Looking at the Data on Smoking and Post-COVID-19 Syndrome—A Literature Review
Abstract
1. Introduction
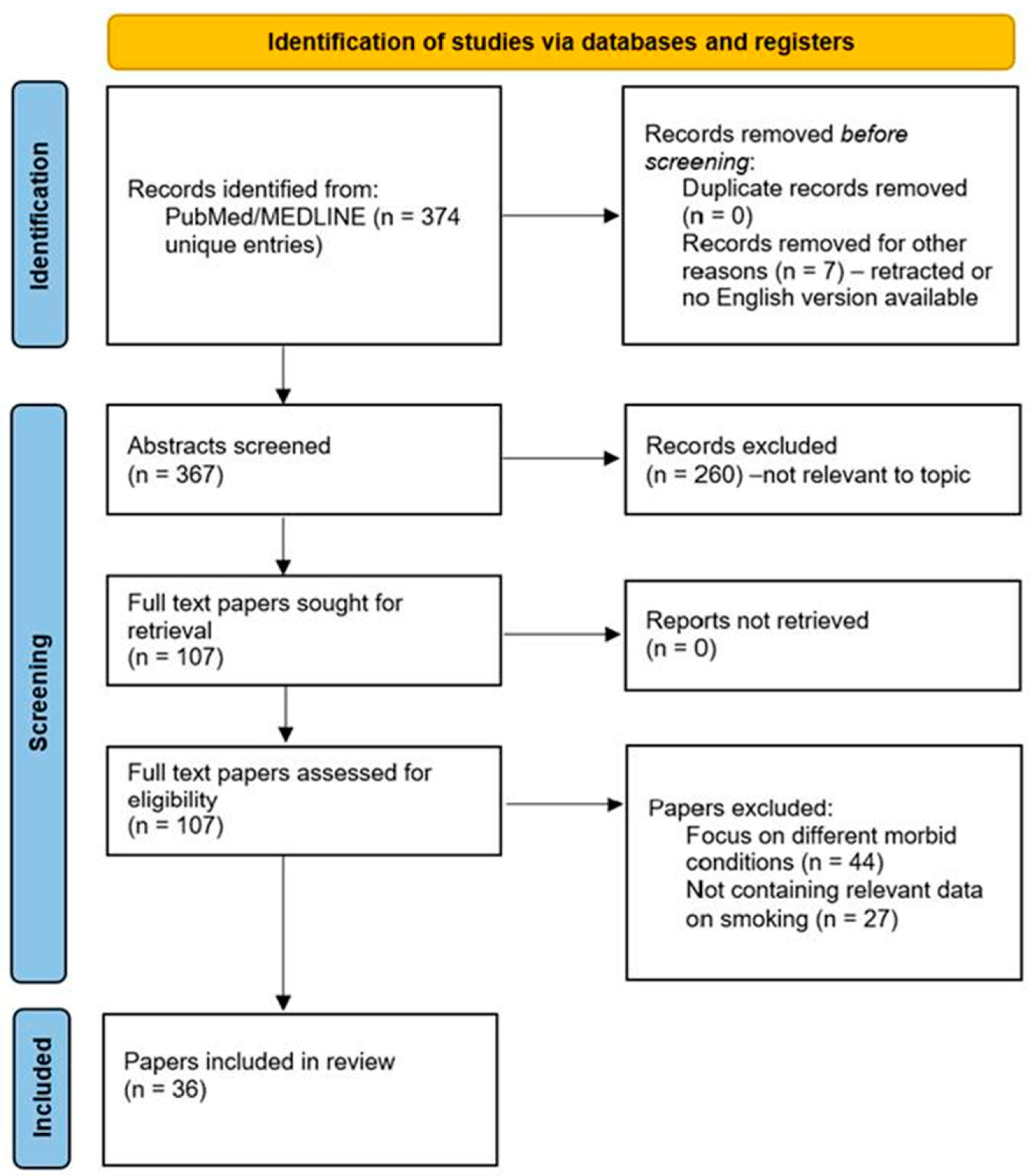
2. Method and Research Design
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Heidemann, C.; Sarganas, G.; Du, Y.; Gaertner, B.; Poethko-Müller, C.; Cohrdes, C.; Schmidt, S.; Schlaud, M.; Scheidt-Nave, C. Long-Term Health Consequences among Individuals with SARS-CoV-2 Infection Compared to Individuals without Infection: Results of the Population-Based Cohort Study CoMoLo Follow-Up. BMC Public Health 2023, 23, 1587. [Google Scholar] [CrossRef] [PubMed]
- Nalbandian, A.; Sehgal, K.; Gupta, A.; Madhavan, M.V.; McGroder, C.; Stevens, J.S.; Cook, J.R.; Nordvig, A.S.; Shalev, D.; Sehrawat, T.S.; et al. Post-Acute COVID-19 Syndrome. Nat. Med. 2021, 27, 601–615. [Google Scholar] [CrossRef]
- Groff, D.; Sun, A.; Ssentongo, A.E.; Ba, D.M.; Parsons, N.; Poudel, G.R.; Lekoubou, A.; Oh, J.S.; Ericson, J.E.; Ssentongo, P.; et al. Short-Term and Long-Term Rates of Postacute Sequelae of SARS-CoV-2 Infection: A Systematic Review. JAMA Netw. Open 2021, 4, e2128568. [Google Scholar] [CrossRef] [PubMed]
- Subramanian, A.; Nirantharakumar, K.; Hughes, S.; Myles, P.; Williams, T.; Gokhale, K.M.; Taverner, T.; Chandan, J.S.; Brown, K.; Simms-Williams, N.; et al. Symptoms and Risk Factors for Long COVID in Non-Hospitalized Adults. Nat. Med. 2022, 28, 1706–1714. [Google Scholar] [CrossRef]
- Lippi, G.; Sanchis Gomar, F.; Henry, B.M. COVID-19 and Its Long-Term Sequelae: What Do We Know in 2023? Pol. Arch. Intern. Med. 2023, 133, 16402. [Google Scholar] [CrossRef] [PubMed]
- Bai, F.; Tomasoni, D.; Falcinella, C.; Barbanotti, D.; Castoldi, R.; Mulè, G.; Augello, M.; Mondatore, D.; Allegrini, M.; Cona, A.; et al. Female Gender Is Associated with Long COVID Syndrome: A Prospective Cohort Study. Clin. Microbiol. Infect. 2022, 28, 611.e9–611.e16. [Google Scholar] [CrossRef] [PubMed]
- Wong, M.C.-S.; Huang, J.; Wong, Y.-Y.; Wong, G.L.-H.; Yip, T.C.-F.; Chan, R.N.-Y.; Chau, S.W.-H.; Ng, S.-C.; Wing, Y.-K.; Chan, F.K.-L. Epidemiology, Symptomatology, and Risk Factors for Long COVID Symptoms: Population-Based, Multicenter Study. JMIR Public. Health Surveill. 2023, 9, e42315. [Google Scholar] [CrossRef] [PubMed]
- Pinato, D.J.; Tabernero, J.; Bower, M.; Scotti, L.; Patel, M.; Colomba, E.; Dolly, S.; Loizidou, A.; Chester, J.; Mukherjee, U.; et al. Prevalence and Impact of COVID-19 Sequelae on Treatment and Survival of Patients with Cancer Who Recovered from SARS-CoV-2 Infection: Evidence from the OnCovid Retrospective, Multicentre Registry Study. Lancet Oncol. 2021, 22, 1669–1680. [Google Scholar] [CrossRef]
- Desgranges, F.; Tadini, E.; Munting, A.; Regina, J.; Filippidis, P.; Viala, B.; Karachalias, E.; Suttels, V.; Haefliger, D.; Kampouri, E.; et al. Post COVID 19 Syndrome in Outpatients: A Cohort Study. J. Gen. Intern. Med. 2022, 37, 1943–1952. [Google Scholar] [CrossRef]
- Conti, V.; Corbi, G.; Sabbatino, F.; De Pascale, D.; Sellitto, C.; Stefanelli, B.; Bertini, N.; De Simone, M.; Liguori, L.; Di Paola, I.; et al. Long COVID: Clinical Framing, Biomarkers, and Therapeutic Approaches. JPM 2023, 13, 334. [Google Scholar] [CrossRef]
- Muzyka, I.; Yakhnytska, M.; Savytska, M.; Zayachkivska, O. Long COVID Prevalence and Physiology-Centered Risks: Population-Based Study in Ukraine. Inflammopharmacol 2023, 31, 597–602. [Google Scholar] [CrossRef]
- Mohamed Hussein, A.R.; Saad, M.; Zayan, H.; Abdelsayed, M.; Moustafa, M.; Ezzat, A.; Helmy, R.; Abd-Elaal, H.; Aly, K.; Abdelrheem, S.; et al. Post-COVID-19 Functional Status: Relation to Age, Smoking, Hospitalization, and Previous Comorbidities. Ann. Thorac. Med. 2021, 16, 260. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Ramasamy, A.; Verduzco-Gutierrez, M.; Brode, W.M.; Melamed, E. Acute and Post-Acute Sequelae of SARS-CoV-2 Infection: A Review of Risk Factors and Social Determinants. Virol. J. 2023, 20, 124. [Google Scholar] [CrossRef] [PubMed]
- Whitaker, M.; Elliott, J.; Chadeau-Hyam, M.; Riley, S.; Darzi, A.; Cooke, G.; Ward, H.; Elliott, P. Persistent COVID-19 Symptoms in a Community Study of 606,434 People in England. Nat. Commun. 2022, 13, 1957. [Google Scholar] [CrossRef] [PubMed]
- Carrasco-Garrido, P.; Fernández-de-Las-Peñas, C.; Hernández-Barrera, V.; Palacios-Ceña, D.; Jiménez-Trujillo, I.; Gallardo-Pino, C. Benzodiazepines and Z-Hypnotics Consumption in Long-COVID-19 Patients: Gender Differences and Associated Factors. Front. Med. 2022, 9, 975930. [Google Scholar] [CrossRef]
- Barthélémy, H.; Mougenot, E.; Duracinsky, M.; Salmon-Ceron, D.; Bonini, J.; Péretz, F.; Chassany, O.; Carrieri, P. Smoking Increases the Risk of Post-Acute COVID-19syndrome: Results from a French Community-Based Survey. Tob. Induc. Dis. 2022, 20, 59. [Google Scholar] [CrossRef]
- Jacobs, E.T.; Catalfamo, C.J.; Colombo, P.M.; Khan, S.M.; Austhof, E.; Cordova-Marks, F.; Ernst, K.C.; Farland, L.V.; Pogreba-Brown, K. Pre-Existing Conditions Associated with Post-Acute Sequelae of COVID-19. J. Autoimmun. 2023, 135, 102991. [Google Scholar] [CrossRef]
- Román-Montes, C.M.; Flores-Soto, Y.; Guaracha-Basañez, G.A.; Tamez-Torres, K.M.; Sifuentes-Osornio, J.; González-Lara, M.F.; León, A.P.D. Post-COVID-19 Syndrome and Quality of Life Impairment in Severe COVID-19 Mexican Patients. Front. Public Health 2023, 11, 1155951. [Google Scholar] [CrossRef]
- Wu, Q.; Ailshire, J.A.; Crimmins, E.M. Long COVID and Symptom Trajectory in a Representative Sample of Americans in the First Year of the Pandemic. Sci. Rep. 2022, 12, 11647. [Google Scholar] [CrossRef]
- Takakura, K.; Suka, M.; Kajihara, M.; Koido, S. Clinical Features, Therapeutic Outcomes, and Recovery Period of Long COVID. J. Med. Virol. 2023, 95, e28316. [Google Scholar] [CrossRef]
- Afroze, F.; Arafat, S.M.; Ahmed, C.M.; Alam, B.; Banu, S.; Islam, M.Z.; Mahfuz, M.; Parvin, I.; Ackhter, M.M.; Shormi, I.; et al. Features and Risk Factors of Post-COVID-19 Syndrome: Findings from a Longitudinal Study in Bangladesh. Lancet Reg. Health Southeast Asia 2023, 11, 100134. [Google Scholar] [CrossRef]
- Buonsenso, D.; Gualano, M.R.; Rossi, M.F.; Valz Gris, A.; Sisti, L.G.; Borrelli, I.; Santoro, P.E.; Tumminello, A.; Gentili, C.; Malorni, W.; et al. Post-Acute COVID-19 Sequelae in a Working Population at One Year Follow-Up: A Wide Range of Impacts from an Italian Sample. Int. J. Environ. Res. Public Health 2022, 19, 11093. [Google Scholar] [CrossRef]
- Tarifi, A.; Al Shdaifat, A.A.; Al-Shudifat, A.M.; Azab, M.; Ismail, J.; Bashir, R.; Amro, A.; Altarifi, A.; Khader, Y. Clinical, Sinonasal, and Long-term Smell and Taste Outcomes in Mildly Symptomatic COVID-19 Patients. Int. J. Clin. Pract. 2021, 75, e14260. [Google Scholar] [CrossRef]
- Kisiel, M.A.; Lee, S.; Malmquist, S.; Rykatkin, O.; Holgert, S.; Janols, H.; Janson, C.; Zhou, X. Clustering Analysis Identified Three Long COVID Phenotypes and Their Association with General Health Status and Working Ability. JCM 2023, 12, 3617. [Google Scholar] [CrossRef] [PubMed]
- Chathoth, A.; Anaswara, N.; Meethal, A.; Vasudevan, J.; Gopal, P. Persisting and New Onset Symptomatology and Determinants of Functional Limitation of Post Acute COVID-19 Syndrome Cases- A Study from a Northern District of Kerala. Indian J. Community Med. 2023, 48, 250. [Google Scholar] [CrossRef] [PubMed]
- Mclaughlin, M.; Cerexhe, L.; Macdonald, E.; Ingram, J.; Sanal-Hayes, N.E.M.; Meach, R.; Carless, D.; Sculthorpe, N. A Cross-Sectional Study of Symptom Prevalence, Frequency, Severity, and Impact of Long-COVID in Scotland: Part I. Am. J. Med. 2023. [Google Scholar] [CrossRef]
- Tene, L.; Bergroth, T.; Eisenberg, A.; David, S.S.B.; Chodick, G. Risk Factors, Health Outcomes, Healthcare Services Utilization, and Direct Medical Costs of Patients with Long COVID. Int. J. Infect. Dis. 2023, 128, 3–10. [Google Scholar] [CrossRef]
- Paul, E.; Fancourt, D. Health Behaviours the Month Prior to COVID-19 Infection and the Development of Self-Reported Long COVID and Specific Long COVID Symptoms: A Longitudinal Analysis of 1581 UK Adults. BMC Public Health 2022, 22, 1716. [Google Scholar] [CrossRef] [PubMed]
- Chilunga, F.P.; Appelman, B.; Van Vugt, M.; Kalverda, K.; Smeele, P.; Van Es, J.; Wiersinga, W.J.; Rostila, M.; Prins, M.; Stronks, K.; et al. Differences in Incidence, Nature of Symptoms, and Duration of Long COVID among Hospitalised Migrant and Non-Migrant Patients in the Netherlands: A Retrospective Cohort Study. Lancet Reg. Health Eur. 2023, 29, 100630. [Google Scholar] [CrossRef]
- Bamps, L.; Armenti, J.-P.; Bojan, M.; Grandbastien, B.; Von Garnier, C.; Du Pasquier, R.; Desgranges, F.; Papadimitriou-Olivgeris, M.; Alberio, L.; Preisig, M.; et al. Long-Term Consequences of COVID-19: A 1-Year Analysis. JCM 2023, 12, 2673. [Google Scholar] [CrossRef]
- Vásconez-González, J.; Fernandez-Naranjo, R.; Izquierdo-Condoy, J.S.; Delgado-Moreira, K.; Cordovez, S.; Tello-De-la-Torre, A.; Paz, C.; Castillo, D.; Izquierdo-Condoy, N.; Carrington, S.J.; et al. Comparative Analysis of Long-Term Self-Reported COVID-19 Symptoms among Pregnant Women. J. Infect. Public Health 2023, 16, 430–440. [Google Scholar] [CrossRef]
- Akinci Ozyurek, B.; Sahin Ozdemirel, T.; Akkurt, E.S.; Yenibertiz, D.; Saymaz, Z.T.; Büyükyaylacı Özden, S.; Eroğlu, Z. What Are the Factors That Affect Post COVID 1st Month’s Continuing Symptoms? Int. J. Clin. Pract. 2021, 75, e14778. [Google Scholar] [CrossRef] [PubMed]
- Hennawi, Y.B.; Alahmadi, R.A.; AlOtaibi, E.; Alosaimi, A.N.; Tashkandi, G.S.; Saleem, N.E.; Bukhari, R.I.; Obaid, M. Olfactory and Gustatory Dysfunctions Following COVID-19 Infection: Factors That Affect Their Duration in Saudi Arabia. Cureus 2023, 15, e37317. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Zhang, X.; Zeng, X.; Xu, T.; Xiao, W.; Yang, X.; Zhan, W.; Zhan, C.; Lai, K. Prevalence and Risk Factors for Postinfectious Cough in Discharged Patients with Coronavirus Disease 2019 (COVID-19). J. Thorac. Dis. 2022, 14, 2079–2088. [Google Scholar] [CrossRef] [PubMed]
- Emecen, A.N.; Keskin, S.; Turunc, O.; Suner, A.F.; Siyve, N.; Basoglu Sensoy, E.; Dinc, F.; Kilinc, O.; Avkan Oguz, V.; Bayrak, S.; et al. The Presence of Symptoms within 6 Months after COVID-19: A Single-Center Longitudinal Study. Ir. J. Med. Sci. 2023, 192, 741–750. [Google Scholar] [CrossRef]
- Cansel, N.; Kayhan Tetik, B.; Hilal Demir, G.; Kurt, O.; Evren, B.; Yücel, A. Assessment of psychological responses and related factors of discharged patients who have been hospitalized with COVID-19. Psychiat Danub. 2021, 33, 611–619. [Google Scholar] [CrossRef]
- Wallis, T.J.M.; Heiden, E.; Horno, J.; Welham, B.; Burke, H.; Freeman, A.; Dexter, L.; Fazleen, A.; Kong, A.; McQuitty, C.; et al. Risk Factors for Persistent Abnormality on Chest Radiographs at 12-Weeks Post Hospitalisation with PCR Confirmed COVID-19. Respir. Res. 2021, 22, 157. [Google Scholar] [CrossRef]
- Tan, H.Q.M.; Pendolino, A.L.; Andrews, P.J.; Choi, D. Prevalence of Olfactory Dysfunction and Quality of Life in Hospitalised Patients 1 Year after SARS-CoV-2 Infection: A Cohort Study. BMJ Open 2022, 12, e054598. [Google Scholar] [CrossRef]
- Li, Z.; He, J.; Wang, Y.; Bai, M.; Zhang, Y.; Chen, H.; Li, W.; Cai, Y.; Chen, S.; Qu, M.; et al. A Cross-Sectional Study on the Mental Health of Patients with COVID-19 1 Year after Discharge in Huanggang, China. Eur. Arch. Psychiatry Clin. Neurosci. 2023, 273, 301–310. [Google Scholar] [CrossRef]
- Karanasos, A.; Aznaouridis, K.; Latsios, G.; Synetos, A.; Plitaria, S.; Tousoulis, D.; Toutouzas, K. Impact of Smoking Status on Disease Severity and Mortality of Hospitalized Patients With COVID-19 Infection: A Systematic Review and Meta-Analysis. Nicotine Tob. Res. 2020, 22, 1657–1659. [Google Scholar] [CrossRef]
- Farsalinos, K.; Bagos, P.G.; Giannouchos, T.; Niaura, R.; Barbouni, A.; Poulas, K. Smoking Prevalence among Hospitalized COVID-19 Patients and Its Association with Disease Severity and Mortality: An Expanded Re-Analysis of a Recent Publication. Harm Reduct. J. 2021, 18, 9. [Google Scholar] [CrossRef]
- Chen, R.; Hui, K.P.-Y.; Liang, Y.; Ng, K.-C.; Nicholls, J.M.; Ip, M.S.-M.; Peiris, M.; Chan, M.C.-W.; Mak, J.C.-W. SARS-CoV-2 Infection Aggravates Cigarette Smoke-Exposed Cell Damage in Primary Human Airway Epithelia. Virol. J. 2023, 20, 65. [Google Scholar] [CrossRef] [PubMed]
- Patanavanich, R.; Glantz, S.A. Smoking Is Associated with Worse Outcomes of COVID-19 Particularly among Younger Adults: A Systematic Review and Meta-Analysis. BMC Public Health 2021, 21, 1554. [Google Scholar] [CrossRef] [PubMed]
- Klok, F.A.; Boon, G.J.A.M.; Barco, S.; Endres, M.; Geelhoed, J.J.M.; Knauss, S.; Rezek, S.A.; Spruit, M.A.; Vehreschild, J.; Siegerink, B. The Post-COVID-19 Functional Status Scale: A Tool to Measure Functional Status over Time after COVID-19. Eur. Respir. J. 2020, 56, 2001494. [Google Scholar] [CrossRef]
- Maamar, M.; Artime, A.; Pariente, E.; Fierro, P.; Ruiz, Y.; Gutiérrez, S.; Tobalina, M.; Díaz-Salazar, S.; Ramos, C.; Olmos, J.M.; et al. Post-COVID-19 Syndrome, Low-Grade Inflammation and Inflammatory Markers: A Cross-Sectional Study. Curr. Med. Res. Opin. 2022, 38, 901–909. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Tan, C.; Wu, J.; Chen, M.; Wang, Z.; Luo, L.; Zhou, X.; Liu, X.; Huang, X.; Yuan, S.; et al. Impact of Coronavirus Disease 2019 on Pulmonary Function in Early Convalescence Phase. Respir. Res. 2020, 21, 163. [Google Scholar] [CrossRef]
- Oakes, J.M.; Fuchs, R.M.; Gardner, J.D.; Lazartigues, E.; Yue, X. Nicotine and the Renin-Angiotensin System. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2018, 315, R895–R906. [Google Scholar] [CrossRef]
- Jacobs, M.; Van Eeckhoutte, H.P.; Wijnant, S.R.A.; Janssens, W.; Joos, G.F.; Brusselle, G.G.; Bracke, K.R. Increased Expression of ACE2, the SARS-CoV-2 Entry Receptor, in Alveolar and Bronchial Epithelium of Smokers and COPD Subjects. Eur. Respir. J. 2020, 56, 2002378. [Google Scholar] [CrossRef]
- Aloufi, N.; Traboulsi, H.; Ding, J.; Fonseca, G.J.; Nair, P.; Huang, S.K.; Hussain, S.N.A.; Eidelman, D.H.; Baglole, C.J. Angiotensin-Converting Enzyme 2 Expression in COPD and IPF Fibroblasts: The Forgotten Cell in COVID-19. Am. J. Physiol. Lung Cell. Mol. Physiol. 2021, 320, L152–L157. [Google Scholar] [CrossRef] [PubMed]
- Bellini, D.; Capodiferro, P.; Vicini, S.; Rengo, M.; Carbone, I. Long COVID in Young Patients: Impact on Lung Volume Evaluated Using Multidetector CT. Tomography 2023, 9, 1276–1285. [Google Scholar] [CrossRef]
- Toh, M.R.; Teo, Y.R.; Poh, L.C.R.; Tang, Y.; Soh, R.Y.; Sharma, K.; Kalyanasundaram, G.; Poh, K.C. Impact of COVID Infection on Lung Function Test and Quality of Life. Sci. Rep. 2023, 13, 17275. [Google Scholar] [CrossRef] [PubMed]
- Hama Amin, B.J.; Kakamad, F.H.; Ahmed, G.S.; Ahmed, S.F.; Abdulla, B.A.; Mohammed, S.H.; Mikael, T.M.; Salih, R.Q.; Ali, R.K.; Salh, A.M.; et al. Post COVID-19 Pulmonary Fibrosis; a Meta-Analysis Study. Ann. Med. Surg. 2022, 77, 103590. [Google Scholar] [CrossRef] [PubMed]
- Aul, D.R.; Gates, D.J.; Draper, D.A.; Dunleavy, D.A.; Ruickbie, D.S.; Meredith, D.H.; Walters, D.N.; Van Zeller, D.C.; Taylor, D.V.; Bridgett, D.M.; et al. Complications after Discharge with COVID-19 Infection and Risk Factors Associated with Development of Post-COVID Pulmonary Fibrosis. Respir. Med. 2021, 188, 106602. [Google Scholar] [CrossRef] [PubMed]
- Delpino, M.V.; Quarleri, J. SARS-CoV-2 Pathogenesis: Imbalance in the Renin-Angiotensin System Favors Lung Fibrosis. Front. Cell. Infect. Microbiol. 2020, 10, 340. [Google Scholar] [CrossRef]
- Hu, Z.-J.; Xu, J.; Yin, J.-M.; Li, L.; Hou, W.; Zhang, L.-L.; Zhou, Z.; Yu, Y.-Z.; Li, H.-J.; Feng, Y.-M.; et al. Lower Circulating Interferon-Gamma Is a Risk Factor for Lung Fibrosis in COVID-19 Patients. Front. Immunol. 2020, 11, 585647. [Google Scholar] [CrossRef]
- Dhillon, N.K.; Murphy, W.J.; Filla, M.B.; Crespo, A.J.; Latham, H.A.; O’Brien-Ladner, A. Down Modulation of IFN-γ Signaling in Alveolar Macrophages Isolated from Smokers. Toxicol. Appl. Pharmacol. 2009, 237, 22–28. [Google Scholar] [CrossRef] [PubMed]
- Samanta, D.; Gonzalez, A.L.; Nagathihalli, N.; Ye, F.; Carbone, D.P.; Datta, P.K. Smoking Attenuates Transforming Growth Factor-β–Mediated Tumor Suppression Function through Downregulation of Smad3 in Lung Cancer. Cancer Prev. Res. 2012, 5, 453–463. [Google Scholar] [CrossRef] [PubMed]
- Baraldo, S. Decreased Expression of TGF- Type II Receptor in Bronchial Glands of Smokers with COPD. Thorax 2005, 60, 998–1002. [Google Scholar] [CrossRef][Green Version]
- Farghaly, S.; Badedi, M.; Ibrahim, R.; Sadhan, M.H.; Alamoudi, A.; Alnami, A.; Muhajir, A. Clinical Characteristics and Outcomes of Post-COVID-19 Pulmonary Fibrosis: A Case-Control Study. Medicine 2022, 101, e28639. [Google Scholar] [CrossRef]
- Lv, D.; Chen, X.; Wang, X.; Mao, L.; Sun, J.; Wu, G.; Lin, Z.; Lin, R.; Yu, J.; Wu, X.; et al. Pulmonary Function of Patients with 2019 Novel Coronavirus Induced-Pneumonia: A Retrospective Cohort Study. Ann. Palliat. Med. 2020, 9, 3447–3452. [Google Scholar] [CrossRef]
- Gao, Q.; Hu, K.; Yan, C.; Zhao, B.; Mei, F.; Chen, F.; Zhao, L.; Shang, Y.; Ma, Y.; Ma, B. Associated Factors of Sarcopenia in Community-Dwelling Older Adults: A Systematic Review and Meta-Analysis. Nutrients 2021, 13, 4291. [Google Scholar] [CrossRef] [PubMed]
- Orea-Tejeda, A.; Robles-Hernández, R.; González-Islas, D.; Jimenez-Gallardo, L.; Gochicoa-Rangel, L.; Castorena-Maldonado, A.; Hernández-Zenteno, R.; Montañez-Orozco, A.; Valderrábano-Salas, B. Dynapenia and Sarcopenia in Post-COVID-19 Syndrome Hospitalized Patients Are Associated with Severe Reduction in Pulmonary Function. JCM 2023, 12, 6466. [Google Scholar] [CrossRef] [PubMed]
- Steffl, M.; Bohannon, R.W.; Petr, M.; Kohlikova, E.; Holmerova, I. Relation Between Cigarette Smoking and Sarcopenia: Meta-Analysis. Physiol. Res. 2015, 64, 419–426. [Google Scholar] [CrossRef]
- Van Bakel, S.I.; Gosker, H.R.; Langen, R.C.; Schols, A.M. Towards Personalized Management of Sarcopenia in COPD. COPD 2021, 16, 25–40. [Google Scholar] [CrossRef] [PubMed]
- Byun, M.K.; Cho, E.N.; Chang, J.; Ahn, C.M.; Kim, H.J. Sarcopenia Correlates with Systemic Inflammation in COPD. COPD 2017, 12, 669–675. [Google Scholar] [CrossRef]
- Sanhueza, S.; Vidal, M.A.; Hernandez, M.A.; Henriquez-Beltran, M.E.; Cabrera, C.; Quiroga, R.; Antilef, B.E.; Aguilar, K.P.; Castillo, D.A.; Llerena, F.J.; et al. Clinical and Pulmonary Function Analysis in Long-COVID Revealed That Long-Term Pulmonary Dysfunction Is Associated with Vascular Inflammation Pathways and Metabolic Syndrome. Front. Med. 2023, 10, 1271863. [Google Scholar] [CrossRef]
- Altara, R.; Manca, M.; Hessel, M.H.; Gu, Y.; Van Vark, L.C.; Akkerhuis, K.M.; Staessen, J.A.; Struijker-Boudier, H.A.J.; Booz, G.W.; Blankesteijn, W.M. CXCL10 Is a Circulating Inflammatory Marker in Patients with Advanced Heart Failure: A Pilot Study. J. Cardiovasc. Trans. Res. 2016, 9, 302–314. [Google Scholar] [CrossRef]
- Wang, H.; Chen, H.; Fu, Y.; Liu, M.; Zhang, J.; Han, S.; Tian, Y.; Hou, H.; Hu, Q. Effects of Smoking on Inflammatory-Related Cytokine Levels in Human Serum. Molecules 2022, 27, 3715. [Google Scholar] [CrossRef]
- Rezel-Potts, E.; Douiri, A.; Sun, X.; Chowienczyk, P.J.; Shah, A.M.; Gulliford, M.C. Cardiometabolic Outcomes up to 12 Months after COVID-19 Infection. A Matched Cohort Study in the UK. PLoS Med. 2022, 19, e1004052. [Google Scholar] [CrossRef]
- Szoltysek-Boldys, I.; Zielinska-Danch, W.; Loboda, D.; Wilczek, J.; Gibinski, M.; Paradowska-Nowakowska, E.; Golba, K.S.; Sarecka-Hujar, B. Photoplethysmographic Measurement of Arterial Stiffness in Polish Patients with Long-COVID-19 Syndrome—The Results of a Cross-Sectional Study. Diagnostics 2022, 12, 3189. [Google Scholar] [CrossRef]
- Da Ré, A.; Gurgel, L.; Buffon, G.; Moura, W.; Marques Vidor, D.; Maahs, M. Tobacco Influence on Taste and Smell: Systematic Review of the Literature. Int. Arch. Otorhinolaryngol. 2018, 22, 081–087. [Google Scholar] [CrossRef] [PubMed]
- Bunyavanich, S.; Do, A.; Vicencio, A. Nasal Gene Expression of Angiotensin-Converting Enzyme 2 in Children and Adults. JAMA 2020, 323, 2427. [Google Scholar] [CrossRef] [PubMed]
- Demir, B.; Beyazyüz, E.; Beyazyüz, M.; Çelikkol, A.; Albayrak, Y. Long-Lasting Cognitive Effects of COVID-19: Is There a Role of BDNF? Eur. Arch. Psychiatry Clin. Neurosci. 2023, 273, 1339–1347. [Google Scholar] [CrossRef] [PubMed]
- Machaalani, R.; Chen, H. Brain Derived Neurotrophic Factor (BDNF), Its Tyrosine Kinase Receptor B (TrkB) and Nicotine. NeuroToxicology 2018, 65, 186–195. [Google Scholar] [CrossRef] [PubMed]
- Neves, C.D.C.; Lacerda, A.C.R.; Lima, L.P.; Lage, V.K.S.; Balthazar, C.H.; Leite, H.R.; Mendonça, V.A. Different Levels of Brain-Derived Neurotrophic Factor and Cortisol in Healthy Heavy Smokers. Braz. J. Med. Biol. Res. 2017, 50, e6424. [Google Scholar] [CrossRef] [PubMed]
- Jamal, M.; Van Der Does, W.; Elzinga, B.M.; Molendijk, M.L.; Penninx, B.W.J.H. Association Between Smoking, Nicotine Dependence, and BDNF Val66Met Polymorphism with BDNF Concentrations in Serum. Nicotine Tob. Res. 2015, 17, 323–329. [Google Scholar] [CrossRef]
- Menuchin-Lasowski, Y.; Schreiber, A.; Lecanda, A.; Mecate-Zambrano, A.; Brunotte, L.; Psathaki, O.E.; Ludwig, S.; Rauen, T.; Schöler, H.R. SARS-CoV-2 Infects and Replicates in Photoreceptor and Retinal Ganglion Cells of Human Retinal Organoids. Stem Cell Rep. 2022, 17, 789–803. [Google Scholar] [CrossRef] [PubMed]
- Kanberg, N.; Grahn, A.; Stentoft, E.; Bremell, D.; Yilmaz, A.; Studahl, M.; Nilsson, S.; Schöll, M.; Gostner, J.M.; Blennow, K.; et al. COVID-19 Recovery: Consistent Absence of Cerebrospinal Fluid Biomarker Abnormalities in Patients with Neurocognitive Post-COVID Complications. J. Infect. Dis. 2023, 77, jiad395. [Google Scholar] [CrossRef]
- Wong, A.C.; Devason, A.S.; Umana, I.C.; Cox, T.O.; Dohnalová, L.; Litichevskiy, L.; Perla, J.; Lundgren, P.; Etwebi, Z.; Izzo, L.T.; et al. Serotonin Reduction in Post-Acute Sequelae of Viral Infection. Cell 2023, 186, 4851–4867.e20. [Google Scholar] [CrossRef]
- Karkala, A.; Moschonas, S.; Sykas, G.; Karagianni, M.; Gilou, S.; Papaefthymiou, O.; Kourtidou-Papadeli, C. Sleep Quality and Mental Health Consequences of COVID-19 Pandemic in the Aviation Community in Greece. J. Occup. Environ. Med. 2022, 64, e567–e574. [Google Scholar] [CrossRef]
- Pascal, O.I.; Trofor, A.C.; Lotrean, L.M.; Filipeanu, D.; Trofor, L. Depression, Anxiety and Panic Disorders in Chronic Obstructive Pulmonary Disease Patients: Correlations with Tobacco Use, Disease Severity and Quality of Life. Tob. Induced Dis. 2017, 15, 23. [Google Scholar] [CrossRef] [PubMed]
- Syed, U.; Subramanian, A.; Wraith, D.C.; Lord, J.M.; McGee, K.; Ghokale, K.; Nirantharakumar, K.; Haroon, S. Incidence of Immune-Mediated Inflammatory Diseases Following COVID-19: A Matched Cohort Study in UK Primary Care. BMC Med. 2023, 21, 363. [Google Scholar] [CrossRef] [PubMed]
- Salehi, Z.; Motlagh Ghoochani, B.F.N.; Hasani Nourian, Y.; Jamalkandi, S.A.; Ghanei, M. The Controversial Effect of Smoking and Nicotine in SARS-CoV-2 Infection. Allergy Asthma Clin. Immunol. 2023, 19, 49. [Google Scholar] [CrossRef] [PubMed]
- Schaffner, A.; Risch, L.; Aeschbacher, S.; Risch, C.; Weber, M.C.; Thiel, S.L.; Jüngert, K.; Pichler, M.; Grossmann, K.; Wohlwend, N.; et al. Characterization of a Pan-Immunoglobulin Assay Quantifying Antibodies Directed against the Receptor Binding Domain of the SARS-CoV-2 S1-Subunit of the Spike Protein: A Population-Based Study. JCM 2020, 9, 3989. [Google Scholar] [CrossRef] [PubMed]
- Dong, X.; Zhou, Y.; Shu, X.; Bernstam, E.V.; Stern, R.; Aronoff, D.M.; Xu, H.; Lipworth, L. Comprehensive Characterization of COVID-19 Patients with Repeatedly Positive SARS-CoV-2 Tests Using a Large U.S. Electronic Health Record Database. Microbiol. Spectr. 2021, 9, e00327-21. [Google Scholar] [CrossRef]
- Johnston, E.; Bains, M.; Hunter, A.; Langley, T. The Impact of the COVID-19 Pandemic on Smoking, Vaping, and Smoking Cessation Services in the United Kingdom: A Qualitative Study. Nicotine Tob. Res. 2023, 25, 339–344. [Google Scholar] [CrossRef]
- Telatar, T.G.; Karadoğan, D.; Baykal, M.H.; Yurtsever, B.A. Role of Tobacco Exposure in the Course of COVID-19 Disease and the Impact of the Disease on Smoking Behavior. Clin. Respir. J. 2022, 16, 57–62. [Google Scholar] [CrossRef]
- Kusuma, D.; Pradeepa, R.; Khawaja, K.I.; Hasan, M.; Siddiqui, S.; Mahmood, S.; Ali Shah, S.M.; De Silva, C.K.; De Silva, L.; Gamage, M.; et al. Low Uptake of COVID-19 Prevention Behaviours and High Socioeconomic Impact of Lockdown Measures in South Asia: Evidence from a Large-Scale Multi-Country Surveillance Programme. SSM Popul. Health 2021, 13, 100751. [Google Scholar] [CrossRef]
- Lampropoulos, I.C.; Kirgou, P.; Raptis, D.G.; Rouka, E.; Kotsiou, O.; Papagiannis, D.; Daniil, Z.; Gourgoulianis, K.I.; Malli, F. Changes in Smoking Habits in Greece During the Lockdown Measures Due to COVID-19. In GeNeDis 2022; Vlamos, P., Ed.; Advances in Experimental Medicine and Biology; Springer: Cham, Switzerland, 2023; Volume 1425, pp. 275–281. ISBN 978-3-031-31985-3. [Google Scholar]
- Tattan-Birch, H.; Perski, O.; Jackson, S.; Shahab, L.; West, R.; Brown, J. COVID-19, Smoking, Vaping and Quitting: A Representative Population Survey in England. Addiction 2021, 116, 1186–1195. [Google Scholar] [CrossRef]
- Gómez-Sánchez, L.; Tamayo-Morales, O.; Suárez-Moreno, N.; Bermejo-Martín, J.F.; Domínguez-Martín, A.; Martín-Oterino, J.A.; Martín-González, J.I.; González-Calle, D.; García-García, Á.; Lugones-Sánchez, C.; et al. Relationship between the Structure, Function and Endothelial Damage, and Vascular Ageing and the Biopsychological Situation in Adults Diagnosed with Persistent COVID (BioICOPER Study). A Research Protocol of a Cross-Sectional Study. Front. Physiol. 2023, 14, 1236430. [Google Scholar] [CrossRef]
| First Author | Year Published | Type (Cohort Study Unless Otherwise Specified) | Cohort Size | Results/Conclusions |
|---|---|---|---|---|
| Subramanian A et al. [4] | 2022 | 486,149 | smoking and former smoking, high BMI, and a wide range of comorbidities were all associated with an increased risk of reporting symptoms ≥12 weeks after infection | |
| Lippi G et al. [5] | 2023 | review | cigarette smoking (OR, 1.26; 95% CI, 1.04–1.54) as a clinical predictor of the risk of developing long COVID | |
| Bai F et al. [6] | 2022 | 377 | active smoking (AOR 0.19 for former smokers vs. active smokers, 95% CI 0.06–0.62, p = 0.002) were also associated with a higher risk of long COVID | |
| Wong MC et al. [7] | 2023 | 2712 | smoking associated with severe long COVID (OR = 1.55, 95% CI 1.17–2.05) | |
| Pinato DJ et al. [8] | 2021 | 2634 cancer patients | patients with a history of smoking (vs. no smoking history; p = 0.0004) at higher risk of developing sequelae | |
| Desgranges F et al. [9] | 2022 | 418 | predictor of memory impairment associated with long COVID | |
| Conti V et al. [10] | 2023 | review | active smoking, older age and female gender associated with higher risk of developing post-COVID-19 syndrome | |
| Muzyka I et al. [11] | 2023 | 332 | unclear effect | |
| Mohamed Hussein AA et al. [12] | 2021 | 444 | smoking status has a detrimental effect on pulmonary function (PCFS scale); assessment at 35.31 ± 18.75 days after symptom onset | |
| Wang C et al. [13] | 2023 | review | smoking possibly associated with an increased risk of developing symptoms of post-acute COVID-19 syndrome | |
| Whitaker M et al. [14] | 2022 | 508,707 + 97,727 | smoking and vaping associated with persistence of one or more symptoms for 12 weeks or more (some models of multivariable analysis) | |
| Carrasco-Garrido P et al. [15] | 2022 | 391 | higher benzodiazepine and Z-hypnotics use among females with long COVID after stratifying for alcohol and tobacco use | |
| Barthélémy H et al. [16] | 2022 | 956 | smoking found to be a predictor of the risk of cutaneous manifestations (OR = 2.34; 95% CI: 1.39–3.92) and tachycardia/hypertension (OR = 2.05; 95% CI: 1.2–3.47); assessment after more than 60 days from onset of symptoms; smoking cessation recommended | |
| Jacobs ET, et al. [17] | 2023 | 1224 | no significant effect of smoking history on risk of developing post-acute COVID-19 | |
| Román-Montes CM et al. [18] | 2023 | 246 | smoking more prevalent among post-COVID-19-syndrome patients; no significant association with dyspnea | |
| Wu Q et al. [19] | 2022 | 308 | no predictive role for current smoking status | |
| Takakura K et al. [20] | 2023 | 286 | improvement of long COVID may be delayed by smoking; smoking cessation recommended | |
| Afroze F et al. [21] | 2022 | 362 | various comorbidities and smoking status are considered independent risk factors for developing neurological and cardiovascular manifestations | |
| Buonsenso D et al. [22] | 2022 | 155 | risk factor for not resuming work among long COVID patients (OR 4.106, CI (0.4–11.9), smoking cessation recommended, anxiety more prevalent among female patients | |
| Tarifi A et al. [23] | 2021 | 86 | no significant effect on smell or taste, possibly due to small cohort size | |
| Kisiel MA et al. [24] | 2023 | 401 + 98 + 85 | smoking and snuff use associated with higher post-COVID-19 symptomatology scores | |
| Chathoth AT et al. [25] | 2023 | 938 | smoking considered a significant predictor of the risk of limited functional status associated with post-COVID-19 syndrome | |
| Mclaughlin M et al. [26] | 2023 | 253 | greater number of symptoms reported by smokers vs non-smokers or ex-smokers | |
| Tene L et al. [27] | 2023 | 180,759 | long COVID associated with smoking (OR = 1.532; 95% CI: 1.358–1.727) | |
| Paul E et al. [28] | 2022 | 1581 | smokers and ex-smokers with long COVID at higher risk for experiencing self-care-related difficulties; smoking cessation recommended | |
| Chilunga FP et al. [29] | 2023 | 1886 | no clear role; possible ethnic differences | |
| Bamps L et al. [30] | 2023 | 1598 | smoking associated with higher risk of long COVID | |
| Vásconez-González J et al. [31] | 2023 | 457 | smoking associated with higher risk of developing persistent fatigue in pregnant women with long COVID | |
| Akinci Ozyurek B et al. [32] | 2021 | 315 | no significant role of smoking; assessment one month after onset of symptoms | |
| Hennawi YB et al. [33] | 2023 | 2497 | smoking associated with significantly longer duration of ageusia | |
| Chen Y et al. [34] | 2022 | 121 | smoking associated with higher risk of chronic cough (OR 6.95 95% CI: 1.46–33.14); secondhand smoking is mentioned | |
| Emecen AN et al. [35] | 2023 | 5610 | current smoking associated with increased self-reporting of chronic symptoms (OR 1.15, 95% CI: 1.02–1.29) | |
| Cansel N et al. [36] | 2021 | 102 | smoking is associated with higher risk of moderate or severe anxiety (OR, 4, 95% CI 1.2–12.5) and higher risk of moderate or severe depression (OR, 8.8, 95% CI 2.5–30.8) | |
| Wallis TJM et al. [37] | 2021 | 101 | smoking status reported as an independent predictor of the risk of chest X-ray anomaly at 12 weeks after recovery from acute SARS-CoV-2 | |
| Tan HQM et al. [38] | 2022 | 150 | no role for smoking in the risk of developing persistent olfactory/taste impairment | |
| Li Z et al. [39] | 2023 | 535 | smoking associated with poor sleep quality (OR 2.005, 95% CI 1.044–3.850), anxiety (OR 4.491, 95% CI 2.276–8.861), and depression (OR 5.459, 95% CI 2.651–11.239) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Trofor, A.C.; Robu Popa, D.; Melinte, O.E.; Trofor, L.; Vicol, C.; Grosu-Creangă, I.A.; Crișan Dabija, R.A.; Cernomaz, A.T. Looking at the Data on Smoking and Post-COVID-19 Syndrome—A Literature Review. J. Pers. Med. 2024, 14, 97. https://doi.org/10.3390/jpm14010097
Trofor AC, Robu Popa D, Melinte OE, Trofor L, Vicol C, Grosu-Creangă IA, Crișan Dabija RA, Cernomaz AT. Looking at the Data on Smoking and Post-COVID-19 Syndrome—A Literature Review. Journal of Personalized Medicine. 2024; 14(1):97. https://doi.org/10.3390/jpm14010097
Chicago/Turabian StyleTrofor, Antigona Carmen, Daniela Robu Popa, Oana Elena Melinte, Letiția Trofor, Cristina Vicol, Ionela Alina Grosu-Creangă, Radu Adrian Crișan Dabija, and Andrei Tudor Cernomaz. 2024. "Looking at the Data on Smoking and Post-COVID-19 Syndrome—A Literature Review" Journal of Personalized Medicine 14, no. 1: 97. https://doi.org/10.3390/jpm14010097
APA StyleTrofor, A. C., Robu Popa, D., Melinte, O. E., Trofor, L., Vicol, C., Grosu-Creangă, I. A., Crișan Dabija, R. A., & Cernomaz, A. T. (2024). Looking at the Data on Smoking and Post-COVID-19 Syndrome—A Literature Review. Journal of Personalized Medicine, 14(1), 97. https://doi.org/10.3390/jpm14010097






