Targeting IL-4 and IL-13 Receptors on Eosinophils in CRSwNP Patients: The Clinical Efficacy of Dupilumab
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients Enrollment and Dupilumab Treatment
2.2. SNOT-22
2.3. NPS
2.4. NRS
2.5. Statistical Analysis
3. Results
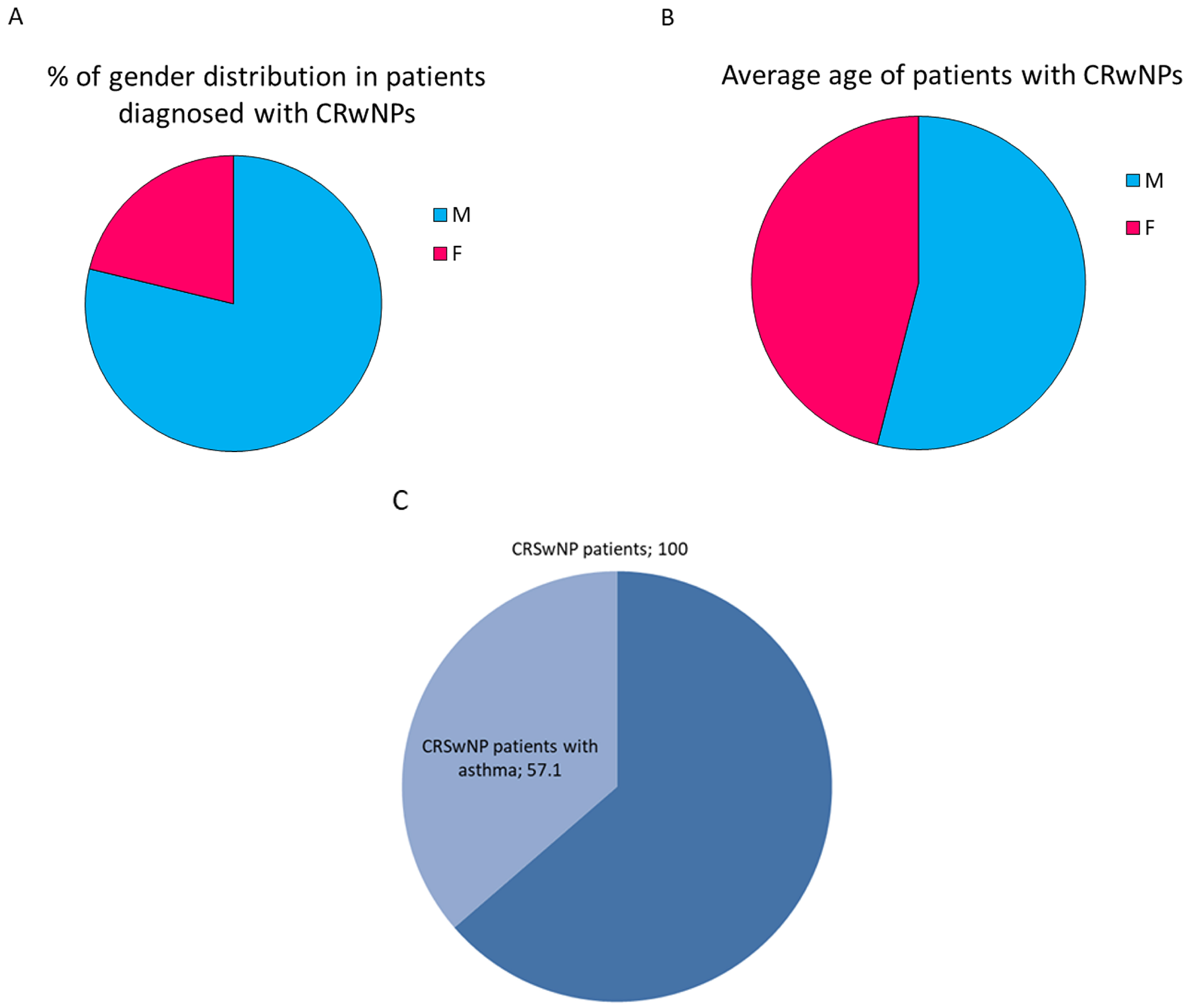
3.1. Distribution of CRSwNP Patients by Gender and Age
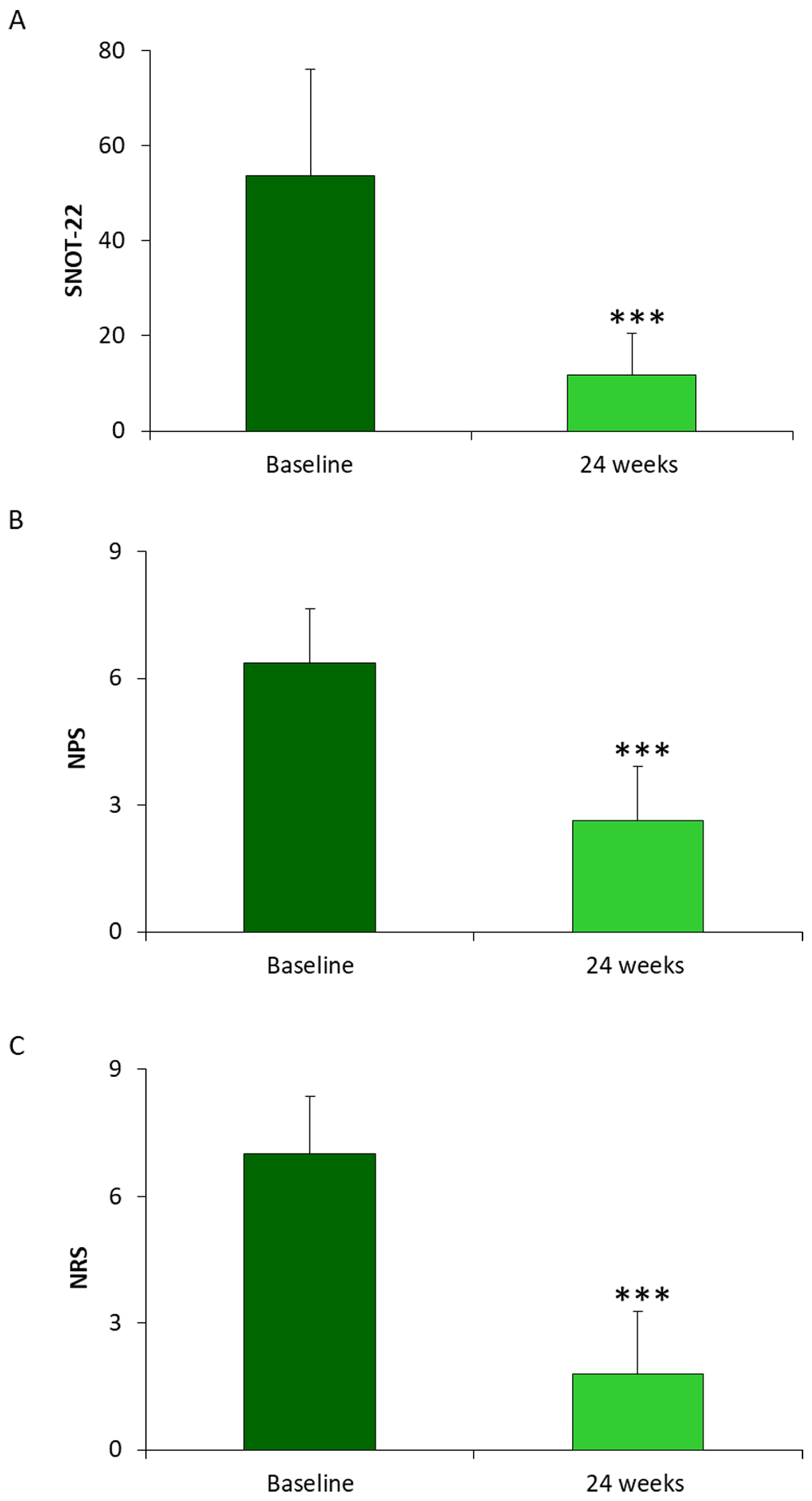
3.2. Determination of SNOT-22, NPS and NRS in Patients Diagnosed CRSwNP and Treated with Dupilumab for 24 Weeks
3.3. Determination of Peripheral Eosinophilia and Total IgE in Patients Diagnosed CRSwNP Treated with Dupilumab for 24 Weeks
3.4. Effectiveness of Dupilumab Administration in 14 CRSwNP Patients
4. Discussion
5. Conclusions
6. Originality and Study Limitation
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Schleimer, R.P. Immunopathogenesis of Chronic Rhinosinusitis and Nasal Polyposis. Annu. Rev. Pathol. 2017, 12, 331–357. [Google Scholar] [CrossRef] [PubMed]
- Mesuraca, M.; Nisticò, C.; Lombardo, N.; Piazzetta, G.L.; Lobello, N.; Chiarella, E. Cellular and Biochemical Characterization of Mesenchymal Stem Cells from Killian Nasal Polyp. Int. J. Mol. Sci. 2022, 23, 13214. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.H.; Hamilos, D.L.; Han, D.H.; Laidlaw, T.M. Phenotypes of Chronic Rhinosinusitis. J. Allergy Clin. Immunol. Pract. 2020, 8, 1505–1511. [Google Scholar] [CrossRef]
- Hopkins, C. Chronic Rhinosinusitis with Nasal Polyps. N. Engl. J. Med. 2019, 4, 55–63. [Google Scholar] [CrossRef]
- Sinead, A.; Anders, C. Inflammation and Endotyping in Chronic Rhinosinusitis—A Paradigm Shift. Medicina 2019, 55, 95. [Google Scholar] [CrossRef]
- Fokkens, W.J.; Lund, V.J.; Hopkins, C.; Hellings, P.W.; Kern, R.; Reitsma, S.; Toppila-Salmi, S.; Bernal-Sprekelsen, M.; Mullol, J.; Alobid, I.; et al. European Position Paper on Rhinosinusitis and Nasal Polyps. Rhinology 2020, 29, 464. [Google Scholar]
- Laidlaw, T.M.; Levy, J.M. NSAID-ERD Syndrome: The New Hope from Prevention, Early Diagnosis, and New Therapeutic Targets. Curr. Allergy Asthma. Rep. 2020, 20, 10. [Google Scholar] [CrossRef]
- Petalas, K.; Goudakos, J.; Konstantinou, J.N. Targeting Epithelium Dysfunction and Impaired Nasal Biofilms to Treat Immunological, Functional, and Structural Abnormalities of Chronic Rhinosinusitis. Int. J. Mol. Sci. 2023, 24, 12379. [Google Scholar] [CrossRef]
- Pelaia, C.; Pelaia, G.; Crimi, C.; Longhini, F.; Lombardo, N.; Savino, R.; Sciacqua, A.; Vatrella, A. Biologics in severe asthma. Minerva Med. 2022, 113, 51–62. [Google Scholar] [CrossRef]
- Chiarella, E.; Nicola Lombardo, N.; Lobello, N.; Giovanna Lucia Piazzetta, G.L.; Morrone, H.L.; Mesuraca, M.; Bond, H.M. Deficit in Adipose Differentiation in Mesenchymal Stem Cells Derived from Chronic Rhinosinusitis Nasal Polyps Compared to Nasal Mucosal Tissue. Int. J. Mol. Sci. 2020, 21, 9214. [Google Scholar] [CrossRef]
- Chiarella, E.; Lombardo, N.; Lobello, N.; Aloisio, A.; Aragona, T.; Pelaia, C.; Scicchitano, S.; Bond, H.M.; Mesuraca, M. Nasal Polyposis: Insights in Epithelial-Mesenchymal Transition and Differentiation of Polyp Mesenchymal Stem Cells. Int. J. Mol. Sci. 2020, 21, 6878. [Google Scholar] [CrossRef] [PubMed]
- Bachert, C.; Akdis, C.A. Phenotypes and Emerging Endotypes of Chronic Rhinosinusitis. J. Allergy Clin. Immunol. Pract. 2016, 4, 621–628. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Zhang, L. Use of biologics in chronic sinusitis with nasal polyps. Curr. Opin. Allergy Clin. Immunol. 2019, 19, 365–372. [Google Scholar] [CrossRef]
- Akdis, C.A.; Bachert, C.; Cingi, C.; Dykewicz, M.S.; Hellings, P.W.; Naclerio, R.M.; Schleimer, R.P.; Ledford, D. Endotypes and phenotypes of chronic rhinosinusitis: A PRACTALL document of the European Academy of Allergy and Clinical Immunology and the American Academy of Allergy, Asthma & Immunology. J. Allergy Clin. Immunol. 2013, 131, 1479–1490. [Google Scholar] [PubMed]
- Tomassen, P.; Vandeplas, G.; van Zele, T.; Cardell, L.O.; Arebro, J.; Olze, H.; Forster-Ruhrmann, U.; Kowalsky, M.L.; Olszewska-Ziaber, A.; Holtappels, G.; et al. Inflammatory endotypes of chronic rhinosinusitis based on cluster analysis of biomarkers. J. Allergy Clin. Immunol. 2016, 137, 1449–1456. [Google Scholar] [CrossRef] [PubMed]
- De Corso, E.; Pipolo, C.; Cantone, E.; Ottaviano, G.; Gallo, S.; Canevari, F.R.M.; Macchi, A.; Monti, G.; Cavaliere, C.; La Mantia, I.; et al. Survey on Use of Local and Systemic Corticosteroids in the Management of Chronic Rhinosinusitis with Nasal Polyps: Identification of Unmet Clinical Needs. J. Pers. Med. 2022, 12, 897. [Google Scholar] [CrossRef]
- Laidlaw, T.M.; Buchheit, K.M. Biologics in chronic rhinosinusitis with nasal polyposis. Ann. Allergy Asthma Immunol. 2020, 124, 326–332. [Google Scholar] [CrossRef]
- Gevaert, P.; Han, J.K.; Smith, S.G.; Sousa, A.R.; Howarth, P.H.; Yancey, S.W.; Chan, R.; Bachert, C. The roles of eosinophils and interleukin-5 in the pathophysiology of chronic rhinosinusitis with nasal polyps. Int. Forum. Allergy Rhinol. 2022, 12, 1413–1423. [Google Scholar] [CrossRef] [PubMed]
- Carsuzaa, F.; Béquignon, E.; Dufour, X.; de Bonnecaze, G.; Lecron, J.C.; Favot, L. Cytokine Signature and Involvement in Chronic Rhinosinusitis with Nasal Polyps. Int. J. Mol. Sci. 2022, 23, 417. [Google Scholar] [CrossRef] [PubMed]
- De Corso, E.; Bellocchi, G.; De Benedetto, M.; Lombardo, N.; Macchi, A.; Malvezzi, L.; Motta, G.; Pagella, F.; Vicini, C.; Passali, D. Biologics for severe uncontrolled chronic rhinosinusitis with nasal polyps: A change management approach. Consensus of the Joint Committee of Italian Society of Otorhinolaryngology on biologics in rhinology. Acta Otorhinolaryngol. Ital. 2022, 42, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Bachert, C.; Zhang, N.; Cavaliere, C.; Weiping, W.; Gevaert, E.; Krysko, O. Biologics for chronic rhinosinusitis with nasal polyps. J. Allergy Clin. Immunol. 2020, 145, 725–739. [Google Scholar] [CrossRef] [PubMed]
- Le Floc’h, A.; Allinne, J.; Nagashima, K.; Scott, G.; Birchard, D.; Asrat, C.S.; Bai, Y.; Lim, W.K.; Martin, J.; Huang, T.; et al. Dual blockade of IL-4 and IL-13 with dupilumab, an IL-4Rα antibody, is required to broadly inhibit type 2 inflammation. Allergy 2020, 75, 1188–1204. [Google Scholar] [CrossRef] [PubMed]
- Bachert, C.; Han, J.K.; Desrosiers, M.; Hellings, P.W.; Amin, N.; Lee, S.E.; Mullol, J.; Greos, L.S.; Bosso, J.V.; Laidlaw, T.M.; et al. Efficacy and safety of dupilumab in patients with severe chronic rhinosinusitis with nasal polyps (LIBERTY NP SINUS-24 and LIBERTY NP SINUS-52): Results from two multicentre, randomised, double-blind, placebo-controlled, parallel-group phase 3 trials. Lancet 2019, 394, 1638–1650. [Google Scholar] [CrossRef] [PubMed]
- Pelaia, C.; Lombardo, N.; Busceti, M.T.; Piazzetta, G.; Crimi, C.; Calabrese, C.; Vatrella, A.; Pelaia, G. Short-Term Evaluation of Dupilumab Effects in Patients with Severe Asthma and Nasal Polyposis. J. Asthma Allergy 2021, 14, 1165–1172. [Google Scholar] [CrossRef] [PubMed]
- Hoy, S.M. Dupilumab: A Review in Chronic Rhinosinusitis with Nasal Polyps. Drugs 2020, 80, 711–717. [Google Scholar] [CrossRef] [PubMed]
- Pavord, I.D.; Deniz, Y.; Corren, J.; Casale, T.B.; FitzGerald, J.M.; Izuhara, K.; Daizadeh, N.; Ortiz, B.; Johnson, R.R.; Harel, S.; et al. Baseline FeNO Independently Predicts the Dupilumab Response in Patients With Moderate-to-Severe Asthma. J. Allergy Clin. Immunol. Pract. 2023, 11, 1213–1220. [Google Scholar] [CrossRef]
- Hamilton, J.D.; Harel, S.; Swanson, B.N.; Brian, W.; Chen, Z.; Rice, M.S.; Amin, N.; Ardeleanu, M.; Radin, A.; Shumel, B.; et al. Dupilumab suppresses type 2 inflammatory biomarkers across multiple atopic, allergic diseases. Clin. Exp. Allergy 2021, 51, 915–931. [Google Scholar] [CrossRef]
- Tandon, M.; Singh, A.; Saluja, V.; Dhankhar, M.; Pandey, C.K.; Jain, P. Validation of a New “Objective Pain Score” vs. “Numeric Rating Scale” For the Evaluation of Acute Pain: A Comparative Study. Anesthesiol. Pain Med. 2016, 6, e32101. [Google Scholar] [CrossRef]
- Galletti, C.; Barbieri, M.A.; Ciodaro, F.; Freni, F.; Galletti, F.; Spina, E.; Galletti, B. Effectiveness and Safety Profile of Dupilumab in Chronic Rhinosinusitis with Nasal Polyps: Real-Life Data in Tertiary Care. Pharmaceuticals 2023, 16, 630. [Google Scholar] [CrossRef] [PubMed]
- De Corso, E.; Seccia, V.; Ottaviano, G.; Cantone, E.; Lucidi, D.; Settimi, S.; Di Cesare, T.; Galli, J. Clinical Evidence of Type 2 Inflammation in Non-allergic Rhinitis with Eosinophilia Syndrome: A Systematic Review. Curr. Allergy Asthma Rep. 2022, 22, 29–42. [Google Scholar] [CrossRef]
- Bansal, A.; Simpson, E.L.; Paller, A.S.; Siegfried, E.C.; Blauvelt, A.; de Bruin-Weller, M.; Corren, J.; Sher, L.; Guttman-Yassky, E.; Chen, Z.; et al. Conjunctivitis in Dupilumab Clinical Trials for Adolescents with Atopic Dermatitis or Asthma. Am. J. Clin. Dermatol. 2021, 22, 101–115. [Google Scholar] [CrossRef]
- Kai, M.; Vion, P.A.; Boussouar, S.; Cacoub, P.; Saadoun, D.; Le Joncour, A. Eosinophilic granulomatosis polyangiitis (EGPA) complicated with periaortitis, precipitating role of dupilumab? A case report a review of the literature. RMD Open 2023, 9, e003300. [Google Scholar] [CrossRef]
- Carsuzaa, F.; Fath, L.; Fieux, M.; Bartier, S.; de Bonnecaze, G.; Rumeau, C.; Michel, J.; Papon, J.F.; Alexandru, M.; Favier, V. Definition of severity and treatment response in chronic rhinosinusitis with nasal polyps: A Delphi study among French experts. Expert Rev. Clin. Immunol. 2023, 19, 1005–1011. [Google Scholar] [CrossRef]
- Peters, A.T.; Wagenmann, M.; Bernstein, J.A.; Khan, A.H.; Nash, S.; Jacob-Nara, J.A.; Siddiqui, S.; Rowe, P.J.; Deniz, Y. Dupilumab efficacy in patients with chronic rhinosinusitis with nasal polyps with and without allergic rhinitis. Allergy Asthma Proc. 2023, 44, 265–274. [Google Scholar] [CrossRef] [PubMed]
- Jansen, F.; Becker, B.; Eden, J.K.; Breda, P.C.; Hot, A.; Oqueka, T.; Betz, C.S.; Hoffmann, A.S. Dupilumab (Dupixent®) tends to be an effective therapy for uncontrolled severe chronic rhinosinusitis with nasal polyps: Real data of a single-centered, retrospective single-arm longitudinal study from a university hospital in Germany. Eur. Arch. Otorhinolaryngol. 2023, 280, 1741–1755. [Google Scholar] [CrossRef]
- Mullol, J.; Bachert, C.; Amin, N.; Desrosiers, M.; Hellings, P.W.; Han, J.K.; Jankowski, R.; Vodicka, J.; Gevaert, P.; Daizadeh, N.; et al. Olfactory Outcomes With Dupilumab in Chronic Rhinosinusitis With Nasal Polyps. J. Allergy Clin. Immunol. Pract. 2022, 10, 1086–1095.e5. [Google Scholar] [CrossRef] [PubMed]
- Ottaviano, G.; Saccardo, T.; Roccuzzo, G.; Bernardi, R.; Chicco, A.D.; Pendolino, A.L.; Scarpa, B.; Mairani, E.; Nicolai, P. Effectiveness of Dupilumab in the Treatment of Patients with Uncontrolled Severe CRSwNP: A “Real-Life” Observational Study in Naïve and Post-Surgical Patients. J. Pers. Med. 2022, 12, 1526. [Google Scholar] [CrossRef]
- De Corso, E.; Pasquini, E.; Trimarchi, M.; La Mantia, I.; Pagella, F.; Ottaviano, G.; Garzaro, M.; Pipolo, C.; Torretta, S.; Seccia, V.; et al. Dupilumab in the treatment of severe uncontrolled chronic rhinosinusitis with nasal polyps (CRSwNP): A multicentric observational Phase IV real-life study (DUPIREAL). Allergy, 2023; online ahead of print. [Google Scholar] [CrossRef]
- Caminati, M.; Olivieri, B.; Dama, A.; Micheletto, C.; Paggiaro, P.; Pinter, P.; Senna, G.; Schiappoli, M. Dupilumab-induced hypereosinophilia: Review of the literature and algorithm proposal for clinical management. Expert Rev. Respir. Med. 2022, 16, 713–721. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Jorizzo, J.L. Retrospective analysis of adverse events with dupilumab reported to the United States Food and Drug Administration. J. Am. Acad. Dermatol. 2021, 84, 1010–1014. [Google Scholar] [CrossRef]


| Patients | Sex | Age |
|---|---|---|
| 1 | M | 52 |
| 2 | M | 75 |
| 3 | F | 61 |
| 4 | F | 31 |
| 5 | M | 47 |
| 6 | F | 68 |
| 7 | M | 79 |
| 8 | M | 73 |
| 9 | M | 59 |
| 10 | M | 54 |
| 11 | M | 66 |
| 12 | M | 59 |
| 13 | M | 62 |
| 14 | M | 62 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Piazzetta, G.L.; Lobello, N.; Chiarella, E.; Rizzuti, A.; Pelaia, C.; Pelaia, G.; Lombardo, N. Targeting IL-4 and IL-13 Receptors on Eosinophils in CRSwNP Patients: The Clinical Efficacy of Dupilumab. J. Pers. Med. 2023, 13, 1404. https://doi.org/10.3390/jpm13091404
Piazzetta GL, Lobello N, Chiarella E, Rizzuti A, Pelaia C, Pelaia G, Lombardo N. Targeting IL-4 and IL-13 Receptors on Eosinophils in CRSwNP Patients: The Clinical Efficacy of Dupilumab. Journal of Personalized Medicine. 2023; 13(9):1404. https://doi.org/10.3390/jpm13091404
Chicago/Turabian StylePiazzetta, Giovanna Lucia, Nadia Lobello, Emanuela Chiarella, Alberta Rizzuti, Corrado Pelaia, Girolamo Pelaia, and Nicola Lombardo. 2023. "Targeting IL-4 and IL-13 Receptors on Eosinophils in CRSwNP Patients: The Clinical Efficacy of Dupilumab" Journal of Personalized Medicine 13, no. 9: 1404. https://doi.org/10.3390/jpm13091404
APA StylePiazzetta, G. L., Lobello, N., Chiarella, E., Rizzuti, A., Pelaia, C., Pelaia, G., & Lombardo, N. (2023). Targeting IL-4 and IL-13 Receptors on Eosinophils in CRSwNP Patients: The Clinical Efficacy of Dupilumab. Journal of Personalized Medicine, 13(9), 1404. https://doi.org/10.3390/jpm13091404







