RA.DI.CA. Splint Therapy in the Management of Temporomandibular Joint Displacement without Reduction
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Sampling
2.2. Treatments and Protocols
- An upper plate made with heat-cured acrylic resin (1),
- A lower plate made with heat-cured acrylic resin (2),
- An anterior hinge (3),
- A total of vestibular springs obtained by an orthodontic wire (4),
- A minimum of 2 Adams clasps with/without 2 ball clasps (5), and
- A steel arch at the level of the vestibular side (6).
2.3. Study Phases
- T0 = recruitment period
- T1 = 4 weeks from the start of therapy
- T2 = 6-month follow-up
2.4. Study Variables
- Demographic independent variables: gender, age, marital status, and job.
- Occlusal and dental variables: occlusal and skeletal class, teeth formula, occlusal alterations, incisal guide, teeth loss, and parafunctions. These parameters were collected based on the clinical examination and standard lateral radiograph and dental orthopantomography.
- Medical history, including trauma, TMJ clicking, and correlated symptoms.
- Pain characterization: TMJ-related pain including arthralgia and muscle pain, headache, familiar related pain, neck pain, and emotional stress, following a verbal numeric scale (VNS) classification conducted with the patients at all follow-up timepoints.
- Functional variables: maximum mouth opening and lateral excursions in mm, with measurements taken with the patients at all follow-up timepoints.
- Days necessary for the closed lock and degree of symptom resolution.
- Residual clicking after the treatment and occlusal change perception of the patients.
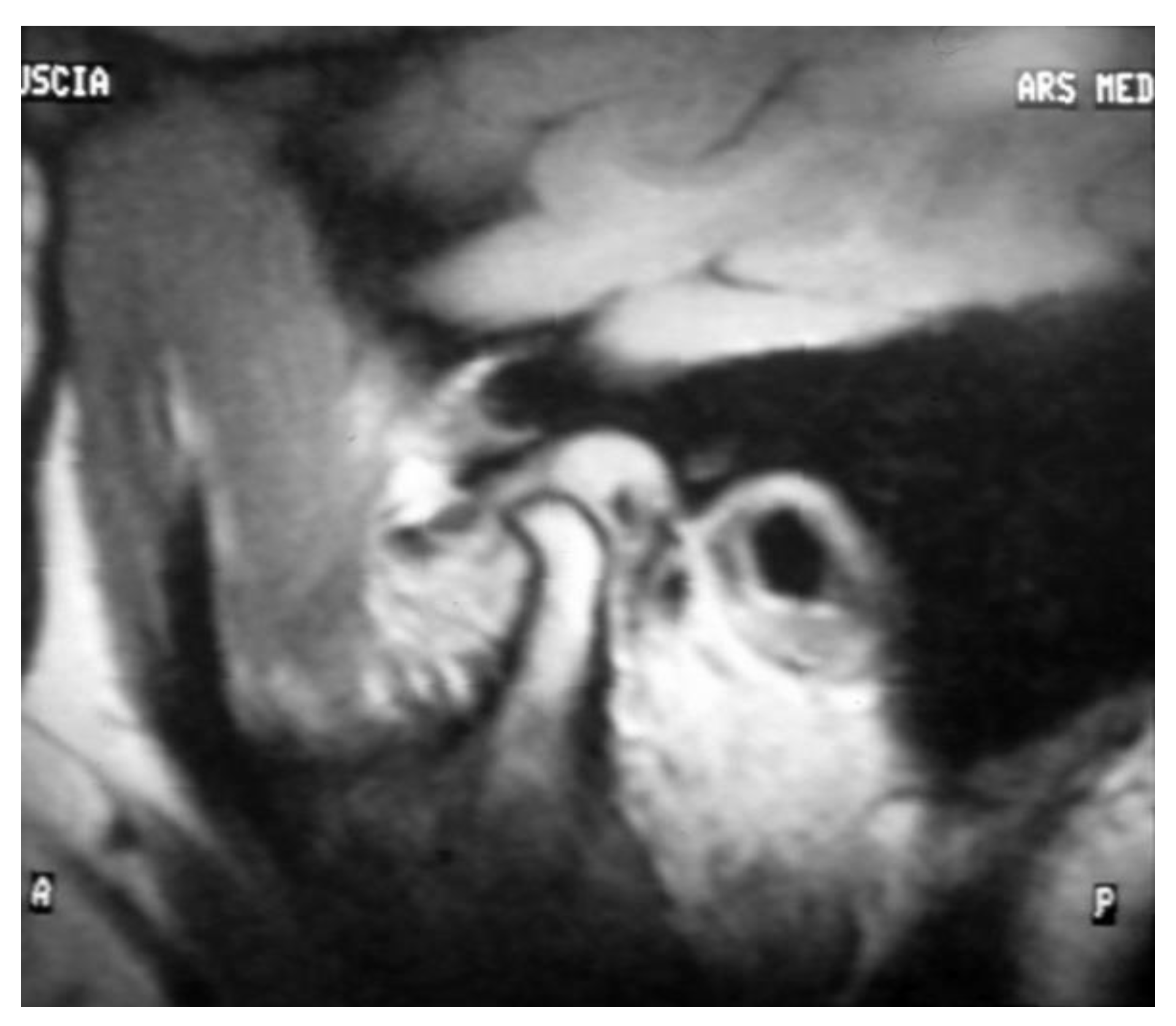
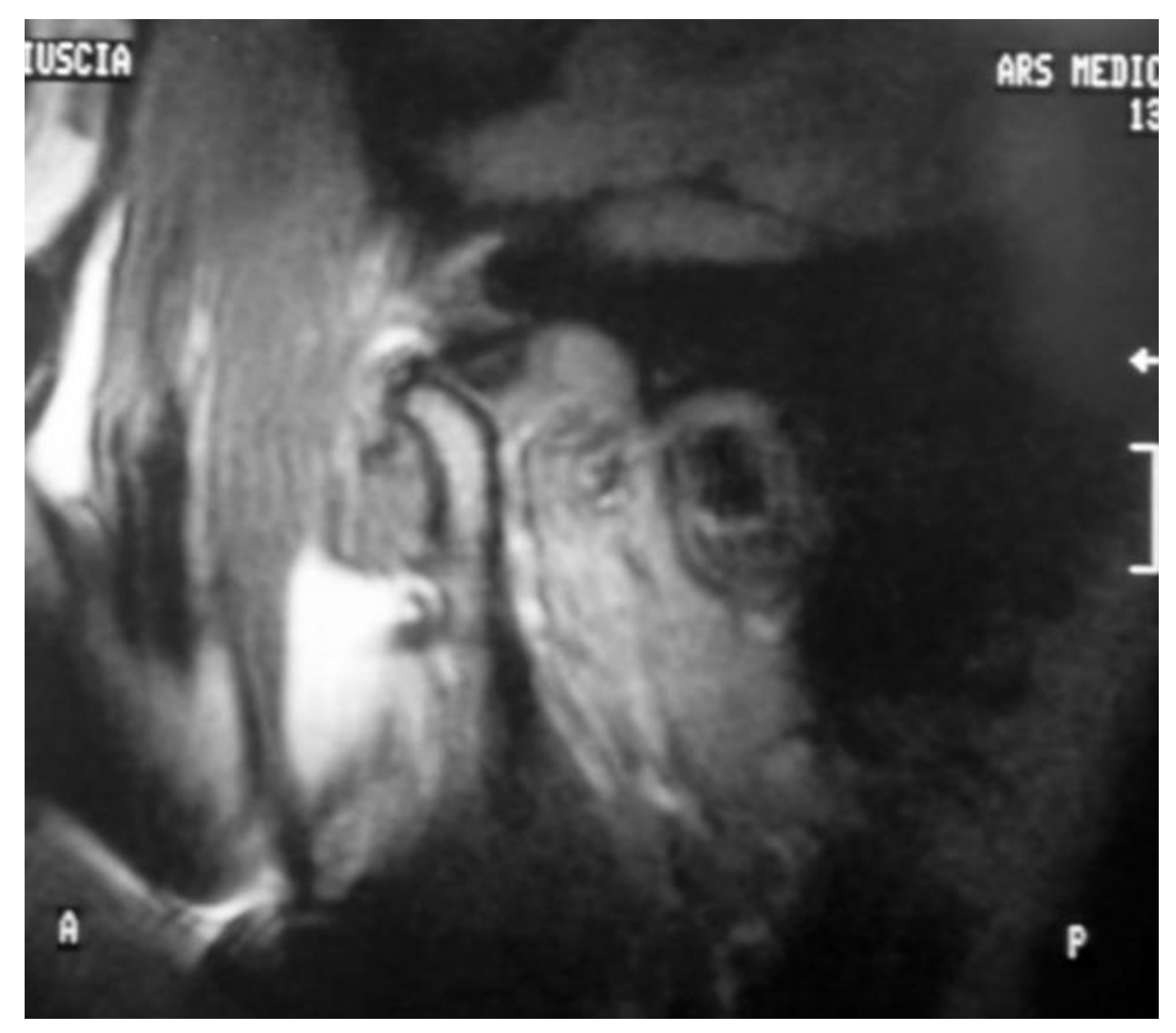
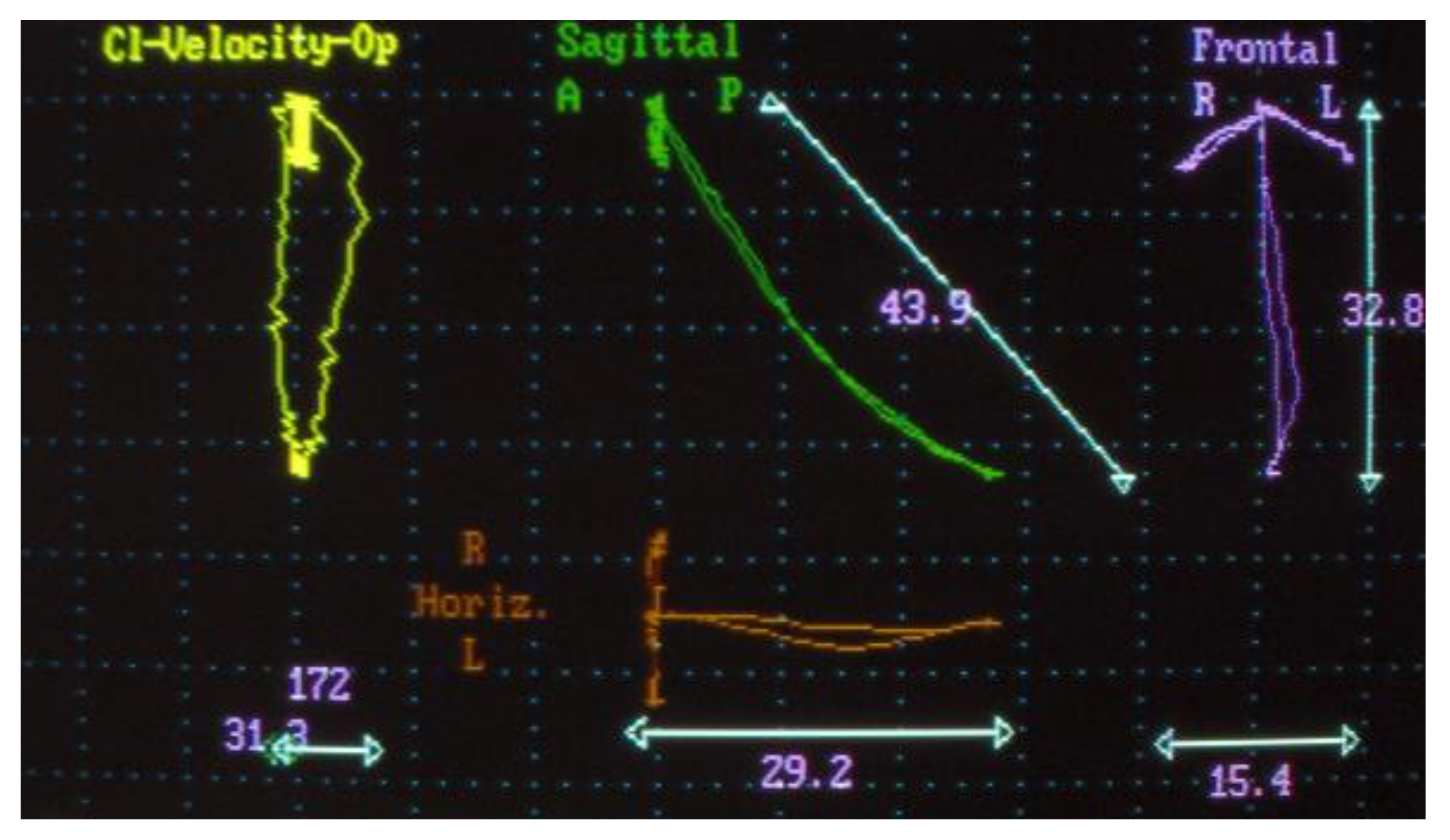
- Electrognathographic parameters. Movement trajectory for opening, closing, and masticatory cycle with elastic hard bolus (Figure 4 and Figure 5). All patients underwent mandibular functional evaluation using the electrognathograph (BioEMG, BioResearch, Inc., Milwaukee, WI, USA) according to our protocol, which included:
- Slow mandibular opening and closing movements starting from the position of maximum intercuspidation.
- Right and left lateral movements starting from the maximum occlusion.
- Chewing for about 1 min of the elastic hard bolus.
2.5. Clinical Calibration
2.6. Statistical Analysis
3. Results
3.1. Descriptive Statistics
3.2. Inferential Statistics
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dowrkin, S.F. Research Diagnostic Criteria for Temporomandibular Disorders: Review, Criteria, Examinations and Specifications, Critique. J. Craniomandib. Disord. 1992, 6, 301–355. [Google Scholar]
- D’Attilio, M.; Scarano, A.; Quaranta, A.; Festa, F.; Caputi, S.; Piattelli, A. Modification of Condyle Anatomy Following a Monolateral Bite Rise: A Histological Study in Rat. Int. J. Immunopathol. Pharm. 2007, 20, 43–47. [Google Scholar] [CrossRef] [PubMed]
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.-P.; List, T.; Svensson, P.; Gonzalez, Y.; Lobbezoo, F.; et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: Recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group. J. Oral. Facial Pain Headache 2014, 28, 6–27. [Google Scholar] [CrossRef] [PubMed]
- Falisi, G.; Gatto, R.; Di Paolo, C.; De Biase, A.; Franceschini, C.; Monaco, A.; Rastelli, S.; Botticelli, G. A Female Psoriatic Arthritis Patient Involving the TMJ. Case Rep. Dent. 2021, 2021, 1–6. [Google Scholar] [CrossRef]
- Miernik, M.; Więckiewicz, W. The Basic Conservative Treatment of TMJ Anterior Disc Displacement Without Reduction—Review. Adv. Clin. Exp. Med. 2015, 24, 731–735. [Google Scholar] [CrossRef]
- Macrì, M.; Murmura, G.; Scarano, A.; Festa, F. Prevalence of Temporomandibular Disorders and Its Association with Malocclusion in Children: A Transversal Study. Front. Public Health 2022, 10, 860833. [Google Scholar] [CrossRef]
- Cascone, P.; Di Paolo, C. Patologia Della Articolazione Temporomandibolare: Dall’eziopatogenesi Alla Terapia; UTET Scienze Mediche: Torino, Italy, 2004. [Google Scholar]
- Rudisch, A.; Innerhorfer, K.; Bertram, S.; Emshoff, R. Magnetic resonance imaging findings of internal derangement and effusion in patients with unilateral temporomandibular joint pain. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2001, 92, 566–571. [Google Scholar] [CrossRef]
- Aoyama, S.; Kino, K.; Amagasa, T.; Sakamoto, I.; Omura, K.; Honda, E.; Kobayashi, K.; Igarashi, C.; Yoda, T. Clinical and magnetic resonance imaging study of unilateral sideways displacements of temporomandibular joint. J. Med. Dent. Sci. 2002, 49, 89–94. [Google Scholar]
- Taskaya-Yilmaz, N.; Ogutcen-Toller, M. Magnetic resonance imaging evaluation of temporomandibular joint disc deformities in relation to type of disc displacement. J. Oral Maxillofac. Surg. 2001, 59, 860–865. [Google Scholar] [CrossRef]
- Tasaki, M.M.; Westesson, P.L.; Kurita, K.; Mohl, N. Magnetic resonance imaging of the temporomandibular joint. Value of axial images. Oral Surg. Oral Med. Oral Pathol. 1993, 75, 528–531. [Google Scholar] [CrossRef]
- Emshoff, R.; Brandlmaier, I.; Bertram, S.; Rudisch, A. Relative odds of temporomandibular joint pain as a function of magnetic resonance imaging findings of internal derangement, osteoarthrosis, effusion, and bone marrow edema. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2003, 95, 437–445. [Google Scholar] [CrossRef] [PubMed]
- Emshoff, R.; Puffer, P.; Rudisch, A.; Gassner, R. Temporomandibular joint pain: Relationship to internal derangement type, osteoarthrosis, and synovial fluid mediator level of tumor necrosis factor-alpha. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2000, 90, 442–449. [Google Scholar] [CrossRef] [PubMed]
- Sano, T. Recent developments in understanding temporomandibular joint disorders. Part 2: Changes in the retrodiscal tissue. Dentomaxillofac Radiol. 2000, 29, 260–263. [Google Scholar] [CrossRef] [PubMed]
- Sano, T.; Westesson, P.L.; Larheim, T.A.; Takagi, R. The association of temporomandibular joint pain with abnormal bone marrow in the mandibular condyle. J. Oral Maxillofac. Surg. 2000, 58, 254–257. [Google Scholar] [CrossRef] [PubMed]
- Senga, K.; Mizutani, H.; Kobayashi, M.; Ueda, M. Ultrastructural study on adhesions in internal derangement of the temporomandibular joint. J. Oral Maxillofac. Surg. 1999, 57, 165–170. [Google Scholar] [CrossRef]
- Fernandes Pinheiro, P.; Andrade Da Cunha, D.; Genuíno Dourado Filho, M.; Salvetti Cavalcanti Caldas, A.; Myriam Aragão Melo, T.; Justino Da Silva, H. The Use of Electrognathography in Jaw Movement Research: A Literature Review. CRANIO® 2012, 30, 293–303. [Google Scholar] [CrossRef]
- Schmitter, M.; Zahran, M.; Duc, J.-M.P.; Henschel, V.; Rammelsberg, P. Conservative Therapy in Patients With Anterior Disc Displacement Without Reduction Using 2 Common Splints: A Randomized Clinical Trial. J. Oral Maxillofac. Surg. 2005, 63, 1295–1303. [Google Scholar] [CrossRef]
- Ohnuki, T.; Fukuda, M.; Nakata, A.; Nagai, H.; Takahashi, T.; Sasano, T.; Miyamoto, Y. Evaluation of the Position, Mobility, and Morphology of the Disc by MRI before and after Four Different Treatments for Temporomandibular Joint Disorders. Dentomaxillofac. Radiol. 2006, 35, 103–109. [Google Scholar] [CrossRef]
- Stiesch-Scholz, M.; Kempert, J.; Wolter, S.; Tschernitschek, H.; Rossbach, A. Comparative Prospective Study on Splint Therapy of Anterior Disc Displacement without Reduction. J. Oral Rehabil. 2005, 32, 474–479. [Google Scholar] [CrossRef]
- Di Paolo, C.; Falisi, G.; Panti, F.; Di Giacomo, P.; Rampello, A. “RA.DI.CA.” Splint for the Management of the Mandibular Functional Limitation: A Retrospective Study on Patients with Anterior Disc Displacement without Reduction. Int. J. Environ. Res. Public Health 2020, 17, 9057. [Google Scholar] [CrossRef]
- Di Giacomo, P.; Di Paolo, C.; Qorri, E.; Gatto, R.; Manes Gravina, G.; Falisi, G. Conservative Therapies for TMJ Closed Lock: A Randomized Controlled Trial. J. Clin. Med. 2022, 11, 7037. [Google Scholar] [CrossRef]
- Birkett, M.A.; Day, S.J. Internal Pilot Studies for Estimating Sample Size. Stat. Med. 1994, 13, 2455–2463. [Google Scholar] [CrossRef]
- Drace, J.E.; Enzmann, D.R. Defining the normal temporomandibular joint: Closed-, partially open-, and open-mouth MR imaging of asymptomatic subjects. Radiology 1990, 177, 67–71. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, M.; Hollender, L.; Anderson, Q.; Kartha, K.; Ohrbach, R.K.; Truelove, E.L.; John, M.T.; Schiffman, E.L. Research Diagnostic Criteria for Temporomandibular Disorders (RDC/ TMD): Development of image analysis crite- ria and examiner reliability for image analysis. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2009, 107, 844–860. [Google Scholar] [CrossRef] [PubMed]
- Sato, S.; Sakamoto, M.; Kawamura, H.; Motegi, K. Long-term changes in clinical signs and symptoms and disc position and morphology in patients with nonreducing disc displacement in the temporomandibular joint. J. Oral Maxillofac. Surg. 1999, 57, 23–29. [Google Scholar] [CrossRef]
- Fernandes, G.; Franco, A.L.; Goncalves, D.A.; Speciali, J.G.; Bigal, M.E.; Camparis, C.M. Temporomandibular disorders, sleep bruxism, and primary headaches are mutually associated. J. Orofac. Pain 2013, 27, 14–20. [Google Scholar]
- Goncalves, D.A.; Camparis, C.M.; Speciali, J.G.; Franco, A.L.; Castanharo, S.M.; Bigal, M.E. Temporomandibular disorders are differentially associated with headache diagnoses: A controlled study. Clin. J. Pain 2011, 27, 611–615. [Google Scholar] [CrossRef] [PubMed]
- Costa, Y.M.; Conti, P.C.; de Faria, F.A.; Bonjardim, L.R. Temporomandibular disorders and painful comorbidities: Clinical association and underlying mechanisms. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2017, 123, 288–297. [Google Scholar] [CrossRef]
- van der Meer, H.A.; Visscher, C.M.; Engelbert, R.H.H.; Mulleners, W.M.; Nijhuis-van der Sanden, M.W.G.; Speksnijder, C.M. Development and psychometric validation of the headache screening questionnaire—Dutch Version. Musculoskelet. Sci. Pract. 2017, 31, 52–61. [Google Scholar] [CrossRef]
- Goncalves, D.A.G.; Camparis, C.M.; Speciali, J.G.; Castanharo, S.M.; Ujikawa, L.T.; Lipton, R.B.; Bigal, M.E. Treatment of comorbid migraine and temporomandibular disorders: A factorial, double-blind, randomized, placebo-controlled study. J. Orofac. Pain 2013, 27, 325–335. [Google Scholar] [CrossRef]
- Maluf, S.; Moreno, B.; Crivello, O.; Cabral, C.; Bortolotti, G.; Marques, A. Global postural reeducation and static stretching exercises in the treatment of myogenic temporomandibular disorders: A randomized study. J. Manip. Physiol. Ther. 2010, 33, 500–507. [Google Scholar] [CrossRef] [PubMed]
- von Piekartz, H.; Rösner, C.; Batz, A.; Hall, T.; Ballenberger, N. Bruxism, temporomandibular dysfunction and cervical impairments in females—Results from an observational study. Musculoskelet. Sci. Pract. 2020, 45, 102073. [Google Scholar] [CrossRef] [PubMed]




| Qualitative Evaluation | Quantitative | ||||
|---|---|---|---|---|---|
| Lateral or Medial Displacement/Anterior | Disc Deformity | Articular Effusion | Retrodiscal Tissues | Disc-Condyle Angle Theta | |
| Subject 1 | Antero-medial | no | Yes | none | 23° |
| Subject 2 | Antero-medial | no | Yes | none | 24° |
| Subject 3 | Anterior | no | Yes | none | 22° |
| Subject 4 | Anterior | no | no | none | 30° |
| Subject 5 | Anterior | yes | no | none | 25° |
| Subject 6 | Antero-medial | yes | Yes | none | 25° |
| Subject 7 | Anterior-medial | no | no | none | 20° |
| Subject 8 | Antero | yes | no | none | 35° |
| Subject 9 | Antero-medial | no | yes | none | 19° |
| Subject 10 | Antero-medial | yes | no | none | 30° |
| Clinical Parameter | T0 (Mean ± SD) | T1 (Mean ± SD) | T2 (Mean ± SD) |
|---|---|---|---|
| Arthralgia | 69.00 ± 17.28 | 39.33 ± 4.84 | 14.80 ± 3.72 |
| Headache | 83.00 ± 13.37 | 46.00 ± 3.69 | 14.66 ± 3.46 |
| Neck pain | 57.00 ± 24.51 | 37.33 ± 5.7 | 24.00 ± 5.08 |
| Maximum mouth opening | 30.40 ± 3.47 | 43.13 ± 0.84 | 44.66 ± 0.791 |
| Parameter | F | p-Value | Post-Hoc Test p Holm Value | ||
|---|---|---|---|---|---|
| T0→T1 | T0→T2 | T1→T2 | |||
| Arthralgia | 60,021 | <0.001 | <0.001 | <0.001 | <0.001 |
| Headache | 25,728 | <0.001 | 0.002 | <0.001 | 0.002 |
| Neck pain | 14,459 | <0.001 | 0.086 | <0.001 | 0.002 |
| Mouth opening | 55,471 | <0.001 | <0.001 | <0.001 | 0.179 |
| Qualitative Evaluation | Quantitative | ||||
|---|---|---|---|---|---|
| Lateral or Medial Displacement/Anterior | Disc Deformity | Articular Effusion | Retrodiscal Tissues | Disc-Condyle Angle Theta | |
| Subject 1 | Normal | no | no | None | −10° |
| Subject 2 | Normal | no | no | None | 8° |
| Subject 3 | Normal | no | no | None | 5° |
| Subject 4 | Anterior-medial | no | no | None | 30° |
| Subject 5 | Normal | yes | no | None | −10° |
| Subject 6 | Normal | yes | no | None | −6° |
| Subject 7 | Anterior-Medial | no | no | None | 20° |
| Subject 8 | Normal | yes | no | None | −11° |
| Subject 9 | Normal | no | no | None | 5° |
| Subject 10 | Anterior | yes | no | None | 30° |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Di Paolo, C.; Qorri, E.; Falisi, G.; Gatto, R.; Tari, S.R.; Scarano, A.; Rastelli, S.; Inchingolo, F.; Di Giacomo, P. RA.DI.CA. Splint Therapy in the Management of Temporomandibular Joint Displacement without Reduction. J. Pers. Med. 2023, 13, 1095. https://doi.org/10.3390/jpm13071095
Di Paolo C, Qorri E, Falisi G, Gatto R, Tari SR, Scarano A, Rastelli S, Inchingolo F, Di Giacomo P. RA.DI.CA. Splint Therapy in the Management of Temporomandibular Joint Displacement without Reduction. Journal of Personalized Medicine. 2023; 13(7):1095. https://doi.org/10.3390/jpm13071095
Chicago/Turabian StyleDi Paolo, Carlo, Erda Qorri, Giovanni Falisi, Roberto Gatto, Sergio Rexhep Tari, Antonio Scarano, Sofia Rastelli, Francesco Inchingolo, and Paola Di Giacomo. 2023. "RA.DI.CA. Splint Therapy in the Management of Temporomandibular Joint Displacement without Reduction" Journal of Personalized Medicine 13, no. 7: 1095. https://doi.org/10.3390/jpm13071095
APA StyleDi Paolo, C., Qorri, E., Falisi, G., Gatto, R., Tari, S. R., Scarano, A., Rastelli, S., Inchingolo, F., & Di Giacomo, P. (2023). RA.DI.CA. Splint Therapy in the Management of Temporomandibular Joint Displacement without Reduction. Journal of Personalized Medicine, 13(7), 1095. https://doi.org/10.3390/jpm13071095











