Revisiting the Institut Mutualiste Montsouris Difficulty Classification of Laparoscopic Liver Resection with the Data from a Personal Series—Evaluations for the Difficulty of Left Medial Sectionectomy and Length of Hospital Stay
Abstract
1. Introduction
2. Left Medial Sectionectomy in IMM Classification System
3. Methods Used for Determining IMM Classification and in the Present Study
- Evaluation of the difficulty of each type of LLR, including LMS, using the data from a personal case series and the IMM classification system
- 2.
- Evaluation of the difficulty using the IMM classification system plus the length of the postoperative hospital stay
4. Results
Backgrounds Factors in Each Group
- Difficulty score for each type of LLR, including LMS, based on the IMM classification system using data from personal case series
- 2.
- Classification of difficulty using the IMM system plus length of postoperative hospital stay
- 3.
- Backgrounds of the patients who underwent right hemihepatectomy
5. Discussion
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Reich, H.; McGlynn, F.; DeCaprio, J.; Budin, R. Laparoscopic excision of benign liver lesions. Obstet. Gynecol. 1991, 78, 956–958. [Google Scholar]
- Katkhouda, N.; Fabiani, P.; Benizri, E.; Mouiel, J. Laser resection of a liver hydatid cyst under videolaparoscopy. Br. J. Surg. 1992, 79, 560–561. [Google Scholar] [CrossRef] [PubMed]
- Gagner, M.; Rheault, M.; Dubuc, J. Laparoscopic partial hepatectomy for liver tumor. Surg. Endosc. 1992, 6, 97–98. [Google Scholar]
- Morise, Z.; Wakabayashi, G. First quarter century of laparoscopic liver resection. World J. Gastroenterol. 2017, 28, 3581–3588. [Google Scholar] [CrossRef]
- Buell, J.F.; Cherqui, D.; Geller, D.A.; O’Rourke, N.; Iannitti, D.; Dagher, I.; Koffron, A.J.; Thomas, M.; Gayet, B.; Han, H.S.; et al. The international position on laparoscopic liver surgery: The Louisville Statement, 2008. Ann. Surg. 2009, 250, 825–830. [Google Scholar] [CrossRef]
- Wakabayashi, G.; Cherqui, D.; Geller, D.A.; Buell, J.F.; Kaneko, H.; Han, H.S.; Asbun, H.; O’Rourke, N.; Tanabe, M.; Koffron, A.J.; et al. Recommendations for laparoscopic liver resection: A report from the second international consensus conference held in Morioka. Ann. Surg. 2015, 261, 619–629. [Google Scholar]
- Cherqui, D.; Wakabayashi, G.; Geller, D.A.; Buell, J.F.; Han, H.S.; Soubrane, O.; O’Rourke, N. International Laparoscopic Liver Society. The need for organization of laparoscopic liver resection. J. Hepatobiliary Pancreat. Sci. 2016, 23, 665–667. [Google Scholar] [CrossRef]
- Ban, D.; Tanabe, M.; Ito, H.; Otsuka, Y.; Nitta, H.; Abe, Y.; Hasegawa, Y.; Katagiri, T.; Takagi, C.; Itano, O.; et al. A novel difficulty scoring system for laparoscopic liver resection. J. Hepatobiliary Pancreat. Sci. 2014, 21, 745–753. [Google Scholar] [CrossRef] [PubMed]
- Wakabayashi, G. What has changed after the Morioka consensus conference 2014 on laparoscopic liver resection? Hepatobiliary Surg. Nutr. 2016, 5, 281–289. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, S.; Kawaguchi, Y.; Kubo, S.; Kanazawa, A.; Takeda, Y.; Hirokawa, F.; Nitta, H.; Nakajima, T.; Kaizu, T.; Kaibori, M.; et al. Validation of index-based IWATE criteria as an improved difficulty scoring system for laparoscopic liver resection. Surgery 2019, 165, 731–740. [Google Scholar] [CrossRef]
- Berardi, G.; Muttillo, E.M.; Colasanti, M.; Mariano, G.; Meniconi, R.L.; Ferretti, S.; Guglielmo, N.; Angrisani, M.; Lucarini, A.; Garofalo, E.; et al. Challenging Scenarios and Debated Indications for Laparoscopic Liver Resections for Hepatocellular Carcinoma. Cancers 2023, 15, 1493. [Google Scholar] [CrossRef]
- Troisi, R.I.; Berardi, G.; Morise, Z.; Cipriani, F.; Ariizumi, S.; Sposito, C.; Panetta, V.; Simonelli, I.; Kim, S.; Goh, B.K.P.; et al. Laparoscopic and open liver resection for hepatocellular carcinoma with Child-Pugh B cirrhosis: Multicentre propensity score-matched study. Br. J. Surg. 2021, 108, 196–204. [Google Scholar] [CrossRef]
- Morise, Z.; Aldrighetti, L.; Belli, G.; Ratti, F.; Cheung, T.T.; Lo, C.M.; Tanaka, S.; Kubo, S.; Okamura, Y.; Uesaka, K.; et al. An International retrospective observational study of liver functional deterioration after repeat liver resection for patients with hepatocellular carcinoma. Cancers 2022, 14, 2598. [Google Scholar] [CrossRef] [PubMed]
- Halls, M.C.; Berardi, G.; Cipriani, F.; Barkhatov, L.; Lainas, P.; Harris, S.; D’Hondt, M.; Rotellar, F.; Dagher, I.; Aldrighetti, L.; et al. Development and validation of a difficulty score to predict intraoperative complications during laparoscopic liver resection. Br. J. Surg. 2018, 105, 1182–1191. [Google Scholar] [CrossRef]
- Hasegawa, Y.; Wakabayashi, G.; Nitta, H.; Takahara, T.; Katagiri, H.; Umemura, A.; Makabe, K.; Sasaki, A. A novel model for prediction of pure laparoscopic liver resection surgical difficulty. Surg. Endosc. 2017, 31, 5356–5363. [Google Scholar] [CrossRef]
- Kawaguchi, Y.; Fuks, D.; Kokudo, N.; Gayet, B. Difficulty of Laparoscopic Liver Resection: Proposal for a New Classification. Ann. Surg. 2018, 267, 13–17. [Google Scholar] [CrossRef] [PubMed]
- Strasberg, S.M.; Phillips, C. Use and dissemination of the brisbane 2000 nomenclature of liver anatomy and resections. Ann. Surg. 2013, 257, 377–382. [Google Scholar] [CrossRef] [PubMed]
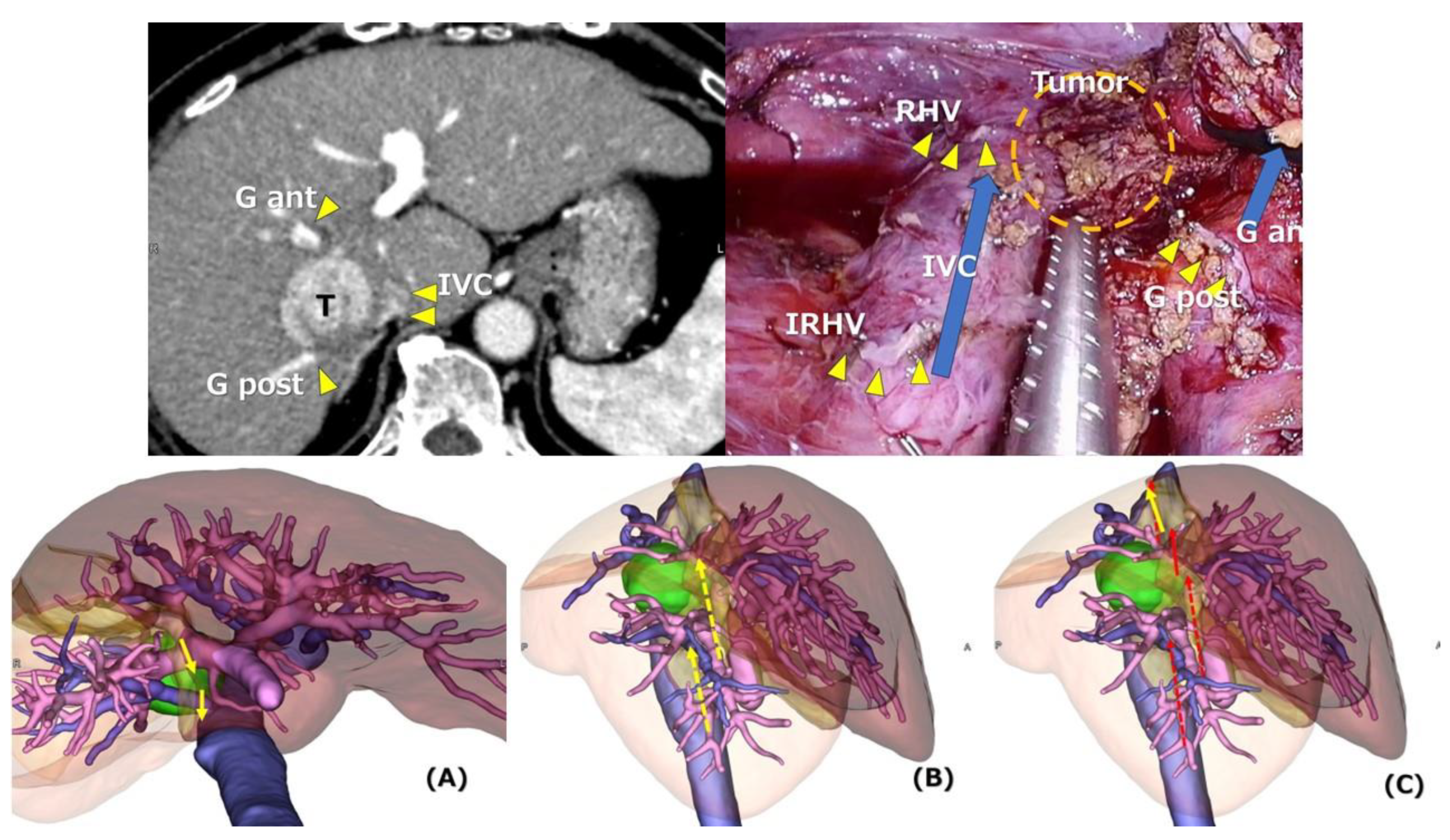
- Tomishige, H.; Morise, Z.; Kawabe, N.; Nagata, H.; Ohshima, H.; Kawase, J.; Arakawa, S.; Yoshida, R.; Isetani, M. Caudal approach to pure laparoscopic posterior sectionectomy under the laparoscopy-specific view. World J. Gastrointest. Surg. 2013, 5, 173–177. [Google Scholar] [CrossRef]
- Krenzien, F.; Wabitsch, S.; Haber, P.; Kamali, C.; Brunnbauer, P.; Benzing, C.; Atanasov, G.; Wakabayashi, G.; Ȕllinger, R.; Pratschke, J.; et al. Validity of the Iwate criteria for patients with hepatocellular carcinoma undergoing minimally invasive liver resection. J. Hepatobiliary Pancreat. Sci. 2018, 25, 403–411. [Google Scholar] [CrossRef]
- Fujiyama, Y.; Wakabayashi, T.; Mishima, K.; Al-Omari, M.A.; Colella, M.; Wakabayashi, G. Latest Findings on Minimally Invasive Anatomical Liver Resection. Cancers 2023, 15, 2218. [Google Scholar] [CrossRef]
- Radtke, A.; Sotiropoulos, G.C.; Molmenti, E.P.; Schroeder, T.; Peitgen, H.O.; Frilling, A.; Broering, D.C.; Broelsch, C.E.; Malago, M. Computer-assisted surgery planning for complex liver resections: When is it helpful? A single-center experience over an 8-year period. Ann. Surg. 2010, 252, 876–883. [Google Scholar] [CrossRef]
- Monden, K.; Sadamori, H.; Hioki, M.; Ohno, S.; Takakura, N. Laparoscopic Anatomic Liver Resection of the Dorsal Part of Segment 8 Using an Hepatic Vein-Guided Approach. Ann. Surg. Oncol. 2022, 29, 341. [Google Scholar] [CrossRef]
- Wakabayashi, T.; Cacciaguerra, A.B.; Abe, Y.; Bona, E.D.; Nicolini, D.; Mocchegiani, F.; Kabeshima, Y.; Vivarelli, M.; Wakabayashi, G.; Kitagawa, Y. Indocyanine Green Fluorescence Navigation in Liver Surgery: A Systematic Review on Dose and Timing of Administration. Ann. Surg. 2022, 275, 1025–1034. [Google Scholar] [CrossRef]
- Kudo, H.; Ishizawa, T.; Tani, K.; Harada, N.; Ichida, A.; Shimizu, A.; Kaneko, J.; Aoki, T.; Sakamoto, Y.; Sugawara, Y.; et al. Visualization of subcapsular hepatic malignancy by indocyanine-green fluorescence imaging during laparoscopic hepatectomy. Surg. Endosc. 2014, 28, 2504–2508. [Google Scholar] [CrossRef]
- Aoki, T.; Yasuda, D.; Shimizu, Y.; Odaira, M.; Niiya, T.; Kusano, T.; Mitamura, K.; Hayashi, K.; Murai, N.; Koizumi, T.; et al. Image-guided liver mapping using fluorescence navigation system with indocyanine green for anatomical hepatic resection. World J. Surg. 2008, 32, 1763–1767. [Google Scholar] [CrossRef]
- Gotohda, N.; Cherqui, D.; Geller, D.A.; Abu Hilal, M.; Berardi, G.; Ciria, R.; Abe, Y.; Aoki, T.; Asbun, H.J.; Chan, A.C.Y.; et al. Expert Consensus Guidelines: How to safely perform minimally invasive anatomic liver resection. J. Hepatobiliary Pancreat. Sci. 2022, 29, 16–32. [Google Scholar] [CrossRef]
- Sugioka, A.; Kato, Y.; Tanahashi, Y. Systematic extrahepatic Glissonean pedicle isolation for anatomical liver resection based on Laennec’s capsule: Proposal of a novel comprehensive surgical anatomy of the liver. J. Hepatobiliary Pancreat. Sci. 2017, 24, 17–23. [Google Scholar] [CrossRef] [PubMed]
- Giulianotti, P.C.; Coratti, A.; Sbrana, F.; Addeo, P.; Bianco, F.M.; Buchs, N.C.; Annechiarico, M.; Benedetti, E. Robotic liver surgery: Results for 70 resections. Surgery 2011, 149, 29–39. [Google Scholar] [CrossRef] [PubMed]
- Kato, Y.; Sugioka, A.; Kojima, M.; Kiguchi, G.; Mii, S.; Uchida, Y.; Takahara, T.; Uyama, I. Initial experience with robotic liver resection: Audit of 120 consecutive cases at a single center and comparison with open and laparoscopic approaches. J. Hepatobiliary Pancreat. Sci. 2022, 30, 72–90. [Google Scholar] [CrossRef] [PubMed]
- Lewandowski, R.J.; Gabr, A.; Abouchaleh, N.; Ali, R.; Asadi, A.A.; Mora, R.A.; Kulik, L.; Ganger, D.; Desai, K.; Thornburg, B.; et al. Radiation Segmentectomy: Potential Curative Therapy for Early Hepatocellular Carcinoma. Radiology 2018, 287, 1050–1058. [Google Scholar] [CrossRef] [PubMed]
| LLR Type (n) | T Number | T Size (mm) | ICGR15 | CLD (%) | Repeat Case (%) |
|---|---|---|---|---|---|
| Right Hep (12) | 2.5 | 60.5 | 8.5 | 33 | 0 |
| Right Anterior (8) | 1.0 | 50.0 | 10.3 | 75 | 0 |
| Left Hep (17) | 1.0 | 80.0 | 10.4 | 41 | 16 |
| Seg 7 or 8 (9) | 2.0 | 26.0 | 10.8 | 56 | 33 |
| Right Posterior (19) | 1.0 | 29.0 | 8.7 | 42 | 5 |
| Left Medial (6) | 1.0 | 35.0 | 11.0 | 50 | 17 |
| Seg or Less Anatomical excluding Seg 7/8 (27) | 1.0 | 20.0 | 13.9 | 59 | 33 |
| Left Lateral (14) | 1.0 | 38.5 | 10.0 | 36 | 21 |
| Partial Resection (119) | 1.0 | 23.0 | 14.8 | 52 | 27 |
| ALL (231) | 1.0 | 25.0 | 11.7 | 50 | 22 |
| LLR Type (n) | Operative Time, min | Blood Loss, mL | Conversion Rate, % | Length of Stay, Day |
|---|---|---|---|---|
| Right Hep (12) | 498.0 [240] | 603.0 [215] | 8.3 [5.1] | 28.00 |
| Right Anterior (8) | 475.5 [205] | 582.5 [300] | 12.5 [18.2] | 22.50 |
| Left Hep (17) | 336.0 [210] | 205.0 [120] | 5.9 [3.8] | 14.00 |
| Seg 7 or 8 (9) | 424.0 [198] | 160.0 [110] | 11.1 [6.5] | 12.00 |
| Right Posterior (19) | 444.0 [300] | 310.0 [350] | 0.0 [14.3] | 15.00 |
| Left Medial (6) | 492.0 | 292.0 | 0.0 | 28.50 |
| Seg or Less Anatomical excluding Seg 7/8 (27) | 351.0 | 150.0 | 0.0 | 16.00 |
| Left Lateral (14) | 261.5 [135] | 50.0 [15] | 0.0 [0] | 12.00 |
| Partial Resection (119) | 246.0 [120, 172] | 50.0 [0, 50] | 1.7 [0, 1.7] | 12.00 |
| ALL case (231) | 323.0 [190] | 108.0 [100] | 3.0 [4.2] | 14.00 |
| LLR Type (n) | Original IMM Score | IMM Score in Present Study | Original IMM Grade | IMM Grade in Present Study | The Levels of Expertise |
|---|---|---|---|---|---|
| Right Hep (12) | 3 | 3 | III | III |  |
| Right Anterior (8) | 3 | 3 | III | III | |
| Left Hep (17) | 2 | 3 | II | III | |
| Seg 7 or 8 (9) | 3 | 3 | III | III | |
| Right Posterior (19) | 3 | 2 | III | II | |
| Left Medial (6) | 2 | II | |||
| Seg or Less Anatomical excluding Seg 7/8 (27) | 2 | 2 | II | II | |
| Left Lateral (14) | 0 | 0 | I | I | Beginning and least complex level |
| Partial Resection (119) | 0 | 0 | I | I | |
| ALL case (231) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Morise, Z. Revisiting the Institut Mutualiste Montsouris Difficulty Classification of Laparoscopic Liver Resection with the Data from a Personal Series—Evaluations for the Difficulty of Left Medial Sectionectomy and Length of Hospital Stay. J. Pers. Med. 2024, 14, 232. https://doi.org/10.3390/jpm14030232
Morise Z. Revisiting the Institut Mutualiste Montsouris Difficulty Classification of Laparoscopic Liver Resection with the Data from a Personal Series—Evaluations for the Difficulty of Left Medial Sectionectomy and Length of Hospital Stay. Journal of Personalized Medicine. 2024; 14(3):232. https://doi.org/10.3390/jpm14030232
Chicago/Turabian StyleMorise, Zenichi. 2024. "Revisiting the Institut Mutualiste Montsouris Difficulty Classification of Laparoscopic Liver Resection with the Data from a Personal Series—Evaluations for the Difficulty of Left Medial Sectionectomy and Length of Hospital Stay" Journal of Personalized Medicine 14, no. 3: 232. https://doi.org/10.3390/jpm14030232
APA StyleMorise, Z. (2024). Revisiting the Institut Mutualiste Montsouris Difficulty Classification of Laparoscopic Liver Resection with the Data from a Personal Series—Evaluations for the Difficulty of Left Medial Sectionectomy and Length of Hospital Stay. Journal of Personalized Medicine, 14(3), 232. https://doi.org/10.3390/jpm14030232







