Physical Examination-Indicated Cerclage in Singleton and Twin Pregnancies and Risk Factors for Predicting Preterm Birth < 28 Weeks
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Stoll, B.J.; Hansen, N.I.; Bell, E.F.; Shankaran, S.; Laptook, A.R.; Walsh, M.C.; Hale, E.C.; Newman, N.S.; Schibler, K.; Carlo, W.A.; et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics 2010, 126, 443–456. [Google Scholar] [CrossRef] [PubMed]
- Manuck, T.A.; Rice, M.M.; Bailit, J.L.; Grobman, W.A.; Reddy, U.M.; Wapner, R.J.; Thorp, J.M.; Caritis, S.N.; Prasad, M.; Tita, A.T.; et al. Preterm neonatal morbidity and mortality by gestational age: A contemporary cohort. Am. J. Obstet. Gynecol. 2016, 215, 103.e1–103.e14. [Google Scholar] [CrossRef] [PubMed]
- Bell, E.F.; Hintz, S.R.; Hansen, N.I.; Bann, C.M.; Wyckoff, M.H.; DeMauro, S.B.; Walsh, M.C.; Vohr, B.R.; Stoll, B.J.; Carlo, W.A.; et al. Mortality, In-Hospital Morbidity, Care Practices, and 2-Year Outcomes for Extremely Preterm Infants in the US, 2013–2018. JAMA 2022, 327, 248–263. [Google Scholar] [CrossRef] [PubMed]
- Draper, E.S.; Manktelow, B.; Field, D.J.; James, D. Prediction of survival for preterm births. BMJ 2000, 321, 237. [Google Scholar] [CrossRef] [PubMed]
- Liem, S.M.; van de Mheen, L.; Bekedam, D.J.; van Pampus, M.G.; Opmeer, B.C.; Lim, A.C.; Mol, B.W. Cervical length measurement for the prediction of preterm birth in symptomatic women with a twin pregnancy: A systematic review and meta-analysis. Obstet. Gynecol. Int. 2013, 2013, 125897. [Google Scholar] [CrossRef]
- Roman, A.; Rochelson, B.; Martinelli, P.; Saccone, G.; Harris, K.; Zork, N.; Spiel, M.; O’Brien, K.; Calluzzo, I.; Palomares, K.; et al. Cerclage in twin pregnancy with dilated cervix between 16 to 24 weeks of gestation: Retrospective cohort study. Am. J. Obstet. Gynecol. 2016, 215, 98.e1–98.e11. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Shen, J.; Hua, K. Cerclage for women with twin pregnancies: A systematic review and metaanalysis. Am. J. Obstet. Gynecol. 2019, 220, 543–557.e1. [Google Scholar] [CrossRef]
- Mathew, G.; Agha, R.; Albrecht, J.; Goel, P.; Mukherjee, I.; Pai, P.; D’Cruz, A.K.; Nixon, I.J.; Roberto, K.; Enam, S.A.; et al. STROCSS 2021: Strengthening the reporting of cohort, cross-sectional and case-control studies in surgery. Int. J. Surg. 2021, 96, 106165. [Google Scholar] [CrossRef]
- Son, G.H.; Chang, K.H.; Song, J.E.; Lee, K.Y. Use of a uniconcave balloon in emergency cerclage. Am. J. Obstet. Gynecol. 2015, 212, 114.e1–114.e4. [Google Scholar] [CrossRef]
- Lee, J.; Romero, R.; Kim, S.M.; Chaemasaithong, P.; Yoon, B.H. A new antibiotic regimen treats and prevents intra-amniotic infection/inflammation in patients with preterm PROM. J. Matern. Fetal. Neonatal. Med. 2016, 29, 2727–2737. [Google Scholar] [CrossRef]
- Martin, J.A.; Hamilton, B.E.; Osterman, M.J.; Driscoll, A.K.; Mathews, T.J. Births: Final Data for 2015. Natl. Vital Stat. Rep. 2017, 66, 1. [Google Scholar] [PubMed]
- Saccone, G.; Rust, O.; Althuisius, S.; Roman, A.; Berghella, V. Cerclage for short cervix in twin pregnancies: Systematic review and meta-analysis of randomized trials using individual patient-level data. Acta Obstet. Gynecol. Scand. 2015, 94, 352–358. [Google Scholar] [CrossRef] [PubMed]
- Rafael, T.J.; Berghella, V.; Alfirevic, Z. Cervical stitch (cerclage) for preventing preterm birth in multiple pregnancy. Cochrane Database Syst. Rev. 2014, 9, CD009166. [Google Scholar] [CrossRef] [PubMed]
- Su, J.; Li, D.; Yang, Y.; Cao, Y.; Yin, Z. Cerclage placement in twin pregnancies with cervical dilation: A systematic review and meta-analysis. J. Matern. Fetal. Neonatal. Med. 2022, 35, 9112–9118. [Google Scholar] [CrossRef] [PubMed]
- Roman, A.; Zork, N.; Haeri, S.; Schoen, C.N.; Saccone, G.; Colihan, S.; Zelig, C.; Gimovsky, A.C.; Seligman, N.S.; Zullo, F.; et al. Physical examination-indicated cerclage in twin pregnancy: A randomized controlled trial. Am. J. Obstet. Gynecol. 2020, 223, 902.e1–902.e11. [Google Scholar] [CrossRef] [PubMed]
- Ekici, H.; Okmen, F.; Saritas, D.G.; Khaligli, G.; Ergenoglu, A.M. Cervical cerclage in twin pregnancies: Obstetric and neonatal outcomes. Ir. J. Med. Sci. 2023, 192, 1751–1755. [Google Scholar] [CrossRef] [PubMed]
- Ponce, J.; Benitez, L.; Banos, N.; Gonce, A.; Bennasar, M.; Munoz, M.; Cobo, T.; Palacio, M. Latency to delivery in physical examination-indicated cerclage in twins is similar to that in singleton pregnancies. Int. J. Gynaecol. Obstet. 2022, 159, 188–194. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Chen, M.; Cao, T.; Zeng, S.; Chen, R.; Liu, X. Cervical cerclage in twin pregnancies: An updated systematic review and meta-analysis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2021, 260, 137–149. [Google Scholar] [CrossRef]
- Miller, E.S.; Rajan, P.V.; Grobman, W.A. Outcomes after physical examination-indicated cerclage in twin gestations. Am. J. Obstet. Gynecol. 2014, 211, 46.e1–46.e5. [Google Scholar] [CrossRef]
- Melchor, J.C.; Khalil, A.; Wing, D.; Schleussner, E.; Surbek, D. Prediction of preterm delivery in symptomatic women using PAMG-1, fetal fibronectin and phIGFBP-1 tests: Systematic review and meta-analysis. Ultrasound Obstet. Gynecol. 2018, 52, 442–451. [Google Scholar] [CrossRef]
- Tripathi, R.; Tyagi, S.; Mala, Y.M.; Singh, N.; Pandey, N.B.; Yadav, P. Comparison of rapid bedside tests for phosphorylated insulin-like growth factor-binding protein 1 and fetal fibronectin to predict preterm birth. Int. J. Gynaecol. Obstet. 2016, 135, 47–50. [Google Scholar] [CrossRef] [PubMed]
- Berghella, V.; Saccone, G. Fetal fibronectin testing for reducing the risk of preterm birth. Cochrane Database Syst. Rev. 2019, 7, CD006843. [Google Scholar] [CrossRef] [PubMed]
- Practice Bulletin No. 171: Management of Preterm Labor. Obstet. Gynecol. 2016, 128, e155–e164.
- Jun, S.Y.; Lee, J.Y.; Kim, H.M.; Kim, M.J.; Cha, H.H.; Seong, W.J. Evaluation of the effectiveness of foetal fibronectin as a predictor of preterm birth in symptomatic preterm labour women. BMC Pregnancy Childbirth 2019, 19, 241. [Google Scholar] [CrossRef]
- Ozel, A.; Alici Davutoglu, E.; Yurtkal, A.; Madazli, R. How do platelet-to-lymphocyte ratio and neutrophil-to-lymphocyte ratio change in women with preterm premature rupture of membranes, and threaten preterm labour? J. Obstet. Gynaecol. 2020, 40, 195–199. [Google Scholar] [CrossRef]
- Balciuniene, G.; Kvederaite-Budre, G.; Gulbiniene, V.; Dumalakiene, I.; Viliene, R.; Pilypiene, I.; Drasutiene, G.S.; Ramasauskaite, D. Neutrophil-lymphocyte ratio for the prediction of histological chorioamnionitis in cases of preterm premature rupture of membranes: A case-control study. BMC Pregnancy Childbirth 2021, 21, 656. [Google Scholar] [CrossRef]


| Twin (n = 28) | Singleton (n = 119) | p-Value | |
|---|---|---|---|
| Maternal age (years) | 33.21 ± 3.25 | 34.08 ± 3.82 | 0.268 |
| Elderly gravida a | 8 (28.6%) | 59 (49.6%) | 0.058 |
| Parity | 0.011 * | ||
| Primiparous | 22 (78.6%) | 61 (51.3%) | |
| Multiparous | 6 (21.4%) | 58 (48.7%) | |
| BMI (kg/m2) | 26.74 ± 5.69 | 25.67 ± 4.56 | 0.287 |
| BMI ≥ 30 | 8 (28.6%) | 20 (16.8%) | 0.182 |
| Prior preterm birth or second-trimester loss | 2 (7.1%) | 12 (10.1%) | 0.633 |
| Prior cervix operation | 0 (0%) | 2 (1.7%) | 0.490 |
| Assisted reproductive technology | 20 (71.4%) | 21 (17.6%) | <0.001 * |
| Twin (n = 28) | Singleton (n = 119) | p-Value | |
|---|---|---|---|
| GA at PEIC (weeks) | 21.34 ± 1.74 | 21.05 ± 1.97 | 0.476 |
| Cervical dilation (cm) | 2.91 ± 1.35 | 2.87 ± 1.31 | 0.865 |
| Prolapsed membrane into vagina | 20 (71.4%) | 84 (70.6%) | 0.930 |
| WBC | 11,889.29 ± 3652.80 | 11,181.76 ± 3002.84 | 0.284 |
| CRP (mg/L) | 9.05 ± 6.30 | 9.51 ± 10.10 | 0.817 |
| NLR | 8.67 ± 5.86 | 7.53 ± 4.40 | 0.252 |
| PLR | 189.63 ± 68.07 | 190.46 ± 72.79 | 0.956 |
| fFN/IGFBP-1 | 16 (57.1%) | 62 (52.1%) | 0.678 |
| Mycoplasma | 0 (0%) | 3 (2.5%) | 0.396 |
| Ureaplasma | 11 (39.3%) | 53 (44.5%) | 0.676 |
| Postoperative CL | 25.79 ± 5.69 | 26.30 ± 7.13 | 0.685 |
| Postoperative funneling | 7 (25.0%) | 18 (15.1%) | 0.262 |
| Twin (n = 28) | Singleton (n = 119) | p-Value | |
|---|---|---|---|
| GA at delivery (weeks) | 28.87 ± 5.15 | 30.67 ± 6.03 | 0.148 |
| <28 weeks | 15 (53.6%) | 43 (36.1%) | 0.131 |
| <32 weeks | 19 (67.9%) | 64 (53.8%) | 0.208 |
| <34 weeks | 19 (67.9%) | 78 (65.5%) | 0.816 |
| Term delivery (≥37 weeks) | 1 (3.6%) | 26 (21.8%) | 0.028 * |
| PEIC-to-delivery latency (days) | 52.75 ± 34.15 | 67.3 ± 42.30 | 0.059 |
| Cesarean section | 24 (85.7%) | 56 (47.1%) | <0.001 * |
| PPROM | 11 (39.3%) | 23 (19.3%) | 0.043 * |
| PTL | 18 (64.3%) | 68 (57.1%) | 0.530 |
| Placenta abruption | 1 (3.6%) | 4 (3.4%) | 0.956 |
| Birth weight (g) | 1313.98 ± 824.65 a | 1806.60 ± 1097.55 | 0.001 * |
| Apgar score at 1 min | 4.54 ± 3.00 a | 5.15 ± 3.11 | 0.219 |
| Apgar score at 5 min | 6.04 ± 3.21 a | 6.65 ± 3.09 | 0.229 |
| Stillbirth/immediate death | 9/56 (16.1%) a | 17 (14.3%) | 0.821 |
| Final Viable pregnancy | 50/56 (89.3%) a | 110 (92.4%) | 0.565 |
| NICU admission | 38/56 (67.9%) a | 80 (67.2%) | 0.934 |
| Composite complication | 16/56 (28.6%) a | 31 (26.1%) | 0.719 |
| <28 Weeks (n = 58) | ≥28 Weeks (n = 89) | p-Value | |
|---|---|---|---|
| Maternal age (years) | 34.52 ± 3.38 | 33.53 ± 3.90 | 0.989 |
| Elderly gravida a | 31 (53.4%) | 36 (40.4%) | 0.131 |
| Parity | 0.309 | ||
| Primiparous | 36 (62.1%) | 47 (52.8%) | |
| Multiparous | 22 (37.9%) | 42 (47.2%) | |
| BMI (kg/m2) | 26.47 ± 5.27 | 25.48 ± 4.44 | 0.223 |
| BMI ≥ 30 | 13 (22.4%) | 15 (16.9%) | 0.401 |
| Prior preterm birth or Second-trimester loss | 4 (6.9%) | 10 (11.2%) | 0.567 |
| Prior cervix operation | 1 (1.7%) | 1 (1.1%) | 0.759 |
| Assisted reproductive technology | 18 (31.0%) | 23 (25.8%) | 0.573 |
| Twin pregnancy | 15 (25.9%) | 13 (14.6%) | 0.131 |
| <28 Weeks (n = 58) | ≥28 Weeks (n = 89) | p-Value | |
|---|---|---|---|
| GA at PEIC (weeks) | 20.85 ± 1.99 | 21.27 ± 1.88 | 0.197 |
| Cervical dilation (cm) | 3.28 ± 1.43 | 2.61 ± 1.16 | 0.002 * |
| Cervical dilation ≥ 3.0 cm | 39 (67.2%) | 42 (47.2%) | 0.019 * |
| Prolapsed membrane into vagina | 47 (81.0%) | 57 (64.0%) | 0.041 * |
| WBC | 11,517.76 ± 3287.59 | 11,185.39 ± 3044.50 | 0.532 |
| CRP (mg/L) | 11.57 ± 10.71 | 8.03 ± 8.33 | 0.028 * |
| CRP ≥ 11.1 mg/L | 25 (43.9%) | 21 (23.9%) | 0.017 * |
| NLR | 8.84 ± 5.66 | 7.03 ± 3.85 | 0.035 * |
| NLR ≥ 7.1 | 31 (53.4%) | 30 (33.7%) | 0.026 * |
| PLR | 202.86 ± 73.98 | 182.13 ± 69.36 | 0.087 |
| fFN/IGFBP-1 | 37 (63.8%) | 41 (46.1%) | 0.043 * |
| Mycoplasma | 2 (3.4%) | 1 (1.1%) | 0.562 |
| Ureaplasma | 27 (46.6%) | 37 (4163%) | 0.611 |
| Postoperative CL | 24.74 ± 7.87 | 27.16 ± 5.98 | 0.049 * |
| Postoperative CL < 21.6 mm | 26 (44.8%) | 13 (14.6%) | <0.001 * |
| Postoperative funneling | 13 (22.4%) | 12 (13.5%) | 0.182 |
| <28 Weeks (n = 58) | ≥28 Weeks (n = 89) | p-Value | |
|---|---|---|---|
| GA at delivery (weeks) | 24.08 ± 2.15 | 34.40 ± 3.49 | <0.001 * |
| PEIC-to-delivery latency (days) | 22.59 ± 14.14 | 91.87 ± 27.69 | <0.001 * |
| Cesarean section | 36 (62.1%) | 44 (49.4%) | 0.175 |
| PPROM | 16 (27.6%) | 18 (20.2%) | 0.322 |
| PTL | 46 (79.3%) | 40 (44.9%) | <0.001 * |
| Placenta abruption | 4 (6.9%) | 1 (1.1%) | 0.079 |
| Birth weight (g) | 668.42 ± 223.45 a | 2350.72 ± 800.85 b | <0.001 * |
| Apgar score at 1 min | 1.97 ± 1.69 a | 7.09 ± 1.81 b | <0.001 * |
| Apgar score at 5 min | 3.47 ± 2.43 a | 8.59 ± 1.23 b | <0.001 * |
| Stillbirth/immediate death | 21/73 (28.8%) a | 5/102 (4.9%) b | <0.001 * |
| Final Viable pregnancy | 59/73 (80.8%) a | 101/102 (99.0%) b | <0.001 * |
| NICU admission | 58/73 (79.5%) a | 60/102 (58.8%) b | 0.005 * |
| Composite complication | 27/73 (37.0%) a | 20/102 (19.6%) | 0.015 * |
| OR | 95% CI | p-Value | |
|---|---|---|---|
| Cervical dilation ≥ 3.0 cm | 2.297 | 1.154–4.572 | 0.018 * |
| Prolapsed membrane | 2.399 | 1.093–5.266 | 0.029 * |
| CRP ≥ 11.1 mg/L | 2.493 | 1.217–5.105 | 0.013 * |
| NLR ≥ 7.1 | 2.258 | 1.147–4.447 | 0.019 * |
| fFN/IGFBP-1 | 2.063 | 1.046–4.066 | 0.037 * |
| Postoperative CL < 21.6 mm | 4.750 | 2.170–10.398 | <0.001 * |
| aOR | 95% CI | p-Value | |
|---|---|---|---|
| Cervical dilation ≥ 3.0 cm | 0.709 | 0.228–2.207 | 0.552 |
| Prolapsed membrane | 2.876 | 0.805–10.280 | 0.104 |
| CRP ≥ 11.1 mg/L | 1.606 | 0.712–3.623 | 0.254 |
| NLR ≥ 7.1 | 2.049 | 0.935–4.490 | 0.073 |
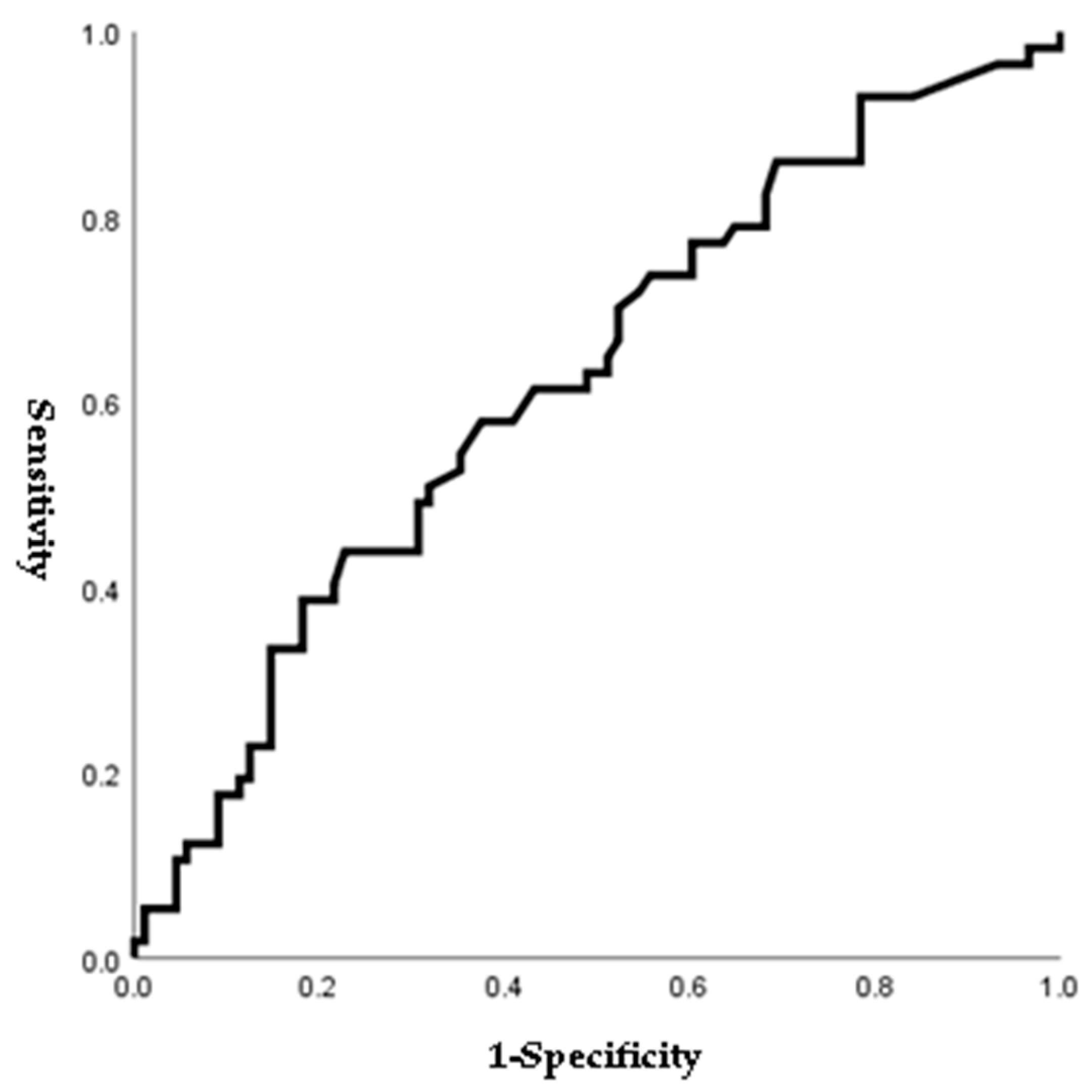
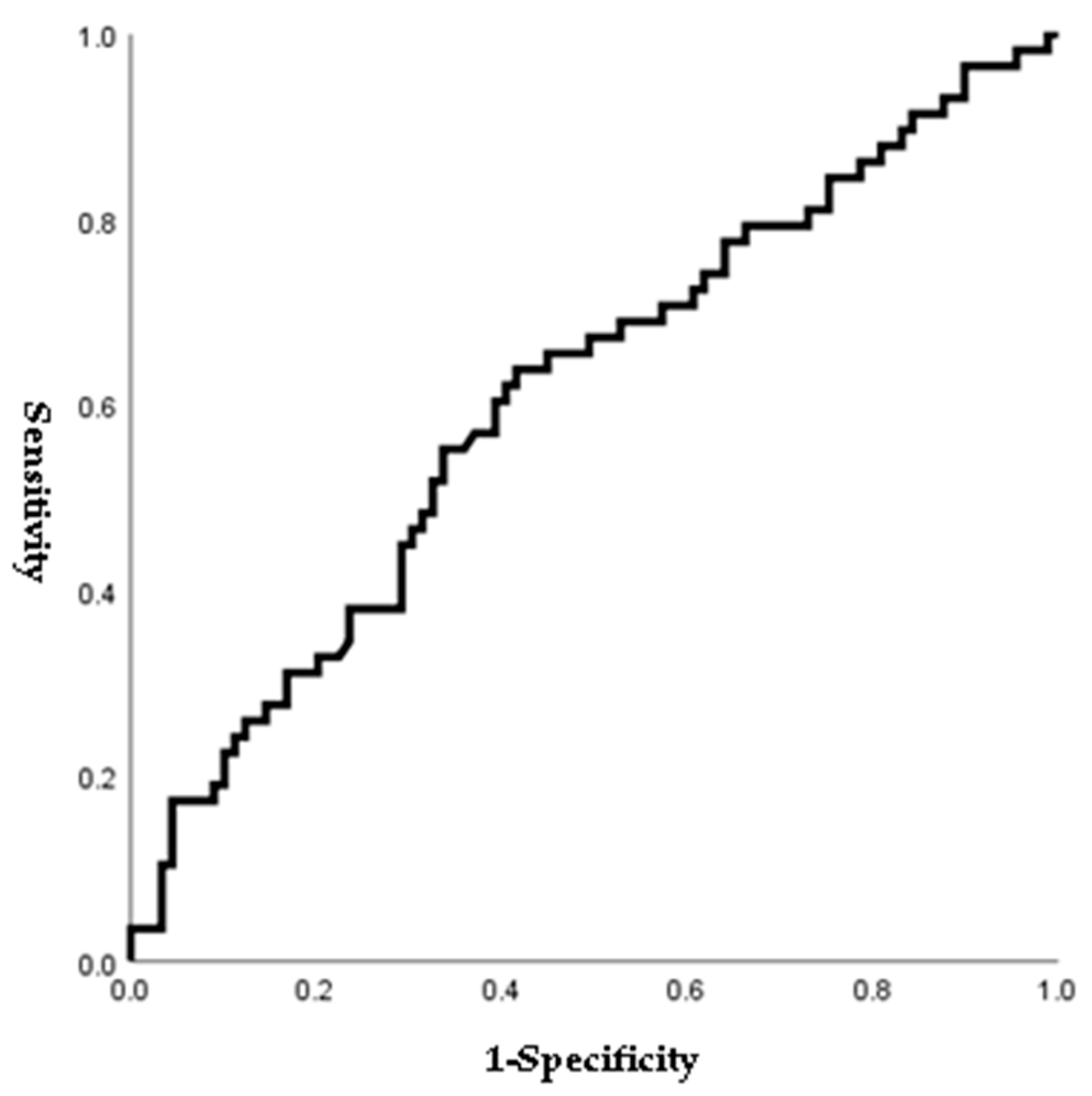
| fFN/IGFBP-1 | 2.311 | 1.042–5.125 | 0.039 * |
| Postoperative CL < 21.6 mm | 4.353 | 1.820–10.411 | 0.001 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Song, J.-E.; Park, S.; Ryu, J. Physical Examination-Indicated Cerclage in Singleton and Twin Pregnancies and Risk Factors for Predicting Preterm Birth < 28 Weeks. J. Pers. Med. 2024, 14, 38. https://doi.org/10.3390/jpm14010038
Song J-E, Park S, Ryu J. Physical Examination-Indicated Cerclage in Singleton and Twin Pregnancies and Risk Factors for Predicting Preterm Birth < 28 Weeks. Journal of Personalized Medicine. 2024; 14(1):38. https://doi.org/10.3390/jpm14010038
Chicago/Turabian StyleSong, Ji-Eun, Suyeon Park, and Jiwon Ryu. 2024. "Physical Examination-Indicated Cerclage in Singleton and Twin Pregnancies and Risk Factors for Predicting Preterm Birth < 28 Weeks" Journal of Personalized Medicine 14, no. 1: 38. https://doi.org/10.3390/jpm14010038
APA StyleSong, J.-E., Park, S., & Ryu, J. (2024). Physical Examination-Indicated Cerclage in Singleton and Twin Pregnancies and Risk Factors for Predicting Preterm Birth < 28 Weeks. Journal of Personalized Medicine, 14(1), 38. https://doi.org/10.3390/jpm14010038




