Reliability and Validity of Emotrics in the Assessment of Facial Palsy
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
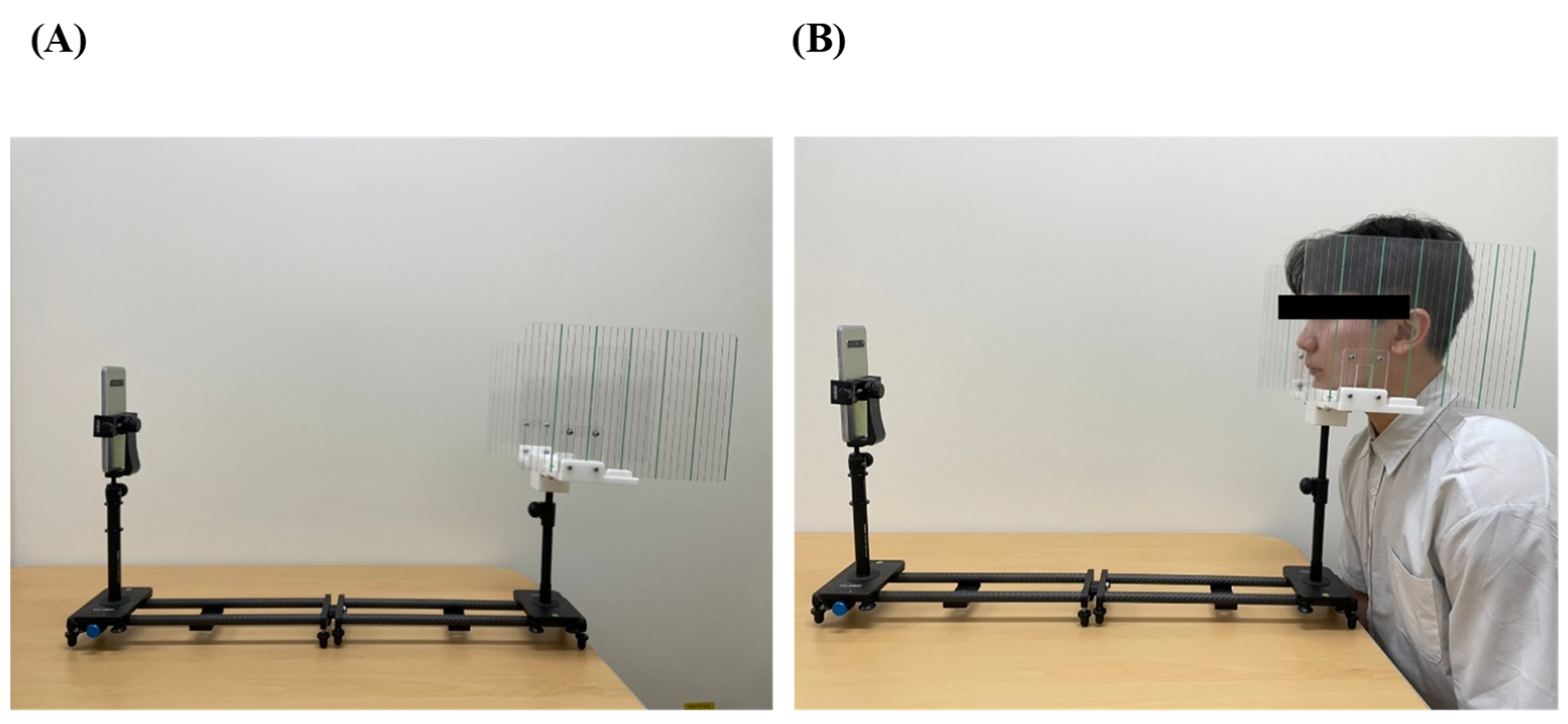
2.2. Interventions
- Distance is fixed (70 cm).
- Do not rotate the head (tilt is acceptable).
- Clean the forehead.
- Perform facial hair removal prior to the evaluation.
- Place the face in the middle of the photograph.
- Camera should be placed parallel to the face.
2.3. Baseline Characteristics
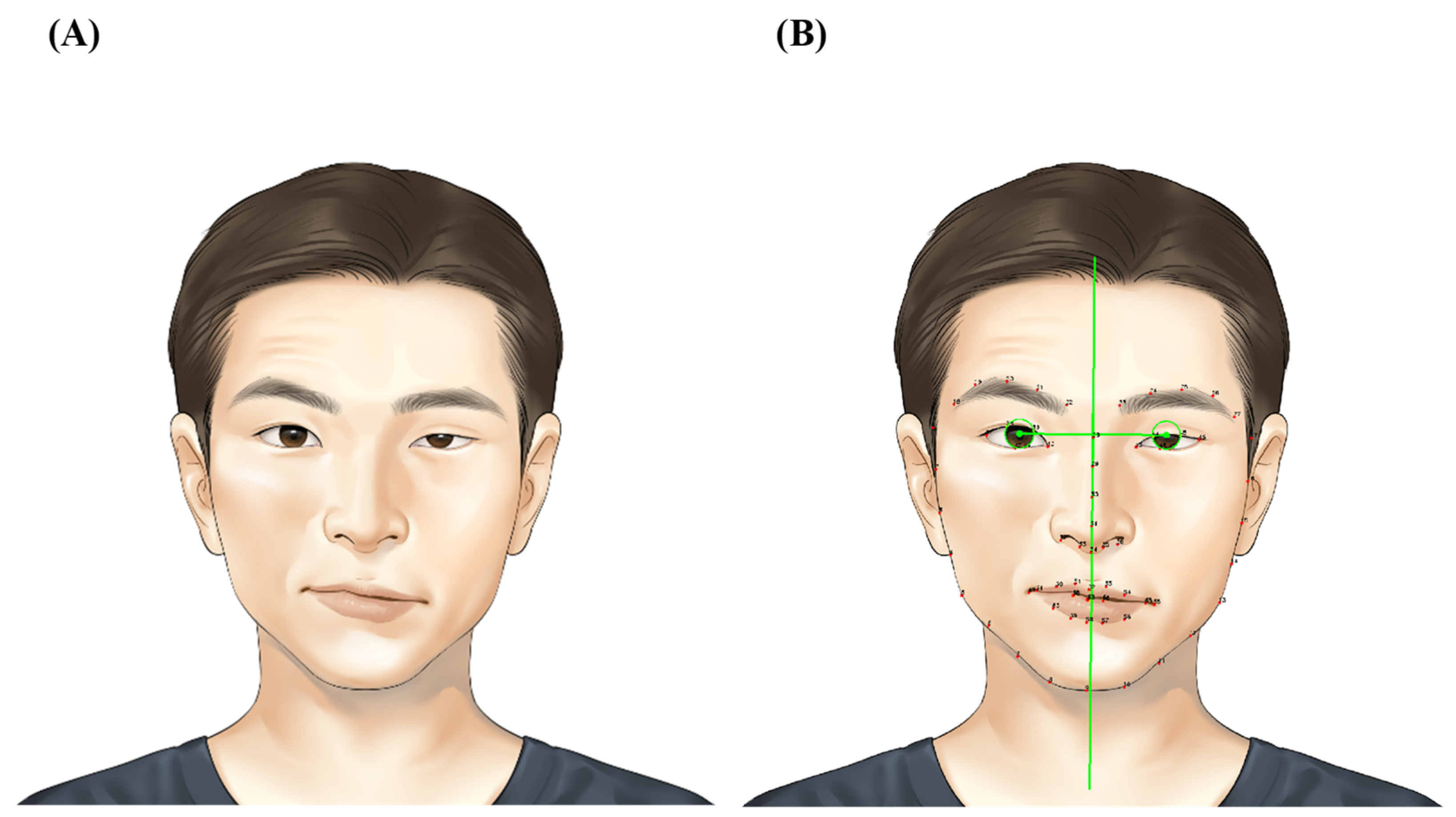
2.4. Emotrics Parameters
2.5. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Facial Palsy Parameters
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Robinson, M.W.; Baiungo, J. Facial Rehabilitation: Evaluation and Treatment Strategies for the Patient with Facial Palsy. Otolaryngol. Clin. N. Am. 2018, 51, 1151–1167. [Google Scholar] [CrossRef] [PubMed]
- Demeco, A.; Marotta, N.; Moggio, L.; Pino, I.; Marinaro, C.; Barletta, M.; Petraroli, A.; Palumbo, A.; Ammendolia, A. Quantitative analysis of movements in facial nerve palsy with surface electromyography and kinematic analysis. J. Electromyogr. Kinesiol. 2021, 56, 102485. [Google Scholar] [CrossRef] [PubMed]
- Bhama, P.; Bhrany, A.D. Ocular protection in facial paralysis. Curr. Opin. Otolaryngol. Head Neck Surg. 2013, 21, 353–357. [Google Scholar] [CrossRef] [PubMed]
- Saleem, F.; Munakomi, S. Pseudobulbar Palsy; StatPearls: St. Petersburg, FL, USA, 2022. [Google Scholar]
- Coulson, S.E.; Croxson, G.R.; Adams, R.D.; O’Dwyer, N.J. Reliability of the “Sydney,” “Sunnybrook,” and “House Brackmann” facial grading systems to assess voluntary movement and synkinesis after facial nerve paralysis. Otolaryngol. Head Neck Surg. 2005, 132, 543–549. [Google Scholar] [CrossRef] [PubMed]
- Dusseldorp, J.R.; Van Veen, M.M.; Mohan, S.; Hadlock, T.A. Outcome Tracking in Facial Palsy. Otolaryngol. Clin. N. Am. 2018, 51, 1033–1050. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez Colon, R.; Park, J.J.; Boczar, D.; Diep, G.K.; Berman, Z.P.; Trilles, J.; Chaya, B.F.; Rodriguez, E.D. Evaluating Functional Outcomes in Reanimation Surgery for Chronic Facial Paralysis: A Systematic Review. Plast. Reconstr. Surg. Glob. Open 2021, 9, e3492. [Google Scholar] [CrossRef] [PubMed]
- Azuma, T.; Fuchigami, T.; Nakamura, K.; Kondo, E.; Sato, G.; Kitamura, Y.; Takeda, N. New method to evaluate sequelae of static facial asymmetry in patients with facial palsy using three-dimensional scanning analysis. Auris Nasus Larynx 2022, 49, 755–761. [Google Scholar] [CrossRef] [PubMed]
- Greene, J.J.; Tavares, J.; Guarin, D.L.; Hadlock, T. Clinician and Automated Assessments of Facial Function Following Eyelid Weight Placement. JAMA Facial Plast. Surg. 2019, 21, 387–392. [Google Scholar] [CrossRef] [PubMed]
- Banks, C.A.; Bhama, P.K.; Park, J.; Hadlock, C.R.; Hadlock, T.A. Clinician-Graded Electronic Facial Paralysis Assessment: The eFACE. Plast Reconstr Surg. 2015, 136, 223e–230e. [Google Scholar] [CrossRef] [PubMed]
- Guarin, D.L.; Dusseldorp, J.; Hadlock, T.A.; Jowett, N. A Machine Learning Approach for Automated Facial Measurements in Facial Palsy. JAMA Facial Plast. Surg. 2018, 20, 335–337. [Google Scholar] [CrossRef] [PubMed]
- De Stefani, E.; Barbot, A.; Zannoni, C.; Belluardo, M.; Bertolini, C.; Cosoli, R.; Bianchi, B.; Ferri, A.; Zito, F.; Bergonzani, M.; et al. Post-surgery Rehabilitative Intervention Based on Imitation Therapy and Mouth-Hand Motor Synergies Provides Better Outcomes in Smile Production in Children and Adults with Long Term Facial Paralysis. Front. Neurol. 2022, 13, 757523. [Google Scholar] [CrossRef] [PubMed]
- Koo, W.Y.; Park, S.O.; Ahn, H.C.; Ryu, S.R. Facial reanimation using the hypoglossal nerve and ansa cervicalis: A short-term retrospective analysis of surgical outcomes. Arch. Craniofac. Surg. 2021, 22, 303–309. [Google Scholar] [CrossRef] [PubMed]
- Tzafetta, K.; Ruston, J.C.; Pinto-Lopes, R.; Mabvuure, N.T. Lower Lip Reanimation: Experience Using the Anterior Belly of Digastric Muscle in 2-stage Procedure. Plast. Reconstr. Surg. Glob. Open 2021, 9, e3461. [Google Scholar] [CrossRef] [PubMed]
- Banks, C.A.; Jowett, N.; Hadlock, T.A. Test-Retest Reliability and Agreement between In-Person and Video Assessment of Facial Mimetic Function Using the eFACE Facial Grading System. JAMA Facial Plast. Surg. 2017, 19, 206–211. [Google Scholar] [CrossRef] [PubMed]
- Blumenfeld, H. Neuroanatomy through Clinical Cases with ebook; Sinauer: Sunderland, MA, USA, 2011; p. 517. [Google Scholar]
- Kim, D.; Park, J.; Jung, J.; Kim, T.; Paik, J. Lens distortion correction and enhancement based on local self-similarity for high-quality consumer imaging systems. IEEE Trans. Consum. Electron. 2014, 60, 18–22. [Google Scholar] [CrossRef]
- Guarin, D.L.; Yunusova, Y.; Taati, B.; Dusseldorp, J.R.; Mohan, S.; Tavares, J.; van Veen, M.M.; Fortier, E.; Hadlock, T.A.; Jowett, N. Toward an Automatic System for Computer-Aided Assessment in Facial Palsy. Facial Plast. Surg. Aesthet. Med. 2020, 22, 42–49. [Google Scholar] [CrossRef]
- Dusseldorp, J.R.; Guarin, D.L.; van Veen, M.M.; Jowett, N.; Hadlock, T.A. In the Eye of the Beholder: Changes in Perceived Emotion Expression after Smile Reanimation. Plast. Reconstr. Surg. 2019, 144, 457–471. [Google Scholar] [CrossRef]
| Characteristics | Total Patients (n = 23) |
|---|---|
| Age, years | 49.4 ± 17.9 |
| Sex | |
| Female | 11/23 (47.8%) |
| Male | 12/23 (52.2%) |
| Facial-palsy-related feature | |
| Laterality | |
| Right | 12/23 (52.2%) |
| Left | 11/23 (47.8%) |
| Type | |
| Central type | 9/23 (39.1%) |
| Peripheral type | 14/23 (60.9%) |
| Etiology | |
| Bell’s palsy | 4/23 (17.4%) |
| Cerebrovascular accident | 6/23 (26.1%) |
| Brain tumor | 10/23 (43.5%) |
| Trauma | 2/23 (8.7%) |
| Unidentified | 1/23 (4.3%) |
| House–Brackmann facial palsy scale | |
| Eye | |
| 1 | 10/23 (43.5%) |
| 2 | 4/23 (17.4%) |
| 3 | 1/23 (4.3%) |
| 4 | 4/23 (17.4%) |
| 5 | 3/23 (13.0%) |
| 6 | 1/23 (4.3%) |
| Mouth | |
| 2 | 3/23 (13.0%) |
| 4 | 10/23 (43.5%) |
| 5 | 10/23 (43.5%) |
| Characteristics | Interrater Reliability | Intrarater Reliability | Intrasubject Reliability |
|---|---|---|---|
| BH_A-U | 0.99 CI (0.98, 0.99) * | 0.97 CI (0.94, 0.99) * | 0.76 CI (0.41, 0.90) * |
| BH_r-c | 0.61 CI (0.02, 0.84) * | 0.95 CI (0.88, 0.98) * | −0.82 CI (−3.48, 0.26) |
| PF_A-U | 0.92 CI (0.80, 0.97) * | 0.92 CI (0.81, 0.97) * | 0.73 CI (0.33, 0.89) * |
| PF_r-c | 0.82 CI (0.57, 0.93) * | 0.82 CI (0.56, 0.93) * | 0.55 CI (−0.12, 0.82) |
| CE_A-U | 0.99 CI (0.97, 0.99) * | 0.93 CI (0.82, 0.97) * | 0.88 CI (0.69, 0.95) * |
| CE_r-s | 0.89 CI (0.74, 0.96) * | 0.85 CI (0.64, 0.94) * | 0.69 CI (0.24, 0.87) * |
| SA_A-U | 0.96 CI (0.91, 0.98) * | 0.96 CI (0.90, 0.98) * | 0.78 CI (0.45, 0.91) * |
| SA_r-s | 0.86 CI (0.65, 0.94) * | 0.80 CI (0.51, 0.92) * | 0.68 CI (0.21, 0.87) * |
| DS_A-U | 0.99 CI (0.97, 0.99) * | 0.97 CI (0.92, 0.99) * | −0.37 CI (−3.10, 0.54) |
| DS_r-s | 0.98 CI (0.96, 0.99) * | 0.96 CI (0.90, 0.98) * | −0.17 CI (−2.48, 0.61) |
| Characteristics | Correlation Coefficient with HB_E * | Correlation Coefficient with HB_M * | p-Value |
|---|---|---|---|
| BH_A-U | −0.07 | - | 0.75 |
| BH_r-c | 0.81 | - | <0.01 |
| PF_A-U | 0.28 | - | 0.22 |
| PF_r-c | −0.64 | - | <0.01 |
| CE_A-U | - | −0.26 | 0.25 |
| CE_r-s | - | −0.10 | 0.66 |
| SA_A-U | - | −0.18 | 0.44 |
| SA_r-s | - | −0.20 | 0.39 |
| DS_A-U | - | −0.40 | 0.11 |
| DS_r-s | - | 0.10 | 0.71 |
| Characteristics | Correlation Coefficient with HB_E * (n = 14) | Correlation Coefficient with HB_M * (n = 14) | p-Value |
|---|---|---|---|
| BH_A-U | −0.17 | - | 0.62 |
| BH_r-c | 0.92 | - | <0.01 |
| PF_A-U | 0.43 | - | 0.19 |
| PF_r-c | −0.77 | - | <0.01 |
| CE_A-U | - | −0.26 | 0.24 |
| CE_r-s | - | −0.17 | 0.62 |
| SA_A-U | - | −0.18 | 0.59 |
| SA_r-s | - | −0.50 | 0.12 |
| DS_A-U | - | −0.41 | 0.21 |
| DS_r-s | - | 0.32 | 0.34 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, M.G.; Bae, C.R.; Oh, T.S.; Park, S.J.; Jeong, J.M.; Kim, D.Y. Reliability and Validity of Emotrics in the Assessment of Facial Palsy. J. Pers. Med. 2023, 13, 1135. https://doi.org/10.3390/jpm13071135
Kim MG, Bae CR, Oh TS, Park SJ, Jeong JM, Kim DY. Reliability and Validity of Emotrics in the Assessment of Facial Palsy. Journal of Personalized Medicine. 2023; 13(7):1135. https://doi.org/10.3390/jpm13071135
Chicago/Turabian StyleKim, Min Gi, Cho Rong Bae, Tae Suk Oh, Sung Jong Park, Jae Mok Jeong, and Dae Yul Kim. 2023. "Reliability and Validity of Emotrics in the Assessment of Facial Palsy" Journal of Personalized Medicine 13, no. 7: 1135. https://doi.org/10.3390/jpm13071135
APA StyleKim, M. G., Bae, C. R., Oh, T. S., Park, S. J., Jeong, J. M., & Kim, D. Y. (2023). Reliability and Validity of Emotrics in the Assessment of Facial Palsy. Journal of Personalized Medicine, 13(7), 1135. https://doi.org/10.3390/jpm13071135






