Abstract
Artificial intelligence (AI) applications have transformed healthcare. This study is based on a general literature review uncovering the role of AI in healthcare and focuses on the following key aspects: (i) medical imaging and diagnostics, (ii) virtual patient care, (iii) medical research and drug discovery, (iv) patient engagement and compliance, (v) rehabilitation, and (vi) other administrative applications. The impact of AI is observed in detecting clinical conditions in medical imaging and diagnostic services, controlling the outbreak of coronavirus disease 2019 (COVID-19) with early diagnosis, providing virtual patient care using AI-powered tools, managing electronic health records, augmenting patient engagement and compliance with the treatment plan, reducing the administrative workload of healthcare professionals (HCPs), discovering new drugs and vaccines, spotting medical prescription errors, extensive data storage and analysis, and technology-assisted rehabilitation. Nevertheless, this science pitch meets several technical, ethical, and social challenges, including privacy, safety, the right to decide and try, costs, information and consent, access, and efficacy, while integrating AI into healthcare. The governance of AI applications is crucial for patient safety and accountability and for raising HCPs’ belief in enhancing acceptance and boosting significant health consequences. Effective governance is a prerequisite to precisely address regulatory, ethical, and trust issues while advancing the acceptance and implementation of AI. Since COVID-19 hit the global health system, the concept of AI has created a revolution in healthcare, and such an uprising could be another step forward to meet future healthcare needs.
1. Introduction
Health systems worldwide are at a crossroads and face exponential healthcare cost developments that have far outpaced GDP growth rates to support health system sustainability [1]. This matter was very straightforward with the emergence of the 2019 coronavirus disease (COVID-19) pandemic and the Ukraine war. There is a combination of tight finances, elderly inhabitants, rising chronic diseases, and the strain on healthcare systems that previously struggled to cope with increased demand for service accessibility and availability. In addition, the COVID-19 pandemic is leading to health system failure in some countries, e.g., India, Brazil, and Indonesia [2].
As health systems depend on firm disease management pathways and evidence-based care tactics to meet needs and regulate practices according to industrial healthcare delivery services, the concept of “HRO” emphasizes a Highly Reliable Organization (HRO) by having its services managed by either an “accountable care organization (ACO)” or a “health maintenance organization (HMO)” [3]. However, the incidence of chronic diseases in the United States (USA) is steadily increasing, i.e., 60% of adults have one chronic disease, and 40% have more than two chronic diseases, totaling USD 3.3 trillion in annual healthcare costs [4]. In addition, this picture quickly changed with the emerging infectious disease, which was first reported in Wuhan, China, in 2019 and designated as COVID-19 by the World Health Organization on 11 February 2020 [5]. Since then, healthcare has been undergoing a digital transformation that will transform many of the fundamental building blocks of medical care [6]. This condition might be due to the massive pressure exerted by COVID-19 on global healthcare and the associated infrastructure, supply chain, and employees. The pandemic also forced healthcare stakeholders to adopt digital technologies [7,8]. Notably, key foundational changes occurred in the healthcare sector during the post-pandemic. For instance, current-generation customers (patients) showed active involvement in healthcare-associated decision making due to the increased acceptance of virtual healthcare systems and associated digital innovations [9]. However, protuberant challenges can occur, and the strategies to overcome them would create a way for the voyage to reach the upcoming healthcare era. Patients and their experiences and needs motivate innovations in the healthcare sector. Their main inclinations comprise the creation of digitally empowered physician–patient interactions, confirming the provision of patient-centric amenities across the globe [10]. The necessity for deploying advanced digital devices has become a requirement to offer augmented customer satisfaction, permitting tracking, checking the health status, and better drug adherence to be achieved [11]. Such aspects would be more beneficial during the post-hospitalization period using digital health platforms. At the same time, healthcare customers are cautious about sharing their confidential data; hence, healthcare organizations (HCOs) are in place to preserve the customer’s trust by representing transparency, empathy, and reliability in their services [11].
The rise of biomedical science, including genomics, digital medicine, artificial intelligence (AI), and its subset, namely, machine learning (ML), provides the backdrop to healthcare transformation, with novel emerging technologies, and there is a prerequisite of a new type of labor force and standard of practice. Genomics and other technologies, including biometrics, tissue engineering, and the vaccine industry, can improve and transform diagnostics, therapeutics, care delivery, regenerative treatment, and precision medicine models [12]. Table 1 describes the definitions of terms related to AI.

Table 1.
Definition of terms related to AI.
Moreover, digital health technologies (DHTs) comprise mobile health (mHealth), health information technology (HIT), wearable devices, telehealth, telemedicine, mobile Internet devices (MIDs), and personalized medicine [37], and recently, innovative technological advancements that are influencing smart health are AI, metaverse, and data sciences [38]. These technologies lead to better prevention; the early detection of fatal diseases; and the remote management of chronic diseases peripherally to the customary care locations, such as wirelessly observed therapy (WOT), following a novel method of monitoring adherence to therapy [39]. The most promising new way is to offer and deliver health services anywhere and at anytime in the age of disruptive and minimally invasive medicine. MIDs allow the recipient to access important resources, including associated applications and social media (SM). The available applications of MIDs are numerous and provide access to scientific databases such as Medscape, Web of Science, and Scopus to professionals. While SM networks, namely, YouTube, Facebook, WhatsApp, Wikipedia, and other instant messaging applications (IMAs), can be available for both professional and non-professionals. Such digital health modalities using AI in healthcare are accelerating in the post-COVID-19 era [40].
AI, ML, and DHT have fueled a revolution in healthcare, especially since COVID-19 crippled the global healthcare system. In particular, AI is presently integrating new technologies, such as the Internet of Things (IoT), into the DHTs used by consumers. As AI and ML are widely implemented in healthcare systems, the IoT is expected to transform into the intelligence of things [1]; how the collected data are utilized to alter processes would swing behavior and values [41]. In addition, intelligent medical technology, i.e., powered AI, has been met with some enthusiasm among ordinary people, because it makes the 4P model of medicine, namely, predictive, preventive, personalized, and participatory, and thus patient autonomy, possible [42]. Integrating AI into healthcare has already been shown to lead to better, faster, and lower-cost healthcare [12].
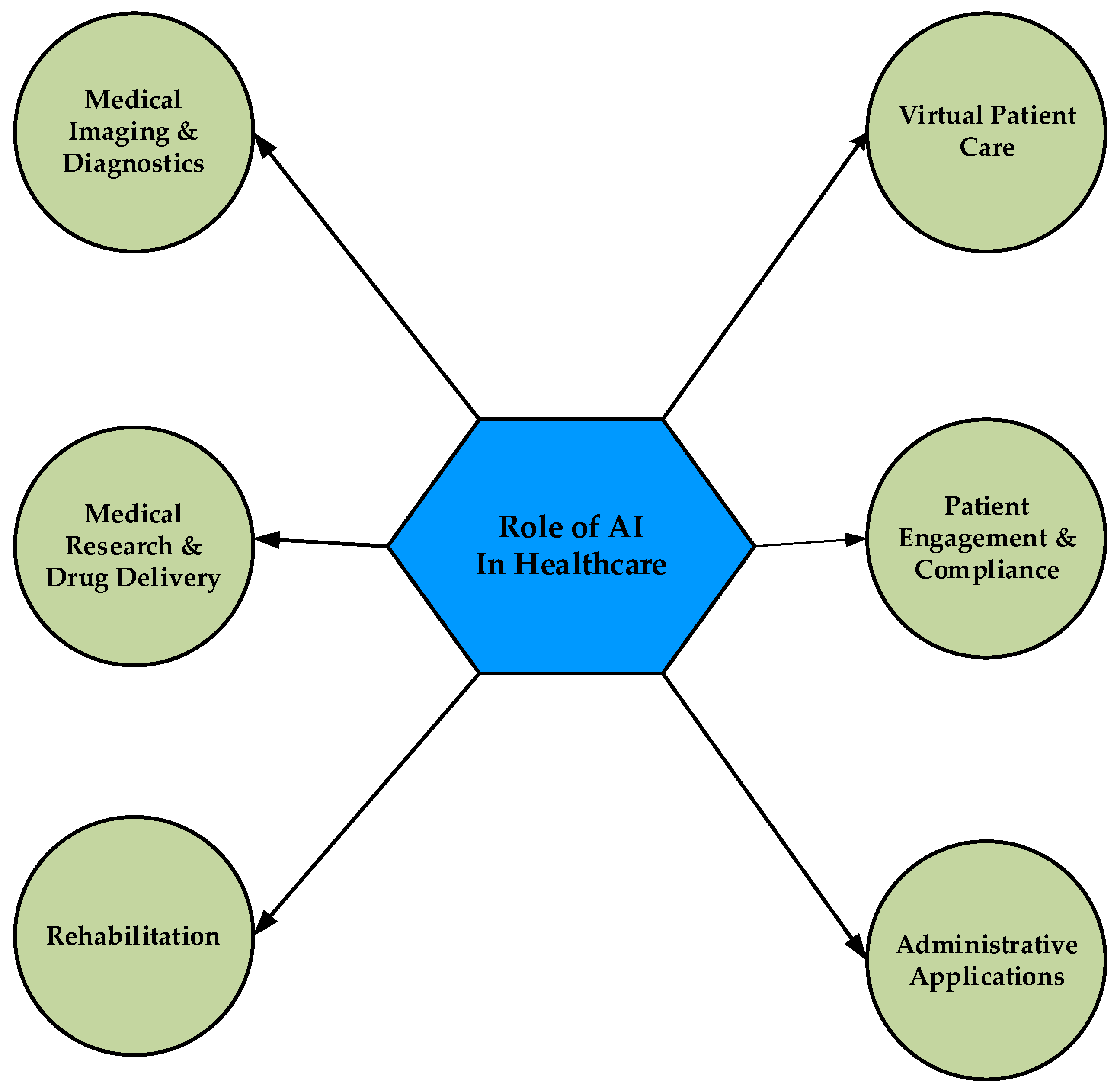
Digital health tools offer healthcare providers a more holistic view of patient health by allowing providers to access patient data. They also allow patients to be provided with more statistics about their health by their physicians. These offer real opportunities to improve therapeutic outcomes and efficacy, although there are concerns that such modalities may have greater psychological impact, particularly with the widespread use of SM and IMAs by patients, the public, and professionals [43]. Additionally, accumulated data from multiple sources, such as health information systems (HISs), wearable devices, telemedicine, mHealth, telehealth, MIDs, and other AI-powered medical technology [44], create big data that accelerate the utilization of ML and AI in health systems using the learning process from the data these sources obtain, including data from research information, user experience, and the investigation of big datasets [45]. Further, electronic health records (EHRs) encompass various healthcare data of patients. Such health datasets can be connected using novel AI technologies to gain accurate insights into patient care. AI has also emerged as a choice for big data applications in healthcare [46]. Moreover, big data analytics enables healthcare providers to improve their clinical services by improving EHRs using analytical algorithms [47]. Such analytics also uses the advancement of AI to filter big data on various grounds for better data analysis [48]. As AI is widely used in various areas of healthcare to improve patient health outcomes and provide healthcare at lower cost, this review aims to reveal its role in healthcare, focusing on the following key aspects (Figure 1): (i) medical imaging and diagnostics, (ii) virtual patient care, (iii) medical research and drug discovery, (iv) patient engagement and compliance, (v) rehabilitation, and (vi) other administrative applications. In addition, the authors address some challenges to using AI in healthcare. These results complement the existing literature to take the benefits of AI tools one step further in healthcare.
Figure 1.
Application of AI in various aspects of healthcare.
2. Role of AI in Healthcare
2.1. Medical Imaging and Diagnostic Services
AI is a powerful tool for image analysis that is increasingly being used by radiology professionals for the early diagnosis of different diseases and for reducing diagnostic errors in the context of prevention. Likewise, AI is a smart and potential tool for analyzing ECG and echocardiography charts that cardiologists use to support their decision making. The Ultromics platform, which was reported in a hospital in Oxford, utilizes AI to analyze echocardiography scans that sense heartbeat patterns and detect ischemic heart disease [49]. AI has presented encouraging results in the early detection of diseases such as breast and skin cancer, eye disease, and pneumonia using body imaging modalities [50,51,52]. AI tools analyze speech patterns to forecast psychotic occurrences, and recognize and screen the features of neurological diseases such as Parkinson’s disease [53,54]. A recent study predicted the onset of diabetes using ML models. The results showed that a two-class augmented decision tree was the best model to predict the different variables of diabetes [55]. Furthermore, Gudigar et al. [56] stated that several medical imaging tools, including X-ray, computed tomography (CT), and ultrasound (US), applying AI techniques have significantly contributed to combating COVID-19 by aiding in early diagnosis. Their results reported that all handcrafted feature learning (HCFL), deep neural networks (DNN), and hybrid methods were able to predict COVID-19 cases. A recent review also explained in detail the use of CT scan, X-rays, MRI, and ultrasound in diagnosing COVID-19. It stated that AI has been instrumental in helping the public fight against the dreaded virus [57]. Moreover, a deep learning model named transformer is used in medical imaging analysis and includes registration, detection, classification, image-to-image translation, segmentation, and video-based applications [34]. Previous studies explained the application of transformers in differentiating COVID-19 from pneumonia using X-ray and CT images to meet the severe prerequisite to quickly and efficiently manage COVID-19 cases [58,59]. Another study applied the ImageNet-pretrained vision transformer (ViT)-B/32 network to detect COVID-19 using inputs such as patches of chest X-ray images [60]. A study by Wang et al. [61] proposed a new hybrid chest CT-built method to automatically detect COVID-19. It is a computer vision-based diagnosis technique based on wavelet Renyi entropy (WRE) and a proposed three-segment biogeography-grounded optimization (3SBBO) algorithm. It comprises WRE, a feedforward neural network (FNN), and the 3SBBO algorithm. WRE extracts image features; 3SBBO optimizes the biases and weights of the network; and the FNN classifies the images. This method showed better performance than kernel-based extreme learning machine, extreme learning machine with bat algorithm, and radial basis function neural network in detecting COVID-19. Additionally, Gheflati et al. [62] reported that the ViT is used to sort normal, malignant, and benign breast tissues based on ultrasound (US) images. It showed better efficacy in the classification of US breast images than convolutional neural networks (CNNs).
Furthermore, AI comprises the application of artificial neural networks, i.e., deep learning techniques named Generative Adversarial Networks (GANs), that impact the field of radiology. GANs contain two artificial neural networks, i.e., (i) a generator that synthesizes images similar to real images, and (ii) a discriminator that reveals the difference between synthetic and real images. Concerning radiology, the generative model can duplicate the images consistent with training and synthesize new images with the features of the images in the training dataset. The discriminant model is trained to classify the images, for example, whether a radiograph displays or not pneumonia. It was concluded that the generator model trained together with the discriminator model can result in progresses in radiological activities such as abnormal detection, image synthesis, and cross-domain image synthesis [63]. Skilled radiologists found it hard to distinguish between lung cancer nodules images generated by GANs and real images [64]. In addition, GANs offer an excellent opportunity to improve medical education and research. They swiftly develop training material and simulations for student learning. For instance, when students find it hard to differentiate “lower lobe collapse” and “consolidation,” samples of each type could be developed and displayed to them. Thus, synthetic data can support student learning by presenting edge-case learning resources. Furthermore, synthetic control arms have been developed by modeling placebo groups grounded on historical information, and those arms reduce the requirement of a real-life placebo group, thereby reducing costs and expanding the count of treatment arms in clinical trials [65]. Additionally, ChatGPT is a deep learning-based large language model used by the public for medical advice; thereby, it has turned into a basis for concern. Substituting professional medical advice, the public could be tempted to use such a model to determine possible diagnoses based on clinical features or gain treatment suggestions [66]. A previous US-based study found that about one-third of adults required Internet-based medical advice for self-diagnoses. Subsequently, about half of them consulted a doctor about the Internet-based outcomes [67].
Apart from this, AI-based medical practice, mainly medical imaging-guided diagnosis and therapy, is facilitated by a metaverse of ”medical technology and AI” (MeTAI). The critical applications of MeTAI include “virtual comparative scanning”, “raw data sharing”, “augmented regulatory science”, and “metaversed medical intervention”. A model execution of the MeTAI ecosystem is described as follows: The patient’s scans are first simulated using virtual machines to reveal the best imaging outcome before he/she undertakes an actual CT scan. Based on this knowledge, a real scan is made. Subsequently, the metaverse images are shared with the patient’s physicians’ squad after obtaining the patient’s approval. Following security procedures, the tomographic raw data and images are shared with the medical researchers. The collection of real and simulated images, data, and other medical evidence can be combined in the metaverse and applied in augmented clinical trials. Lastly, the patient is exposed to a metaverse-assisted remote robotic operation and followed up in the metaverse for rehabilitation if it is therapeutically advised. However, MeTAI experiences challenges such as security, disparity, investment, and privacy [68].
Additionally, medical scans are systematically gathered and saved for some time and are freely obtainable to train AI systems [69]. Those AI systems could reduce the time and cost of examining medical scans and potentially allow more scans to be taken for superior targeted management [70]. AI is also impacting clinical decision making and disease diagnosis. It can process, analyze, and report a large number of data across different modalities for disease diagnosis and clinical decision making. It can support physicians to make better clinical decisions or even replace human decisions in therapeutic zones [71]. Furthermore, investigations leveraging computer-aided diagnostics have presented outstanding sensitivity, accuracy, and specificity in uncovering minor radiographic deviations, with the capacity to advance public health. Nonetheless, outcome assessment in AI imaging studies is usually described as lesion detection, ignoring the biological severity and nature/type of a lesion, which could give a skewed picture of AI output. In addition, applying non-patient-related radiological and pathological endpoints could increase the expected sensitivity at the cost of increasing false positives and possibly overdiagnosing by detecting minor abnormalities that might mimic subclinical disease [72].
2.2. Virtual Patient Care
Baig et al. [73] noted that the advancement of wearable technology and the potential of using ML and AI in healthcare is an idea that has already been explored. Thus, patient monitoring and management via virtual care with active and sensible wearable technology solutions have become a reality and part of the standards of care. In addition, AI plays a role in controlling chronic diseases such as diabetes mellitus, hypertension, sleep apnea, and chronic bronchial asthma using wearable, non-invasive sensors. [74]. A previous study recommended a smart sensor system based on a combined sensor network to observe a person’s home and environment and obtain data on a person’s health status and behavior. The recommended platform includes sensors that are unobtrusive, biomedical, and wearable. These sensors monitor physiological variables such as respiratory rate, pulse rate, breathing waveform, blood pressure, and ECG. A smart device (such as a tablet) has been proposed to act as an interface between the person and the sensors. In addition, the collected data are sent to the cloud for storage and data analysis for elderly care [75]. A case report by Patel and Tarakji [76] also discussed a patient in whom atrial fibrillation was positively detected as the probable cause of her stroke following a broad negative examination. The patient was warned to record ECG signals using a wearable digital device. Her electrophysiologist later confirmed those recorded signals. Thus, consumer wearable digital devices support reaching the precise diagnosis. Regarding mental health disorders, Sukei et al. [77] demonstrated the possibility of building ML models for predicting emotional states using mobile sensor data that can handle diverse data with large amounts of missing information. Such models could provide valuable tools for physicians to assess patients’ mood states. Further research is recommended to find a solution for sparse and lost tagged data so that future focus can be placed on developing more innovative models.
Since the prevalence of SARS-CoV-2 has caused the COVID-19 pandemic worldwide, progress has been observed in wearable devices that measure physiological changes in biometrics or even transmit online active patient monitoring [78]. Bogu and Snyder [79] suggested that wearable sensor data could be used as indicators for the early prediction of COVID-19, and with real-time wearable research on COVID-19 cases, the clinical features glossed over by users and justified by laboratory investigations will continue to improve knowledge related to tracking and detecting COVID-19 outbreaks. AI using predictive modules with ML and big data can help predict the progression of some diseases, such as diabetic nephropathy, and even diagnose SARS-CoV-2 infection in solid organ transplantation [80]. Yu et al. [81] emphasized the importance of integrating AI into bedside care in COVID-19 and the coming pandemic after examining encounters in emerging AI-enabled applications for point-of-care use in such events. In addition, the necessity of remote healthcare services has been created due to the COVID-19 pandemic. Metaverse applications can deliver a better experience than traditional videoconferencing-grounded telemedicine applications [82]. A recent study stated that the growth of telemedicine with metaverse development increased 38-fold during COVID-19 [68]. Such growth could have been due to the decrease in face-to-face consultations and the control of the risk of spreading the virus during the COVID-19 pandemic [83,84]. It also revealed the possibility of new metaverse tools, namely, virtual comparative scanning and raw data sharing, which would be consistent, easy to use, and inexpensive, and would work well [68]. Additionally, metaverse systems could utilize augmented reality (AR) glasses so that the users can access live videotapes and audio chats to interact with clinicians in real time. AR solutions would allow users to connect directly and offer a live flow of emergency circumstances for remote physicians to deliver on-time, faster, and on-spot management [85]. The application of current technologies such as AI, telepresence, blockchain, virtual reality (VR), augmented reality (AR), and digital twinning provides the experience of innovative means for offering low-cost management that improves patient outcomes. The metaverse develops a virtual world experience using the Internet in which human emotions and motions are simulated. It comprises the comprehensive financial and social constructs of both real and virtual environments [86]. Furthermore, AI could aid in reinforcing the metaverse structure to improve the 3D immersive experience and enhance the essential services of virtual worlds [87].
Remote patient monitoring (RPM) is a subset of telehealth, and it permits HCPs to monitor, investigate, and report patient conditions away from the traditional location. RPM smooths the performance of medical action using sensors and communication technologies. It makes it easier to remotely examine health data or patient issues. It also allows patients to engage and recognize their health condition [88]. The reliability of conventional patient-monitoring structures hinges on HCPs’ time management, which relies on their workload. Such surveillance also includes invasive methods requiring skin contact to screen health status. RPM in healthcare is achieved by integrating novel IoT methods: contact-based sensors, wearable devices, and telehealth applications. It is often applied to examine vital signs or other physiological variables such as the recognition of motion, which can support medical judgment or therapeutic regimens for diseases such as psychological illnesses and movement disorders [89]. Additionally, healthcare providers leveraged RPM platforms to facilitate the continuity of patient care during the COVID pandemic. A recent study evaluated two remote patient-monitoring platforms, the CareSimple COVID platform and the Telecare COVID platform, for monitoring COVID-19 patients. These two platforms were reported to have been well received by COVID-19 patients, with minimal significant discrepancies in patients’ experiences of the two platforms. It is recommended to consider using these platforms in a post-pandemic and post-hospitalization period [90]. Concerning RPM applications, conventional ML and deep learning are commonly used AI technologies to sense and forecast vital signs and classify patients’ physical movements. AI-powered RPM designs have transformed healthcare monitoring applications to detect early patient deterioration, absorb patient behavior patterns using reinforcement learning, and personalize the monitoring of patient health variables using federated learning. However, AI can transform RPM facilities, but it has some challenges, such as privacy, signal processing, data volume, uncertainty, imbalanced datasets, feature extraction, and explainability [89].
Moreover, ChatGPT, an AI language model, was developed by OpenAI. It functions as a more accurate AI-powered chatbot that can understand natural language conversations and respond to user queries. The ChatGPT-powered chatbot delivers information about a particular medical disease or management regime. It delivers precise and current replies to the patient’s questions concerning their clinical features, prescription drugs, and therapeutic procedures in various languages. It outlines patients’ medical information for HCPs and may aid them in performing RPM to sustain patient health. Further, it reminds patients to check their vital signs so that they can alarm HCPs if any abnormal changes occur. It allows patients to fix their appointments with physicians [91]. ChatGPT might also offer responses for a computer program that helps patients handle their treatment, similar to a virtual assistant who alerts them to follow their medical prescription and provide information about their health status. The growth of virtual assistants for patients is an example of how ChatGPT is applied in medicine. A virtual assistant may counsel in treating a chronic disease such as diabetes or prescribe over-the-counter drugs or home medicines to flu or cold patients. Digital platforms such as mobile applications, voice assistants, and websites may be applied to access these virtual assistants. However, ChatGPT in healthcare has limitations, namely, issues related to medical ethics, data interpretation, privacy, security, consent, and liability [91].
On the other hand, data connectivity is a disadvantage of installed Wearable Patient-Monitoring (WPM) systems, where patients are secured inside fixed spaces with low-Bluetooth-range monitoring devices. In addition, end-user acceptance is a crucial aspect of WPM systems. It relies on user awareness, and patient and physician acceptance. Cost issues can arise when using mobile data for communication over time and different data collections [73].
2.3. Medical Research and Drug Discovery
AI is ideally suited to analyze the large and complex datasets used in medical research [92]. In addition, it can be applied to hunt scientific research works, integrates various types of data, and supports drug innovation [93]. Pharmaceutical agencies are focusing on AI to streamline drug development. Scientists can utilize predictive analytics to recognize appropriate aspirants for clinical trials and develop exact models of biological processes [92]. ML contributes to clinical trials in the pre-trial phase, choosing the cohort, organizing of participants, and collecting and analyzing data. It can augment the patient-oriented view, generalizability, efficacy, and achievement of clinical trials. However, ML needs more emphasis on its functional and philosophical obstacles in clinical trials. In addition to ML, natural language processing (NLP) has exposed potential across various actions enhancing participant management in clinical trials; however, these tools’ effects on clinical trial quality and participant experience are uncertain. Further research can be conducted comparing different methods to improve participant management [94]. In clinical research, generative AI may be used to create synthetic data to enhance datasets and increase diversity [65]. Additionally, researchers can perform trials in an immersive and controlled setting using metaverse applications. The benefit of applying the metaverse is aiding research collaboration among the researchers who are physically distant. The metaverse permits them to research together in a virtual space similar to researchers that are in the same chamber [95]. Another AI-based tool, ChatGPT, may be used in clinical trials to support data collection and provide information about clinical trials [91]. It can aid in condensing pertinent publications and recognizing significant results, supporting medical researchers to competently navigate massive Internet-based evidence [96]. In addition, a chatbot employing ChatGPT aids in translating the medical language for medical researchers. Nevertheless, more ethical issues may arise when using chatbots in medical research [91].
Moreover, AI technologies in drug discovery have developed from ML, bioinformatics, and cheminformatics models [97]. These technologies can dramatically decrease the high cost and time needed for new-drug discovery [98]. An earlier study stated that an AI-based robot scientist (Eve) performed the drug development process rapidly and economically [99]. Concerning drug discovery, AI is mainly used to search for candidate molecules, but it is probable that it could be dynamically used in drug discovery in the future [98]. Many drug discovery successes supported by AI indicate the capability of AI-built-in firms of rapidly exploring drug candidates. For instance, Toronto-based deep genomics utilized an AI workbench platform to create a new genetic target and the respective oligonucleotide drug candidate DG12P1 for managing an unusual, inherited form of Wilsons’ disease [97]. Furthermore, recognizing new drug targets is crucial while conducting drug discovery research for finding new first-in-class clinical drugs [97]. AI can detect hit and lead compounds and offer the rapid authentication of the drug target and the better scheming of drug structure design [100,101]. The capability of AI of forecasting the interaction between drug and target was also utilized to aid the repurposing of current drugs and to evade polypharmacology. Repurposing a current drug passes it toward subsequent phases of clinical trials [100]. Previous studies stated that ChatGPT might be applied to assess a large body of scientific evidence, comprising patents and research publications; thereby, new drug targets and creating innovative ideas are determined. In the case of drug development, it helps train the model on a massive volume of scientific evidence before the model is used to deliver assumptions or suggestions for further research [102,103]. Apart from this, AI is used for drug screening [104]. Previous studies stated that various algorithms, namely, extreme learning machines, DNNs, random forest (RF), support vector machines (SVMs), and nearest-neighbor classifiers, are applied for virtual screening (VS) grounded on synthesis viability and for forecasting in vivo toxicity and activity [105,106].
Notably, reviewing the proteins constituting a virus (spike protein) is the function of AI in vaccine development. The categorization of numerous components in a complicated structure can be feasible using an AI system to determine the one that most probably elicits a robust immunological response [107]. Further, the evolution of AI systems in healthcare supports the innovation of the genomic series of the COVID-19 virus and its variants. It also aids in developing vaccines and drugs (comprising drug repurposing) to obtain active preventive and healing agents for restraining the COVID-19 pandemic [108].
2.4. Patient Engagement and Compliance
Patient engagement and compliance is healthcare’s ‘last stretch’ issue and the end blockade between better and poor health outcomes. Non-compliance means when a patient fails to shadow a treatment course or take the recommended medications. If patients are highly engaged in healthcare, their health outcomes are probably better, i.e., healthcare utilization, cost, and patient experience [109]. A healthcare leaders and executives survey reported that less than 50% of their patients were highly involved in treatment plans [110]. Healthcare providers use their clinical experts to develop treatment plans to improve patients’ acute or chronic health. Nevertheless, mostly, it does not matter when a patient misses the required behavioral changes, such as controlling weight, scheduling a follow-up visit, and obeying a treatment plan [109]. Such conditions raised the implementation of AI to successfully enhance patient engagement. ML and workflow engines are progressively being applied to driving composite interventions and the care spectrum [111]. Messaging alarms and appropriate custom-made material that encourage behavior at moments is the auspicious pitch of research [109].
Moreover, a study reveals that leveraging apps and online portals facilitating patient communication with HCPs can improve engagement rates by up to 60% and above. Healthcare apps collect, save, and distribute patient data on the cloud. These apps also permit users to access data wherever and whenever they want and possess the capacity to enhance a patient’s health outcomes. These are AI-based apps for medical consultation that let patients obtain info (non-emergency). Certain apps have also been given the ability to follow up with the patient and give alarms for drug intake [112]. Furthermore, ChatGPT is being utilized in various healthcare apps, including in automating long tasks such as summary, note writing, and report production, thereby making those tasks time-saving and more efficient. It assists patients in checking symptoms, fixing appointments, and managing drugs, aiding patient compliance and education, and the self-management of chronic diseases [91].
2.5. Rehabilitation
AI has innovative applications in the field of rehabilitation. It is an idea that includes physical (robotics) and virtual (informatics) branches. Additionally, a subset of AI known as ML refers to precise methods for building algorithms that naturally improve with practice. In rehabilitation, ML is used for perioperative medicine, brain–computer interface technology, myoelectric control, symbiotic neuroprosthetics, etc. ML methods have also been applied in the field of the musculoskeletal system, e.g., in the evaluation of patient data, clinical decision support, and diagnostic imaging. In therapy, an artificial cognitive application was used to judge rehabilitation exercises based on the signals from the machine [113].
As a result of technological advancement, AI and robotics are transforming approaches and competencies in rehabilitation research and practice. For example, smart homes can assist residents with daily activities and alert caregivers when assistance is needed. In addition, smart mobile and wearable devices are available to collect data and provide users with information to assess health improvement and review progress toward personalized rehabilitation goals [114]. Additionally, inertial sensors in wearable technology can be recognized to check whether individuals are properly performing and adhering to exercise regimens [115]. Such exercise adherence was assessed in normal individuals following a rotator-cuff exercise regimen while wearing an Apple iWatch. Several supervised learning methods were applied to accurately categorize exercise accuracy across all algorithms [116]. A neural network achieved 99.4 percent detection accuracy, demonstrating the potential utility of wearable devices and ML in exercise tracking. However, assessing performance using wearable devices alone could possibly be insufficient to enhance adherence because of the variable snags to adherence connected with exercise efficacy [117,118]. Additionally, physically and socially supportive robots can be used to help individuals recover from injury or illness. These robots also support bridging gaps resulting from cognitive, motor, or sensory losses. These technologies play an important role in helping people increase their functional ability, independence, and healthy well-being [114]. Patients with musculoskeletal dysfunction were treated with simple mobilization using dextrous or soft robotic hands. However, the long-term efficacy of such treatment has yet to be demonstrated [119]. A recent study suggests that AI-enabled robotics could monitor the patient for perfection of movement and help the patient efficiently perform movements in the future [120]. Frackiewicz [121] stated that HCPs could match the gap between the need for rehabilitation services and the obtainability of trained therapists by adding an AI-driven tool, ChatGPT, to the rehabilitation sessions. Those can provide patients with an AI-driven method that complements conventional therapy. Using ChatGPT, the patients are provided with tailored and collaborative assistance; therefore, patients remain engaged and interested during their recovery process. ChatGPT can be programmed to deliver exercise recommendations and screen progress and offer feedback to individuals recovering from physical injuries. Further, it can also assist stroke or head injury patients in practicing their speech and language skills by involving them in conversation. This tool can be easily accessible using digital devices at home or outside. A recent study stated that a language model such as ChatGPT was trained to redraft text in a highly empathic way. It provides easy communication in a peer-to-peer mental health assistance system and improves non-expert conversational skills. It emphasizes the possibility of using human–AI partnerships to improve various community-based tasks relying on self- or peer-managed therapy, such as cognitive behavioral therapy [122].
Additionally, metaverse neurorehabilitation encompasses an AI-based gross motor function classification system (GMFCS), rehabilitation materials as a reward through rehabilitation, virtual character movement using weight shift, and deep learning-based movement assessment. It is planned to enhance interest and entertainment, deliver remedial exercises with AI, and limit the risk of COVID-19 transmission [123,124]. A recent study observed that metaverse physiotherapy (MPT) reduced perceived COVID-19 infection and enhanced cardiopulmonary and gross motor function compared with conventional physiotherapy in treating CP children [125]. In addition, AI has been used in gait analysis, where ML-driven video analysis demonstrated the ability of computers to automate the detection of gait abnormalities and related pathologies in patients with osteoarthritis and Parkinson’s disease [126]. Physiotherapy at home can be successfully delivered with counselling/advice, real-time observation, and remote tracking by digital therapists [120]. Lambercy et al. [127] envisioned an approach to delivering remote neurorehabilitation using digital interventions such as minimally supervised assisted therapy, which could help stroke victims continue care from the hospital and to their homes. However, AI-embedded technologies for remote neurorehabilitation should meet the technical needs, namely, utility, safety, and robustness, as the patients are trained with the devices at home, and their needs are met. These technologies should be scalable, and their application in neurorehabilitation requires a clinically motivated and transparent approach to patients and their families as well as HCPs. This condition could increase confidence in technology-enhanced rehabilitation in a home model. Additionally, all of these characteristics are critical to ensuring that patients with neurological disorders consent to technology-enhanced rehabilitation and actively engage in therapy [128]. Such technology-assisted rehabilitation at home notably impacted neurorehabilitation during and after the COVID-19 pandemic by providing widespread access to high-quality, sustained, and high-dose therapy that enhanced long-term functional outcomes and promoted independence and quality of life in stroke patients [127].
Concerning sports medicine, a recent review found that AI is a promising avenue for integration into wearable technologies. AI techniques processing data from sensors could monitor patterns in physiological measurements, as well as positional and kinematic data, to indicate how athletes can improve their performance. AI can improve how injury prediction models work, increase the diagnostic precision of risk stratification systems, provide a reliable technique for continuously monitoring patient health data, and improve the quality of patient experience. Although AI has beneficial applications in sports medicine, several challenges may hamper its adoption in wearable devices [129]. These challenges include missing data, socioeconomic bias, data security, outliers, signal noise, and the difficulty in obtaining high-quality data with wearable technology [129,130]. For example, sensors that monitor heart rate detect artifacts due to arm movements during physical tasks: Such a situation could be handled by highly complex sensors that could collect and transmit clean data [129]. Another critical challenge to their adoption is patient acceptance. Previous studies stated that half of consumers with a wearable device had stopped using it, and this condition had occurred within six months in one-third of them [131,132]. A previous study reported that half of patients felt that the use of AI in wearable technology was a significant opening, while 11% felt that it was harmful. Patients feared that the technology could exploit and misuse their data and affect the human aspect of healthcare. Therefore, patient education on how AI supports clinicians, and their abilities and limitations is needed to improve their acceptability and adoptability of AI [133].
2.6. Administrative Applications
AI can reduce administrative burdens by automatically populating structured data areas from therapeutic notes, retrieving key data from past medical records, and collecting documented patient encounters [134]. For example, the average nurse in the United States spends a quarter of his/her working hours on regulatory and administrative duties [135]. Physicians’ and nurses’ time could be saved using voice text writing [134]. Although rule-based systems integrated with electronic health record (EHR) systems are extensively used, they lack the accuracy of additional algorithmic systems based on ML [110]. Wang et al. [68] stated that Amazon is working on an innovative ML solution to extract valuable information from unstructured EHR data and scientific notes. Furthermore, Li et al. [32] introduced bidirectional encoder representations from a transformer for EHR (BEHRT), a deep neural sequence transduction model for EHRs. The BEHRT showed the ability of using various embeddings, such as age, position, visit, and event, to characterize the patient’s clinical history. It can concurrently forecast the probability of 301 conditions in an individual’s future visits. It significantly improves the average precision scores in various tasks compared with present deep EHR models. It can integrate various heterogeneous concepts, such as assessment, diagnosis, and drugs, due to its stretchy construction, thereby enhancing the accuracy of its predictions. A recent study proposed a hierarchical BEHRT (Hi-BEHRT) model, a hierarchical transformer-based model, for risk prediction. The study observed a significant performance of Hi-BEHRT compared with existing deep-learning models in risk prediction tasks for patients with a long clinical history of diabetes, heart failure, stroke, and chronic kidney disease [35].
Interestingly, Robotic Process Automation (RPA) can be used for various healthcare functions. These functions include clinical records, revenue cycle administration, claim handling, and medical record management [136]. Additionally, chatbots have been used by healthcare organizations (HCOs) for telehealth, mental health, and patient interfaces. These NLP-based tools can be helpful for simple transactions such as booking appointments or refilling prescriptions [137]. Regarding payment administration and claims, another AI technology, ML, can be applied to match data across different websites [134]. Insurance agencies are responsible for verifying the accuracy of many claims. Inappropriate claims slipping through the cracks demonstrate significant monetary potential waiting to be resolved using data reconciliation and claim scrutiny [109].
In addition, Corny et al. [138] concluded that a hybrid ML-based decision support system (ML rule-based expert system) was remarkably more accurate in detecting prescribing errors in a clinical setting. A recent review examined the development of AI tools for clinical pharmaceutical services and found that ML techniques and subsets, namely, NLP and deep learning, were widely used. It concluded that the growth of AI-based applications and tools for clinical pharmacy services is just beginning. Significant action needs to be taken in conjunction with data professionals to better assess whether these AI tools have value for clinical pharmacy services in real-world settings. Pharmacists need to recognize these gains in order to properly employ them while maintaining their social relationships with patients and healthcare teams [139].
3. Challenges Faced by AI Utilization in Healthcare
3.1. Ethical and Social Challenges
Several ethical and social disputes raised by AI overlap with those raised by high reliance on technology; automation; data usage and issues arising from the usefulness of ‘telehealth’ and assistive technologies, as the effectiveness of AI increases ethical concerns, including the issue of accountability when AI is used in decision making; the ability of AI to make erroneous judgments; AI yield authentication issues; the confirmation of the protection of sensitive data; intrinsic biases in the data used in AI system tests; maintaining public confidence in the growth and benefits of AI systems; influencing the sense of dignity and social isolation of the public in care settings; implications for HCPs’ roles and skill requirements; and the ability of AI to be used for malicious activity. Furthermore, safety and reliability problems may occur while using AI to deliver treatment, make decisions, and control healthcare equipment. AI could cause errors, and those might be challenging to detect or might induce adverse effects, which could lead to severe consequences [69]. For instance, the AI app predicting pneumonia-related complications mistakenly advised physicians to discharge patients with asthma because it failed to consider related information [140]. Concerning transparency and accountability, queries arise about the accountability of AI-made decisions and compensation for individuals affected by AI use. Issues related to AI output authentication and error or data bias recognition arise, especially with ML technologies, which could be mainly non-transparent due to the method whereby they constantly review their own limits and guidelines as they learn [69]. Additionally, explainability denotes a main obstacle facing AI regarding its practical implications in various domains. It is crucial and tackled by “Explainable artificial intelligence (XAI),” a branch of AI research, to overcome the poor understanding of AI-based applications and improve the acceptance of those applications concerning the decision-critical domain [141]. Furthermore, the internal mechanisms of AI are commonly non-transparent and complex for humans to comprehend. This condition can result in poor trust and comprehension concerning AI-made decisions. To overcome such issues, XAI is used to make the internal mechanisms of AI transparent and explainable to humans to create trust in and comprehension of AI-made decisions [142]. It is a pool of techniques that understand and trust the outcomes of ML algorithms [143]. In healthcare, doctors and patients can realize the reasons behind diagnosis using XAI, since it can explain diagnostic decisions made by AI [142]. A recent study found that XAI establishes trust in AI by giving visual feedback to the user regarding significant metrics that are used to obtain the model prediction [144]. Another study observed that XAI methods are required to improve radiologists’ trust in classification predictions of CT images with the acquisition of numerous visual insights into the automatic workflow [145].
Furthermore, AI might poorly function with data scarcity or difficulties in digital data collection. This state could impact the individuals understated in clinical trials or those with rare medical diseases [69]. While training AI applications using data, these applications can replicate and strengthen data biases even though those can decrease human error and bias [146]. Such data for training AI could poorly represent the broader populace and result in unfair decisions replicating more comprehensive biases in societies [70]. Those applications in healthcare also face data privacy and security challenges, because they utilize sensitive and private data bound by legal panels. Although AI can be applied for detecting cyber attacks and protecting healthcare desktops, there is the possibility for AI systems to be hacked to access sensitive data or spammed with biased or false data in such a way that might not be simply traceable [69]. Sunarti et al. [147] also listed the ethical issues faced by clinical AI applications: privacy, safety, security, the right to choose and try, cost, information and consent, access, and efficacy. Therefore, critical medical–ethical principles, such as beneficence, autonomy, equity, and non-maleficence, should be emphasized before integrating AI into healthcare systems [148].
3.2. Governance Challenges
As the implementation of AI technologies in healthcare increases, there is a serious requirement for proper governance to overcome regulatory, ethical, and trust issues [149,150]. Active governance at the hospital level offers an opportunity to accurately address these issues in the implementation and use of AI [151]. Additionally, a recent study found that governing AI technologies at the healthcare system level is critical to patient safety and healthcare system accountability. Such governance also increases clinician confidence, improves acceptance, and makes significant health consequences possible. The governance structure should be comprehensive to address the challenges related to clinical, operational, and leadership domains while deploying AI-powered applications [152].
Additionally, AI has applications in areas that need regulation, including healthcare, research, and privacy. Nonetheless, AI is developing rapidly and commercially, which could challenge the known outlines [70]. National and international regulations are, therefore, required to introduce AI-controlled applications in healthcare as part of the principles of medical ethics. As such, the European Union (EU) developed general data protection regulation (GDPR), a data protection regulation in 2018, to control AI. GDPR shields the personal data dealt with by a data processor or controller recognized inside the EU. It is a base for essential reforms in the United States and Canada [153]. Recently, the revealed artificial intelligence act (AIA) was developed by the European Commission to address various risks related to the social adoption of AI. It is a set of regulations encouraging the acceptance of AI and intends to avoid or alleviate harms connected to specific usages of technology. According to the proposed act, high-risk AI systems must undergo pre-deployment conformity appraisals and post-market observational analysis to confirm that they meet all the necessities of AIA [154].
3.3. Technical Challenges
Technically, AI models must be simple in their properties and functions in order for HCPs to efficiently operate them [155]. On the other hand, there are a few hurdles to adopting AI in healthcare, including the lack of capacity of developing and maintaining IT infrastructure to support the AI process, the increased costs associated with storing and backing up data for research purposes, and the high cost of augmenting data validity [156]. In addition, AI algorithms can suffer from a variety of shortcomings, including inapplicability outside of the training domain, bias, and brittleness (tendency to be easily fooled) [157]. Important factors to consider include dataset shifts, randomly matching confounders instead of true signals, the prevalence of unintended biases in clinical practice, providing interpretability for algorithms, developing reliable measures of confidence in the model, and challenging the generalization to different populations [158]. Therefore, healthcare providers should develop and implement an effective strategic plan for implementing AI in healthcare to address the issues related to cost, technological infrastructure, and the use of AI systems for HCPs.
Additionally, HCPs often mistrust or poorly understand AI-grounded clinical decision support systems because of unidentified risks, a vital blockade to extensive adoption. In such circumstances, XAI solutions are emphasized to enhance end-user trust and overcome low AI adoption [144]. Additionally, Choudhury and Asan [159] found that factors such as risks and trustworthiness of AI, workload, and willingness to receive AI training influenced clinicians’ perceptions of the use of AI in healthcare. The lack of AI accountability has also been identified as an inhibiting element in using AI. It is recommended that AI training be included in medical and nursing curricula to enable AI to be safely used in the future.
Similar to our brains, AI systems receive inputs and provide outputs. However, HCPs have no idea about what is being measured and how an AI system arrives at a result; all they know is the final output. This challenge in AI systems is called black-box problem [160]. Therefore, blaming healthcare practitioners for AI errors could be an obstacle to AI adoption, and it is recommended to develop policies and measures to protect doctors and AI in healthcare. This also emphasizes improving healthcare professionals’ risk perception and performance expectations of AI. It is crucial to ensure a user-friendly AI interface in which the information presented must have clinical relevance. There is a need to engage all stakeholders (providers, payers, and patients) and understand clinical needs before developing and promoting AI in healthcare.
4. Disadvantages of AI in Healthcare
Huge datasets are mandatory for machine learning and deep learning models to appropriately categorize or forecast various tasks. Nevertheless, the healthcare industry possesses a composite problem with data accessibility, since patient records are confidential and given the usual hesitancy among HCOs to exchange health data. In addition, data are not readily available once an algorithm is initially executed using them. Notably, ML-based systems can continually progress as additional data are provided to their training set; however, it is hard to attain this scenario due to internal corporate resistance [161]. Moreover, AI-based applications raise data security- and privacy-related issues. Hackers usually focus on health records during data breaches, since those records are significant and vulnerable. Hence, it is vital to uphold the confidentiality of health records [162].
Additionally, the overfitting issue occurs when the algorithm absorbs the connections between patient characteristics and results. This problem occurs due to numerous variables affecting the outcomes, which makes the algorithm make inaccurate predictions. Data leakage is another concern that describes AI’s ability to predict incidences beyond the diminished training dataset when the algorithm attains greater prediction accuracy [163,164,165]. Further, deep learning algorithms are less capable of giving substantial explanations for their predictions. An algorithm experiences difficulty in protecting itself legally when recommendations go wrong. It makes it difficult for experts to comprehend how the data are associated with their forecasts. The black-box issue in AI systems may lead the public to lose faith in healthcare systems [166].
The healthcare workforce may fear AI in healthcare, which might reduce their occupations and replace them. At the same time, they are in need to be re-engineered. Another issue with AI is the price tag covering the time and resources invested in training HCPs to successfully use AI [161]. In healthcare, insufficient experimental data authenticating the efficacy of AI-based drugs in planned clinical trials is a critical hindrance to the positive employment of AI. AI research has been mainly performed in non-clinical environments. Hence, the generalization of findings might be difficult. Similarly, the institutions are uncertain and reluctant to execute AI-based solutions because of the lack of empirical data and the rutted quality of research [167]. Other disadvantages of AI, in general, include the high costs of creating AI-based applications, making humans lazy, creating unemployment due to replacing repetitive tasks with AI, and a lack of emotions and creativity in machines [168].
5. Conclusions
AI technologies are being used for a range of healthcare applications. These technologies have been developed to support medical imaging and diagnostic services, fight the pandemic, provide virtual patient care, increase patient engagement and adherence to treatment plans, reduce the administrative burden on healthcare professionals, drive drug and vaccine innovation, monitor the compliance of patients with exercises, and carry out gait analyses used in technology-assisted rehabilitation. However, AI also faces various technical, ethical, and governance challenges as it moves forward in healthcare. It raises data security- and privacy-related issues because it utilizes sensitive and confidential data bound by legal panels. The use of AI in addressing challenges could be limited by the quality of existing health data and AI’s failure to reflect certain human characteristics, such as compassion. AI is more beneficial while functioning efficiently; however, it cannot replace the human connections that form teams. Human functions such as teamwork and team management are not possible-to-achieve goals, since machines cannot form a bond with humans. A key challenge to be solved for the future governance of AI technologies will be to confirm that AI can be developed and implemented in a way that aligns with people’s interests and takes into account technical, ethical, and social aspects. This study adds to the existing literature compiling the application of AI in medical imaging and diagnostics, virtual patient care, medical research and drug discovery, patient engagement and adherence, rehabilitation, and other administrative applications. Additionally, this is the latest update in the literature to address the ethical, social, governance, and technical challenges that HCPs face in adopting AI in healthcare.
Future Directions
Since this study is based on a general literature review, future research could focus on conducting a more comprehensive systematic literature review that can provide a deeper insight into this research topic. In addition, future research should focus on a cross-sectional survey of HCPs to collect primary data on all the key issues addressed in this study.
Author Contributions
Conceptualization, A.A.K. and F.A.A.-M.; writing—original draft preparation, A.V.S. and A.A.-M.; writing—review and editing, K.N., A.A.-R., A.A.K., S.A.-S. and D.A.M.; project administration, F.A.A.-M. and A.A.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
The authors thank Imam Abdulrahman Bin Faisal University (IAU) for providing the necessary resources and support to complete this research work.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Snowdon, A. Digital Health: A Framework for Healthcare Transformation. 2020. Available online: https://www.gs1ca.org/documents/digital_health-affht.pdf (accessed on 23 January 2023).
- Williams, O.D. COVID-19 and Private Health: Market and Governance Failure. Development 2020, 63, 181–190. [Google Scholar] [CrossRef] [PubMed]
- Tabriz, A.A.; Nouri, E.; Vu, H.T.; Nghiem, V.T.; Bettilyon, B.; Gholamhoseyni, P.; Kiapour, N. What should accountable care organizations learn from the failure of health maintenance organizations? A theory based systematic review of the literature. Soc. Determ. Health 2017, 3, 222–247. [Google Scholar] [CrossRef]
- Rand Review. Chronic Conditions in America: Price and Prevalence. 2017. Available online: https://www.rand.org/blog/rand-review/2017/07/chronic-conditions-in-america-price-and-prevalence.html (accessed on 11 July 2021).
- World Health Organization. Naming the Coronavirus Disease (COVID-19) and the Virus that Causes It. 2020. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(COVID-2019)-and-the-virus-that-causes-it (accessed on 6 July 2021).
- Butcher, C.J.T.; Hussain, W. Digital Healthcare: The Future, RCP Journals. Royal College of Physicians. 2022. Available online: https://www.rcpjournals.org/content/futurehosp/9/2/113 (accessed on 16 January 2023).
- Siriwardhana, Y.; Gür, G.; Ylianttila, M.; Liyanage, M. The role of 5G for digital healthcare against COVID-19 pandemic: Opportunities and challenges. ICT Express 2020, 7, 244–252. [Google Scholar] [CrossRef]
- Shakeel, T.; Habib, S.; Boulila, W.; Koubaa, A.; Javed, A.R.; Rizwan, M.; Gadekallu, T.R.; Sufiyan, M. A survey on COVID-19 impact in the healthcare domain: Worldwide market implementation, applications, security and privacy issues, challenges and future prospects. Complex Intell. Syst. 2022, 9, 1027–1058. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.M.; Lee, D. Opportunities and challenges for contactless healthcare services in the post-COVID-19 Era. Technol. Forecast. Soc. Chang. 2021, 167, 120712. [Google Scholar] [CrossRef]
- Carroll, W.M. Digital health and new technologies. In Nursing and Informatics for the 21st Century Embracing a Digital World, 3rd ed.; Productivity Press: New York, NY, USA, 2022; pp. 29–48. [Google Scholar]
- Mistry, C.; Thakker, U.; Gupta, R.; Obaidat, M.S.; Tanwar, S.; Kumar, N.; Rodrigues, J.J.P.C. MedBlock: An AI-enabled and blockchain-driven medical healthcare system for COVID-19. In Proceedings of the IEEE International Conference Communication, Montreal, QC, Canada, 14–23 June 2021; pp. 1–6. [Google Scholar] [CrossRef]
- Ng, R.; Tan, K.B. Implementing an Individual-Centric Discharge Process across Singapore Public Hospitals. Int. J. Environ. Res. Public Health 2021, 18, 8700. [Google Scholar] [CrossRef]
- Bajwa, J.; Munir, U.; Nori, A.; Williams, B. Artificial intelligence in healthcare: Transforming the practice of medicine. Future Healthcare J. 2021, 8, e188–e194. [Google Scholar] [CrossRef]
- Tagliaferri, S.D.; Angelova, M.; Zhao, X.; Owen, P.J.; Miller, C.T.; Wilkin, T.; Belavy, D.L. Artificial intelligence to improve back pain outcomes and lessons learnt from clinical classification approaches: Three systematic reviews. npj Digit. Med. 2020, 3, 1–16. [Google Scholar] [CrossRef]
- Tran, B.X.; Vu, G.T.; Ha, G.H.; Vuong, Q.-H.; Ho, M.-T.; Vuong, T.-T.; La, V.-P.; Ho, M.-T.; Nghiem, K.-C.P.; Nguyen, H.L.T.; et al. Global Evolution of Research in Artificial Intelligence in Health and Medicine: A Bibliometric Study. J. Clin. Med. 2019, 8, 360. [Google Scholar] [CrossRef]
- Jiang, F.; Jiang, Y.; Zhi, H.; Dong, Y.; Li, H.; Ma, S.; Wang, Y.; Dong, Q.; Shen, H.; Wang, Y. Artificial intelligence in healthcare: Past, present and future. Stroke Vasc. Neurol. 2017, 2, 230–243. [Google Scholar] [CrossRef]
- Javaid, M.; Haleem, A.; Singh, R.P.; Suman, R.; Rab, S. Significance of machine learning in healthcare: Features, pillars and applications. Int. J. Intell. Networks 2022, 3, 58–73. [Google Scholar] [CrossRef]
- Coursera. What Is Machine Learning in Health Care? Applications and Opportunities. 2022. Available online: https://www.coursera.org/articles/machine-learning-in-health-care (accessed on 30 March 2023).
- Hashimy, L.; Treiblmaier, H.; Jain, G. Distributed ledger technology as a catalyst for open innovation adoption among small and medium-sized enterprises. J. High Technol. Manag. Res. 2021, 32, 100405. [Google Scholar] [CrossRef]
- Stampa, K. How Distributed Ledger Technology Will Transform Health Data. Healthcare. 2020. Available online: https://healthcare-digital.com/technology-and-ai/how-distributed-ledger-technology-will-transform-health-data (accessed on 30 March 2023).
- Alruwaili, F.F. Artificial intelligence and multi agent based distributed ledger system for better privacy and security of electronic healthcare records. PeerJ Comput. Sci. 2020, 6, e323. [Google Scholar] [CrossRef] [PubMed]
- Sadiku, M.N.O.; Zhou, Y.; Musa, S.M. Natural Language Processing. Int. J. Adv. Sci. Res. Eng. 2018, 4, 68–70. [Google Scholar] [CrossRef]
- Iroju, O.G.; Olaleke, J.O. A Systematic Review of Natural Language Processing in Healthcare. Int. J. Inf. Technol. Comput. Sci. 2015, 7, 44–50. [Google Scholar] [CrossRef]
- Trunfio, M.; Rossi, S. Advances in Metaverse Investigation: Streams of Research and Future Agenda. Virtual Worlds 2022, 1, 103–129. [Google Scholar] [CrossRef]
- Park, S.-M.; Kim, Y.-G. A metaverse: Taxonomy, components, applications, and open challenges. IEEE Access 2022, 10, 4209–4251. [Google Scholar] [CrossRef]
- Petrigna, L.; Musumeci, G. The Metaverse: A New Challenge for the Healthcare System: A Scoping Review. J. Funct. Morphol. Kinesiol. 2022, 7, 63. [Google Scholar] [CrossRef] [PubMed]
- Thomason, J. MetaHealth-How will the Metaverse Change Health Care? J. Metaverse 2021, 1, 13–16. Available online: https://dergipark.org.tr/en/download/article-file/2167692 (accessed on 31 December 2022).
- Hassani, H.; Silva, E.S. The Role of ChatGPT in Data Science: How AI-Assisted Conversational Interfaces Are Revolutionizing the Field. Big Data and Cogn. Comput. 2023, 7, 62. [Google Scholar] [CrossRef]
- Sallam, M. ChatGPT Utility in Healthcare Education, Research, and Practice: Systematic Review on the Promising Perspectives and Valid Concerns. Healthcare 2023, 11, 887. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.; Sanders, L.; Li, K.; Chow, J.C.L. Chatbot for Health Care and Oncology Applications Using Artificial Intelligence and Machine Learning: Systematic Review. JMIR Cancer 2021, 7, e27850. [Google Scholar] [CrossRef] [PubMed]
- Lin, T.; Wang, Y.; Liu, X.; Qiu, X. A survey of transformers. AI Open 2022, 3, 111–132. [Google Scholar] [CrossRef]
- Li, Y.; Rao, S.; Solares, J.R.A.; Hassaine, A.; Ramakrishnan, R.; Canoy, D.; Zhu, Y.; Rahimi, K.; Salimi-Khorshidi, G. BEHRT: Transformer for Electronic Health Records. Sci. Rep. 2020, 10, 7155. [Google Scholar] [CrossRef] [PubMed]
- Shome, D.; Kar, T.; Mohanty, S.N.; Tiwari, P.; Muhammad, K.; AlTameem, A.; Zhang, Y.; Saudagar, A.K.J. COVID-Transformer: Interpretable COVID-19 Detection Using Vision Transformer for Healthcare. Int. J. Environ. Res. Public Health 2021, 18, 11086. [Google Scholar] [CrossRef]
- He, K.; Gan, C.; Li, Z.; Rekik, I.; Yin, Z.; Ji, W.; Gao, Y.; Wang, Q.; Zhang, J.; Shen, D. Transformers in medical image analysis. Intell. Med. 2023, 3, 59–78. [Google Scholar] [CrossRef]
- Li, Y.; Mamouei, M.; Salimi-Khorshidi, G.; Rao, S.; Hassaine, A.; Canoy, D.; Lukasiewicz, T.; Rahimi, K. Hi-BEHRT: Hierarchical Transformer-Based Model for Accurate Prediction of Clinical Events Using Multimodal Longitudinal Electronic Health Records. IEEE J. Biomed. Health Inform. 2023, 27, 1106–1117. Available online: https://ieeexplore.ieee.org/stamp/stamp.jsp?arnumber=9964038 (accessed on 10 May 2023). [CrossRef]
- Shamshad, F.; Khan, S.; Zamir, S.W.; Khan, M.H.; Hayat, M.; Khan, F.S.; Fu, H. Transformers in medical imaging: A survey. Med. Image Anal. 2023, 102802. [Google Scholar] [CrossRef]
- U.S. Food and Drug Administration (US-FDA). What Is Digital Health. 2020. Available online: https://www.fda.gov/medical-devices/digital-health-center-excellence/what-digital-health (accessed on 11 July 2021).
- Yang, Y.; Siau, K.; Xie, W.; Sun, Y. Smart Health. J. Organ. End User Comput. 2022, 34, 1–14. [Google Scholar] [CrossRef]
- Kumar, K.; Loebinger, M.R.; Ghafur, S. The role of wirelessly observed therapy in improving treatment adherence. Futur. Healthcare J. 2022, 9, 179–182. [Google Scholar] [CrossRef]
- Kumar, A.; Gadag, S.; Nayak, U.Y. The Beginning of a New Era: Artificial Intelligence in Healthcare. Adv. Pharm. Bull. 2020, 11, 414–425. [Google Scholar] [CrossRef]
- Wallace, P. Learning Healthcare System. The Learning Healthcare Project. 2015. Available online: http://www.learninghealthcareproject.org/section/evidence/25/66/dr-paul-wallace-interview (accessed on 10 July 2022).
- Orth, M.; Averina, M.; Chatzipanagiotou, S.; Faure, G.; Haushofer, A.; Kusec, V.; Machado, A.; A Misbah, S.; Oosterhuis, W.; Pulkki, K.; et al. Opinion: Redefining the role of the physician in laboratory medicine in the context of emerging technologies, personalised medicine and patient autonomy (‘4P medicine’). J. Clin. Pathol. 2017, 72, 191–197. [Google Scholar] [CrossRef]
- World Health Organization. Global Strategy on Digital Health 2020–2025. 2021, pp. 7–13. Available online: https://www.who.int/docs/defaultsource/documents/gs4dhdaa2a9f352b0445bafbc79ca799dce4d.pdf (accessed on 10 December 2022).
- Briganti, G.; Le Moine, O. Artificial Intelligence in Medicine: Today and Tomorrow. Front. Med. 2020, 7, 27. [Google Scholar] [CrossRef] [PubMed]
- Hu, J.; Perer, A.; Wang, F. Data driven analytics for personalized healthcare. In Healthcare Information Management Systems; Weaver, C.B.M., Ed.; Springer: Berlin/Heidelberg, Germany, 2016; pp. 529–554. [Google Scholar]
- Dash, S.; Shakyawar, S.K.; Sharma, M.; Kaushik, S. Big data in healthcare: Management, analysis and future prospects. J. Big Data 2019, 6, 54. [Google Scholar] [CrossRef]
- Zhang, C.; Ma, R.; Sun, S.; Li, Y.; Wang, Y.; Yan, Z. Optimizing the Electronic Health Records Through Big Data Analytics: A Knowledge-Based View. IEEE Access 2019, 7, 136223–136231. [Google Scholar] [CrossRef]
- Rawat, S. How Is Big Data Analytics Using AI? 2021. Available online: https://www.analyticssteps.com/blogs/how-big-data-analytics-using-ai (accessed on 11 January 2023).
- Ghosh, P. AI Early Diagnosis Could Save Heart and Cancer Patients. Science Correspondent. BBC News. 2018. Available online: https://www.bbc.com/news/health-42357257 (accessed on 11 July 2021).
- Wang, D.; Khosla, A.; Gargeya, R.; Irshad, H.; Beck, A.H. Deep learning for identifying metastatic breast cancer. arXiv 2016, arXiv:1606.05718. [Google Scholar]
- Esteva, A.; Kuprel, B.; Novoa, R.A.; Ko, J.; Swetter, S.M.; Blau, H.M.; Thrun, S. Dermatologist-level classification of skin cancer with deep neural networks. Nature 2017, 542, 115–118. [Google Scholar] [CrossRef]
- Rajpurkar, P.; Irvin, J.; Zhu, K.; Yang, B.; Mehta, H.; Duan, T.; Ding, D.; Bagul, A.; Langlotz, C.; Shpanskaya, K.; et al. Chexnet: Radiologist-level pneumonia detection on chest x-rays with deep learning. arXiv 2017, arXiv:1711.05225. [Google Scholar]
- Bedi, G.; Carrillo, F.; Cecchi, G.A.; Slezak, D.F.; Sigman, M.; Mota, N.B.; Ribeiro, S.; Javitt, D.C.; Copelli, M.; Corcoran, C.M. Automated analysis of free speech predicts psychosis onset in high-risk youths. NPJ Schitzophrenia 2015, 1, 15030. [Google Scholar] [CrossRef]
- IBM Research. IBM 5 in 5: With AI, Our Words Will Be a Window into Our Mental Health. 2017. Available online: https://www.ibm.com/blogs/research/2017/1/ibm-5-in-5-our-words-will-be-the-windows-to-our-mental-health/ (accessed on 25 December 2022).
- Chou, C.-Y.; Hsu, D.-Y.; Chou, C.-H. Predicting the Onset of Diabetes with Machine Learning Methods. J. Pers. Med. 2023, 13, 406. [Google Scholar] [CrossRef]
- Gudigar, A.; Raghavendra, U.; Nayak, S.; Ooi, C.P.; Chan, W.Y.; Gangavarapu, M.R.; Dharmik, C.; Samanth, J.; Kadri, N.A.; Hasikin, K.; et al. Role of Artificial Intelligence in COVID-19 Detection. Sensors 2021, 21, 8045. [Google Scholar] [CrossRef] [PubMed]
- Khanna, V.V.; Chadaga, K.; Sampathila, N.; Prabhu, S.; Chadaga, R.; Umakanth, S. Diagnosing COVID-19 using artificial intelligence: A comprehensive review. Netw. Model Anal Health Inf. Bioinforma 2022, 11, 25. [Google Scholar] [CrossRef]
- Costa, G.S.S.; Paiva, A.C.; Junior, G.B.; Ferreira, M.M. COVID-19 automatic diagnosis with ct images using the novel transformer architecture. In Proceedings of the 21st Brazilian Symposium on Computing Applied to Health, Rio de Janeiro, Brazil, 15–18 June 2021; pp. 293–301. [Google Scholar]
- van Tulder, G.; Tong, Y.; EMarchiori, E. Multi-view analysis of unregistered medical images using cross-view transformers. In Proceedings of the Medical Image Computing and Computer Assisted Intervention–MICCAI 2021: 24th International Conference, Part III 24, Strasbourg, France, 27 September–1 October 2021; Springer Nature: Basel, Switzerland, 2021; pp. 104–113. [Google Scholar]
- Krishnan, K.S.; Krishnan, K.S. Vision transformer based COVID-19 detection using chest x-rays. In Proceedings of the 2021 6th International Conference on Signal Processing, Computing and Control (ISPCC), Solan, India, 7–9 October 2021; pp. 644–648. [Google Scholar] [CrossRef]
- Wang, S.-H.; Wu, X.; Zhang, Y.-D.; Tang, C.; Zhang, X. Diagnosis of COVID-19 by Wavelet Renyi Entropy and Three-Segment Biogeography-Based Optimization. Int. J. Comput. Intell. Syst. 2020, 13, 1332–1344. [Google Scholar] [CrossRef]
- Gheflati, B.; Rivaz, H. Vision transformer for classification of breast ultrasound images. arXiv 2021, arXiv:211014731. [Google Scholar] [CrossRef]
- Wolterink, J.M.; Mukhopadhyay, A.; Leiner, T.; Vogl, T.J.; Bucher, A.M.; Išgum, I. Generative Adversarial Networks: A Primer for Radiologists. RadioGraphics 2021, 41, 840–857. [Google Scholar] [CrossRef]
- Chuquicusma, M.J.M.; Hussein, S.; Burt, J.; Bagci, U. How to fool radiologists with generative adversarial networks? A visual turing test for lung cancer diagnosis. In Proceedings of the IEEE 15th International Symposium on Biomedical Imaging, Washington, DC, USA, 4–7 April 2018; pp. 240–244. [Google Scholar]
- Arora, A.; Arora, A. Generative adversarial networks and synthetic patient data: Current challenges and future perspectives. Futur. Healthcare J. 2022, 9, 190–193. [Google Scholar] [CrossRef]
- Will ChatGPT transform healthcare? Nat. Med. 2023, 29, 505–506. [CrossRef]
- Kuehn, B.M. More Than One-Third of US Individuals Use the Internet to Self-diagnose. JAMA 2013, 309, 756–757. [Google Scholar] [CrossRef]
- Wang, G.; Badal, A.; Jia, X.; Maltz, J.S.; Mueller, K.; Myers, K.J.; Niu, C.; Vannier, M.; Yan, P.; Yu, Z.; et al. Development of metaverse for intelligent healthcare. Nat. Mach. Intell. 2022, 4, 922–929. [Google Scholar] [CrossRef]
- Nuffield Council on Bioethics. Artificial Intelligence (AI) in Healthcare and Research. Nuffield Council on Bioethics. 2018. Available online: https://www.nuffieldbioethics.org/assets/pdfs/Artificial-Intelligence-AI-in-healthcare-and-research.pdf (accessed on 11 December 2022).
- House of Lords. AI in the UK: Ready, Willing and Able? House of Lords Select Committee on Artificial Intelligence: Report of Session 2017–2019. Authority of the House of Lords. 2018. Available online: https://publications.parliament.uk/pa/ld201719/ldselect/ldai/100/100.pdf (accessed on 16 December 2022).
- Secinaro, S.; Calandra, D.; Secinaro, A.; Muthurangu, V.; Biancone, P. The role of artificial intelligence in healthcare: A structured literature review. BMC Med. Inform. Decis. Mak. 2021, 21, 1–23. [Google Scholar] [CrossRef]
- Oren, O.; Gersh, B.J.; Bhatt, D.L. Artificial intelligence in medical imaging: Switching from radiographic pathological data to clinically meaningful endpoints. Lancet Digit. Health 2020, 2, e486–e488. [Google Scholar] [CrossRef] [PubMed]
- Baig, M.M.; GholamHosseini, H.; Moqeem, A.A.; Mirza, F.; Lindén, M. A Systematic Review of Wearable Patient Monitoring Systems–Current Challenges and Opportunities for Clinical Adoption. J. Med. Syst. 2017, 41, 115. [Google Scholar] [CrossRef]
- Kim, J.; Campbell, A.S.; Wang, J. Wearable non-invasive epidermal glucose sensors: A review. Talanta 2018, 177, 163–170. [Google Scholar] [CrossRef]
- Andrea, M.; Mario, R.P.; Emanuele, F.; Sauro, L.; Filippo, P.; Sara, C.; Lorenzo, S.; Annalisa, C.; Luca, R.; Riccardo, B.; et al. A smart sensing architecture for domestic monitoring: Methodological approach and experimental validation. Sensors 2018, 18, 1–22. [Google Scholar]
- Patel, D.; Tarakji, K.G. Smartwatch diagnosis of atrial fibrillation in patient with embolic stroke of unknown source: A case report. Cardiovasc. Digit. Health J. 2021, 2, 84–87. [Google Scholar] [CrossRef] [PubMed]
- Sükei, E.; Norbury, A.; Perez-Rodriguez, M.M.; Olmos, P.M.; Artés, A. Predicting Emotional States Using Behavioral Markers Derived From Passively Sensed Data: Data-Driven Machine Learning Approach. JMIR mHealth uHealth 2021, 9, e24465. [Google Scholar] [CrossRef] [PubMed]
- Natarajan, A.; Su, H.-W.; Heneghan, C. Assessment of physiological signs associated with COVID-19 measured using wearable devices. NPJ Digit. Med. 2020, 3, 1–8. [Google Scholar] [CrossRef]
- Bogu, G.; Snyder, M. Deep learning-based detection of COVID-19 using wearables data. Deep Learning-Based Detection of COVID-19 Using Wearables Data. MedRxiv 2021. [Google Scholar] [CrossRef]
- Tschopp, J.; L’Huillier, A.G.; Mombelli, M.; Mueller, N.J.; Khanna, N.; Garzoni, C.; Meloni, D.; Papadimitriou-Olivgeris, M.; Neofytos, D.; Hirsch, H.H.; et al. First experience of SARS-CoV-2 infections in solid organ transplant recipients in the Swiss Transplant Cohort Study. Am. J. Transplant. 2020, 20, 2876–2886. [Google Scholar] [CrossRef]
- Yu, M.; Tang, A.; Brown, K.; Bouchakri, R.; St-Onge, P.; Wu, S.; Reeder, J.; Mullie, L.; Chassé, M. Integrating artificial intelligence in bedside care for COVID-19 and future pandemics. BMJ 2021, 375, e068197. [Google Scholar] [CrossRef]
- Garavand, A.; Aslani, N. Metaverse phenomenon and its impact on health: A scoping review. Inform. Med. Unlocked 2022, 32, 101029. [Google Scholar] [CrossRef]
- Ganapathy, K. Telemedicine and Neurological Practice in the COVID-19 Era. Neurol. India 2020, 68, 555–559. [Google Scholar] [CrossRef] [PubMed]
- Lukas, H.; Xu, C.; Yu, Y.; Gao, W. Emerging telemedicine tools for remote COVID-19 diagnosis, monitoring, and management. ACS Nano 2020, 14, 16180–16193. [Google Scholar] [CrossRef] [PubMed]
- Chen, D.; Zhang, R. Exploring Research Trends of Emerging Technologies in Health Metaverse: A Bibliometric Analysis; Elsevier: Amsterdam, The Netherlands, 2022. [Google Scholar] [CrossRef]
- Gadekallu, T.R.; Huynh-The, T.; Wang, W.; Yenduri, G.; Ranaweera, P.; Pham, Q.-V.; da Costa, D.B.; Liyange, M. Blockchain for the metaverse: A review. arXiv 2022, arXiv:2203.09738. [Google Scholar]
- Chengoden, R.; Victor, N.; Huynh-The, T.; Yenduri, G.; Jhaveri, R.H.; Alazab, M.; Bhattacharya, S.; Hegde, P.; Maddikunta, P.K.R.; Gadekallu, T.R. Metaverse for Healthcare: A Survey on Potential Applications, Challenges and Future Directions. IEEE Access 2023, 11, 12765–12795. [Google Scholar] [CrossRef]
- Futurside. Remote Patient Monitoring Devices, Technology, and Its Future. 2022. Available online: https://futurside.com/how-wearable-medical-device-is-reshaping-remote-patient-monitoring-rpm/ (accessed on 11 January 2023).
- Shaik, T.; Tao, X.; Higgins, N.; Li, L.; Gururajan, R.; Zhou, X.; Acharya, U.R. Remote patient monitoring using artificial intelligence: Current state, applications, and challenges. WIREs Data Min. Knowl. Discov. 2023, 13, 1485. [Google Scholar] [CrossRef]
- Bouabida, K.; Malas, K.; Talbot, A.; Desrosiers, M.; Lavoie, F.; Lebouché, B.; Taguemout, M.; Rafie, E.; Lessard, D.; Pomey, M.-P. Remote Patient Monitoring Program for COVID-19 Patients Following Hospital Discharge: A Cross-Sectional Study. Front. Digit. Health 2021, 3, 153. [Google Scholar] [CrossRef]
- Javaid, M.; Haleem, A.; Singh, R.P. ChatGPT for healthcare services: An emerging stage for an innovative perspective. BenchCouncil Trans. Benchmarks Stand. Eval. 2023, 3, 100105. [Google Scholar] [CrossRef]
- Academy of Royal Medical Colleges. Artificial Intelligence in Healthcare. 2019. Available online: https://www.aomrc.org.uk/wpcontent/uploads/2019/01/Artificial_intelligence_in_healthcare_0119.pdf (accessed on 11 January 2023).
- O’mara-Eves, A.; Thomas, J.; McNaught, J.; Miwa, M.; Ananiadou, S. Using text mining for study identification in systematic reviews: A systematic review of current approaches. Syst. Rev. 2015, 4, 5. [Google Scholar] [CrossRef]
- Weissler, E.H.; Naumann, T.; Andersson, T.; Ranganath, R.; Elemento, O.; Luo, Y.; Freitag, D.F.; Benoit, J.; Hughes, M.C.; Khan, F.; et al. The role of machine learning in clinical research: Transforming the future of evidence generation. Trials 2021, 22, 1–15. [Google Scholar] [CrossRef]
- Suh, I.; McKinney, T.; Siu, K.-C. Current Perspective of Metaverse Application in Medical Education, Research and Patient Care. Virtual Worlds 2023, 2, 115–128. [Google Scholar] [CrossRef]
- Khan, R.A.; Jawaid, M.; Khan, A.R.; Sajjad, M. ChatGPT-Reshaping medical education and clinical management. Pak. J. Med. Sci. 2023, 39, 7653. [Google Scholar] [CrossRef] [PubMed]
- Buvailo, A. Artificial Intelligence in Drug Discovery and Biotech: 2022 Recap and Key Trends. 2022. Available online: https://www.biopharmatrend.com/post/615-pharmaceutical-artificial-intelligence-key-developments-in-2022/ (accessed on 31 January 2023).
- Son, W.S. Drug Discovery Enhanced by Artificial Intelligence. Biomed. J. Sci. Tech. Res. 2018, 12, 8936–8938. [Google Scholar] [CrossRef]
- Williams, K.; Bilsland, E.; Sparkes, A.; Aubrey, W.; Young, M.; Soldatova, L.N.; De Grave, K.; Ramon, J.; de Clare, M.; Sirawaraporn, W.; et al. Cheaper faster drug development validated by the repositioning of drugs against neglected tropical diseases. J. R. Soc. Interface 2015, 12, 20141289. [Google Scholar] [CrossRef] [PubMed]
- Mak, K.-K.; Pichika, M.R. Artificial intelligence in drug development: Present status and future prospects. Drug Discov. Today 2019, 24, 773–780. [Google Scholar] [CrossRef]
- Sellwood, M.A. Artificial intelligence in drug discovery. Fut. Sci. 2018, 10, 2025–2028. [Google Scholar] [CrossRef]
- Chen, T.-J. ChatGPT and other artificial intelligence applications speed up scientific writing. J. Chin. Med. Assoc. 2023, 86, 351–353. [Google Scholar] [CrossRef]
- Taecharungroj, V. “What Can ChatGPT Do?” Analyzing Early Reactions to the Innovative AI Chatbot on Twitter. Big Data Cogn. Comput. 2023, 7, 35. [Google Scholar] [CrossRef]
- Paul, D.; Sanap, G.; Shenoy, S.; Kalyane, D.; Kalia, K.; Tekade, R.K. Artificial intelligence in drug discovery and development. Drug Discov. Today 2020, 26, 80–93. [Google Scholar] [CrossRef]
- Álvarez-Machancoses, O.; Fernández-Martínez, J.L. Using artificial intelligence methods to speed up drug discovery. Expert Opin. Drug Discov. 2019, 14, 769–777. [Google Scholar] [CrossRef]
- Dana, D.; Gadhiya, S.V.; St. Surin, L.G.; Li, D.; Naaz, F.; Ali, Q.; Paka, L.; Yamin, M.A.; Narayan, M.; Goldberg, I.D.; et al. Deep Learning in Drug Discovery and Medicine; Scratching the Surface. Molecules 2018, 23, 2384. [Google Scholar] [CrossRef]
- Sharma, A.; Virmani, T.; Pathak, V.; Sharma, A.; Pathak, K.; Kumar, G.; Pathak, D. Artificial Intelligence-Based Data-Driven Strategy to Accelerate Research, Development, and Clinical Trials of COVID Vaccine. Biomed Res Int. 2022, 2022, 7205241. [Google Scholar] [CrossRef] [PubMed]
- Bagabir, S.A.; Ibrahim, N.K.; Ateeq, R.H. COVID-19 and Artificial Intelligence: Genome sequencing, drug development and vaccine discovery. J. Infect. Public Health 2022, 15, 289–296. [Google Scholar] [CrossRef] [PubMed]
- Davenport, T.; Kalakota, R. The potential for artificial intelligence in healthcare. Future Healthcare J. 2019, 6, 94–98. [Google Scholar] [CrossRef]
- Davenport, T.H.; Hongsermeier, T.; Mc Cord, K.A. Using AI to Improve Electronic Health Records. Harvard Business Review. 2018. Available online: https://hbr.org/2018/12/using-ai-to-improve-electronic-health-records (accessed on 28 December 2022).
- Volpp, K.; Mohta, S. Improved Engagement Leads to Better Outcomes, But Better Tools Are Needed. Insights Report. NEJM Catalyst. 2016. Available online: https://catalyst.nejm.org/patient-engagementreport-improved-engagement-leads-better-outcomes-better-toolsneeded (accessed on 15 January 2023).
- Hukunda, B.; Rau, A.; Upadhyay, P. Reimaging Healthcare Opportunities with Artificial Intelligence. Infosys Navigate Your Next. 2018. Available online: https://www.infosys.com/industries/healthcare/featuresopinions/Documents/reimagining-healthcare-opportunities.pdf (accessed on 10 January 2023).
- Anderson, D. Artificial Intelligence and Applications in PM&R. Am. J. Phys. Med. Rehabil. 2019, 98, e128–e129. [Google Scholar] [CrossRef]
- Luxton, D.D.; Riek, L.D. Artificial intelligence and robotics in rehabilitation. In Handbook of Rehabilitation Psychology; Brenner, L.A., Reid-Arndt, S.A., Elliott, T.R., Frank, R.G., Caplan, B., Eds.; American Psychological Association: Washington, DC, USA, 2019; pp. 507–520. [Google Scholar] [CrossRef]
- Goldzweig, C.L.; Orshansky, G.; Paige, N.M.; Towfigh, A.A.; Haggstrom, D.A.; Miake-Lye, I.; Beroes, J.M.; Shekelle, P.G. Electronic Patient Portals: Evidence on Health Outcomes, Satisfaction, Efficiency, and Attitudes. Ann. Intern. Med. 2013, 159, 677–687. [Google Scholar] [CrossRef] [PubMed]
- Sinsky, C.A.; Willard-Grace, R.; Schutzbank, A.M.; Margolius, D.; Bodenheimer, T. In Search of Joy in Practice: A Report of 23 High-Functioning Primary Care Practices. Ann. Fam. Med. 2013, 11, 272–278. [Google Scholar] [CrossRef]
- Sinsky, C.; Colligan, L.; Li, L.; Prgomet, M.; Reynolds, M.S.; Goeders, M.L.; Westbrook, J.; Tutty, M.; Blike, G. Allocation of Physician Time in Ambulatory Practice: A Time and Motion Study in 4 Specialties. Ann. Intern. Med. 2016, 165, 753–760. [Google Scholar] [CrossRef]
- Lin, S.; Khoo, J.; Schillinger, E. Next big thing: Integrating medical scribes into academic medical centres. BMJ Simul. Technol. Enhanc. Learn. 2016, 2, 27–29. [Google Scholar] [CrossRef]
- Choi, C.; Schwarting, W.; DelPreto, J.; Rus, D. Learning Object Grasping for Soft Robot Hands. IEEE Robot. Autom. Lett. 2018, 3, 2370–2377. [Google Scholar] [CrossRef]
- Aggarwal, R.; Ganvir, S.S. Artificial intelligence in physiotherapy. Physiother. J. Indian Assoc. Physiother. 2021, 15, 55. [Google Scholar] [CrossRef]
- Frackiewicz, M. ChatGPT and the Future of Rehabilitation Therapy: An AI-Driven Approach. TS2 Space. 2023. Available online: https://ts2.space/en/chatgpt-and-the-future-of-rehabilitation-therapy-an-ai-driven-approach/ (accessed on 10 May 2023).
- Sharma, A.; Lin, I.W.; Miner, A.S.; Atkins, D.C.; Althoff, T. Human–AI collaboration enables more empathic conversations in text-based peer-to-peer mental health support. Nat. Mach. Intell. 2023, 5, 46–57. [Google Scholar] [CrossRef]
- Chung, E.J.; Lee, B.-H. The effects of flipped learning on learning motivation and attitudes in a class of college physical therapy students. J. Probl. Learn. 2018, 5, 29–36. [Google Scholar] [CrossRef]
- Nadarzynski, T.; Miles, O.; Cowie, A.; Ridge, D. Acceptability of artificial intelligence (AI)-led chatbot services in healthcare: A mixed-methods study. Digit. Health 2019, 5, 2055207619871808. [Google Scholar] [CrossRef]
- Moon, I.; An, Y.; Min, S.; Park, C. Therapeutic Effects of Metaverse Rehabilitation for Cerebral Palsy: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2023, 20, 1578. [Google Scholar] [CrossRef]
- Kidziński, Ł.; Delp, S.; Schwartz, M. Automatic real-time gait event detection in children using deep neural networks. PLoS ONE 2019, 14, e0211466. [Google Scholar] [CrossRef]
- Lambercy, O.; Lehner, R.; Chua, K.; Wee, S.K.; Rajeswaran, D.K.; Kuah, C.W.K.; Ang, W.T.; Liang, P.; Campolo, D.; Hussain, A.; et al. Neurorehabilitation From a Distance: Can Intelligent Technology Support Decentralized Access to Quality Therapy? Front. Robot. 2021, 8, 612415. [Google Scholar] [CrossRef]
- Neibling, B.A.; Jackson, S.M.; Hayward, K.S.; Barker, R.N. Perseverance with technology-facilitated home-based upper limb practice after stroke: A systematic mixed studies review. J. Neuroeng. Rehabil. 2021, 18, 1–26. [Google Scholar] [CrossRef]
- Chidambaram, S.; Maheswaran, Y.; Patel, K.; Sounderajah, V.; Hashimoto, D.A.; Seastedt, K.P.; McGregor, A.H.; Markar, S.R.; Darzi, A. Using Artificial Intelligence-Enhanced Sensing and Wearable Technology in Sports Medicine and Performance Optimisation. Sensors 2022, 22, 6920. [Google Scholar] [CrossRef]
- Gichoya, J.W.; McCoy, L.G.; Celi, L.A.; Ghassemi, M. Equity in essence: A call for operationalising fairness in machine learning for healthcare. BMJ Health Care Inform. 2021, 28, e100289. [Google Scholar] [CrossRef]
- Soliño-Fernandez, D.; Ding, A.; Bayro-Kaiser, E.; Ding, E.L. Willingness to adopt wearable devices with behavioral and economic incentives by health insurance wellness programs: Results of a US cross-sectional survey with multiple consumer health vignettes. BMC Public Health 2019, 19, 1649. [Google Scholar] [CrossRef]
- Gao, Y.; Li, H.; Luo, Y. An empirical study of wearable technology acceptance in healthcare. Ind. Manag. Data Syst. 2015, 115, 1704–1723. [Google Scholar] [CrossRef]
- Tran, V.-T.; Riveros, C.; Ravaud, P. Patients’ views of wearable devices and AI in healthcare: Findings from the ComPaRe e-cohort. NPJ Digit. Med. 2019, 2, 53. [Google Scholar] [CrossRef]
- Wani, S.U.D.; Khan, N.A.; Thakur, G.; Gautam, S.P.; Ali, M.; Alam, P.; Alshehri, S.; Ghoneim, M.M.; Shakeel, F. Utilization of Artificial Intelligence in Disease Prevention: Diagnosis, Treatment, and Implications for the Healthcare Workforce. Healthcare 2022, 10, 608. [Google Scholar] [CrossRef]
- Berg, S. Nudge Theory Explored to Boost Medication Adherence. Chicago: American Medical Association. 2018. Available online: www.ama-assn.org/delivering-care/patient-support-advocacy/nudge-theory-exploredboost-medication-adherence (accessed on 1 January 2023).
- Commins, J. Nurses Say Distractions Cut Bedside Time by 25%. HealthLeaders. 2010. Available online: www.healthleadersmedia.com/nursing/nurses-say-distractions-cut-bedside-time-25 (accessed on 5 January 2023).
- Utermohlen, K. Four Robotic Process Automation (RPA) Applications in the Healthcare Industry. Medium. 2018. Available online: https://medium.com/@karl.utermohlen/4-robotic-process-automation-rpa-applications-inthe-healthcare-industry-4d449b24b613 (accessed on 29 December 2022).
- Corny, J.; Rajkumar, A.; Martin, O.; Dode, X.; Lajonchère, J.-P.; Billuart, O.; Bézie, Y.; Buronfosse, A. A machine learning–based clinical decision support system to identify prescriptions with a high risk of medication error. J. Am. Med. Inform. Assoc. 2020, 27, 1688–1694. [Google Scholar] [CrossRef]
- Ranchon, F.; Chanoine, S.; Lambert-Lacroix, S.; Bosson, J.-L.; Moreau-Gaudry, A.; Bedouch, P. Development of artificial intelligence powered apps and tools for clinical pharmacy services: A systematic review. Int. J. Med. Inform. 2023, 172, 104983. [Google Scholar] [CrossRef]
- Caruana, R.; Lou, Y.; Gehrke, J.; Koch, P.; Sturm, M.; Elhadad, N. Intelligible Models for HealthCare: Predicting Pneumonia Risk and Hospital 30-day Readmission. In Proceedings of the 21th ACM SIGKDD International Conference on Knowledge Discovery and Data Mining, Sydney, Australia, 10 August 2015; ACM Press: Sydney, NSW, Australia, 2015; pp. 1721–1730. [Google Scholar]
- Clement, T.; Kemmerzell, N.; Abdelaal, M.; Amberg, M. XAIR: A Systematic Metareview of Explainable AI (XAI) Aligned to the Software Development Process. Mach. Learn. Knowl. Extr. 2023, 5, 78–108. [Google Scholar] [CrossRef]
- Tiwari, R. Explainable AI (XAI) and its Applications in Building Trust and Understanding in AI Decision Making. International J. Sci. Res. Eng. Manag. 2023, 7, 1–13. [Google Scholar] [CrossRef]
- Alvarez-Melis, D.; Jaakkola, T.S. Towards robust interpretability with self-explaining neural networks. arXiv 2018, arXiv:1806.07538. [Google Scholar] [CrossRef]
- Giuste, F.; Shi, W.; Zhu, Y.; Naren, T.; Isgut, M.; Sha, Y.; Tong, L.; Gupte, M.; Wang, M.D. Explainable Artificial Intelligence Methods in Combating Pandemics: A Systematic Review. IEEE Rev. Biomed. Eng. 2022, 16, 5–21. [Google Scholar] [CrossRef]
- Jadhav, S.; Deng, G.; Zawin, M.; Kaufman, A.E. COVID-view: Diagnosis of COVID-19 using Chest CT. IEEE Trans. Vis. Comput. Graph. 2021, 28, 227–237. [Google Scholar] [CrossRef]
- Dilsizian, S.E.; Siegel, E.L. Artificial Intelligence in Medicine and Cardiac Imaging: Harnessing Big Data and Advanced Computing to Provide Personalized Medical Diagnosis and Treatment. Curr. Cardiol. Rep. 2013, 16, 1–8. [Google Scholar] [CrossRef]
- Sunarti, S.; Rahman, F.F.; Naufal, M.; Risky, M.; Febriyanto, K.; Masnina, R. Artificial intelligence in healthcare: Opportunities and risk for future. Gac. Sanit. 2021, 35, S67–S70. [Google Scholar] [CrossRef]
- Farhud, D.D.; Zokaei, S. Ethical Issues of Artificial Intelligence in Medicine and Healthcare. Iran. J. Public Health 2021, 50, i–v. [Google Scholar] [CrossRef]
- Reddy, S.; Allan, S.; Coghlan, S.; Cooper, P. A governance model for the application of AI in health care. J. Am. Med. Inform. Assoc. 2019, 27, 491–497. [Google Scholar] [CrossRef]
- World Health Organization. Ethics and Governance of Artificial Intelligence for Health: WHO Guidance; World Health Organization: Geneva, Switzerland, 2021; p. 150. Available online: https://www.who.int/publications/i/item/9789240029200 (accessed on 29 December 2022).
- Marwaha, J.S.; Landman, A.B.; Brat, G.A.; Dunn, T.; Gordon, W.J. Deploying digital health tools within large, complex health systems: Key considerations for adoption and implementation. NPJ Digit. Med. 2022, 5, 13. [Google Scholar] [CrossRef]
- Liao, F.; Adelaine, S.; Afshar, M.; Patterson, B.W. Governance of Clinical AI applications to facilitate safe and equitable deployment in a large health system: Key elements and early successes. Front. Digit. Health 2022, 4, 931439. [Google Scholar] [CrossRef]
- Forcier, M.B.; Gallois, H.; Mullan, S.; Joly, Y. Integrating artificial intelligence into health care through data access: Can the GDPR act as a beacon for policymakers? J. Law Biosci. 2019, 6, 317–335. [Google Scholar] [CrossRef]
- Schaake, M. The European Commission’s Artificial Intelligence Act. Standford Univeristy Human-Centered Artificial Intelligence (BHAI), Standford, Canada. 2021. Available online: https://hai.stanford.edu/sites/default/files/2021-06/HAI_Issue-Brief_The-European-Commissions-Artificial-Intelligence-Act.pdf (accessed on 5 May 2023).
- Brown, R. Challenges to Successful AI Implementation in Healthcare. Data Science Central. 2022. Available online: https://www.datasciencecentral.com/challenges-to-successful-ai-implementation-in-healthcare/ (accessed on 30 March 2023).
- Tachkov, K.; Zemplenyi, A.; Kamusheva, M.; Dimitrova, M.; Siirtola, P.; Pontén, J.; Nemeth, B.; Kalo, Z.; Petrova, G. Barriers to Use Artificial Intelligence Methodologies in Health Technology Assessment in Central and East European Countries. Front. Public Health 2022, 10, 921226. [Google Scholar] [CrossRef]
- Marcus, G. Deep learning: A Critical Appraisal. arXiv 2018. Available online: https://arxiv.org/abs/1801.00631 (accessed on 1 May 2019).
- Kelly, C.J.; Karthikesalingam, A.; Suleyman, M.; Corrado, G.; King, D. Key challenges for delivering clinical impact with artificial intelligence. BMC Med. 2019, 17, 195. [Google Scholar] [CrossRef]
- Choudhury, A.; Asan, O. Impact of accountability, training, and human factors on the use of artificial intelligence in healthcare: Exploring the perceptions of healthcare practitioners in the US. Hum. Factors Healcare 2022, 2, 100021. [Google Scholar] [CrossRef]
- Joshi, N. 5 AI Implementation Challenges in Healthcare. 2020. Available online: https://www.allerin.com/blog/5-ai-implementation-challenges-in-healthcare (accessed on 31 March 2023).
- Khan, B.; Fatima, H.; Qureshi, A.; Kumar, S.; Hanan, A.; Hussain, J.; Abdullah, S. Drawbacks of Artificial Intelligence and Their Potential Solutions in the Healthcare Sector. Biomed. Mater. Devices 2023, 1–8. [Google Scholar] [CrossRef]
- Baowaly, M.K.; Lin, C.-C.; Liu, C.-L.; Chen, K.-T. Synthesizing electronic health records using improved generative adversarial networks. J. Am. Med. Inform. Assoc. 2018, 26, 228–241. [Google Scholar] [CrossRef]
- Neill, D.B. Using artifcial intelligence to improve hospital inpatient care. IEEE Intell. Syst. 2013, 28, 92–95. [Google Scholar] [CrossRef]
- Fernandes, M.; Vieira, S.M.; Leite, F.; Palos, C.; Finkelstein, S.; Sousa, J.M. Clinical Decision Support Systems for Triage in the Emergency Department using Intelligent Systems: A Review. Artif. Intell. Med. 2020, 102, 101762. [Google Scholar] [CrossRef]
- Gama, F.; Tyskbo, D.; Nygren, J.; Barlow, J.; Reed, J.; Svedberg, P. Implementation Frameworks for Artificial Intelligence Translation Into Health Care Practice: Scoping Review. J. Med. Internet Res. 2022, 24, e32215. [Google Scholar] [CrossRef]
- Wolff, J.; Pauling, J.; Keck, A.; Baumbach, J. Systematic Review of Economic Impact Studies of Artificial Intelligence in Health Care. J. Med. Internet Res. 2020, 22, e16866. [Google Scholar] [CrossRef]
- Alami, H.; Lehoux, P.; Denis, J.L.; Motulsky, A.; Petitgand, C.; Savoldelli, M.; Rouquet, R.; Gagnon, M.P.; Roy, D.; Fortin, J.P. Organizational readiness for artifcial intelligence in health care: Insights for decision-making and practice. J. Health Organ. Manag. 2021, 35, 106–114. [Google Scholar] [CrossRef]
- Duggal, N. Advantages and Disadvantages of Artificial Intelligence. Simplilearn. 2023. Available online: https://www.simplilearn.com/advantages-and-disadvantages-of-artificial-intelligence-article (accessed on 11 May 2023).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).