Surgical Outcomes of Craniocervical Junction Fractures in Elderly Patients: A Retrospective Single-Center Series
Abstract
1. Introduction
1.1. Anatomy of Craniocervical Junction (CCJ)
1.2. Cause of CCJ Fractures and Surgical Treatment
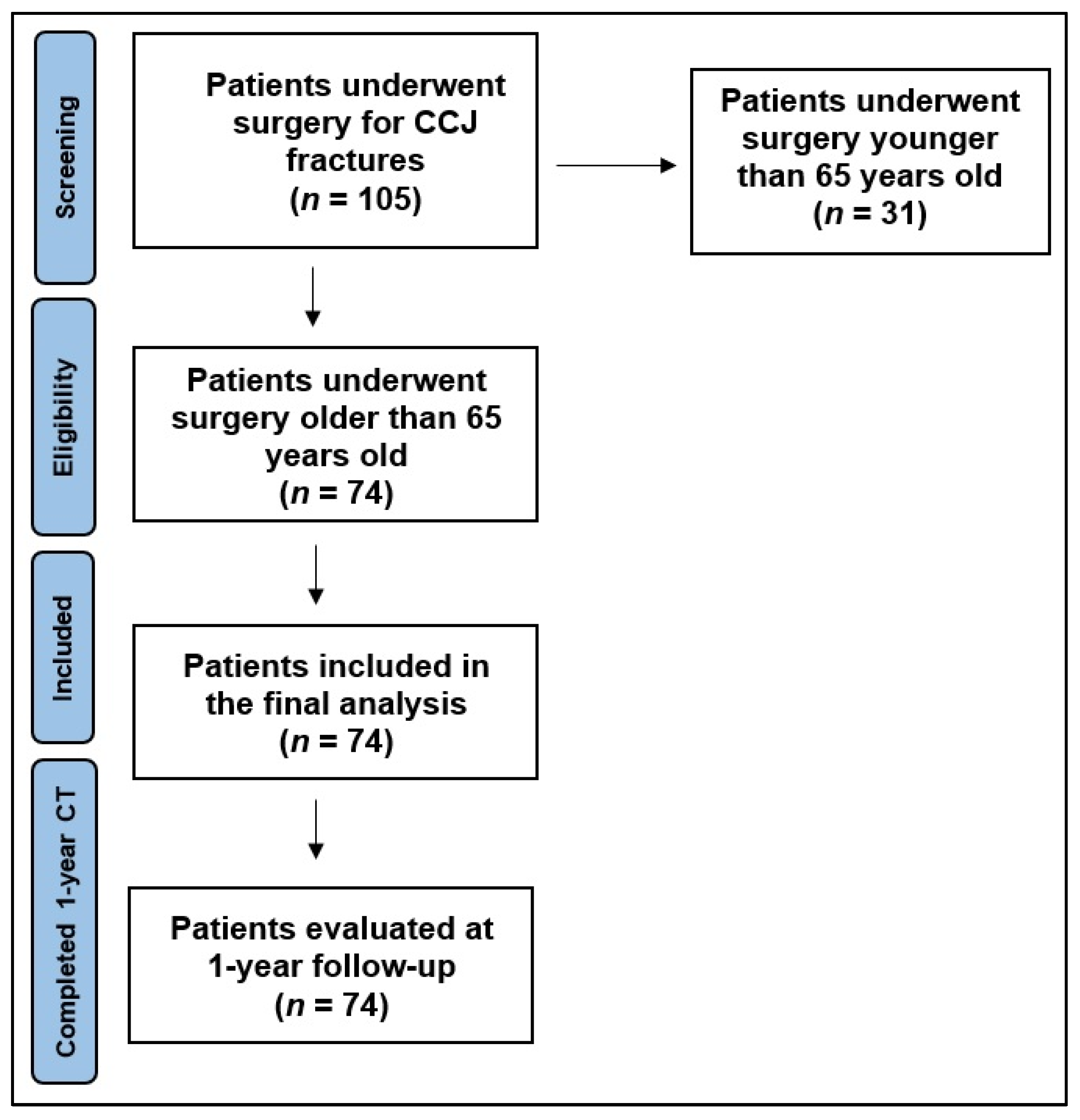
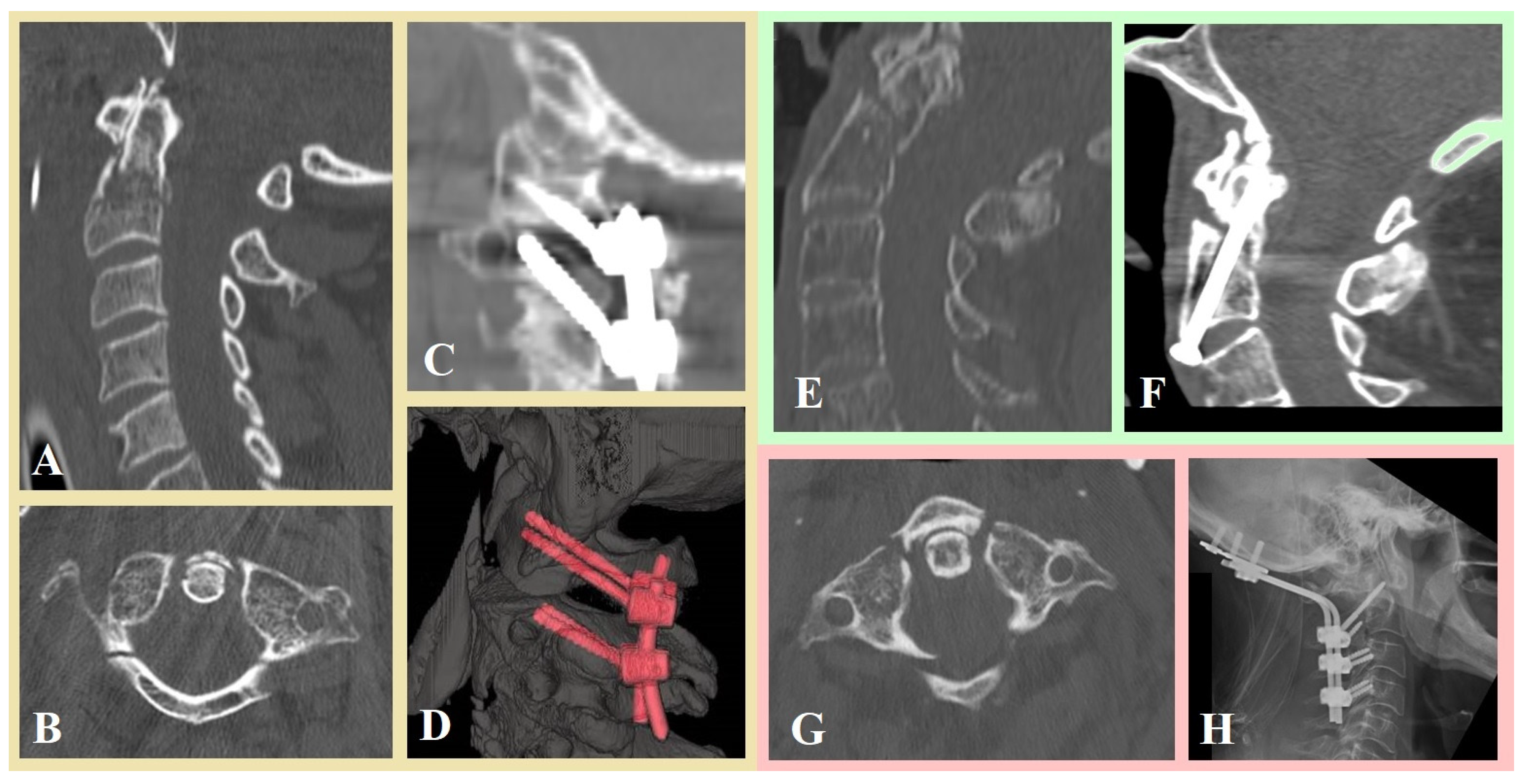
2. Materials and Methods
2.1. Patient Population
2.2. Surgical Outcome
2.3. Statistical Analysis
3. Results
Statistical Analysis on Clinical and Fusion Rate Outcome
4. Discussion
4.1. Functional Outcomes
4.2. Mortality
4.3. Fusion Rates
4.4. Study Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tinner, C.; Aregger, F.C.; Deml, M.C. Transoral unilateral lag screw osteosynthesis for coronal split fracture of the lateral mass of the atlas–case report, operative technique and review of the literature. Brain Spine 2023, 3, 101761. [Google Scholar] [CrossRef]
- Unni, C.; Pettakkandy, V.; Soren, S.K.J. Atlantoaxial Stabilization by Posterior C1 and C2 Screw-Rod Fixation for Various Pathologies: Case Series and Comprehensive Review of Literature. J. Neurosci. Rural Pract. 2021, 12, 228–235. [Google Scholar] [CrossRef] [PubMed]
- Lu, M.; Wang, Z.; Yuan, B.; Tang, Y.; Gu, C.; Zhou, S.; Chen, X. The C2 isthmus screw provided sufficient biomechanical stability in the setting of atlantoaxial dislocation-a finite element study. BMC Musculoskelet. Disord. 2024, 25, 423. [Google Scholar] [CrossRef]
- Henderson, J.J. The epidemiology of fractures and fracture-dislocations of the cervical spine. Injury 1992, 23, 38–40. [Google Scholar] [CrossRef] [PubMed]
- Goel, A. Vertical facetal instability: Is it the point of genesis of spinal spondylotic disease? J. Craniovertebral Junction Spine 2015, 6, 47–48. [Google Scholar] [CrossRef] [PubMed]
- Avila, M.J.; Farber, S.H.; Rabah, N.M.; Hopp, M.J.; Chapple, K.M.; Hurlbert, R.J.; Tumialán, L.M. Nonoperative versus operative management of type II odontoid fracture in older adults: A systematic review and meta-analysis. J. Neurosurg. Spine 2023, 40, 45–53. [Google Scholar] [CrossRef]
- Goel, A. Artificial atlantoaxial and subaxial facetal joint—Proposal of models. J. Craniovertebral Junction Spine 2022, 13, 107–109. [Google Scholar] [CrossRef]
- Salunke, P.; Karthigeyan, M.; Kodigudla, M.K.; Kelkar, A.V.; Goel, V.K. C1-C2 arthroplasty for craniovertebral junction instability: A preliminary proof of concept in human cadavers. J. Craniovertebral Junction Spine 2022, 13, 159–162. [Google Scholar] [CrossRef]
- Nouri, A.; Da Broi, M. Odontoid Fractures: A review of the current State of the Art. J. Clin. Med. 2024, 13, 12. [Google Scholar] [CrossRef]
- Jo, W.R.; Lee, C.Y.; Kwon, S.M.; Kim, C.H.; Kwon, M.Y.; Kim, J.H.; Ko, Y.S. Does the Surgical Approach Matter in Treating Odontoid Fractures? A Comparison of Mechanical Complication Rates Between Anterior Versus Posterior Surgical Approaches: A Meta-Analysis and Systematic Review. Korean J. Neurotrauma 2023, 19, 409–421. [Google Scholar] [CrossRef]
- Leonhardt, L.G.; Münch, M.; Schroeder, M.; Dirks, M.; Kleinertz, H.; Kammal, A.L.; Ondruschka, B.; von Kroge, S.; Rolvien, T.; Frosch, K.H.; et al. Geriatric Type II Fractures of the Dens Axis: Biomechanical Superiority of a New Osteosynthesis Plate Compared to Common Anterior Screw Fixation. Glob. Spine J. 2025, 29, 21925682251338814. [Google Scholar] [CrossRef]
- Montemurro, N.; Perrini, P.; Mangini, V.; Galli, M.; Papini, A. The Y-shaped trabecular bone structure in the odontoid process of the axis: A CT scan study in 54 healthy subjects and biomechanical considerations. J. Neurosurg. Spine 2019, 30, 585–592. [Google Scholar] [CrossRef]
- Davidson, C.T.; Bergin, P.F.; Varney, E.T.; Jones, L.C.; Ward, M.S. Planning C2 pedicle screw placement with multiplanar reformatted cervical spine computed tomography. J. Craniovertebral Junction Spine 2019, 10, 46–50. [Google Scholar] [CrossRef]
- Perrini, P.; Montemurro, N. Congenital absence of a cervical spine pedicle. Neurol. India 2016, 64, 189–190. [Google Scholar] [CrossRef] [PubMed]
- Umana, G.E.; Scalia, G.; Ricciardi, L.; Lofrese, G.; Mongardi, L.; Montemurro, N.; Acerbi, F.; Strigari, L.; Cardozo, M.R.; Capo, G.; et al. Surgical strategies and outcomes in degenerative myelopathy at the cervico-thoracic junction: A multicenter retrospective analysis. Eur. Spine J. 2025, 34, 3453–3463. [Google Scholar] [CrossRef] [PubMed]
- Amling, M.; Pösl, M.; Wening, V.J.; Ritzel, H.; Hahn, M.; Delling, G. Structural heterogeneity within the axis: The main cause in the etiology of dens fractures. A histomorphometric analysis of 37 normal and osteoporotic autopsy cases. J. Neurosurg. 1995, 83, 330–335. [Google Scholar] [CrossRef]
- Chibbaro, S.; Mallereau, C.-H.; Ganau, M.; Zaed, I.; Bozzi, M.T.; Scibilia, A.; Cebula, H.; Ollivier, I.; Loit, M.-P.; Chaussemy, D.; et al. Odontoid Type II fractures in elderly: What are the real management goals and how to best achieve them? A multicenter European study on functional outcome. J. Neurosurg. Rev. 2022, 45, 709–718. [Google Scholar] [CrossRef]
- Barrey, C.Y.; di Bartolomeo, A.; Barresi, L.; Bronsard, N.; Allia, J.; Blondel, B.; Fuentes, S.; Nicot, B.; Challier, V.; Godard, J.; et al. C1–C2 Injury: Factors influencing mortality, outcome, and fracture healing. Eur. Spine J. 2021, 30, 1574–1584. [Google Scholar] [CrossRef]
- Rizvi, S.A.M.; Helseth, E.; Rønning, P.; Mirzamohammadi, J.; Harr, M.E.; Brommeland, T.; Aarhus, M.; Høstmælingen, C.T.; Ølstørn, H.; Rydning, P.N.F.; et al. Odontoid fractures: Impact of age and comorbidities on surgical decision making. BMC Surg. 2020, 20, 236. [Google Scholar] [CrossRef]
- Montemurro, N.; Cocciaro, A.; Liberti, G.; Cosottini, M.; Perrini, P. The Internal Trabecular Bone Structure of the Odontoid Process of the Axis: A Retrospective Single-Center Comparative Study in Patients Following Cervical Trauma. J. Neurol. Surg. A Cent. Eur. Neurosurg. 2025, 86, 417–422. [Google Scholar] [CrossRef] [PubMed]
- Anderson, L.D.; D’Alonzo, R.T. Fractures of the odontoid process of the axis. J. Bone Jt. Surg. Am. 1974, 56, 1663–1674. [Google Scholar] [CrossRef]
- Wagner, S.C.; Schroeder, G.D.; Kepler, C.K.; Schupper, A.J.; Kandziora, F.; Vialle, E.N. Controversies in the management of geriatric odontoid fractures. J. Orthop. Trauma 2017, 4, S44–S48. [Google Scholar] [CrossRef]
- Fehlings, M.G.; Tetreault, L.; Nater, A.; Choma, T.; Harrop, J.; Mroz, T. The Aging of the Global Population: The Changing Epi-demiology of Disease and Spinal Disorders. Neurosurgery 2015, 4, S1–S5. [Google Scholar] [CrossRef]
- Iyer, S.; Hurlbert, R.J.; Albert, T.J. Management of Odontoid Fractures in the Elderly: A Review of the Literature and an Evi-dence-Based Treatment Algorithm. Neurosurgery 2018, 82, 419–430. [Google Scholar] [CrossRef]
- Canseco, J.A.; Schroeder, G.D.; Patel, P.D.; Grasso, G.; Chang, M.; Kandziora, F. Regional and experiential differences in surgeon preference for the treatment of cervical facet injuries: A case study survey with the AO Spine Cervical Classification Validation Group. Eur. Spine J. 2021, 30, 517–523. [Google Scholar] [CrossRef] [PubMed]
- Schroeder, G.D.; Canseco, J.A.; Patel, P.D.; Divi, S.N.; Karamian, B.A.; Kandziora, F. Establishing the Injury Severity of Subaxial Cervical Spine Trauma: Validating the Hierarchical Nature of the AO Spine Subaxial Cervical Spine Injury Classification System. Spine 2021, 46, 649–657. [Google Scholar] [CrossRef]
- Shafafy, R.; Valsamis, E.M.; Luck, J.; Dimock, R.; Rampersad, S.; Kieffer, W.; Morassi, G.L.; Elsayed, S. Predictors of mortality in the elderly patient with a fracture of the odontoid process. Bone Jt. J. 2019, 101, 253–259. [Google Scholar] [CrossRef] [PubMed]
- Rizvi, S.A.M.; Helseth, E.; Harr, M.E.; Mirzamohammadi, J.; Rønning, P.; Mejlænder-Evjensvold, M.; Linnerud, H. Management and long-term outcome of type II acute odontoid fractures: A population-based consecutive series of 282 patients. Spine J. 2021, 21, 627–637. [Google Scholar] [CrossRef]
- Liu, J.; Liu, S.; Jiang, E.; Tan, Y.; Bao, X.; Niu, D.; Guo, C.; Qi, J.; Shi, Z.; Xu, G. Clinical and Radiographic Outcomes of Modified Posterior Atlantoaxial Temporary Fixation with Preservation of Semispinalis Cervicis: A Comparative Study. Glob. Spine J. 2024, 14, 272–282. [Google Scholar] [CrossRef]
- Magerl, F.; Seemann, P. Stable posterior fusion of the atlas and axis by transarticular screw fixation. In Cervical Spine; Society CSR, Ed.; Springer-Verlag: New York, NY, USA, 1986; Volume 1, pp. 322–327. [Google Scholar]
- Harms, J.; Melcher, R.P. Posterior C1–C2 fusion with polyaxial screw and rod fixation. Spine 2001, 26, 2467–2471. [Google Scholar] [CrossRef]
- Sakti, Y.M.; Lanodiyu, Z.A.; Wijanarko, S.; Alhaq, Z.A.; Sakadewa, G.P.; Ahmad, H.; Desfiandi, P.; Magetsari, R. Occipitocervical fixation: A case report of our techniques and results. Int. J. Surg. Case Rep. 2022, 90, 106633. [Google Scholar] [CrossRef]
- Finn, M.A.; MacDonald, J.D. C2–C3 Anterior Cervical Fusion: Technical Report. Clin. Spine Surg. 2016, 29, E536–E541. [Google Scholar] [CrossRef]
- Vaccaro, A.R.; Lambrechts, M.J.; Karamian, B.A.; Canseco, J.A.; Oner, C.; Vialle, E.; Rajasekaran, S.; Dvorak, M.R.; Benneker, L.M.; Kandziora, F.; et al. AO Spine upper cervical injury classification system: A description and reliability study. Spine J. 2022, 22, 2042–2049. [Google Scholar] [CrossRef] [PubMed]
- Vaccaro, A.R.; Lambrechts, M.J.; Karamian, B.A.; Canseco, J.A.; Oner, C.; Benneker, L.M.; Bransford, R.; Kandziora, F.; Shanmuganathan, R.; El-Sharkawi, M.; et al. Global Validation of the AO Spine Upper Cervical Injury Classification. Spine 2022, 47, 1541–1548. [Google Scholar] [CrossRef] [PubMed]
- Lambrechts, M.J.; Schroeder, G.D.; Karamian, B.A.; Canseco, J.A.; Oner, F.C.; Benneker, L.M.; Bransford, R.J.; Kandziora, F.; Rajasekaran, S.; El-Sharkawi, M.; et al. Effect of surgical experience and spine subspecialty on the reliability of the AO Spine Upper Cervical Injury Classification System. J. Neurosurg. Spine 2022, 38, 31–41. [Google Scholar] [CrossRef]
- American Spinal Injury Association. International Standards for Neurological Chandramohan Classifications of Spinal Cord Injury, 2nd ed.; American Spinal Injury Association: Chicago, IL, USA, 2000; Volume 1, pp. 1–23. [Google Scholar]
- Delgado, D.A.; Lambert, B.S.; Boutris, N.; McCulloch, P.C.; Robbins, A.B.; Moreno, M.R.; Harris, J.D. Validation of Digital Visual Analog Scale Pain Scoring With a Traditional Paper-based Visual Analog Scale in Adults. J. Am. Acad. Orthop. Surg. Glob. Res. Rev. 2018, 2, e088. [Google Scholar] [CrossRef]
- MacDermid, J.C.; Walton, D.M.; Avery, S.; Blanchard, A.; Etruw, E.; McAlpine, C.; Goldsmith, C.H. Measurement properties of the neck disability index: A systematic review. J. Orthop. Sports Phys. Ther. 2009, 39, 400–417. [Google Scholar] [CrossRef] [PubMed]
- Dolp, A.; Khamis, A.; Fandino, J.; Kienzler, J.C. Clinical and Radiological Outcome of Posterior Cervical Fusion Using Philips AlluraXper FD20 Angiography Suite. Brain Sci. 2025, 15, 160. [Google Scholar] [CrossRef]
- Soriano Sánchez, J.A.; Soriano Solís, S.; Soto García, M.E.; Soriano Solís, H.A.; Torres, B.Y.A.; Romero Rangel, J.A.I. Radiological diagnostic accuracy study comparing Lenke, Bridwell, BSF, and CT-HU fusion grading scales for minimally invasive lumbar interbody fusion spine surgery and its correlation to clinical outcome. Medicine 2020, 99, e19979. [Google Scholar] [CrossRef]
- Jang, H.J.; Kim, K.H.; Park, J.Y.; Kim, K.S.; Cho, Y.E.; Chin, D.K. Endplate-specific fusion rate 1 year after surgery for two-level anterior cervical discectomy and fusion(ACDF). Acta Neurochir. 2022, 164, 3173–3180. [Google Scholar] [CrossRef]
- Bridwell, K.H.; Lenke, L.G.; McEnery, K.W.; Baldus, C.; Blanke, K. Anterior fresh frozen structural allografts in the thoracic and lumbar spine. Do they work if combined with posterior fusion and instrumentation in adult patients with kyphosis or anterior column defects? Spine 1995, 20, 1410–1418. [Google Scholar] [CrossRef]
- Lenke, L.G.; Bridwell, K.H.; Bullis, D.; Betz, R.R.; Baldus, C.; Schoenecker, P.L. Results of in situ fusion for isthmic spondylo-lis-thesis. Clin. Spine Surg. 1992, 5, 433–442. [Google Scholar]
- Kleinstück, F.S.; Fekete, T.F.; Loibl, M.; Jeszenszky, D.; Haschtmann, D.; Porchet, F.; Mannion, A.F. Patient-rated outcome after atlantoaxial (C1-C2) fusion: More than a decade of evaluation of 2-year outcomes in 126 patients. Eur. Spine J. 2021, 30, 3620–3630. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Kim, E.S.; Sung, J.K.; Park, Y.M.; Eoh, W.J. Clinical and radiological comparison of treatment of atlantoaxial instability by posterior C1–C2 transarticular screw fixation or C1 lateral mass-C2 pedicle screw fixation. Clin. Neurosci. 2010, 17, 886–892. [Google Scholar] [CrossRef] [PubMed]
- Zou, X.; Cai, M.; Yang, H.; Zhang, S.; Deng, C.; Chen, J.; Ma, R.; Chen, Z.; Xia, H.; Ma, X. Transoral atlantoaxial reduction plate (TARP) technique for the treatment of irreducible atlantoaxial dislocation (IAAD) caused by old odontoid fracture. Glob. Spine J. 2024, 15, 2340–2347. [Google Scholar] [CrossRef]
- Montemurro, N.; Carnesecchi, S. Is Direct Transpedicular C2 Fixation (Judet Approach) a Timeless Technique to Learn for C2 Fractures? Glob. Spine J. 2025, 11, 21925682251367412. [Google Scholar] [CrossRef]
- von der Höh, N.H.; Keuchel, J.; Pieroh, P.; Spiegl, U.J.A.; Osterhoff, G.; Heyde, C.E. Inpatient outcomes of upper cervical fractures in the elderly: A retrospective analysis of 268 cases. BMC Geriatr. 2025, 25, 237. [Google Scholar] [CrossRef]
- Franke, A.; Bieler, D.; Wern, R.; Trotzke, T.; Hentsch, S.; Kollig, E. Anterior management of C2 fractures using miniplate fixation: Outcome, function and quality of life in a case series of 15 patients. Eur. Spine J. 2018, 27, 1332–1341. [Google Scholar] [CrossRef]
- Gembruch, O.; Ahmadipour, Y.; Lemonas, E.; Müller, O. The Anterior Transarticular Fixation of C1/C2 in the Elderly with Dens Fractures. Int. J. Spine Surg. 2020, 14, 162–169. [Google Scholar] [CrossRef]
- Jain, A.K.; Tawari, M.; Rathore, L.; Sahana, D.; Mishra, H.; Kumar, S.; Sahu, R.K. An experience with Goel-Harms C1-C2 fixation for type II odontoid fractures. J. Craniovertebral Junction Spine 2022, 13, 175–181. [Google Scholar] [CrossRef]
- Scarola, R.; Montemurro, N.; Ferrara, E.; Corsalini, M.; Converti, I.; Rapone, B. Temporomandibular Disorders and Fibromyalgia: A Narrative Review. Open Access Maced. J. Med. Sci. 2021, 9, 106–112. [Google Scholar] [CrossRef]
- Sander, A.L.; El Saman, A.; Delfosse, P.; Wutzler, S.; Meier, S.; Marzi, I.; Laurer, H. Cervical spine fractures in the elderly: Morbidity and mortality after operative treatment. Eur. J. Trauma Emerg. Surg. 2013, 39, 469–476. [Google Scholar] [CrossRef]
- De Bonis, P.; Iaccarino, C.; Musio, A.; Martucci, A.; De Iure, F.; Donati, R.; Cultrera, F.; Tosatto, L.; Servadei, F.; Alesi, D.; et al. Functional Outcome of Elderly Patients Treated for Odontoid Fracture: A Multicenter Study. Spine 2019, 44, 951–958. [Google Scholar] [CrossRef]
- Sasagawa, T.; Yokogawa, N.; Hayashi, H.; Tsuchiya, H.; Ando, K.; Nakashima, H.; Segi, N.; Watanabe, K.; Nori, S.; Takeda, K.; et al. A multicenter study of 1-year mortality and walking capacity after spinal fusion surgery for cervical fracture in elderly patients. BMC Musculoskelet. Disord. 2022, 23, 798. [Google Scholar] [CrossRef]
- Harrop, J.S.; Hart, R.; Anderson, P.A. Optimal treatment for odontoid fractures in the elderly. Spine 2010, 35, S219–S227. [Google Scholar] [CrossRef] [PubMed]
- Reyes-Soto, G.; Corona De la Torre, A.; Honda Partida, K.G.; Nurmukhametov, R.; Encarnacion Ramirez, M.J.; Montemurro, N. Clivus-Cervical Stabilization through Transoral Approach in Patients with Craniocervical Tumor: Three Cases and Surgical Technical Note. Brain Sci. 2024, 14, 254. [Google Scholar] [CrossRef] [PubMed]
- Ramirez, M.J.E.; Montemurro, N.; Musa, G.; Chmutin, G.E.; Nurmukhametov, R.; Rosario, A.R.; Barza, J.L.; Kaprovoy, S.; Konovalov, N.; Kudriavtsev, D.; et al. On the balance beam: Facing the challenges of neurosurgical education in the third mil-lennium. Surg. Neurol. Int. 2024, 15, 102. [Google Scholar] [CrossRef]
- De Jesus Encarnacion Ramirez, M.; Chmutin, G.; Nurmukhametov, R.; Soto, G.R.; Kannan, S.; Piavchenko, G.; Nikolenko, V.; Efe, I.E.; Romero, A.R.; Mukengeshay, J.N.; et al. Integrating Augmented Reality in Spine Surgery: Redefining Precision with New Technologies. Brain Sci. 2024, 14, 645. [Google Scholar] [CrossRef]
- Delcourt, T.; Bégué, T.; Saintyves, G.; Mebtouche, N.; Cottin, P. Management of upper cervical spine fractures in elderly patients: Current trends and outcomes. Injury 2015, 46, S24–S27. [Google Scholar] [CrossRef]
- Chen, Y.R.; Boakye, M.; Arrigo, R.T.; Kalanithi, P.S.; Cheng, I.; Alamin, T.; Carragee, E.J.; Mindea, S.A.; Park, J. Morbidity and mortality of C2 fractures in the elderly: Surgery and conservative treatment. Neurosurgery 2012, 70, 1055–1059. [Google Scholar] [CrossRef]
- Chan, H.H.; Segreto, F.A.; Horn, S.R.; Bortz, C.; Choy, G.G.; Passias, P.G.; Deverall, H.H.; Baker, J.F. Fractures in the Elderly: Single-Center Evaluation of Risk Factors for Mortality. Asian Spine J. 2019, 13, 746–752. [Google Scholar] [CrossRef]
- Zanin, L.; Broglio, L.; Panciani, P.P.; Bergomi, R.; De Rosa, G.; Ricciardi, L.; Guzzi, G.; Fiorindi, A.; Brembilla, C.; Restelli, F.; et al. Intraoperative Neurophysiological Monitoring in Contemporary Spinal Surgery: A Systematic Review of Clinical Outcomes and Cost-Effectiveness. Brain Sci. 2025, 15, 768. [Google Scholar] [CrossRef]
- Dobran, M.; Nasi, D.; Esposito, D.P.; Iacoangeli, M. Posterior Fixation with C1 Lateral Mass Screws and C2 Pars Screws for Type II Odontoid Fracture in the Elderly: Long-Term Follow-Up. World Neurosurg. 2016, 96, 152–158. [Google Scholar] [CrossRef]
- Barbagallo, G.M.V.; Certo, F.; Vitaliti, C.; Bonomo, G. Neuronavigation-guided Judet screw technique for C2 pedicle fractures: How I do it. Acta Neurochir. 2025, 167, 69. [Google Scholar] [CrossRef] [PubMed]
- Montemurro, N.; Scerrati, A.; Ricciardi, L.; Trevisi, G. The Exoscope in Neurosurgery: An Overview of the Current Literature of Intraoperative Use in Brain and Spine Surgery. J. Clin. Med. 2021, 11, 223. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.; Chen, F.; Mo, J.; Lin, T.; Wang, Z.; Liu, W. Cervical Spine Microsurgery with the High-Definition 3D Exoscope: Ad-vantages and Disadvantages. World Neurosurg. 2022, 161, e1–e7. [Google Scholar] [CrossRef] [PubMed]
| Fusion Grade | Description of Fusion |
|---|---|
| A | Solid, big trabeculated fusions bilaterally |
| B | Solid unilateral fusion with small contralateral aspect |
| C | Small thin fusion masses bilaterally with possible crack |
| D | Graft resorption bilaterally or bilateral pseudoarthrosis |
| n° (%) | |
|---|---|
| Patients | 74 (100) |
| Age (mean) | 76.9 |
| Sex | |
| Male | 33 (44.6) |
| Female | 41 (55.4) |
| Type of fracture | |
| type II | 6 (8.1) |
| type III | 68 (91.1) |
| ASIA scale | |
| Asia C | 2 (2.7) |
| Asia E | 72 (97.3) |
| Positive CT head scan for SAH or IH | 20 (27) |
| Stay in hospital (mean, days) | 10.6 |
| Follow-up (mean, months) | 15 |
| n° (%) | |
|---|---|
| Surgical treatment | 74 (100) |
| C2 dens screwing | 22 (29.7) |
| C2–C3 discectomy and fixation with plate | 8 (10.8) |
| Occipitocervical fixation | 11 (14.9) |
| C1–C2 fixation Harms technique | 25 (33.8) |
| C1–C2 fixation Magerl technique | 8 (10.8) |
| Postoperative complications | 9 (12.2) |
| wound infection | 5 (6.8) |
| postoperative hematoma | 1 (1.4) |
| vein thrombosis | 3 (4.1) |
| Clinical outcome | |
| VAS (mean) | 2.95 |
| NDI (mean) | 5.9% |
| Radiological outcome (Lenke et al. [44]) | |
| Fusion grade A–B | 53 (71.6) |
| Fusion grade C–D | 21 (28.4) |
| Mortality | |
| at 3 months | 3 (4.1%) |
| at 1 year | 13 (17.6) |
| Postoperative Complications | Mortality at 1-Year FU | Fusion Rate | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Prognostic Factors | No | Yes | p-Value | No | Yes | p-Value | Fusion Grade C–D | Fusion Grade A–B | p-Value |
| Gender | 0.969 | 0.624 | 0.850 | ||||||
| Male | 29 | 4 | 28 | 5 | 9 | 24 | |||
| Female | 36 | 5 | 33 | 8 | 12 | 29 | |||
| Age | 0.257 | 0.496 | 0.285 | ||||||
| <80 y.o. | 42 | 4 | 39 | 7 | 11 | 35 | |||
| ≥80 y.o. | 23 | 5 | 22 | 6 | 10 | 18 | |||
| Type of fractures (yes) | |||||||||
| Type II, type B | 3 | 1 | 0.428 | 4 | 0 | 0.342 | 2 | 2 | 0.324 |
| Type II, type C | 2 | 0 | 0.706 | 0 | 2 | 0.002 | 0 | 2 | 0.367 |
| Type III, type B | 43 | 4 | 0.218 | 41 | 6 | 0.190 | 10 | 36 | 0.104 |
| Type III, type C | 17 | 4 | 0.267 | 16 | 5 | 0.374 | 9 | 12 | 0.082 |
| Surgical treatment (yes) | |||||||||
| Occipitocervical fixation | 9 | 2 | 0.522 | 8 | 3 | 0.359 | 2 | 9 | 0.416 |
| C2 dens screwing | 19 | 3 | 0.823 | 18 | 4 | 0.928 | 9 | 13 | 0.120 |
| C1–C2 fixation Harms | 22 | 3 | 0.975 | 20 | 5 | 0.694 | 5 | 20 | 0.253 |
| C1–C2 fixation Magerl | 7 | 1 | 0.988 | 7 | 1 | 0.690 | 2 | 6 | 0.822 |
| C2–C3 anterior fixation | 8 | 0 | 0.261 | 8 | 0 | 0.167 | 3 | 5 | 0.545 |
| Surgical approach | 0.613 | 0.429 | 0.067 | ||||||
| Posterior | 38 | 6 | 35 | 9 | 9 | 35 | |||
| Anterior | 27 | 3 | 26 | 4 | 12 | 18 | |||
| VAS | NDI | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Univariate Analysis | Multivariate Analysis * | Univariate Analysis | Multivariate Analysis * | |||||||
| Prognostic Factors | Mean | sd | p-Value | RC | p-Value | Mean | sd | p-Value | RC | p-Value |
| Age | ||||||||||
| <80 | 2.85 | 1.32 | 0.381 | 4.93 | 3.85 | 0.013 | 3.08 (1.17; 4.98) | 0.002 | ||
| ≥80 | 3.11 | 1.07 | 7.54 | 4.90 | ||||||
| Gender | ||||||||||
| Male | 2.94 | 1.37 | 0.967 | 6.12 | 4.04 | 0.727 | ||||
| Female | 2.95 | 1.12 | 5.76 | 4.76 | ||||||
| Type of fracture (yes) | ||||||||||
| Type II, type B | 4.25 | 1.26 | 0.028 | 0.66 (−0.36; 1.67) | 0.199 | 5.00 | 1.63 | 0.673 | ||
| Type II, type C | 3.50 | 2.12 | 0.521 | 14.50 | 9.19 | 0.005 | 8.67 (2.67; 14.7) | < 0.005 | ||
| Type III, type B | 3.04 | 1.23 | 0.384 | 5.72 | 4.43 | 0.619 | ||||
| Type III, type C | 2.52 | 0.93 | 0.062 | 5.71 | 3.91 | 0.805 | ||||
| SAH or IH at CT scan | ||||||||||
| no | 2.98 | 1.25 | 0.626 | 5.38 | 3.76 | 0.045 | 1.67 (−0.67; 4.02) | 0.160 | ||
| yes | 2.81 | 1.17 | 7.88 | 6.05 | ||||||
| Surgical treatment (yes) | ||||||||||
| Occipitocervical fixation | 3.64 | 0.67 | 0.042 | 0.10 (−0.60; 0.80) | 0.770 | 7.27 | 6.15 | 0.275 | ||
| C2 dens screwing | 2.05 | 0.95 | <0.001 | * | * | 6.68 | 5.34 | 0.339 | ||
| C1–C2 fixation Harms | 3.44 | 0.96 | 0.012 | * | * | 4.96 | 2.75 | 0.186 | ||
| C1–C2 fixation Magerl | 4.00 | 1.31 | 0.009 | 0.50 (−0.27; 1.28) | 0.197 | 6.88 | 4.85 | 0.522 | ||
| C2–C3 anterior fixation | 1.88 | 0.83 | 0.004 | −0.17 (−0.95; 0.61) | 0.664 | 4.00 | 1.60 | 0.098 | ||
| Surgical approach | ||||||||||
| Posterior | 3.59 | 0.97 | <0.001 | −1.37 (−1.92; −0.81) | <0.001 | 5.89 | 4.24 | 0.940 | ||
| Anterior | 2.00 | 0.91 | 5.97 | 4.77 | ||||||
| Constant | 3.4 (3.03; 3.79) | <0.001 | 4.16 (2.88; 5.44) | <0.001 | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Montemurro, N.; Carnesecchi, S.; Morganti, R.; De Carlo, A.; Cocciaro, A. Surgical Outcomes of Craniocervical Junction Fractures in Elderly Patients: A Retrospective Single-Center Series. J. Pers. Med. 2025, 15, 485. https://doi.org/10.3390/jpm15100485
Montemurro N, Carnesecchi S, Morganti R, De Carlo A, Cocciaro A. Surgical Outcomes of Craniocervical Junction Fractures in Elderly Patients: A Retrospective Single-Center Series. Journal of Personalized Medicine. 2025; 15(10):485. https://doi.org/10.3390/jpm15100485
Chicago/Turabian StyleMontemurro, Nicola, Stefano Carnesecchi, Riccardo Morganti, Antonella De Carlo, and Ardico Cocciaro. 2025. "Surgical Outcomes of Craniocervical Junction Fractures in Elderly Patients: A Retrospective Single-Center Series" Journal of Personalized Medicine 15, no. 10: 485. https://doi.org/10.3390/jpm15100485
APA StyleMontemurro, N., Carnesecchi, S., Morganti, R., De Carlo, A., & Cocciaro, A. (2025). Surgical Outcomes of Craniocervical Junction Fractures in Elderly Patients: A Retrospective Single-Center Series. Journal of Personalized Medicine, 15(10), 485. https://doi.org/10.3390/jpm15100485








