, S. Beyond the Coronal Plane in Robotic Total Knee Arthroplasty-Part 2: Combined Flexion Does Not Affect Outcomes. Knee Surg. Sports Traumatol. Arthrosc. Off. J. ESSKA 2025, 33, 2939–2949. [Google Scholar] [CrossRef]
- Andriollo, L.; Koutserimpas, C.; Gregori, P.; Servien, E.; Batailler, C.; Lustig, S. A New Parameter in the Era of Robotic Total Knee Arthroplasty: Coronal Alignment at 90° of Flexion Impacts Clinical Outcomes. Knee Surg. Sports Traumatol. Arthrosc. Off. J. ESSKA 2025, 33, 2581–2591. [Google Scholar] [CrossRef]
- Vermue, H.; Andriollo, L.; Servien, E.; Batailler, C.; Lustig, S. Functional Knee Positioning in Total Knee Arthroplasty: Rationale and Current Evidence. J. Jt. Surg. Res. 2025. [Google Scholar] [CrossRef]
- Simon, J.M.; Bauer, L.; Thorwächter, C.; Woiczinski, M.; Simon, F.; Müller, P.E.; Holzapfel, B.M.; Niethammer, T.R. The Influence of Kinematic Alignment on Patellofemoral Joint Biomechanics in Total Knee Arthroplasty. J. Clin. Med. 2024, 13, 6894. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hsieh, S.L.; Lin, T.L.; Hung, C.H.; Fong, Y.C.; Chen, H.T.; Tsai, C.H. Clinical and Radiographic Outcomes of Inversed Restricted Kinematic Alignment Total Knee Arthroplasty by Asia Specific (Huang’s) Phenotypes, a Prospective Pilot Study. J. Clin. Med. 2023, 12, 2110. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
| Approach | Principle | Advantages | Limitations |
|---|---|---|---|
| Mechanical Alignment (MA) | Restores neutral HKA = 180°, cuts perpendicular to mechanical axes. | Standardized, strong long-term survival data, implant longevity. | Does not respect native anatomy in most patients, ~10% dissatisfaction. |
| Anatomical Alignment (AA) | Reproduces the anatomical axis with physiological joint line obliquity. | Respects native anatomy, improves patellofemoral biomechanics. | Historically associated with polyethylene wear, requires high surgical accuracy. |
| Kinematic Alignment (KA) | Recreates pre-arthritic patient-specific alignment (“true resurfacing”). | Ligament-sparing, bone-preserving, improved ROM, satisfaction, and pain relief. | Safe zones not standardized, limited long-term data. |
| Adjusted Mechanical Alignment (aMA) | Maintains up to 3° of constitutional deformity, reducing releases. | More personalized than MA, reduces non-physiological resections. | Still requires non-anatomical resections in many cases, potential dissatisfaction. |
| Restricted Kinematic Alignment (rKA) | KA within defined safety boundaries (±5° from mechanical axes). | Compromise between personalization and safety, higher satisfaction rates. | Mid- to long-term outcomes still under investigation. |
| Inverse Kinematic Alignment (iKA) | “Tibia-first” technique restoring tibial joint line obliquity. | Precise with robotic assistance, better patellofemoral outcomes. | Novel approach, limited long-term validation. |
| Functional Alignment (FA) | Focus on real-time ligament balancing with robotic/navigation guidance. | 3D individualized alignment, fewer releases, favorable early outcomes. | Requires advanced technology, higher costs, learning curve. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cinelli, V.; Marescalchi, M.; Picchi, A.; De Mattia, G.; Andriollo, L.; Fidanza, A.; Logroscino, G.; Sangaletti, R.; Benazzo, F.; Rossi, S.M.P. Total Knee Arthroplasty and the Evolution of Coronal Alignment: From Mechanical to Personalized Strategies. J. Pers. Med. 2025, 15, 524. https://doi.org/10.3390/jpm15110524
Cinelli V, Marescalchi M, Picchi A, De Mattia G, Andriollo L, Fidanza A, Logroscino G, Sangaletti R, Benazzo F, Rossi SMP. Total Knee Arthroplasty and the Evolution of Coronal Alignment: From Mechanical to Personalized Strategies. Journal of Personalized Medicine. 2025; 15(11):524. https://doi.org/10.3390/jpm15110524
Chicago/Turabian StyleCinelli, Virginia, Marina Marescalchi, Aurelio Picchi, Gerardo De Mattia, Luca Andriollo, Andrea Fidanza, Giandomenico Logroscino, Rudy Sangaletti, Francesco Benazzo, and Stefano Marco Paolo Rossi. 2025. "Total Knee Arthroplasty and the Evolution of Coronal Alignment: From Mechanical to Personalized Strategies" Journal of Personalized Medicine 15, no. 11: 524. https://doi.org/10.3390/jpm15110524
APA StyleCinelli, V., Marescalchi, M., Picchi, A., De Mattia, G., Andriollo, L., Fidanza, A., Logroscino, G., Sangaletti, R., Benazzo, F., & Rossi, S. M. P. (2025). Total Knee Arthroplasty and the Evolution of Coronal Alignment: From Mechanical to Personalized Strategies. Journal of Personalized Medicine, 15(11), 524. https://doi.org/10.3390/jpm15110524






