The Impact of Chemotherapy and Transforming Growth Factor-β1 in Liver Regeneration after Hepatectomy among Colorectal Cancer Patients
Abstract
1. Background
2. Materials and Methods
2.1. Ethics
2.2. Participants and Data Collection
2.3. Calculation of Liver Volume by CT
2.4. Liver Stiffness Analysis
2.5. ELISA and Immunohistochemistry for HGF and TGF β1
2.6. Study Outcomes and Statistical Analysis
3. Results
3.1. Patients
3.2. Liver Resection
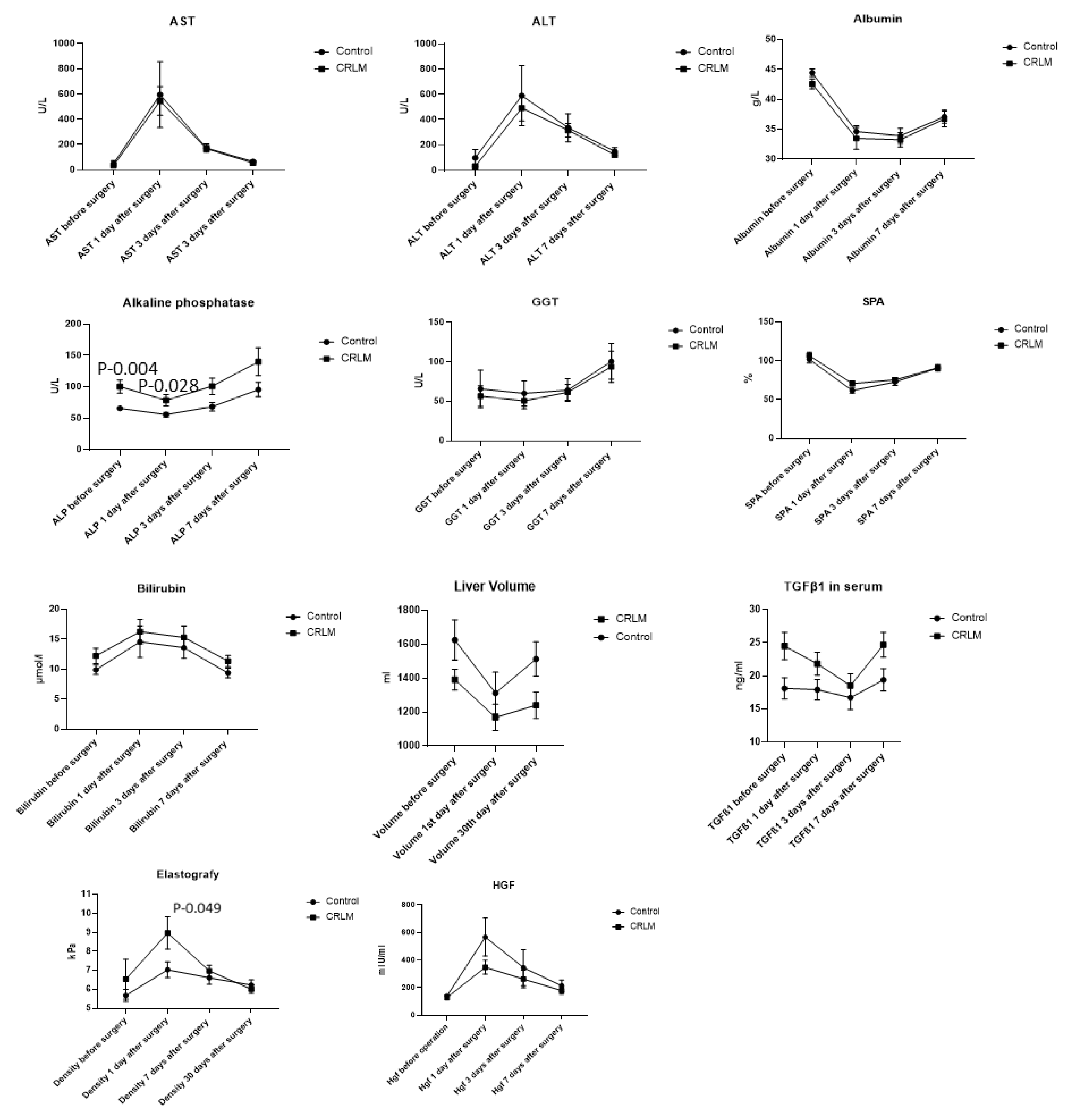
3.3. Postoperative Liver Regeneration
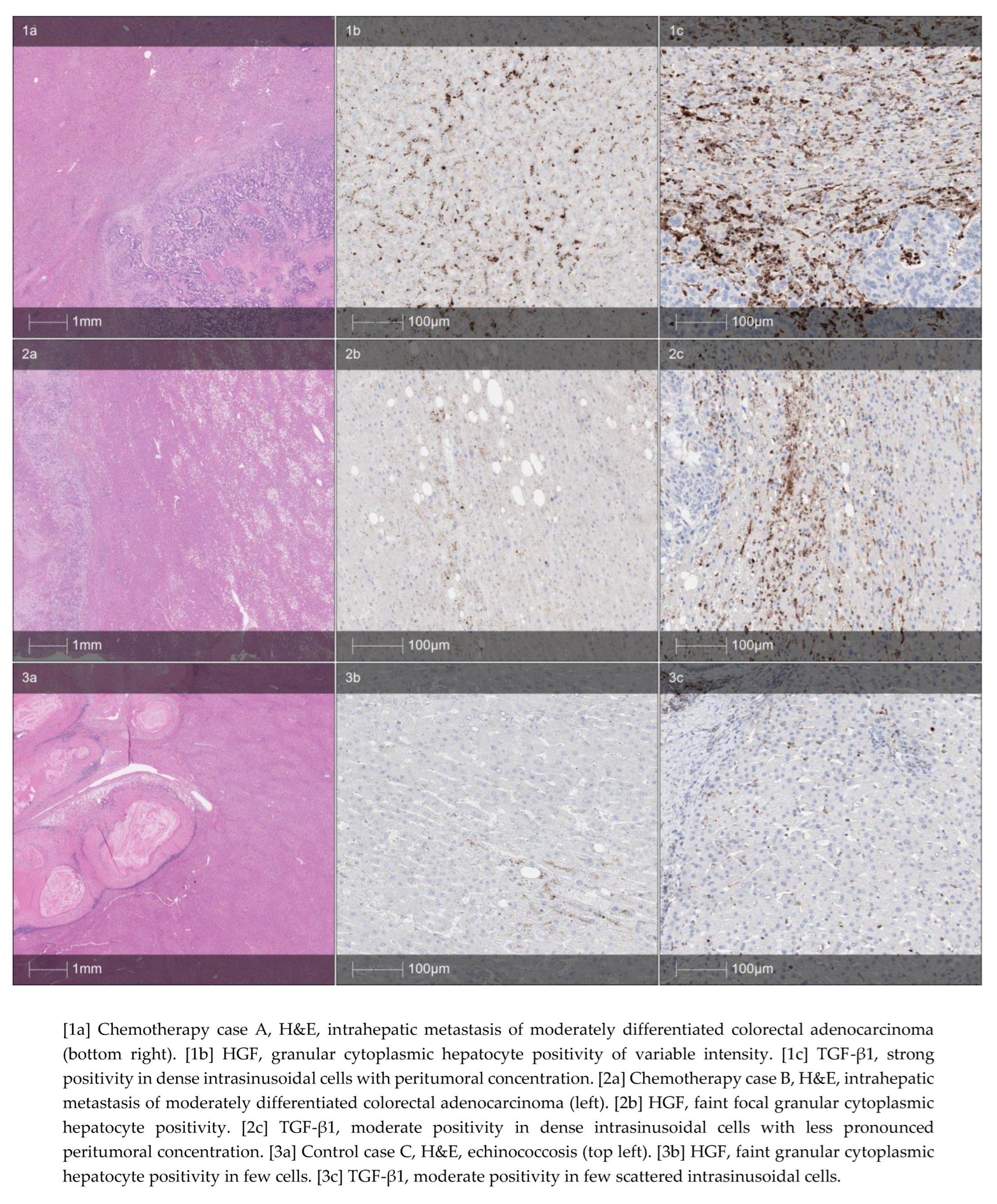
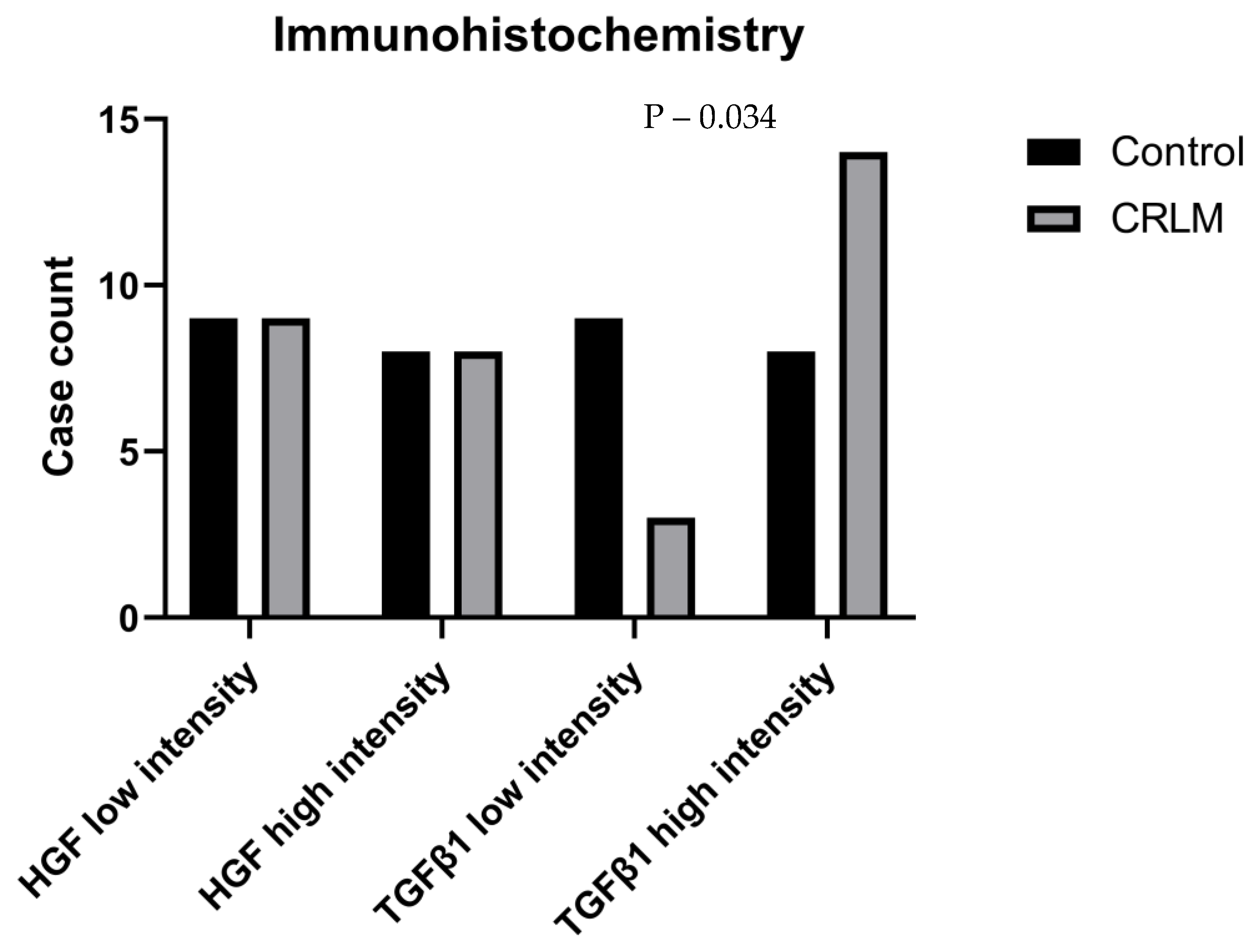
3.4. Biomarkers for Liver Regeneration
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ALP | Alkaline phosphatase |
| ALT | Alanine aminotransferase |
| ALPPS | Associating liver partition and portal vein ligation surgery |
| AST | Aspartate aminotransferase |
| BMI | Body mass index |
| CA 19.9 | Cancer antigen 19.9 |
| CEA | Carcinoembryonic antigen |
| C-D | Clavien–Dindo |
| CT | Computed tomography |
| FNH | Focal nodular hyperplasia |
| FOLFOX | Leucovorin, fluoruracil, oxaliplatin |
| GE | General Electrics |
| GGT | Gamma-glutamyl transferase |
| HGF | Hepatocyte growth factor |
| IHC | Immunohistochemistry |
| SPA | Prothrombin |
| TGF-β1 | Tumor growth factor β1 |
| XELOX | Oxaliplatin and capecitabine |
References
- Sung, H.A.-O.; Ferlay, J.; Siegel, R.A.-O.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Inoue, Y.; Fujii, K.; Tashiro, K.; Ishii, M.; Masubuchi, S.; Yamamoto, M.; Shimizu, T.; Asakuma, M.; Hirokawa, F.; Hayashi, M.; et al. Preoperative Chemotherapy May Not Influence the Remnant Liver Regenerations and Outcomes After Hepatectomy for Colorectal Liver Metastasis. World J. Surg. 2018, 42, 3316–3330. [Google Scholar] [CrossRef]
- Maneikyte, J.; Bausys, A.; Leber, B.; Horvath, A.; Feldbacher, N.; Hoefler, G.; Strupas, K.; Stiegler, P.; Schemmer, P. Dietary glycine decreases both tumor volume and vascularization in a combined colorectal liver metastasis and chemotherapy model. Int. J. Biol. Sci. 2019, 15, 1582–1590, (1449-2288 (Electronic)). [Google Scholar] [CrossRef]
- Balzan, S.; Belghiti, J.; Farges, O.; Ogata, S.; Sauvanet, A.; Delefosse, D.; Durand, F. The “50-50 criteria” on postoperative day 5: An accurate predictor of liver failure and death after hepatectomy. Ann. Surg. 2005, 242, 824–828, discussion 828–829. [Google Scholar] [CrossRef]
- Clavien, P.-A.; Petrowsky, H.; DeOliveira, M.L.; Graf, R. Strategies for Safer Liver Surgery and Partial Liver Transplantation. N. Engl. J. Med. 2007, 356, 1545–1559. [Google Scholar] [CrossRef] [PubMed]
- Jones, R.P.; Stättner, S.; Sutton, P.; Dunne, D.F.; McWhirter, D.; Fenwick, S.W.; Malik, H.Z.; Poston, G.J. Controversies in the oncosurgical management of liver limited stage IV colorectal cancer. Surg. Oncol. 2014, 23, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Michalopoulos, G.K.; Bhushan, B. Liver regeneration: Biological and pathological mechanisms and implications. Nat. Rev. Gastroenterol. Hepatol. 2021, 18, 40–55. [Google Scholar] [CrossRef]
- Sturesson, C.; Nilsson, J.; Eriksson, S.; Spelt, L.; Andersson, R. Limiting factors for liver regeneration after a major hepatic resection for colorectal cancer metastases. HPB 2013, 15, 646–652. [Google Scholar] [CrossRef] [PubMed]
- Pavel, M.C.; Casanova, R.; Estalella, L.; Memba, R.; Llacer-Millan, E.; Julia, E.; Merino, S.; Geoghegan, J.; Jorba, R. Impact of neoadjuvant chemotherapy on post-hepatectomy regeneration for patients with colorectal cancer liver metastasis—Systematic review and meta-analysis. Eur. J. Surg. Oncol. 2023, 49, 533–541. [Google Scholar] [CrossRef] [PubMed]
- Tao, Y.; Wang, M.; Chen, E.; Tang, H. Liver Regeneration: Analysis of the Main Relevant Signaling Molecules. Mediat. Inflamm 2017, 2017, 4256352. [Google Scholar] [CrossRef]
- Romero-Gallo, J.; Sozmen Eg Fau-Chytil, A.; Chytil, A. Fau-Russell, W.E.; Russell We Fau-Whitehead, R.; Whitehead R. Fau-Parks, W.T.; Parks Wt Fau-Holdren, M.S.; Holdren Ms Fau-Her, M.F.; Her Mf Fau-Gautam, S.; Gautam S. Fau-Magnuson, M.; Magnuson M. Fau-Moses, H.L.; et al. Inactivation of TGF-beta signaling in hepatocytes results in an increased proliferative response after partial hepatectomy. Oncogene 2005, 24, 3028–3041, (0950-9232 (Print)). [Google Scholar]
- Siriwardena, A.A.-O.; Serrablo, A.; Fretland Å., A. A.-O.; Wigmore, S.J.; Ramia-Angel, J.A.-O.; Malik, H.Z.; Stättner, S.; Søreide, K.; Zmora, O.; Meijerink, M.; et al. Multisocietal European consensus on the terminology, diagnosis, and management of patients with synchronous colorectal cancer and liver metastases: An E-AHPBA consensus in partnership with ESSO, ESCP, ESGAR, and CIRSE. Br. J. Surg. 2023, 110, 1161–1170, (1365-2168 (Electronic)). [Google Scholar]
- Barr, R.A.-O.; Wilson, S.A.-O.; Rubens, D.A.-O.X.; Garcia-Tsao, G.; Ferraioli, G.A.-O.X. Update to the Society of Radiologists in Ultrasound Liver Elastography Consensus Statement. Therap. Adv. Gastroenterol. 2022, 15, 17562848221140657, (1527-1315 (Electronic)). [Google Scholar] [CrossRef]
- Laurinavicius, A.; Plancoulaine, B.; Laurinaviciene, A.; Herlin, P.; Meskauskas, R.; Baltrusaityte, I.; Besusparis, J.; Dasevicius, D.; Elie, N.; Iqbal, Y.; et al. A methodology to ensure and improve accuracy of Ki67 labelling index estimation by automated digital image analysis in breast cancer tissue. Breast Cancer Res. 2014, 16, R35. [Google Scholar] [CrossRef] [PubMed]
- Sandhu, J.; Lavingia, V.; Fakih, M. Systemic treatment for metastatic colorectal cancer in the era of precision medicine. J. Surg. Oncol. 2019, 119, 564–582. [Google Scholar] [CrossRef] [PubMed]
- Kvietkauskas, M.A.-O.; Zitkute, V.A.-O.; Leber, B.A.-O.; Strupas, K.; Stiegler, P.; Schemmer, P.A.-O. Dietary Melatonin and Glycine Decrease Tumor Growth through Antiangiogenic Activity in Experimental Colorectal Liver Metastasis. Nutrients 2021, 13, 2035, (2072-6643 (Electronic)). [Google Scholar] [CrossRef] [PubMed]
- Vauthey, J.N.; Pawlik, T.M.; Ribero, D.; Wu, T.T.; Zorzi, D.; Hoff, P.M.; Xiong, H.Q.; Eng, C.; Lauwers, G.Y.; Mino-Kenudson, M.; et al. Chemotherapy regimen predicts steatohepatitis and an increase in 90-day mortality after surgery for hepatic colorectal metastases. J. Clin. Oncol. 2006, 24, 2065–2072. [Google Scholar] [CrossRef] [PubMed]
- Kingham, T.P.; Correa-Gallego, C.; D’Angelica, M.I.; Gönen, M.; DeMatteo, R.P.; Fong, Y.; Allen, P.J.; Blumgart, L.H.; Jarnagin, W.R. Hepatic parenchymal preservation surgery: Decreasing morbidity and mortality rates in 4152 resections for malignancy. J. Am. Coll. Surg. 2014, 220, 471–479, (1879-1190 (Electronic)). [Google Scholar] [CrossRef] [PubMed]
- Mullen, J.T.; Ribero, D.; Fau-Reddy, S.K.; Reddy Sk Fau Donadon, M.; Donadon, M.; Fau-Zorzi, D.; Zorzi, D.; Fau-Gautam, S.; Gautam, S.; Fau-Abdalla, E.K.; et al. Hepatic insufficiency and mortality in 1059 noncirrhotic patients undergoing major hepatectomy. J. Am. Coll. Surg. 2007, 204, 854–862, (1072-7515 (Print)). [Google Scholar] [CrossRef] [PubMed]
- Rahnemai-Azar, A.A.; Cloyd, J.M.; Weber, S.M.; Dillhoff, M.; Schmidt, C.; Winslow, E.R.; Pawlik, T.M. Update on Liver Failure Following Hepatic Resection: Strategies for Prediction and Avoidance of Post-operative Liver Insufficiency. J. Clin. Transl. Hepatol. 2018, 6, 97–104. [Google Scholar] [CrossRef] [PubMed]
- Milana, F.A.-O.; Famularo, S.A.-O.; Diana, M.A.-O.; Mishima, K.A.-O.; Reitano, E.A.-O.; Cho, H.D.; Kim, K.H.; Marescaux, J.A.-O.; Donadon, M.A.-O.; Torzilli, G.A.-O. How Much Is Enough? A Surgical Perspective on Imaging Modalities to Estimate Function and Volume of the Future Liver Remnant before Hepatic Resection. Diagnostics 2023, 13, 2726, (2075-4418 (Print)). [Google Scholar] [CrossRef] [PubMed]
- Done, J.A.-O.; Papanikolaou, A.; Stem, M.; Radomski, S.N.; Chen, S.Y.; Atallah, C.; Efron, J.E.; Safar, B. Impact of preoperative chemotherapy on perioperative morbidity in combined resection of colon cancer and liver metastases. J. Gastrointest. Surg. 2023, 27, 2380–2387, (1873-4626 (Electronic)). [Google Scholar] [CrossRef] [PubMed]
- Huang, R.A.-O.; Zhang, X.; Gracia-Sancho, J.; Xie, W.A.-O.X. Liver regeneration: Cellular origin and molecular mechanisms. Liver Int. 2022, 42, 1486–1495, (1478-3231 (Electronic)). [Google Scholar] [CrossRef] [PubMed]
- Sparrelid, E.; Johansson, H.; Gilg, S.; Nowak, G.; Ellis, E.; Isaksson, B. Serial Assessment of Growth Factors Associated with Liver Regeneration in Patients Operated with Associating Liver Partition and Portal Vein Ligation for Staged Hepatectomy. Eur. Surg. Res. 2018, 59, 72–82, (1421-9921 (Electronic)). [Google Scholar] [CrossRef]
- Matsumoto, K.; Miyake, Y.; Fau-Umeda, Y.; Umeda, Y.; Fau-Matsushita, H.; Matsushita, H.; Fau-Matsuda, H.; Matsuda, H.; Fau-Takaki, A.; Takaki, A.; et al. Serial changes of serum growth factor levels and liver regeneration after partial hepatectomy in healthy humans. Int. J. Mol. Sci. 2013, 14, 20877–20889, (1422-0067 (Electronic)). [Google Scholar] [CrossRef] [PubMed]
- Michalopoulos, G.K. Principles of liver regeneration and growth homeostasis. Compr. Physiol. 2013, 3, 485–513, (2040-4603 (Electronic)). [Google Scholar] [PubMed]
- Kobayashi, K.; Hirota, S.; Kako, Y.; Yamamoto, S.; Takaki, H.; Yamakado, K. Changes in liver stiffness on real-time tissue elastography before and after occlusion of spontaneous portosystemic shunts. Diagn. Interv. Imaging 2017, 98, 321–326, (1095-8673 (Electronic)). [Google Scholar] [CrossRef] [PubMed]
- Lee, S.C.; Jeong, H.J.; Choi, B.J.; Kim, S.J. Role of the spleen in liver regeneration in relation to transforming growth factor-β1 and hepatocyte growth factor. J. Surg. Res. 2015, 196, 270–277. [Google Scholar] [CrossRef]
- Fausto, N.; Campbell, J.S.; Riehle, K.J. Liver Regeneration. Hepatology 2006, 43, S45–S53. [Google Scholar] [CrossRef]
- Mai, R.A.-O.; Wang, Y.Y.; Bai, T.; Chen, J.; Xiang, B.D.; Wu, G.A.-O.; Wu, F.X.; Li, L.A.-O.; Ye, J.Z. Combination of ALBI and APRI to Predict Post-Hepatectomy Liver Failure after Liver Resection for HBV-Related HCC Patients. Cancer Manag. Res. 2019, 11, 8799–8806, (1179-1322 (Print)). [Google Scholar] [CrossRef]
- Nanashima, A.; Tobinaga, S.; Fau-Abo, T.; Abo, T.; Fau-Nonaka, T.; Nonaka, T.; Fau-Takeshita, H.; Takeshita, H.; Fau-Hidaka, S.; Hidaka, S.; et al. Reducing the incidence of post-hepatectomy hepatic complications by preoperatively applying parameters predictive of liver function. J. Hepatobiliary Pancreat Sci. 2010, 17, 871–878, (1868-6982 (Electronic)). [Google Scholar] [CrossRef] [PubMed]
- Primavesi, F.; Maglione, M.; Cipriani, F.; Denecke, T.; Oberkofler, C.E.; Starlinger, P.; Dasari, B.V.M.; Heil, J.; Sgarbura, O.; Soreide, K.; et al. E-AHPBA-ESSO-ESSR Innsbruck consensus guidelines for preoperative liver function assessment before hepatectomy. Br. J. Surg. 2023, 110, 1331–1347. [Google Scholar] [CrossRef] [PubMed]
| Control Group (n = 17) | CRLM Group (n = 17) | p-Value | ||
|---|---|---|---|---|
| Age (years), mean (SD) | 50 ± 14. | 59 ± 12 | 0.07 | |
| Gender, M/F | 5/12 | 5/12 | 0.99 | |
| BMI (kg/m2), mean (SD) | 30.7 ± 7.3 | 25.6 ± 5.9 | 0.07 | |
| Comorbidities, n (%) | Cardiovascular | 2 (11.7%) | 9 (52.9%) | 0.06 |
| Diabetes | 2 (11.7%) | 0 (0%) | 0.48 | |
| Other | 1 (5.8%) | 0 (0%) | 0.99 | |
| Primary tumor site, n (%) | Cecum | N/A | 2 (11.9%) | N/A |
| Hepatic flexure | 2 (11.9%) | |||
| Sigmoid colon | 7 (41.2%) | |||
| Rectum | 6 (35.3%) | |||
| Number of metastases, n (%) | 1 | N/A | 11 (64.7%) | N/A |
| 2–5 | 4 (23.5%) | |||
| >5 | 2 (11.8%) | |||
| Type of metastases, n (%) | Synchronous | N/A | 5 (29.4%) | N/A |
| Metachronous | 12 (70.6%) | |||
| Preoperative CEA level (ng/mL), mean (SD) | N/A | 44 ± 167 | N/A | |
| Preoperative CA 19.9 (U/mL), mean (SD) | N/A | 37 ± 78 | N/A | |
| Median number of preoperative chemotherapy cycles (Q1–Q3) | N/A | 8 (6; 12) | N/A | |
| Type of first-line preoperative chemotherapy, n (%) | FOLFOX | N/A | 5 (29.4%) | N/A |
| FOLFOX + bevacizumab | N/A | 7 (41.2%) | N/A | |
| XELOX | N/A | 1 (5.9%) | N/A | |
| XELOX + bevacizumab | N/A | 2, (11.9%) | ||
| Capecetabin | N/A | 2, (11.9%) | ||
| Control Group (n = 17) | CRLM Group (n = 17) | p-Value | ||
|---|---|---|---|---|
| Type of liver resection, n (%) | Atypical | 8 (47.1%) | 11 (64.7%) | 0.21 |
| Left lobectomy | 4 (23.5%) | 3 (17.6%) | ||
| Right lobectomy | 1 (5.9%) | 0 (0%) | ||
| Left hepatectomy | 1 (5.9%) | 1 (5.9%) | ||
| Right hepatectomy | 3 (17.6%) | 0 (0%) | ||
| ALPPS | 0 | 2 (11.9%) | ||
| Length of surgery (minutes), mean (SD) | 181 ± 64 | 251 ± 168 | 0.12 | |
| Blood loss (mL), mean (SE) | 520 ± 552 | 516 ± 648 | 0.98 | |
| Patients requiring postoperative blood transfusions, n (%) | 6 (35.3%) | 5 (29.4%) | 0.58 | |
| Postoperative hemotransfusion units, mean (SD) | 0.53 ± 1.12 | 0.76 ± 1.30 | 0.58 | |
| Variable | β Coefficient (95% Confidence Interval) | p-Value |
|---|---|---|
| Baseline HGF value | 0.52 (−0.27–1.31) | 0.189 |
| Baseline albumin value | 7.11 (−10.01–23.24) | 0.403 |
| Baseline alkaline phosphatase value | −1.403 (−2.95–0.14) | 0.074 |
| Resected liver volume | 0.31 (0.14–0.47) | 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Račkauskas, R.; Lukšaitė-Lukštė, R.; Stulpinas, R.; Baušys, A.; Paškonis, M.; Kvietkauskas, M.; Sokolovas, V.; Laurinavičius, A.; Strupas, K. The Impact of Chemotherapy and Transforming Growth Factor-β1 in Liver Regeneration after Hepatectomy among Colorectal Cancer Patients. J. Pers. Med. 2024, 14, 144. https://doi.org/10.3390/jpm14020144
Račkauskas R, Lukšaitė-Lukštė R, Stulpinas R, Baušys A, Paškonis M, Kvietkauskas M, Sokolovas V, Laurinavičius A, Strupas K. The Impact of Chemotherapy and Transforming Growth Factor-β1 in Liver Regeneration after Hepatectomy among Colorectal Cancer Patients. Journal of Personalized Medicine. 2024; 14(2):144. https://doi.org/10.3390/jpm14020144
Chicago/Turabian StyleRačkauskas, Rokas, Raminta Lukšaitė-Lukštė, Rokas Stulpinas, Augustinas Baušys, Marius Paškonis, Mindaugas Kvietkauskas, Vitalijus Sokolovas, Arvydas Laurinavičius, and Kęstutis Strupas. 2024. "The Impact of Chemotherapy and Transforming Growth Factor-β1 in Liver Regeneration after Hepatectomy among Colorectal Cancer Patients" Journal of Personalized Medicine 14, no. 2: 144. https://doi.org/10.3390/jpm14020144
APA StyleRačkauskas, R., Lukšaitė-Lukštė, R., Stulpinas, R., Baušys, A., Paškonis, M., Kvietkauskas, M., Sokolovas, V., Laurinavičius, A., & Strupas, K. (2024). The Impact of Chemotherapy and Transforming Growth Factor-β1 in Liver Regeneration after Hepatectomy among Colorectal Cancer Patients. Journal of Personalized Medicine, 14(2), 144. https://doi.org/10.3390/jpm14020144








