Prognostic Role of Clinical Features of Moderate Forms of COVID-19 Requiring Hospitalization
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Peñalvo, J.L.; Mertens, E.; Ademović, E.; Akgun, S.; Baltazar, A.L.; Buonfrate, D.; Čoklo, M.; Devleesschauwer, B.; Diaz Valencia, P.A.; Fernandes, J.C.; et al. Unravelling Data for Rapid Evidence-Based Response to COVID-19: A Summary of the UnCoVer Protocol. BMJ Open 2021, 11, e055630. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.; Khan, H.; Khan, S.; Nawaz, M. Epidemiological and clinical characteristics of coronavirus disease (COVID-19) cases at a screening clinic during the early outbreak period: A single-centre study. J. Med. Microbiol. 2020, 69, 1114–1123. [Google Scholar] [CrossRef] [PubMed]
- Lian, J.; Jin, X.; Hao, S.; Jia, H.; Cai, H.; Zhang, X.; Hu, J.; Zheng, L.; Wang, X.; Zhang, S.; et al. Epidemiological, clinical, and virological characteristics of 465 hospitalized cases of coronavirus disease 2019 (COVID-19) from Zhejiang province in China. Influenza Other Respi. Viruses 2020, 14, 564–574. [Google Scholar] [CrossRef] [PubMed]
- Tharakan, S.; Nomoto, K.; Miyashita, S.; Ishikawa, K. Body temperature correlates with mortality in COVID-19 patients. Crit. Care 2020, 24, 298. [Google Scholar] [CrossRef]
- Lai, F.; Li, X.; Liu, T.; Wang, X.; Wang, Q.; Chen, S.; Wei, S.; Xiong, Y.; Hou, Q.; Zeng, X.; et al. Optimal diagnostic fever thresholds using non-contact infrared thermometers under COVID-19. Front. Public Health 2022, 10, 985553. [Google Scholar] [CrossRef]
- Grünebaum, A.; Chervenak, F.A.; McCullough, L.B.; Dudenhausen, J.W.; Bornstein, E.; Mackowiak, P.A. How fever is defined in COVID-19 publications: A disturbing lack of precision. J. Perinat. Med. 2021, 49, 255–261. [Google Scholar] [CrossRef]
- Liang, W.; Liang, H.; Ou, L.; Chen, B.; Chen, A.; Li, C.; Li, Y.; Guan, W.; Sang, L.; Lu, J.; et al. Development and Validation of a Clinical Risk Score to Predict the Occurrence of Critical Illness in Hospitalized Patients With COVID-19. JAMA Intern. Med. 2020, 180, 1081. [Google Scholar] [CrossRef]
- Mudatsir, M.; Fajar, J.K.; Wulandari, L.; Soegiarto, G.; Ilmawan, M.; Purnamasari, Y.; Mahdi, B.A.; Jayanto, G.D.; Suhendra, S.; Setianingsih, Y.A.; et al. Predictors of COVID-19 severity: A systematic review and meta-analysis. F1000Research 2021, 9, 1107. [Google Scholar] [CrossRef]
- Lopez-Leon, S.; Wegman-Ostrosky, T.; Perelman, C.; Sepulveda, R.; Rebolledo, P.A.; Cuapio, A.; Villapol, S. More than 50 long-term effects of COVID-19: A systematic review and meta-analysis. Sci. Rep. 2021, 11, 16144. [Google Scholar] [CrossRef]
- Misra, S.; Kolappa, K.; Prasad, M.; Radhakrishnan, D.; Thakur, K.T.; Solomon, T.; Michael, B.D.; Winkler, A.S.; Beghi, E.; Guekht, A.; et al. Frequency of Neurologic Manifestations in COVID-19: A Systematic Review and Meta-analysis. Neurology 2021, 97, e2269–e2281. [Google Scholar] [CrossRef]
- Islam, M.A.; Cavestro, C.; Alam, S.S.; Kundu, S.; Kamal, M.A.; Reza, F. Encephalitis in Patients with COVID-19: A Systematic Evidence-Based Analysis. Cells 2022, 11, 2575. [Google Scholar] [CrossRef]
- Islam, M.A.; Alam, S.S.; Kundu, S.; Hossan, T.; Kamal, M.A.; Cavestro, C. Prevalence of Headache in Patients With Coronavirus Disease 2019 (COVID-19): A Systematic Review and Meta-Analysis of 14,275 Patients. Front. Neurol. 2020, 11, 562634. [Google Scholar] [CrossRef]
- Gonzalez-Martinez, A.; Fanjul, V.; Ramos, C.; Serrano Ballesteros, J.; Bustamante, M.; Villa Martí, A.; Álvarez, C.; García del Álamo, Y.; Vivancos, J.; Gago-Veiga, A.B. Headache during SARS-CoV-2 infection as an early symptom associated with a more benign course of disease: A case–control study. Eur. J. Neurol. 2021, 28, 3426–3436. [Google Scholar] [CrossRef]
- Fernández-de-las-Peñas, C.; Gómez-Mayordomo, V.; Cuadrado, M.L.; Palacios-Ceña, D.; Florencio, L.L.; Guerrero, A.L.; García-Azorín, D.; Hernández-Barrera, V.; Arendt-Nielsen, L. The presence of headache at onset in SARS-CoV-2 infection is associated with long-term post-COVID headache and fatigue: A case-control study. Cephalalgia 2021, 41, 1332–1341. [Google Scholar] [CrossRef]
- Uygun, Ö.; Ertaş, M.; Ekizoğlu, E.; Bolay, H.; Özge, A.; Kocasoy Orhan, E.; Çağatay, A.A.; Baykan, B. Headache characteristics in COVID-19 pandemic-a survey study. J. Headache Pain 2020, 21, 121. [Google Scholar] [CrossRef]
- Caronna, E.; Pozo-Rosich, P. Headache as a Symptom of COVID-19: Narrative Review of 1-Year Research. Curr. Pain Headache Rep. 2021, 25, 73. [Google Scholar] [CrossRef]
- Togha, M.; Hashemi, S.M.; Yamani, N.; Martami, F.; Salami, Z. A Review on Headaches Due to COVID-19 Infection. Front. Neurol. 2022, 13, 942956. [Google Scholar] [CrossRef]
- Göbel, C.H.; Heinze, A.; Karstedt, S.; Morscheck, M.; Tashiro, L.; Cirkel, A.; Hamid, Q.; Halwani, R.; Temsah, M.-H.; Ziemann, M.; et al. Clinical characteristics of headache after vaccination against COVID-19 (coronavirus SARS-CoV-2) with the BNT162b2 mRNA vaccine: A multicentre observational cohort study. Brain Commun. 2021, 3, fcab169. [Google Scholar] [CrossRef]
- Eliezer, M.; Hautefort, C.; Hamel, A.-L.; Verillaud, B.; Herman, P.; Houdart, E.; Eloit, C. Sudden and Complete Olfactory Loss of Function as a Possible Symptom of COVID-19. JAMA Otolaryngol. Head Neck Surg. 2020, 146, 674. [Google Scholar] [CrossRef]
- Lechien, J.R.; Chiesa-Estomba, C.M.; De Siati, D.R.; Horoi, M.; Le Bon, S.D.; Rodriguez, A.; Dequanter, D.; Blecic, S.; El Afia, F.; Distinguin, L.; et al. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): A multicenter European study. Eur. Arch. Oto-Rhino-Laryngol. 2020, 277, 2251–2261. [Google Scholar] [CrossRef]
- Lee, M.-H.; Perl, D.P.; Nair, G.; Li, W.; Maric, D.; Murray, H.; Dodd, S.J.; Koretsky, A.P.; Watts, J.A.; Cheung, V.; et al. Microvascular Injury in the Brains of Patients with COVID-19. N. Engl. J. Med. 2021, 384, 481–483. [Google Scholar] [CrossRef] [PubMed]
- Brann, D.H.; Tsukahara, T.; Weinreb, C.; Lipovsek, M.; Van den Berge, K.; Gong, B.; Chance, R.; Macaulay, I.C.; Chou, H.-J.; Fletcher, R.B.; et al. Non-neuronal expression of SARS-CoV-2 entry genes in the olfactory system suggests mechanisms underlying COVID-19-associated anosmia. Sci. Adv. 2020, 6, eabc5801. [Google Scholar] [CrossRef] [PubMed]
- Brandão Neto, D.; Fornazieri, M.A.; Dib, C.; Di Francesco, R.C.; Doty, R.L.; Voegels, R.L.; de Rezende Pinna, F. Chemosensory Dysfunction in COVID-19: Prevalences, Recovery Rates, and Clinical Associations on a Large Brazilian Sample. Otolaryngol.-Head Neck Surg. 2021, 164, 512–518. [Google Scholar] [CrossRef] [PubMed]
- Favas, T.T.; Dev, P.; Chaurasia, R.N.; Chakravarty, K.; Mishra, R.; Joshi, D.; Mishra, V.N.; Kumar, A.; Singh, V.K.; Pandey, M.; et al. Neurological manifestations of COVID-19: A systematic review and meta-analysis of proportions. Neurol. Sci. 2020, 41, 3437–3470. [Google Scholar] [CrossRef] [PubMed]
- Porta-Etessam, J.; Núñez-Gil, I.J.; González García, N.; Fernandez-Perez, C.; Viana-Llamas, M.C.; Eid, C.M.; Romero, R.; Molina, M.; Uribarri, A.; Becerra-Muñoz, V.M.; et al. COVID-19 anosmia and gustatory symptoms as a prognosis factor: A subanalysis of the HOPE COVID-19 (Health Outcome Predictive Evaluation for COVID-19) registry. Infection 2021, 49, 677–684. [Google Scholar] [CrossRef]
- Mercier, J.; Osman, M.; Bouiller, K.; Tipirdamaz, C.; Gendrin, V.; Chirouze, C.; Lepiller, Q.; Bouvier, E.; Royer, P.; Pierron, A.; et al. Olfactory dysfunction in COVID-19, new insights from a cohort of 353 patients: The ANOSVID study. J. Med. Virol. 2022, 94, 4762–4775. [Google Scholar] [CrossRef]
- Hoong, C.W.S.; Amin, M.N.M.E.; Tan, T.C.; Lee, J.E. Viral arthralgia a new manifestation of COVID-19 infection? A cohort study of COVID-19-associated musculoskeletal symptoms. Int. J. Infect. Dis. 2021, 104, 363–369. [Google Scholar] [CrossRef]
- Jiang, X.; Coffee, M.; Bari, A.; Wang, J.; Jiang, X.; Huang, J.; Shi, J.; Dai, J.; Cai, J.; Zhang, T.; et al. Towards an Artificial Intelligence Framework for Data-Driven Prediction of Coronavirus Clinical Severity. Comput. Mater. Contin. 2020, 62, 537–551. [Google Scholar] [CrossRef]
- Lippi, G.; Wong, J.; Henry, B.M. Myalgia may not be associated with severity of coronavirus disease 2019 (COVID-19). World J. Emerg. Med. 2020, 11, 193. [Google Scholar] [CrossRef]
- Herndon, C.M.; Nguyen, V. Patterns of Viral Arthropathy and Myalgia Following COVID-19: A Cross-Sectional National Survey. JPR 2022, 15, 3069–3077. [Google Scholar] [CrossRef]
- Pal, A.; Roongta, R.; Mondal, S.; Sinha, D.; Sinhamahapatra, P.; Ghosh, A.; Chattopadhyay, A. Does post-COVID reactive arthritis exist? Experience of a tertiary care centre with a review of the literature. Reumatol. Clínica 2023, 19, 67–73. [Google Scholar] [CrossRef]
- Vojdani, A.; Vojdani, E.; Kharrazian, D. Reaction of Human Monoclonal Antibodies to SARS-CoV-2 Proteins With Tissue Antigens: Implications for Autoimmune Diseases. Front. Immunol. 2021, 11, 617089. [Google Scholar] [CrossRef]
- Anaya, J.-M.; Rojas, M.; Salinas, M.L.; Rodríguez, Y.; Roa, G.; Lozano, M.; Rodríguez-Jiménez, M.; Montoya, N.; Zapata, E.; Monsalve, D.M.; et al. Post-COVID syndrome. A case series and comprehensive review. Autoimmun. Rev. 2021, 20, 102947. [Google Scholar] [CrossRef]
- Guan, W.; Ni, Z.; Hu, Y.; Liang, W.; Ou, C.; He, J.; Liu, L.; Shan, H.; Lei, C.; Hui, D.S.C.; et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef]
- Hoffmann, M.; Kleine-Weber, H.; Schroeder, S.; Krüger, N.; Herrler, T.; Erichsen, S.; Schiergens, T.S.; Herrler, G.; Wu, N.-H.; Nitsche, A.; et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell 2020, 181, 271–280.e8. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.; Liu, P.; Shi, X.L.; Chu, Y.L.; Zhang, J.; Xia, J.; Gao, X.Z.; Qu, T.; Wang, M.Y. SARS-CoV-2 induced diarrhoea as onset symptom in patient with COVID-19. Gut 2020, 69, 1143–1144. [Google Scholar] [CrossRef]
- Wang, M.-K.; Yue, H.-Y.; Cai, J.; Zhai, Y.-J.; Peng, J.-H.; Hui, J.-F.; Hou, D.-Y.; Li, W.-P.; Yang, J.-S. COVID-19 and the digestive system: A comprehensive review. WJCC 2021, 9, 3796–3813. [Google Scholar] [CrossRef]
- Li, K.; Wu, J.; Wu, F.; Guo, D.; Chen, L.; Fang, Z.; Li, C. The Clinical and Chest CT Features Associated With Severe and Critical COVID-19 Pneumonia. Investig. Radiol. 2020, 55, 327–331. [Google Scholar] [CrossRef] [PubMed]
- Hedayat, B.; Hosseini, K. Chest pain and high troponin level without significant respiratory symptoms in young patients with COVID-19. Casp. J. Intern. Med. 2020, 11 (Suppl. S1), 561. [Google Scholar] [CrossRef]
- Puntmann, V.O.; Carerj, M.L.; Wieters, I.; Fahim, M.; Arendt, C.; Hoffmann, J.; Shchendrygina, A.; Escher, F.; Vasa-Nicotera, M.; Zeiher, A.M.; et al. Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020, 5, 1265. [Google Scholar] [CrossRef]
- Filippetti, L.; Pace, N.; Marie, P.Y. Cardiac Involvement After Recovering From COVID-19. JAMA Cardiol. 2021, 6, 243. [Google Scholar] [CrossRef] [PubMed]
- Ammirati, E.; Lupi, L.; Palazzini, M.; Hendren, N.S.; Grodin, J.L.; Cannistraci, C.V.; Schmidt, M.; Hekimian, G.; Peretto, G.; Bochaton, T.; et al. Prevalence, Characteristics, and Outcomes of COVID-19–Associated Acute Myocarditis. Circulation 2022, 145, 1123–1139. [Google Scholar]
- Guo, T.; Fan, Y.; Chen, M.; Wu, X.; Zhang, L.; He, T.; Wang, H.; Wan, J.; Wang, X.; Lu, Z. Cardiovascular Implications of Fatal Outcomes of Patients With Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020, 5, 811. [Google Scholar] [CrossRef]
- Jia, J.L.; Kamceva, M.; Rao, S.A.; Linos, E. Cutaneous manifestations of COVID-19: A preliminary review. J. Am. Acad. Dermatol. 2020, 83, 687–690. [Google Scholar] [CrossRef]
- Bartleson, J.M.; Radenkovic, D.; Covarrubias, A.J.; Furman, D.; Winer, D.A.; Verdin, E. SARS-CoV-2, COVID-19 and the aging immune system. Nat. Aging 2021, 1, 769–782. [Google Scholar] [CrossRef]
- Wang, L.; He, W.; Yu, X.; Hu, D.; Bao, M.; Liu, H.; Zhou, J.; Jiang, H. Coronavirus disease 2019 in elderly patients: Characteristics and prognostic factors based on 4-week follow-up. J. Infect. 2020, 80, 639–645. [Google Scholar] [CrossRef]
- Herrera-Esposito, D.; de los Campos, G. Age-specific rate of severe and critical SARS-CoV-2 infections estimated with multi-country seroprevalence studies. BMC Infect. Dis. 2022, 22, 311. [Google Scholar] [CrossRef]
| Clinical Feature | Present at Admission |
|---|---|
| cough | 312 (69%) |
| shortness of breath | 250 (55.3%) |
| fatigue | 219 (48.4%) |
| fever | 203 (44.9%) |
| myalgia | 96 (21.2%) |
| headache | 95 (21%) |
| anorexia | 73 (16.1%) |
| chest pain | 62 (13.7%) |
| diarrhea | 51 (11.2%) |
| smell loss | 51 (11.2%) |
| nausea | 50 (11%) |
| arthralgia | 45 (9.9%) |
| sore throat | 41 (9%) |
| abdominal pain | 24 (5.3%) |
| taste loss | 21 (4.6%) |
| confusion | 20 (4.4%) |
| nasal discharge | 15 (3.3%) |
| convulsions | 3 (0.6%) |
| wheezing | 3 (0.6%) |
| skin rash | 0 (0%) |
| Recovered | Transferred | Deceased | p Value (Chi Square) | ||
|---|---|---|---|---|---|
| confusion | absent | 350 (77.7%) | 41 (9.1%) | 39 (8.6%) | <0.001 |
| present | 8 (1.7%) | 6 (1.3%) | 6 (1.3%) | ||
| shortness of breath | absent | 176 (39%) | 6 (1.3%) | 19 (4.2%) | <0.001 |
| present | 183 (40.6%) | 41 (9.1%) | 26 (5.7%) |
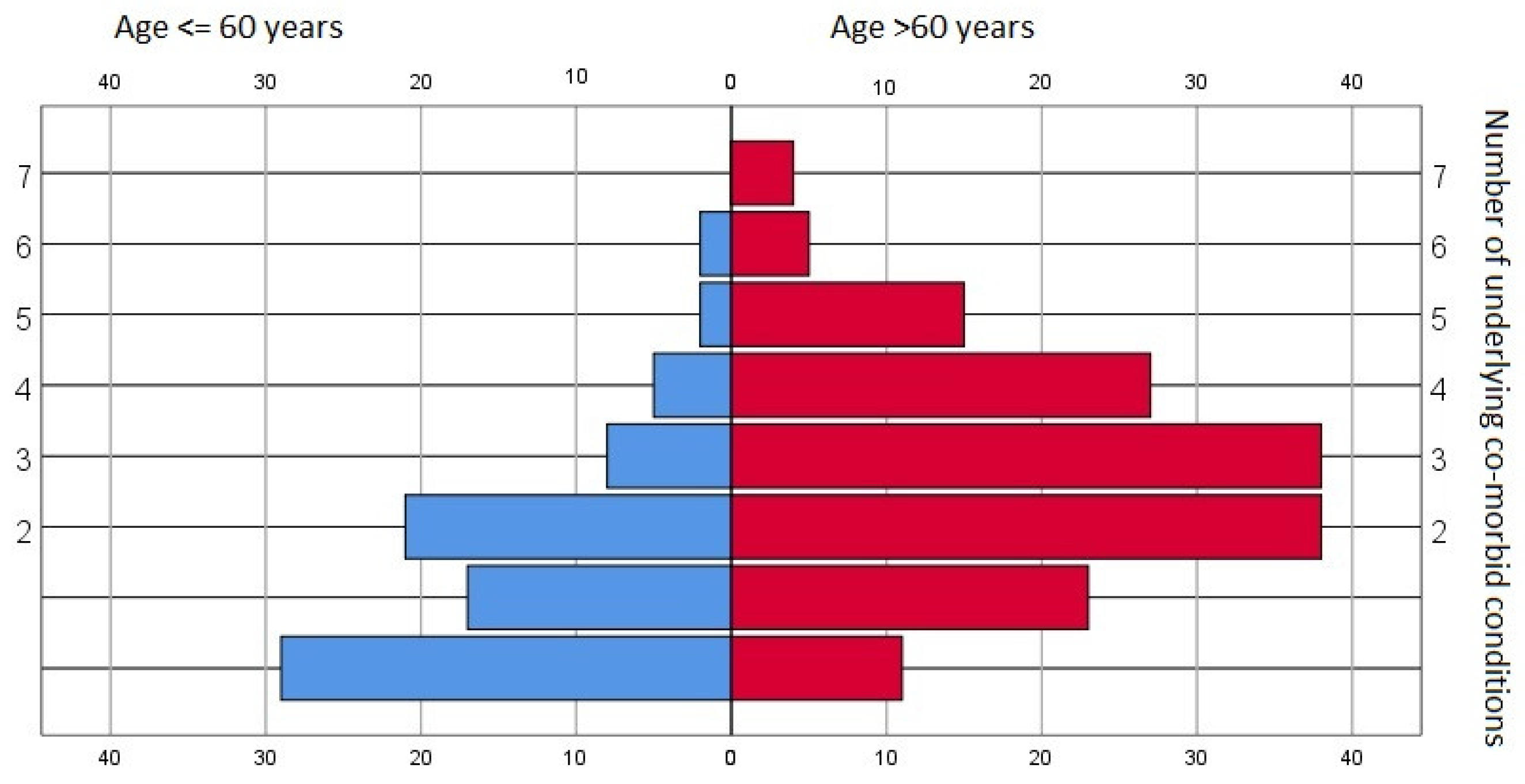
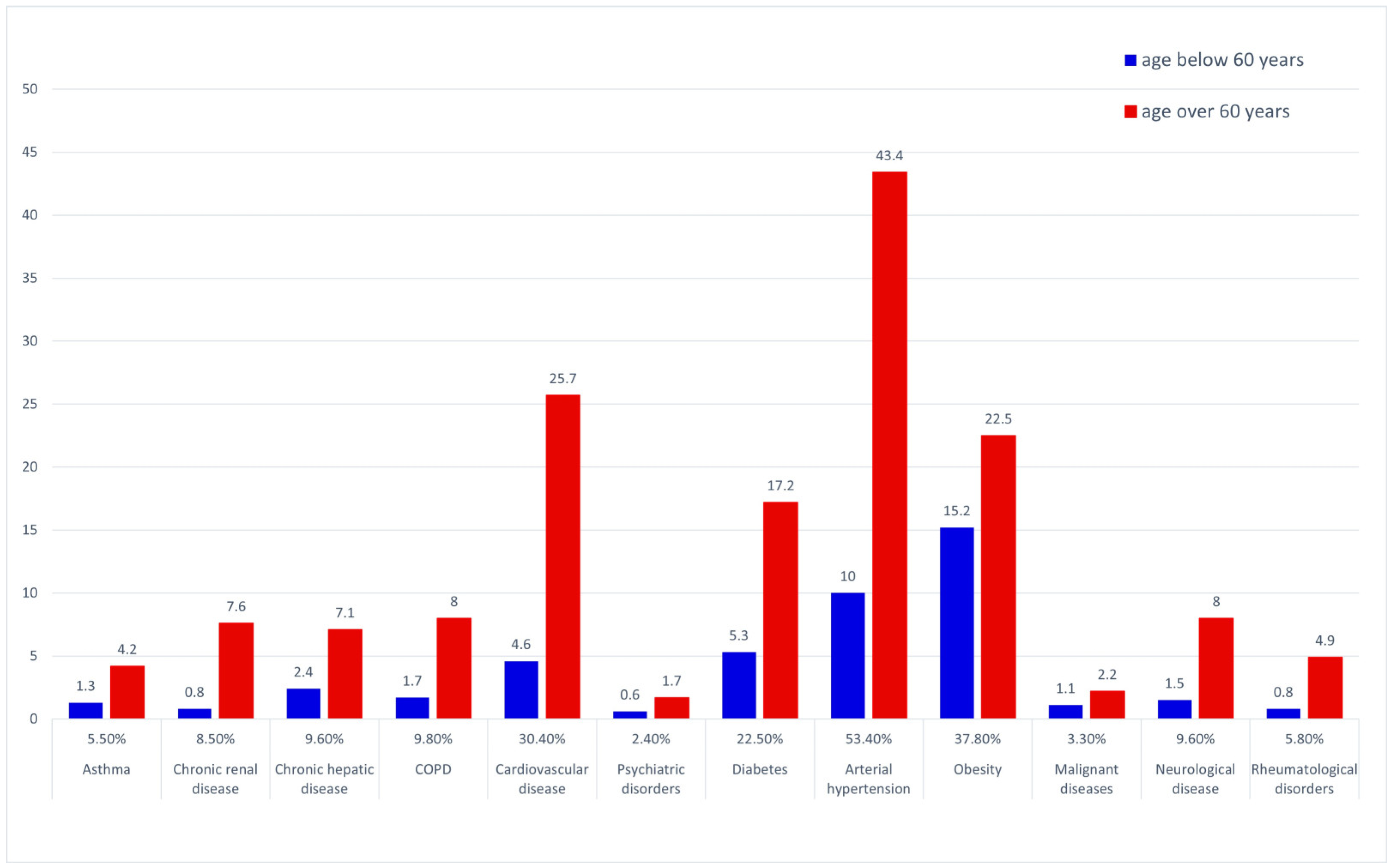
| Age ≤ 60 Years | Age > 60 Years | Age ≤ 60 Years (%) | Age > 60 Years (%) | p Value (Chi Square) | |
|---|---|---|---|---|---|
| cough | 119 | 190 | 67.2 | 70.1 | |
| shortness of breath | 76 | 174 | 42.9 | 64.2 | <0.001 * |
| fatigue | 72 | 146 | 40.6 | 54.4 | 0.005 |
| fever | 90 | 111 | 50.8 | 40.9 | 0.025 |
| myalgia | 41 | 53 | 23.1 | 19.7 | |
| headache | 42 | 52 | 23.7 | 19.3 | |
| anorexia | 24 | 48 | 13.6 | 17.8 | |
| chest pain | 22 | 39 | 12.4 | 14.4 | |
| diarrhea | 17 | 34 | 9.6 | 12.5 | |
| nausea | 19 | 31 | 10.7 | 11.5 | |
| arthralgia | 17 | 28 | 9.6 | 10.3 | |
| smell loss | 30 | 20 | 17 | 7.5 | 0.002 |
| confusion | 4 | 16 | 2.2 | 5.9 | |
| abdominal pain | 9 | 14 | 5 | 5.1 | |
| sore throat | 27 | 13 | 15.2 | 4.8 | <0.001 * |
| taste loss | 13 | 8 | 7.7 | 3.1 | 0.028 |
| runny nose | 7 | 8 | 3.9 | 2.9 | |
| wheezing | 1 | 2 | 0.5 | 0.7 | |
| convulsions | 2 | 1 | 1.1 | 0.3 |
| Odds Ratio | 95% IC | p Value | |
|---|---|---|---|
| confusion | 5.73 | 2.17–15.17 | 0.0001 |
| shortness of breath | 2.08 | 1.22–3.53 | 0.007 |
| age > 60 years | 3.29 | 1.81–5.97 | 0.0001 |
| Shortness of Breath Absent | Present | p Value (Chi Square) | ||
|---|---|---|---|---|
| Arterial hypertension | absent | 117 (26.1%) | 91 (20.3%) | <0.001 * |
| present | 83 (18.5%) | 157 (35%) | ||
| Cardiovascular disease | absent | 156 (34.8%) | 156 (34.8%) | 0.001 * |
| present | 45 (10%) | 93 (20.7%) | ||
| COPD | absent | 189 (42.1%) | 217 (48.4%) | 0.016 |
| present | 12 (2.6%) | 32 (7.1%) | ||
| Confusion absent | present | p value (chi square) | ||
| Neurological disease | absent | 391 (87.2%) | 11 (2.4%) | <0.001 * |
| present | 35 (7.8) | 8 (1.7%) | ||
| Hepatic disease | absent | 391 (87.2%) | 14 (3.1%) | 0.001 * |
| present | 37 (8.2%) | 6 (1.3%) | ||
| Cardiovascular disease | absent | 302 (67.4%) | 9 (2%) | 0.024 |
| present | 127 (28.3%) | 11 (2.4%) | ||
| Arterial hypertension | absent | 203 (45.3%) | 4 (0.8%) | 0.02 |
| present | 224 (50%) | 16 (3.5%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Trofor, A.C.; Cernomaz, A.T.; Lotrean, L.M.; Crișan-Dabija, R.A.; Penalvo, J.L.; Melinte, O.E.; Popa, D.R.; Man, M.A. Prognostic Role of Clinical Features of Moderate Forms of COVID-19 Requiring Hospitalization. J. Pers. Med. 2023, 13, 900. https://doi.org/10.3390/jpm13060900
Trofor AC, Cernomaz AT, Lotrean LM, Crișan-Dabija RA, Penalvo JL, Melinte OE, Popa DR, Man MA. Prognostic Role of Clinical Features of Moderate Forms of COVID-19 Requiring Hospitalization. Journal of Personalized Medicine. 2023; 13(6):900. https://doi.org/10.3390/jpm13060900
Chicago/Turabian StyleTrofor, Antigona Carmen, Andrei Tudor Cernomaz, Lucia Maria Lotrean, Radu Adrian Crișan-Dabija, Jose L. Penalvo, Oana Elena Melinte, Daniela Robu Popa, and Milena Adina Man. 2023. "Prognostic Role of Clinical Features of Moderate Forms of COVID-19 Requiring Hospitalization" Journal of Personalized Medicine 13, no. 6: 900. https://doi.org/10.3390/jpm13060900
APA StyleTrofor, A. C., Cernomaz, A. T., Lotrean, L. M., Crișan-Dabija, R. A., Penalvo, J. L., Melinte, O. E., Popa, D. R., & Man, M. A. (2023). Prognostic Role of Clinical Features of Moderate Forms of COVID-19 Requiring Hospitalization. Journal of Personalized Medicine, 13(6), 900. https://doi.org/10.3390/jpm13060900









