How Relevant Is the Parallax Effect on Low Centered Pelvic Radiographs in Total Hip Arthroplasty
Abstract
1. Introduction
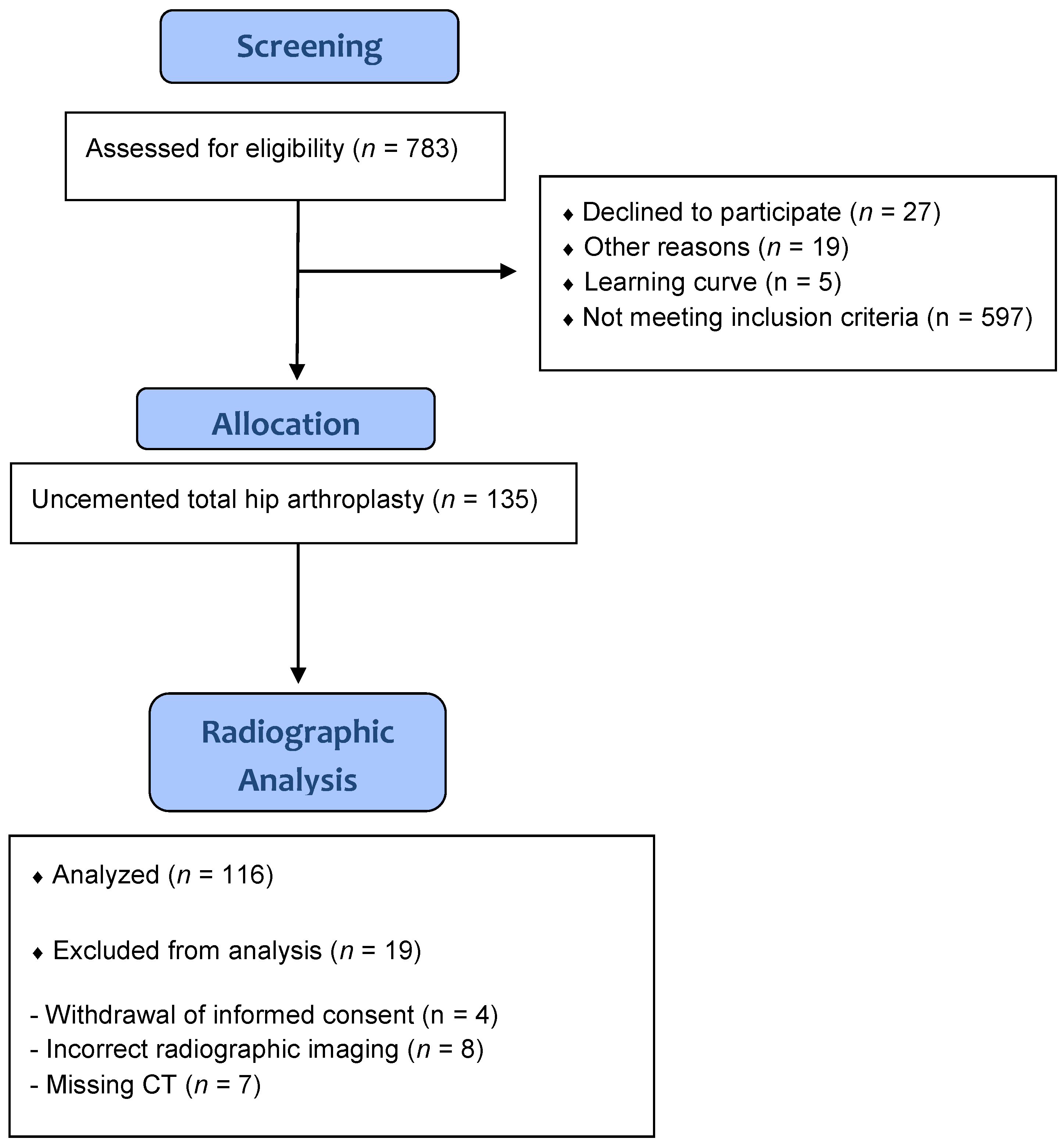
2. Subjects
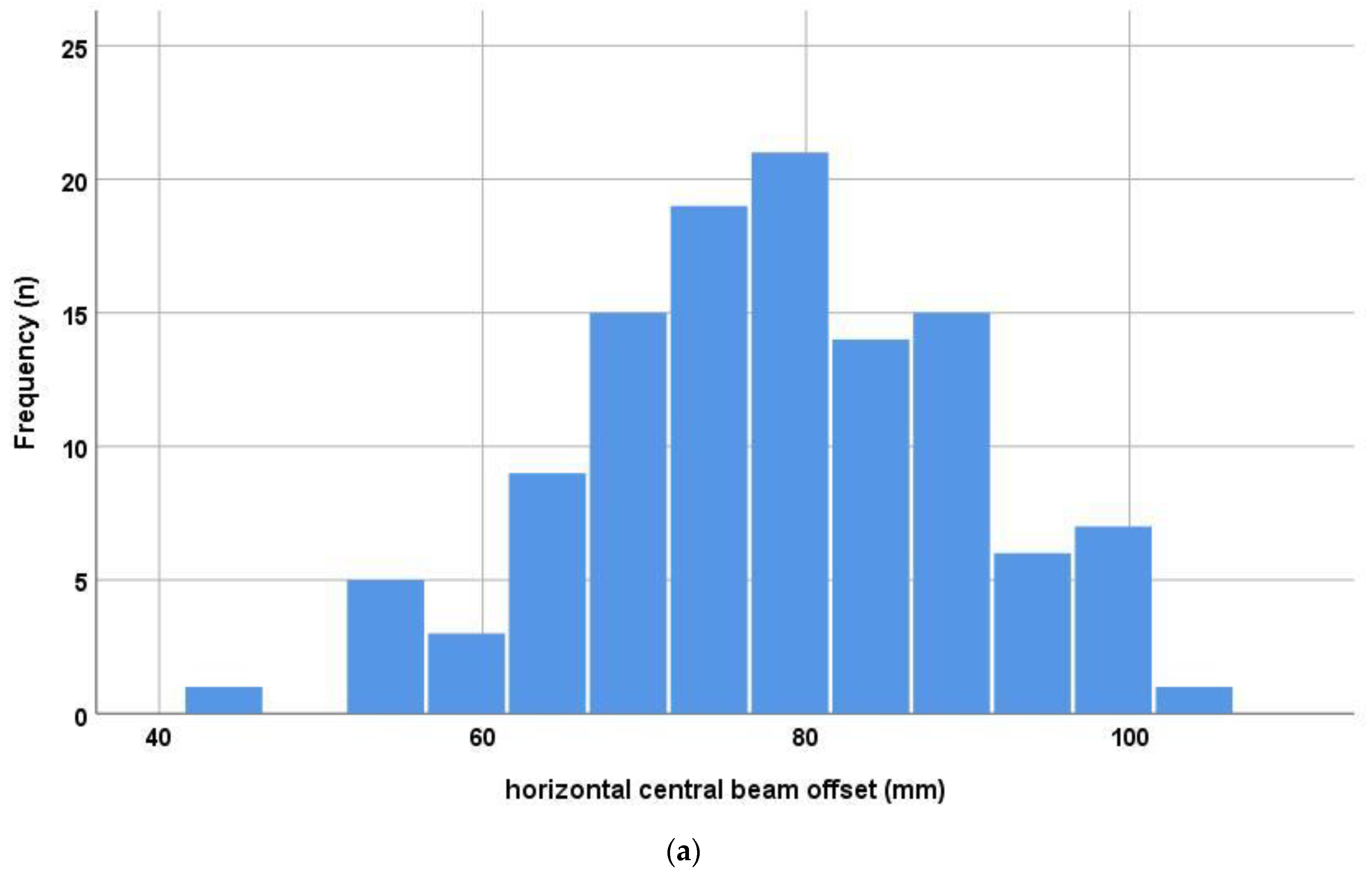
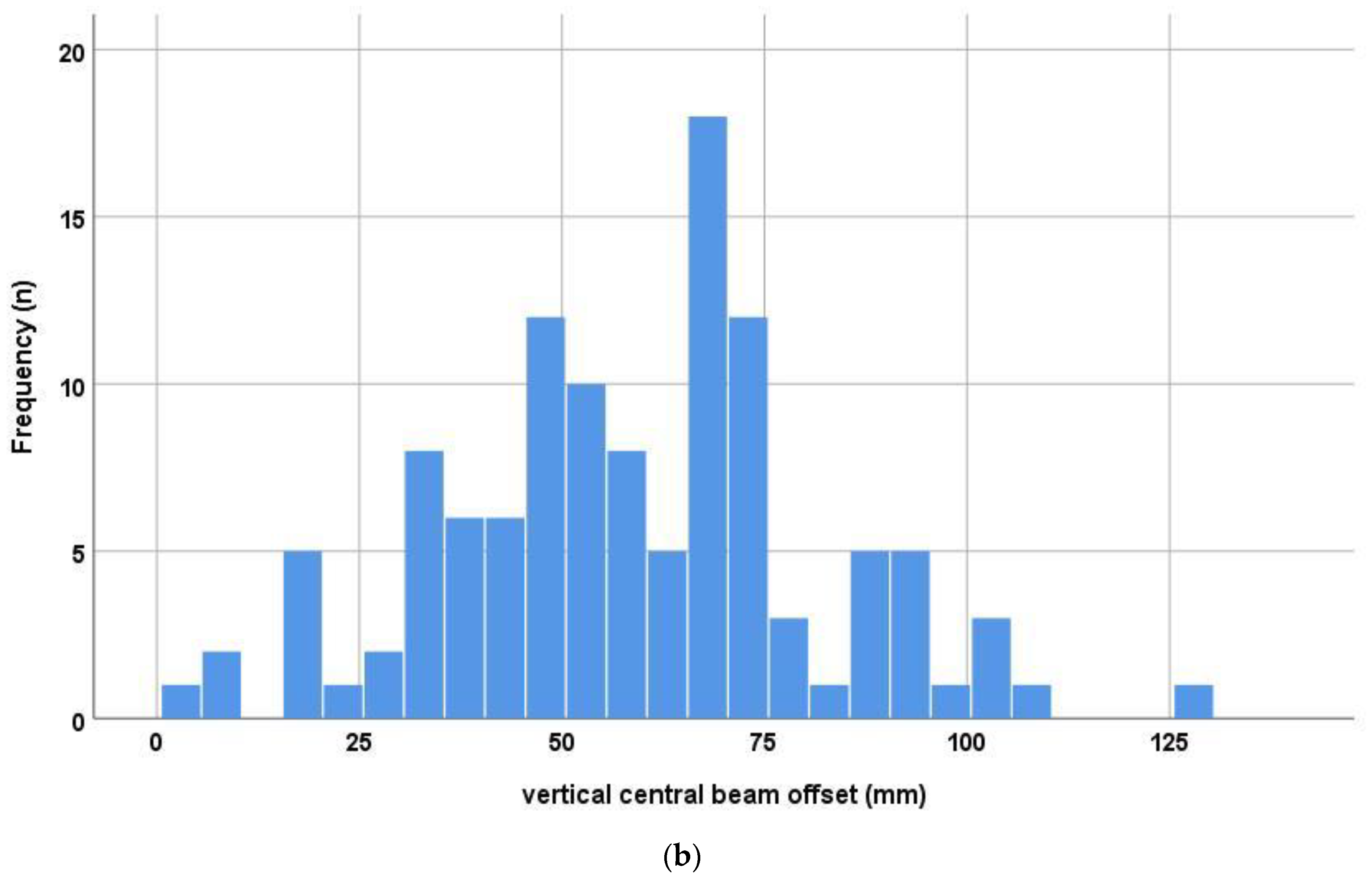
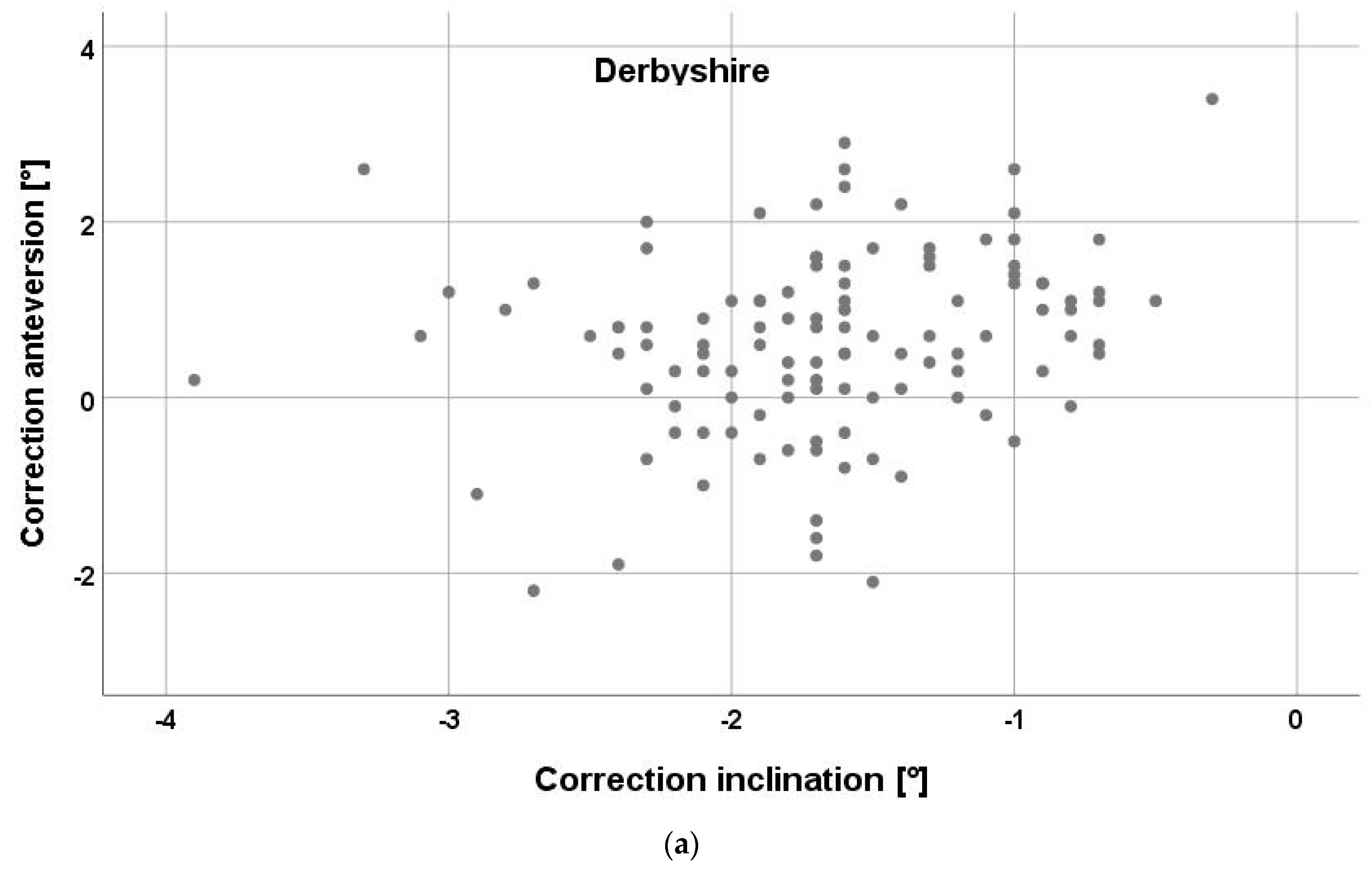
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
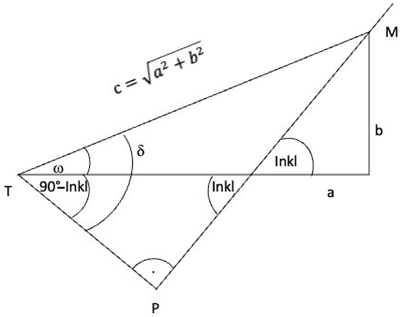
Appendix A
References
- Tezuka, T.; Heckmann, N.D.; Bodner, R.J.; Dorr, L.D. Functional Safe Zone Is Superior to the Lewinnek Safe Zone for Total Hip Arthroplasty: Why the Lewinnek Safe Zone Is Not Always Predictive of Stability. J. Arthroplast. 2019, 34, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Devane, P.A.; Horne, J.G.; Martin, K.; Coldham, G.; Krause, B. Three-dimensional polyethylene wear of a press-fit titanium prosthesis. Factors influencing generation of polyethylene debris. J. Arthroplast. 1997, 12, 256–266. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, M.; Akisue, T.; Bauer, T.W.; Hashimoto, Y. The spatial location of impingement in total hip arthroplasty. J. Arthroplast. 2000, 15, 305–313. [Google Scholar] [CrossRef] [PubMed]
- Weber, M.; von Kunow, F.; Innmann, M.; Meyer, M.; Thieme, M.; Jerabek, S.; Renkawitz, T. Which Safe Zone Is Safe in Total Hip Arthroplasty? The Effect of Bony Impingement. J. Pers. Med. 2022, 12, 812. [Google Scholar] [CrossRef] [PubMed]
- Bayraktar, V.; Weber, M.; von Kunow, F.; Zeman, F.; Craiovan, B.; Renkawitz, T.; Grifka, J.; Woerner, M. Accuracy of measuring acetabular cup position after total hip arthroplasty: Comparison between a radiographic planning software and three-dimensional computed tomography. Int. Orthop. 2017, 41, 731–738. [Google Scholar] [CrossRef] [PubMed]
- Derbyshire, B. Correction of acetabular cup orientation measurements for X-ray beam offset. Med. Eng. Phys. 2008, 30, 1119–1126. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, T.; Weber, M.; Worner, M.; Renkawitz, T.; Grifka, J.; Craiovan, B. Central X-ray beam correction of radiographic acetabular cup measurement after THA: An experimental study. Int. J. Comput. Assist. Radiol. Surg. 2017, 12, 829–837. [Google Scholar] [CrossRef] [PubMed]
- Renkawitz, T.; Weber, M.; Springorum, H.R.; Sendtner, E.; Woerner, M.; Ulm, K.; Weber, T.; Grifka, J. Impingement-free range of movement, acetabular component cover and early clinical results comparing ‘femur-first’ navigation and ‘conventional’ minimally invasive total hip arthroplasty: A randomised controlled trial. Bone Jt. J. 2015, 97-B, 890–898. [Google Scholar] [CrossRef] [PubMed]
- Michel, M.C.; Witschger, P. MicroHip: A minimally invasive procedure for total hip replacement surgery using a modified Smith-Peterson approach. Ortop. Traumatol. Rehabil. 2007, 9, 46–51. [Google Scholar] [PubMed]
- Nomura, T.; Naito, M.; Nakamura, Y.; Ida, T.; Kuroda, D.; Kobayashi, T.; Sakamoto, T.; Seo, H. An analysis of the best method for evaluating anteversion of the acetabular component after total hip replacement on plain radiographs. Bone Jt. J. 2014, 96-B, 597–603. [Google Scholar] [CrossRef] [PubMed]
- Lewinnek, G.E.; Lewis, J.L.; Tarr, R.; Compere, C.L.; Zimmerman, J.R. Dislocations after total hip-replacement arthroplasties. J. Bone Jt. Surg. Am. 1978, 60, 217–220. [Google Scholar] [CrossRef]
- Murray, D.W. The definition and measurement of acetabular orientation. J. Bone Jt. Surg. Br. 1993, 75, 228–232. [Google Scholar] [CrossRef] [PubMed]
- Ellingson, A.M.; Boelter, K.; Sembrano, J.N.; Takahashi, T.; Polly, D.W., Jr. Intraoperative stitched fluoroscopic images: Effect of parallax on angular measurements of the spine. Spine J. 2022, 22, 1012–1015. [Google Scholar] [CrossRef] [PubMed]
- Weldon, M.; Arenas, A.; Abraham, A.; Haidar, L.A.; Warth, R.J.; Mansour, A., 3rd. Attention to Detail: The Effect of Fluoroscopic Parallax on Limb Alignment Assessment During Corrective Osteotomy. J. Am. Acad. Orthop. Surg. Glob. Res. Rev 2023, 7, e22.00289. [Google Scholar] [CrossRef]
- Frandsen, J.J.; Kahn, T.L.; Anderson, L.A.; Pelt, C.E.; Peters, C.L.; Gililland, J.M. Managing Hip-Spine Concepts in the Direct Anterior Approach With Use of Fluoroscopy. J. Arthroplast. 2021, 36, S104–S110. [Google Scholar] [CrossRef] [PubMed]
- Abdel, M.P.; von Roth, P.; Jennings, M.T.; Hanssen, A.D.; Pagnano, M.W. What Safe Zone? The Vast Majority of Dislocated THAs Are Within the Lewinnek Safe Zone for Acetabular Component Position. Clin. Orthop. Relat. Res. 2016, 474, 386–391. [Google Scholar] [CrossRef] [PubMed]
- Weber, M.; Woerner, M.; Messmer, B.; Grifka, J.; Renkawitz, T. Navigation is Equal to Estimation by Eye and Palpation in Preventing Psoas Impingement in THA. Clin. Orthop. Relat. Res. 2017, 475, 196–203. [Google Scholar] [CrossRef] [PubMed]
- Murphy, M.P.; Killen, C.J.; Ralles, S.J.; Brown, N.M.; Hopkinson, W.J.; Wu, K. A precise method for determining acetabular component anteversion after total hip arthroplasty. Bone Jt. J. 2019, 101-B, 1042–1049. [Google Scholar] [CrossRef] [PubMed]
- Weber, M.; Suess, F.; Jerabek, S.A.; Meyer, M.; Grifka, J.; Renkawitz, T.; Dendorfer, S. Kinematic pelvic tilt during gait alters functional cup position in total hip arthroplasty. J. Orthop. Res. 2021, 40, 846–853. [Google Scholar] [CrossRef] [PubMed]
- Widmer, K.H. The Impingement-free, Prosthesis-specific, and Anatomy-adjusted Combined Target Zone for Component Positioning in THA Depends on Design and Implantation Parameters of both Components. Clin. Orthop. Relat. Res. 2020, 478, 1904–1918. [Google Scholar] [CrossRef] [PubMed]


| Study group | number (n) = 116 |
| Gender (female/male) | 64/52 |
| Age (years) | 62.7 ± 7.6 |
| BMI (kg/m2) | 27.0 ± 4.1 |
| Treatment side (left/right) | 53/63 |
| ASA 1 | 24 (20.7%) |
| ASA 2 | 60 (51.7%) |
| ASA 3 | 32 (27.6%) |
| Cup size | 54 (48–62) |
| Femoral component size | 12 (9–16) |
| Operation time (minutes) | 67.3 ± 13.8 |
| CT Cup inclination APP radiographic (°) | 42.6 ± 5.9 |
| CT Cup anteversion APP radiographic (°) | 18.1 ± 8.1 |
| X-ray Cup inclination APP radiographic (°) | 44.6 ± 5.3 |
| X-ray Cup anteversion APP radiographic (°) | 18.7 ± 6.0 |
| Cup | 30_5 | 40_5 | 50_5 | |||
| Anteversion | Inclination | Anteversion | Inclination | Anteversion | Inclination | |
| MW | −0.6 | −0.5 | 0.2 | −0.6 | 1.1 | −0.6 |
| STD | 1.1 | 0.1 | 1.1 | 0.1 | 1.0 | 0.1 |
| Min | −3.6 | −0.7 | −2.4 | −0.8 | −1.2 | −0.9 |
| Max | 1.9 | −0.3 | 2.6 | −0.3 | 3.2 | −0.3 |
| Cup | 30_15 | 40_15 | 50_15 | |||
| Anteversion | Inclination | Anteversion | Inclination | Anteversion | Inclination | |
| MW | −0.7 | −1.4 | 0.2 | −1.5 | 1.1 | −1.5 |
| STD | 1.1 | 0.2 | 1.1 | 0.2 | 1.0 | 0.3 |
| Min | −3.7 | −1.9 | −2.5 | −2.1 | −1.3 | −2.2 |
| Max | 1.9 | −1 | 2.6 | −0.9 | 3.2 | −0.8 |
| Cup | 30_25 | 40_25 | 50_25 | |||
| Anteversion | Inclination | Anteversion | Inclination | Anteversion | Inclination | |
| MW | −0.7 | −2.4 | 0.2 | −2.5 | 1.0 | −2.5 |
| STD | 1.1 | 0.3 | 1.1 | 0.4 | 1.0 | 0.4 |
| Min | −3.8 | −3.2 | −2.6 | −3.5 | −1.3 | −3.7 |
| Max | 1.8 | −1.7 | 2.5 | −1.5 | 3.1 | −1.3 |
| Inclination | Coefficient | 95% Confidence Interval | p Value | |
| Sex | 0.30 | 0.06 | 0.25 | 0.002 |
| Age | 0.05 | 0.00 | 0.01 | 0.6 |
| BMI | 0.07 | −0.01 | 0.02 | 0.5 |
| Treamtment Side | −0.10 | −0.14 | 0.04 | 0.3 |
| Anteversion | Coefficient | 95% Confidence Interval | p Value | |
| Sex | 0.33 | 0.31 | 1.0 | <0.001 |
| Age | −0.01 | −0.02 | 0.2 | 1.0 |
| BMI | 0.23 | 0.01 | 0.14 | 0.01 |
| Treamtment Side | 0.07 | −0.22 | 0.49 | 0.4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Weber, M.; Meyer, M.; Von Kunow, F.; Füchtmeier, B.; Hillmann, A.; Wulbrand, C. How Relevant Is the Parallax Effect on Low Centered Pelvic Radiographs in Total Hip Arthroplasty. J. Pers. Med. 2023, 13, 881. https://doi.org/10.3390/jpm13060881
Weber M, Meyer M, Von Kunow F, Füchtmeier B, Hillmann A, Wulbrand C. How Relevant Is the Parallax Effect on Low Centered Pelvic Radiographs in Total Hip Arthroplasty. Journal of Personalized Medicine. 2023; 13(6):881. https://doi.org/10.3390/jpm13060881
Chicago/Turabian StyleWeber, Markus, Matthias Meyer, Frederik Von Kunow, Bernd Füchtmeier, Axel Hillmann, and Christian Wulbrand. 2023. "How Relevant Is the Parallax Effect on Low Centered Pelvic Radiographs in Total Hip Arthroplasty" Journal of Personalized Medicine 13, no. 6: 881. https://doi.org/10.3390/jpm13060881
APA StyleWeber, M., Meyer, M., Von Kunow, F., Füchtmeier, B., Hillmann, A., & Wulbrand, C. (2023). How Relevant Is the Parallax Effect on Low Centered Pelvic Radiographs in Total Hip Arthroplasty. Journal of Personalized Medicine, 13(6), 881. https://doi.org/10.3390/jpm13060881






