Minimally Invasive Postero-Inferior Sacroiliac Joint Fusion: Surgical Technique and Procedural Details
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Structural Anatomy Overview
3.2. Patient Selection
- Moderate to severe pain with functional impairment and pain persists despite a minimum of 6 months of intensive nonoperative treatment that must include medication optimization, activity modification, bracing, and active therapeutic exercise targeted at the lumbar spine, pelvis, SIJ, and hip including a home exercise program.
- A patient that reports typically unilateral pain that is caudal to the lumbar spine (L5 vertebrae), localized over the posterior SIJ, and consistent with SIJ pain.
- A thorough physical examination demonstrating localized tenderness with palpation over the sacral sulcus (Fortin’s point) in the absence of tenderness of similar severity elsewhere (e.g., greater trochanter, lumbar spine, and coccyx) and that other obvious sources for their pain have been ruled out.
- Positive response to a cluster of 3 provocative tests (e.g., thigh thrust test, compression test, Gaenslen’s test, distraction test, FABER test, and posterior provocation test).
- Absence of generalized pain behavior or generalized pain disorders (e.g., fibromyalgia) contributing to the SIJ-area pain.
- Diagnostic imaging studies that include ALL of the following:
- −
- Imaging (plain radiographs and a CT or MRI) of the SIJ that excludes the presence of destructive lesions (e.g., tumor, infection), fracture, traumatic SIJ instability, or inflammatory arthropathy that would not be properly addressed by percutaneous SIJ fusion;
- −
- Imaging of the pelvis (AP plain radiograph) to rule out concomitant hip pathology;
- −
- Imaging of the lumbar spine (CT or MRI) to rule out neural compression or other degenerative condition that can be causing low back or buttock pain.
- At least a 75 percent reduction of pain for the expected duration of a standard anesthetic agent, and the ability to perform previously painful maneuvers, following an image-guided, contrast-enhanced intra-articular SIJ injection;
- A trial of at least two or more intra-articular SIJ injections, with at least one injection being therapeutic (i.e., corticosteroid injection).
3.3. Surgical Technique
3.3.1. Patient Positioning
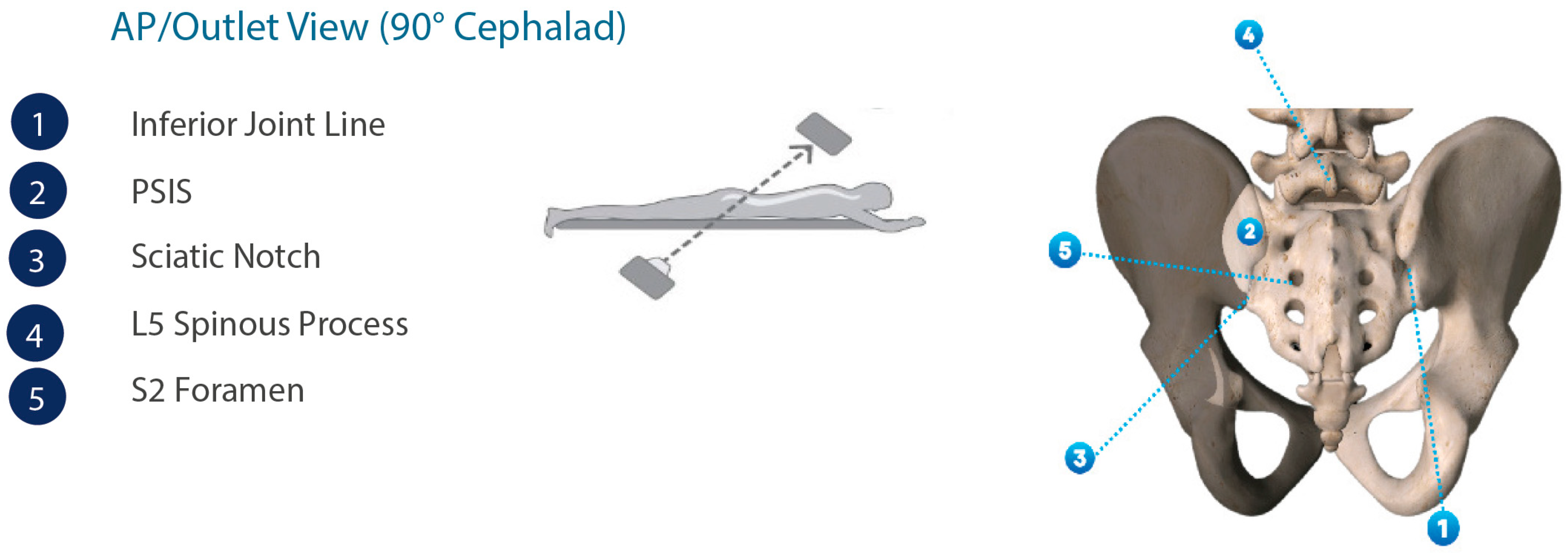
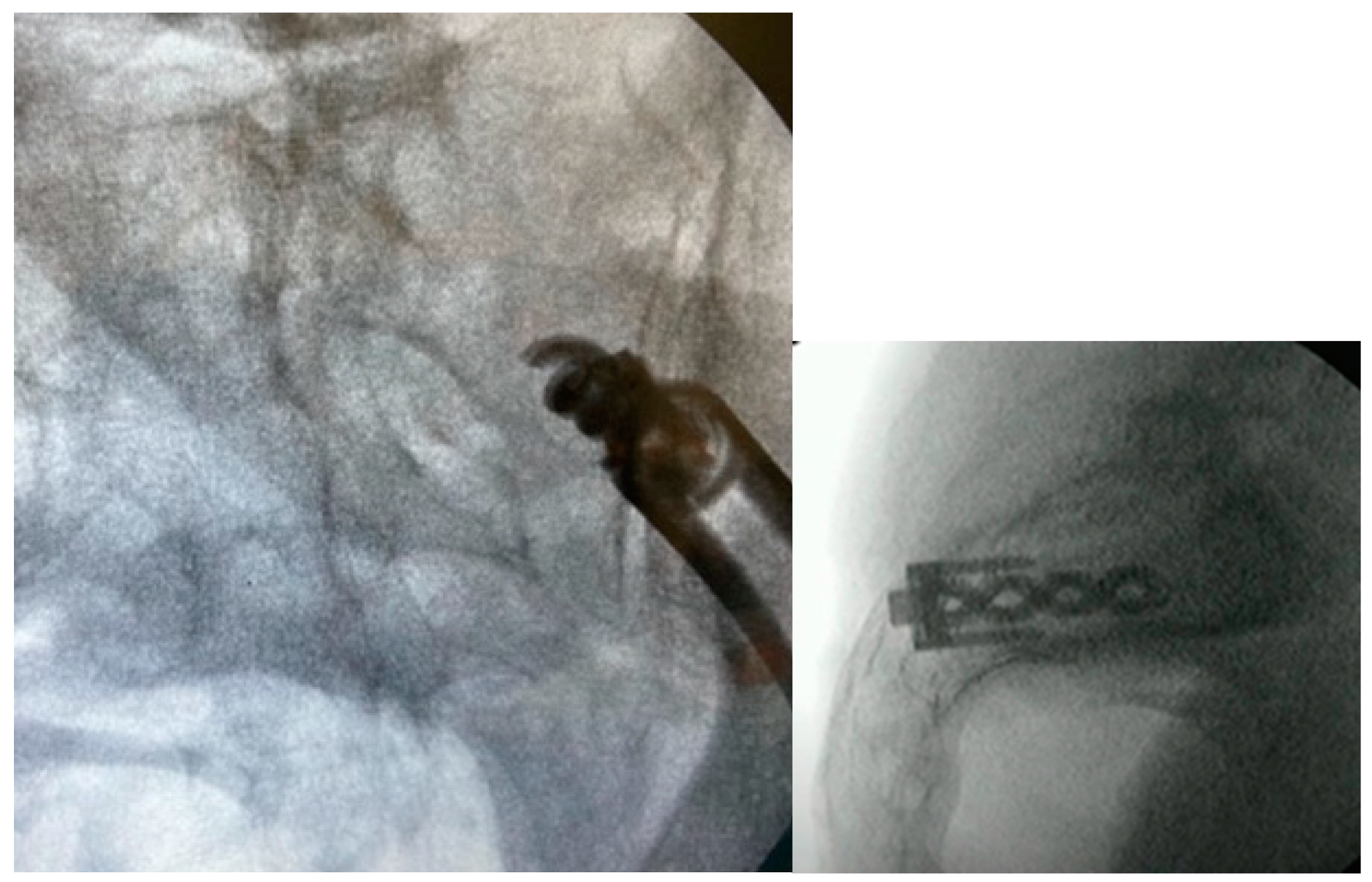
3.3.2. Intraoperative Imaging
3.3.3. Approach and Incision
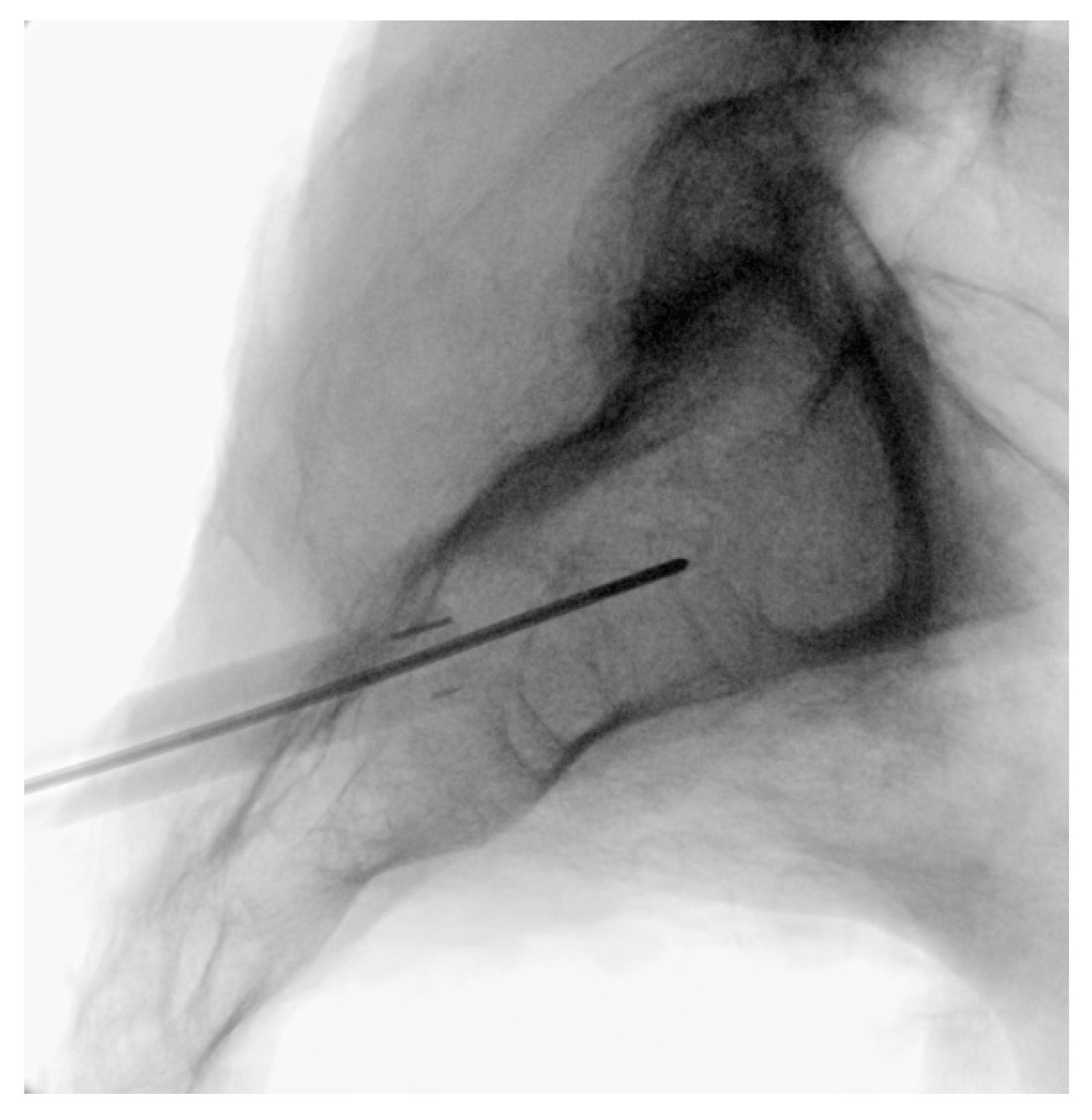
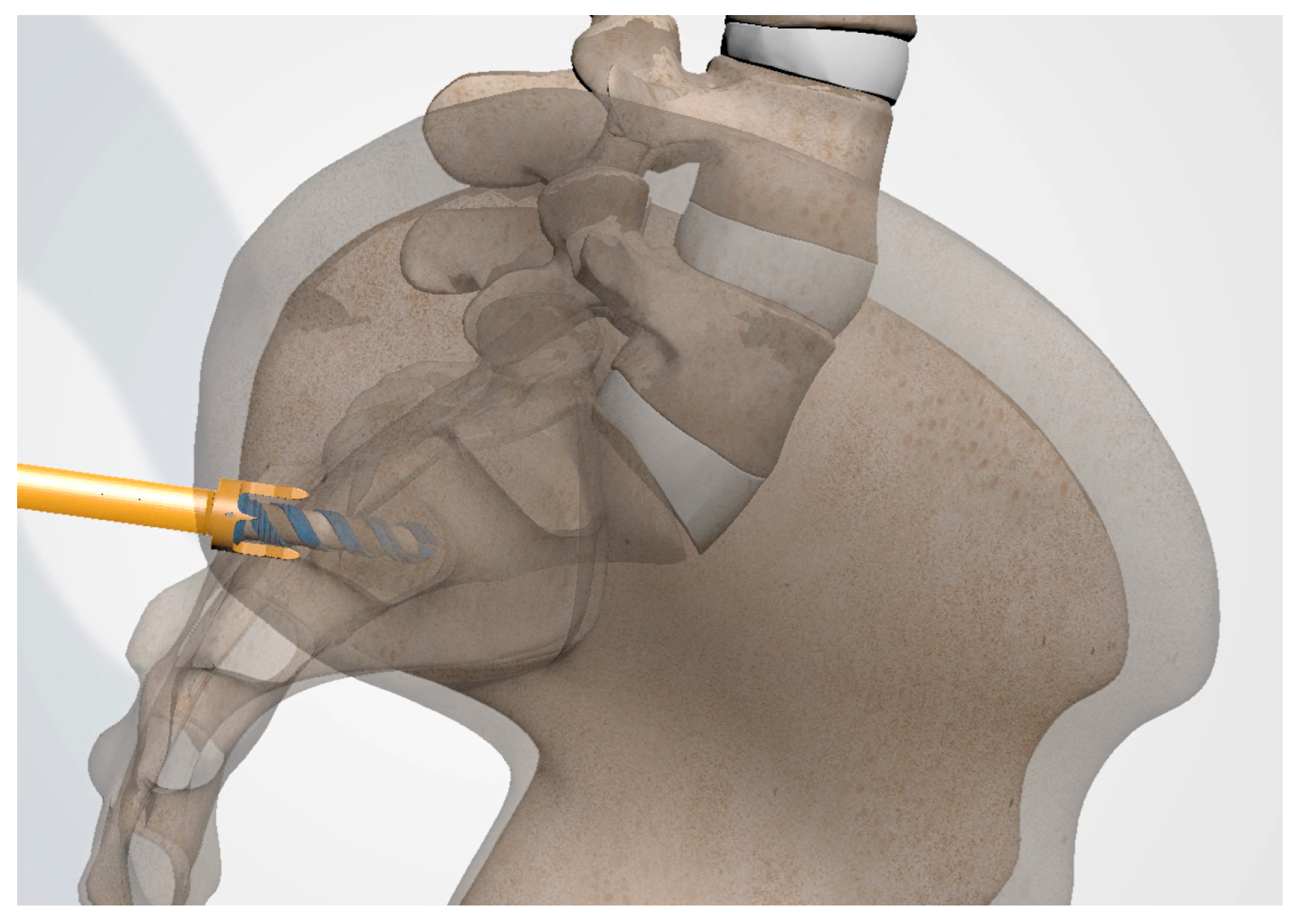
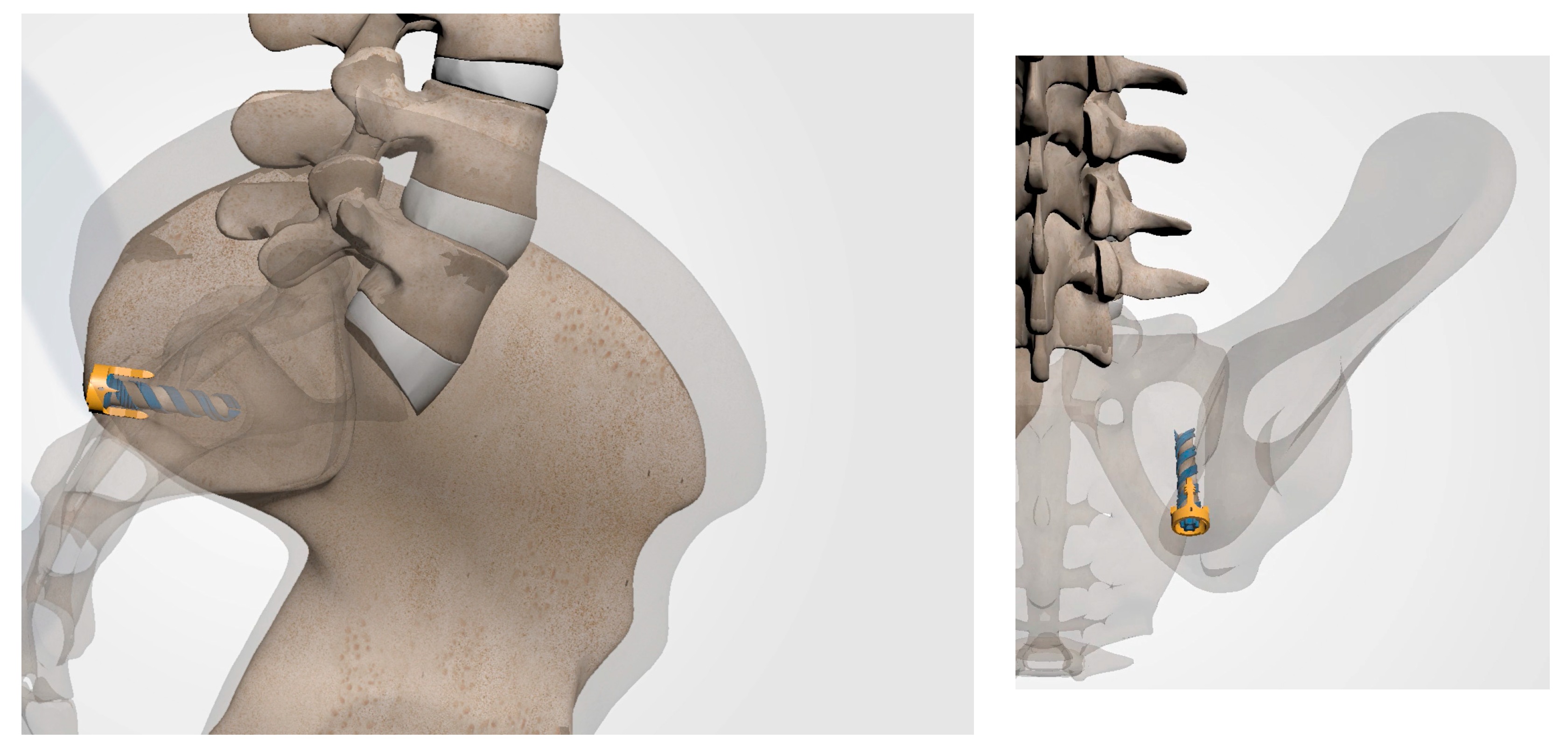
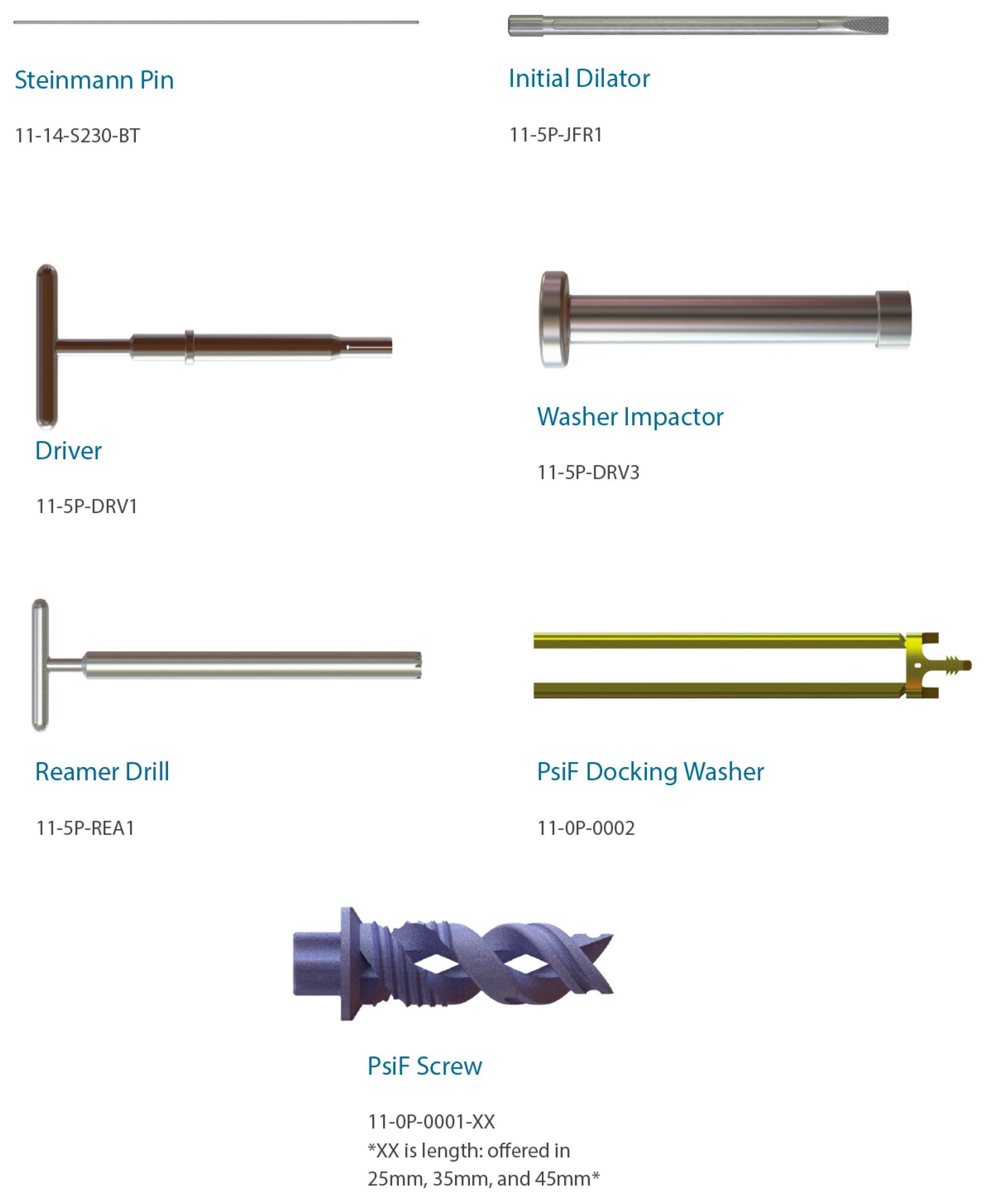
3.3.4. Steinman Pin Placement
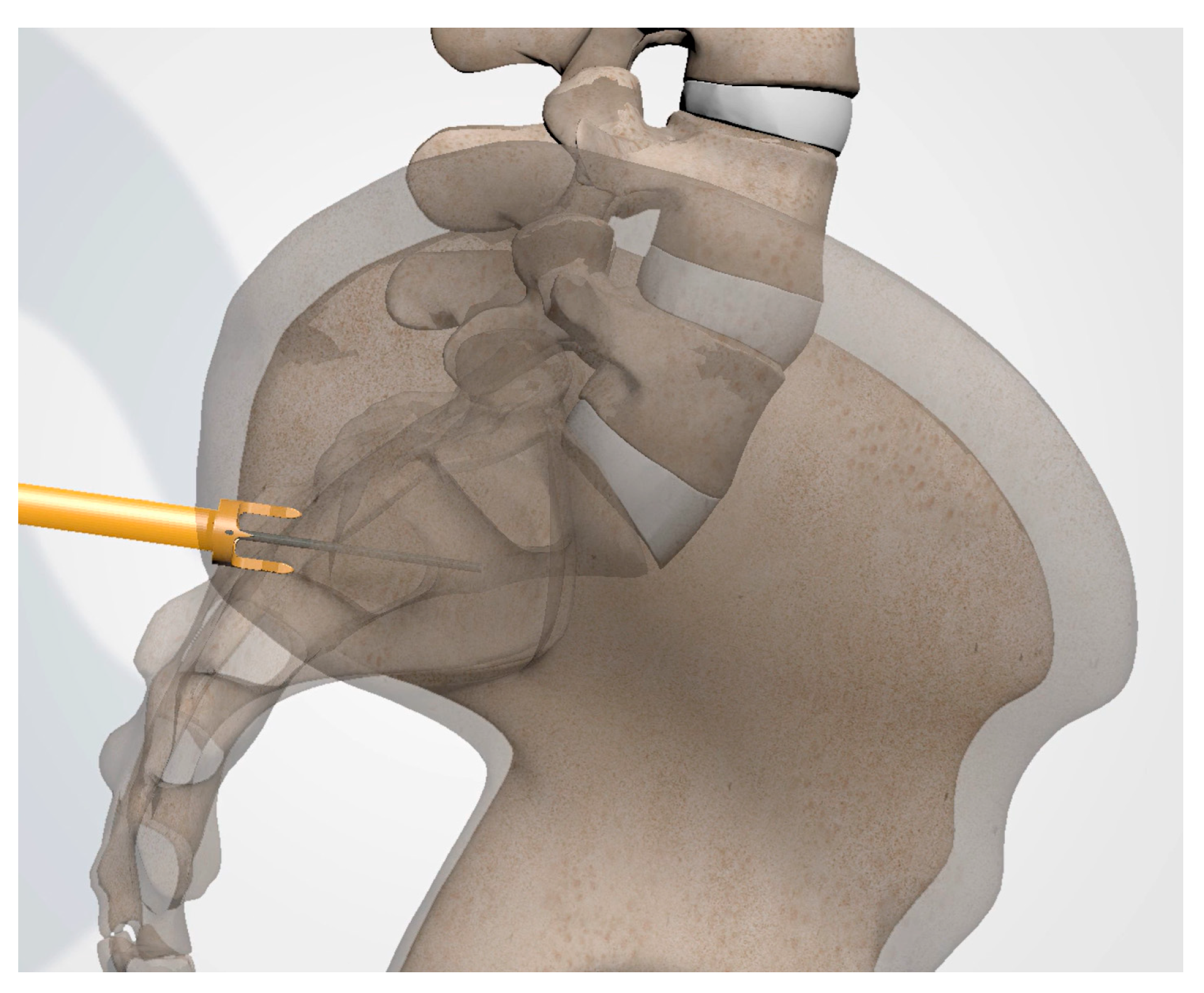
3.3.5. Tissue Dilation
3.3.6. Implant Preparation
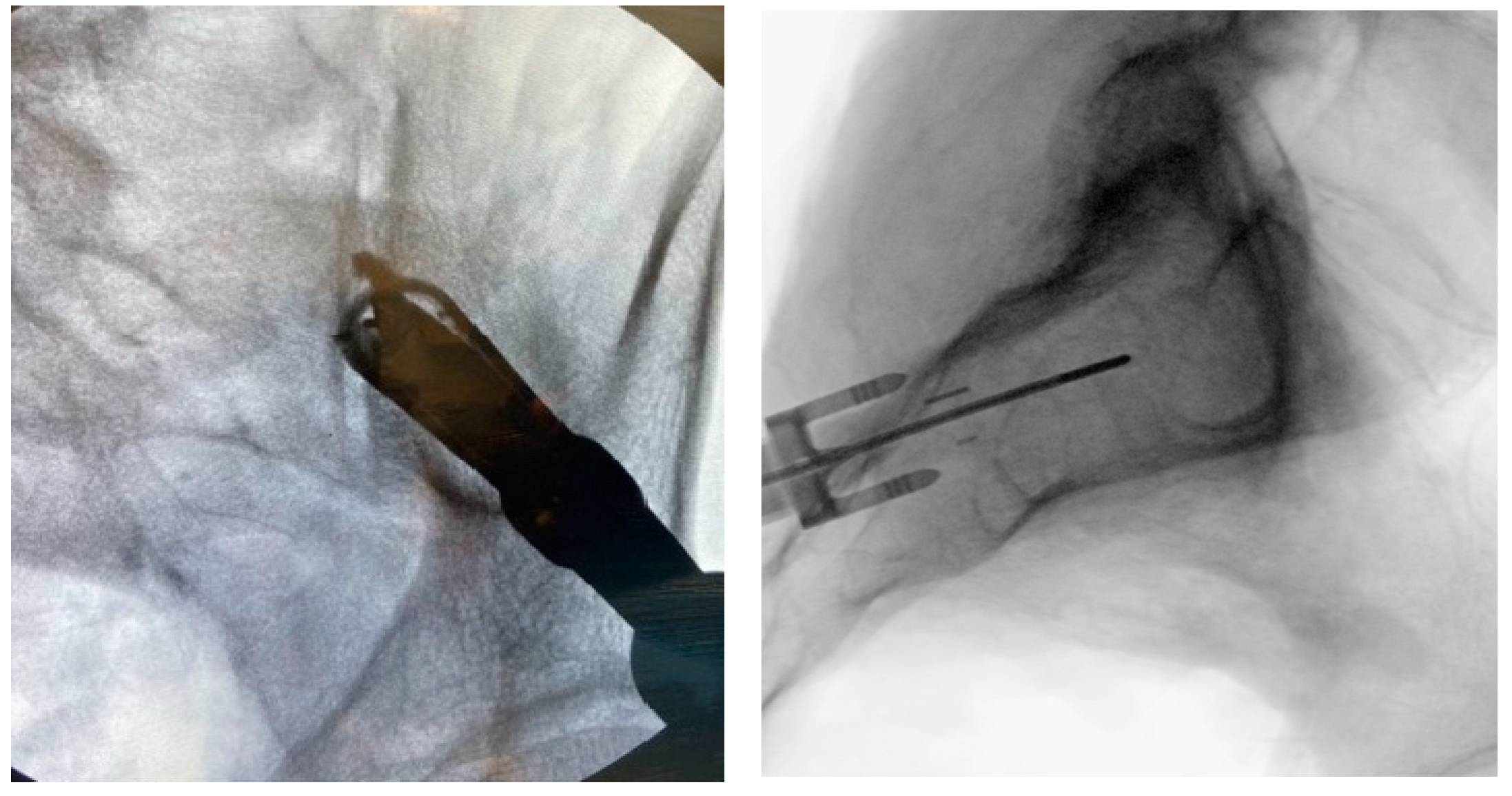
3.3.7. Docking Washer Introduction
3.3.8. Implant Insertion
3.3.9. Final Implant Placement
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ou-Yang, D.C.; York, P.J.; Kleck, C.J.; Patel, V.V. Diagnosis and Management of Sacroiliac Joint Dysfunction. J. Bone Joint Surg. Am. 2017, 99, 2027–2036. [Google Scholar] [CrossRef] [PubMed]
- Schwarzer, A.C.; Aprill, C.N.; Bogduk, N. The sacroiliac joint in chronic low back pain. Spine 1995, 20, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Vleeming, A.; Schuenke, M.D.; Masi, A.T.; Carreiro, J.E.; Danneels, L.; Willard, F.H. The sacroiliac joint: An overview of its anatomy, function and potential clinical implications. J. Anat. 2012, 221, 537–567. [Google Scholar] [CrossRef] [PubMed]
- DePalma, M.J.; Ketchum, J.M.; Saullo, T.R. Etiology of chronic low back pain in patients having undergone lumbar fusion. Pain Med. 2011, 12, 732–739. [Google Scholar] [CrossRef] [PubMed]
- Liliang, P.C.; Lu, K.; Liang, C.L.; Tsai, Y.D.; Wang, K.W.; Chen, H.J. Sacroiliac joint pain after lumbar and lumbosacral fusion: Findings using dual sacroiliac joint blocks. Pain Med. 2011, 12, 565–570. [Google Scholar] [CrossRef] [PubMed]
- Maigne, J.Y.; Planchon, C.A. Sacroiliac joint pain after lumbar fusion. A study with anesthetic blocks. Eur. Spine J. 2005, 14, 654–658. [Google Scholar] [CrossRef] [PubMed]
- Martin, C.T.; Haase, L.; Lender, P.A.; Polly, D.W. Minimally Invasive Sacroiliac Joint Fusion: The Current Evidence. Int. J. Spine Surg. 2020, 14, 20–29. [Google Scholar] [CrossRef] [PubMed]
- Belanger, T.A.; Dall, B.E. Sacroiliac arthrodesis using a posterior midline fascial splitting approach and pedicle screw instrumentation: A new technique. J. Spinal Disord. 2001, 14, 118–124. [Google Scholar] [CrossRef] [PubMed]
- Kaye, A.D.; Edinoff, A.N.; Scoon, L.; Youn, S.; Farrell, K.J.; Kaye, A.J.; Shah, R.J.; Cornett, E.M.; Chami, A.A.; Dixon, B.M.; et al. Novel Interventional Techniques for Chronic Pain with Minimally Invasive Arthrodesis of the Sacroiliac Joint: (INSITE, iFuse, Tricor, Rialto, and others). Rheumatol. Ther. 2021, 8, 1061–1072. [Google Scholar] [CrossRef] [PubMed]
- Wise, C.L.; Dall, B.E. Minimally invasive sacroiliac arthrodesis: Outcomes of a new technique. J. Spinal Disord. Tech. 2008, 21, 579–584. [Google Scholar] [CrossRef] [PubMed]
- Cross, W.W.; Delbridge, A.; Hales, D.; Fielding, L.C. Minimally Invasive Sacroiliac Joint Fusion: 2-Year Radiographic and Clinical Outcomes with a Principles-Based SIJ Fusion System. Open Orthop. J. 2018, 12, 7–16. [Google Scholar] [CrossRef] [PubMed]
- Rahl, M.D.; Weistroffer, J.; Dall, B.E. Analysis of Complications in Sacroiliac Joint Fusions Using FDA 510(k) Cleared Devices. Clin. Spine Surg. 2022, 35, E363–E367. [Google Scholar] [CrossRef] [PubMed]
- Schoell, K.; Buser, Z.; Jakoi, A.; Pham, M.; Patel, N.N.; Hsieh, P.C.; Liu, J.C.; Wang, J.C. Postoperative complications in patients undergoing minimally invasive sacroiliac fusion. Spine J. 2016, 16, 1324–1332. [Google Scholar] [CrossRef] [PubMed]
- Shamrock, A.G.; Patel, A.; Alam, M.; Shamrock, K.H.; Al Maaieh, M. The Safety Profile of Percutaneous Minimally Invasive Sacroiliac Joint Fusion. Glob. Spine J. 2019, 9, 874–880. [Google Scholar] [CrossRef] [PubMed]
- Lynch, P.J.; Tubic, G.; Foster, J.M.; Puri, S.; Burnette, C.A.; Block, J.E. Minimally Invasive Inferior Intra-Articular Sacroiliac Joint Fusion: Successful Application of Osseous Stabilization Using Allograft Bone. Orthop. Res. Rev. 2022, 14, 429–435. [Google Scholar] [CrossRef] [PubMed]
- Kiapour, A.; Joukar, A.; Elgafy, H.; Erbulut, D.U.; Agarwal, A.K.; Goel, V.K. Biomechanics of the Sacroiliac Joint: Anatomy, Function, Biomechanics, Sexual Dimorphism, and Causes of Pain. Int. J. Spine Surg. 2020, 14, 3–13. [Google Scholar] [CrossRef] [PubMed]
- DonTigny, R.L. Function and pathomechanics of the sacroiliac joint. A review. Phys. Ther. 1985, 65, 35–44. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.W.; Patterson, D.G.; Sayed, D. Review of Current Evidence for Minimally Invasive Posterior Sacroiliac Joint Fusion. Int. J. Spine Surg. 2021, 15, 514–524. [Google Scholar] [CrossRef] [PubMed]




Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Latif, U.; Hubbell, P.J., III; Tubic, G.; Guerrero, L.A.; Skaribas, I.M.; Block, J.E. Minimally Invasive Postero-Inferior Sacroiliac Joint Fusion: Surgical Technique and Procedural Details. J. Pers. Med. 2023, 13, 1136. https://doi.org/10.3390/jpm13071136
Latif U, Hubbell PJ III, Tubic G, Guerrero LA, Skaribas IM, Block JE. Minimally Invasive Postero-Inferior Sacroiliac Joint Fusion: Surgical Technique and Procedural Details. Journal of Personalized Medicine. 2023; 13(7):1136. https://doi.org/10.3390/jpm13071136
Chicago/Turabian StyleLatif, Usman, Paul J. Hubbell, III, Goran Tubic, Luis A. Guerrero, Ioannis M. Skaribas, and Jon E. Block. 2023. "Minimally Invasive Postero-Inferior Sacroiliac Joint Fusion: Surgical Technique and Procedural Details" Journal of Personalized Medicine 13, no. 7: 1136. https://doi.org/10.3390/jpm13071136
APA StyleLatif, U., Hubbell, P. J., III, Tubic, G., Guerrero, L. A., Skaribas, I. M., & Block, J. E. (2023). Minimally Invasive Postero-Inferior Sacroiliac Joint Fusion: Surgical Technique and Procedural Details. Journal of Personalized Medicine, 13(7), 1136. https://doi.org/10.3390/jpm13071136






