Demographic and Socioeconomic Factors in Prospective Retina-Focused Clinical Trial Screening and Enrollment
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Collection
2.2. Statistical Analysis
3. Results
3.1. Factors Statistically Significantly Associated with Clinical Trial Recruitment Status
3.1.1. Age (n = 1476)
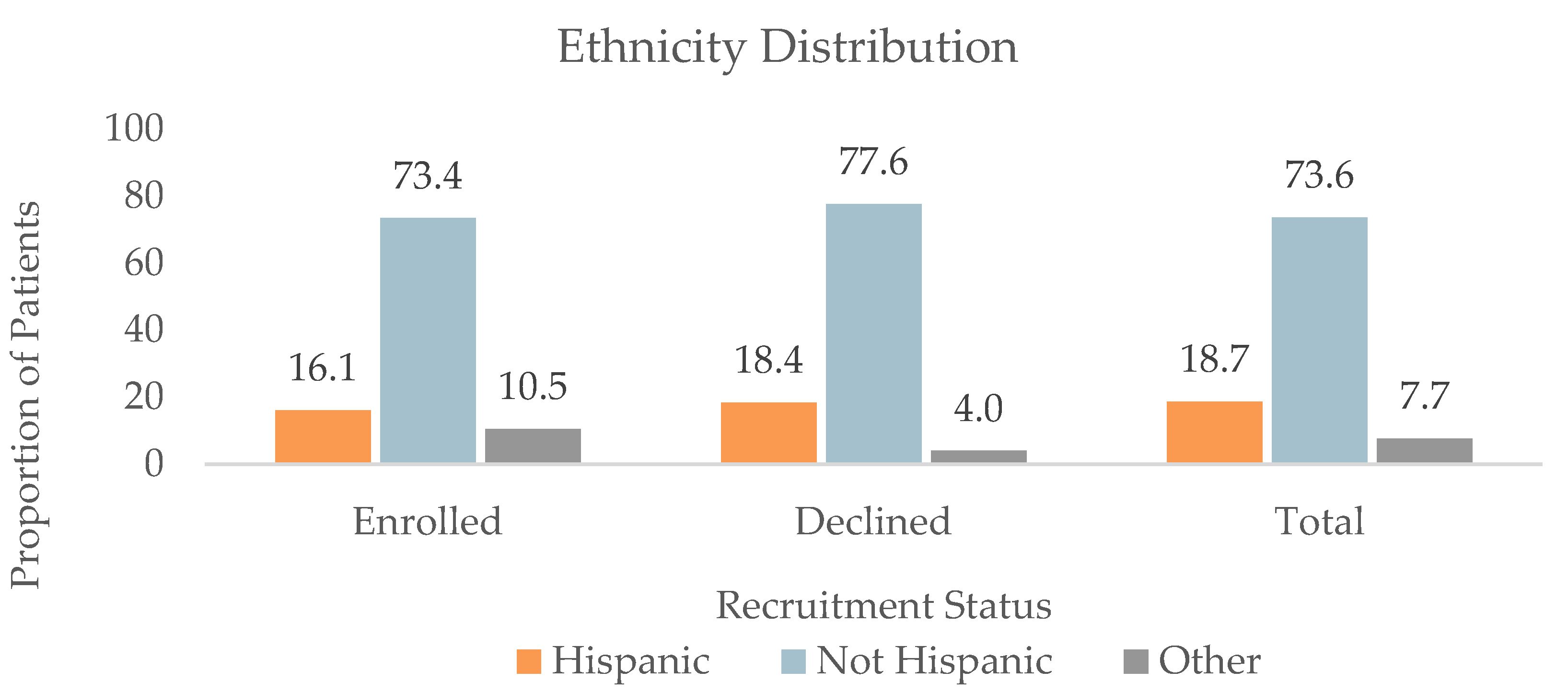
3.1.2. Ethnicity (n = 1472)
3.1.3. Preferred Language (n = 1442)
3.1.4. Insurance Status (n = 1477)
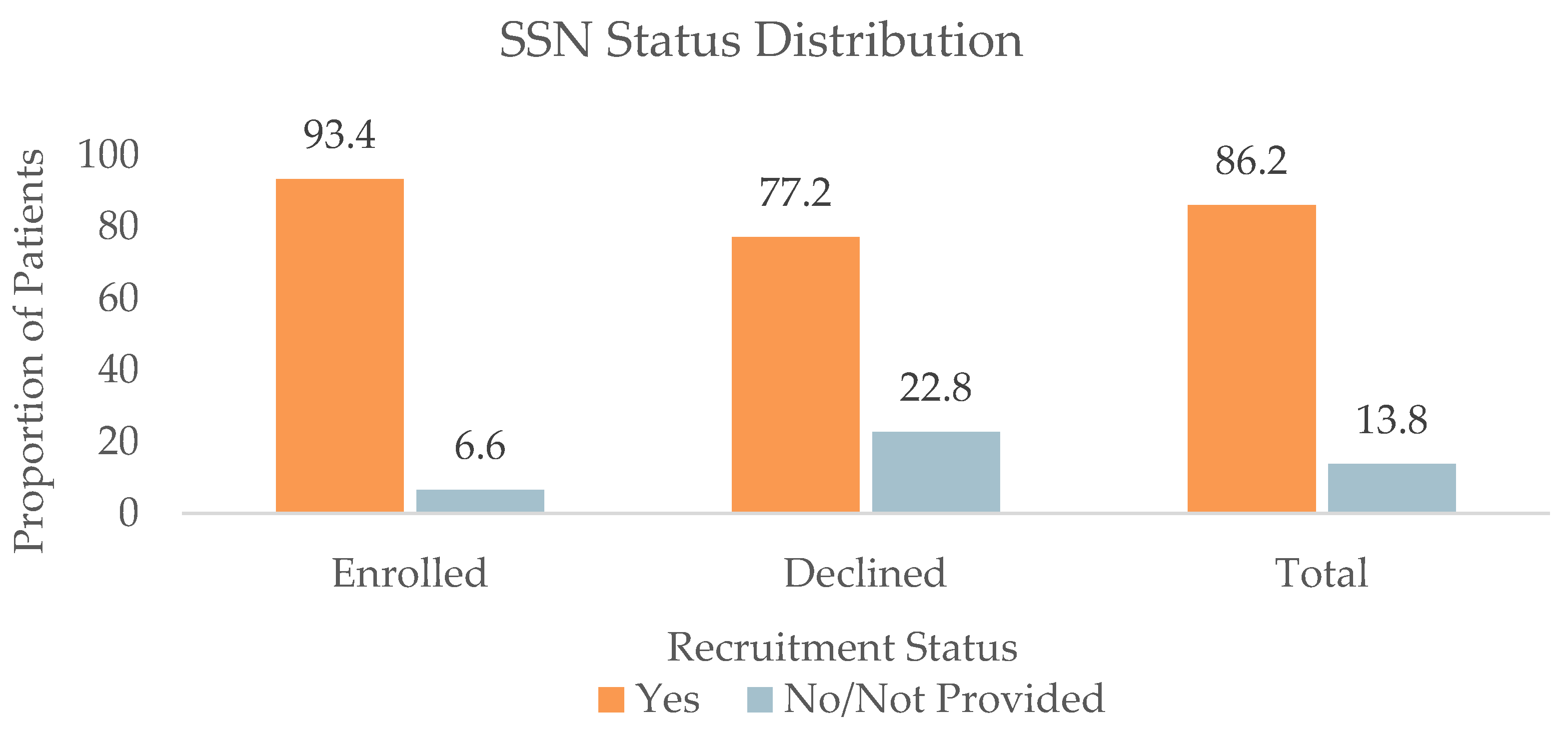
3.1.5. SSN Status (n = 1477)
3.2. Factors Not Significantly Associated with Clinical Trial Recruitment Status
3.3. Multivariable Analysis for Demographic Factors: Odds Ratios
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rosenblatt, T.R.; Vail, D.; Saroj, N.; Boucher, N.; Moshfeghi, D.M.; Moshfeghi, A.A. Increasing Incidence and Prevalence of Common Retinal Diseases in Retina Practices Across the United States. Ophthalmic Surg. Lasers Imaging Retin. 2021, 52, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Rein, D.B.; Wittenborn, J.S.; Burke-Conte, Z.; Gulia, R.; Robalik, T.; Ehrlich, J.R.; Lundeen, E.A.; Flaxman, A.D. Prevalence of Age-Related Macular Degeneration in the US in 2019. JAMA Ophthalmol. 2022, 140, 1202–1208. [Google Scholar] [CrossRef] [PubMed]
- Sinclair, S.H.; Schwartz, S.S. Diabetic Retinopathy–An Underdiagnosed and Undertreated Inflammatory, Neuro-Vascular Complication of Diabetes. Front. Endocrinol. 2019, 10, 843. [Google Scholar] [CrossRef]
- Varma, R.; Bressler, N.M.; Doan, Q.V.; Gleeson, M.; Danese, M.; Bower, J.K.; Selvin, E.; Dolan, C.; Fine, J.; Colman, S.; et al. Prevalence of and Risk Factors for Diabetic Macular Edema in the United States. JAMA Ophthalmol. 2014, 132, 1334–1340. [Google Scholar] [CrossRef]
- Zhang, X.; Cotch, M.F.; Ryskulova, A.; Primo, S.A.; Nair, P.; Chou, C.-F.; Geiss, L.S.; Barker, L.; Elliott, A.F.; Crews, J.E.; et al. Vision Health Disparities in the United States by Race/Ethnicity, Education, and Economic Status: Findings from Two Nationally Representative Surveys. Am. J. Ophthalmol. 2012, 154, S53–S62.e1. [Google Scholar] [CrossRef]
- Yip, J.L.Y.; Muthy, Z.; Peto, T.; Lotery, A.; Foster, P.J.; Patel, P. Socioeconomic Risk Factors and Age-Related Macular Degeneration in the UK Biobank Study. BMJ Open Ophthalmol. 2021, 6, e000585. [Google Scholar] [CrossRef] [PubMed]
- Rogers, S.; McIntosh, R.L.; Cheung, N.; Lim, L.; Wang, J.J.; Mitchell, P.; Kowalski, J.W.; Nguyen, H.; Wong, T.Y. The Prevalence of Retinal Vein Occlusion: Pooled Data from Population Studies from the United States, Europe, Asia, and Australia. Ophthalmology 2010, 117, 313–319.e1. [Google Scholar] [CrossRef]
- Pérez-Stable, E.J.; Alvidrez, J.; Hill, C.V. Definitions, Principles, and Concepts for Minority Health and Health Disparities Research. In The Science of Health Disparities Research; Wiley: Hoboken, NJ, USA, 2021; pp. 1–12. ISBN 978-1-119-37485-5. [Google Scholar]
- Coney, J.M.; Scott, A.W. Racial Disparities in the Screening and Treatment of Diabetic Retinopathy. J. Natl. Med. Assoc. 2022, 114, 171–181. [Google Scholar] [CrossRef]
- Varma, R.; Torres, M.; Peña, F.; Klein, R.; Azen, S.P. Prevalence of Diabetic Retinopathy in Adult Latinos: The Los Angeles Latino Eye Study. Ophthalmology 2004, 111, 1298–1306. [Google Scholar] [CrossRef]
- Varma, R.; Ying-Lai, M.; Klein, R.; Azen, S.P. Prevalence and Risk Indicators of Visual Impairment and Blindness in Latinos: The Los Angeles Latino Eye Study. Ophthalmology 2004, 111, 1132–1140. [Google Scholar] [CrossRef]
- Muñoz, B.; O’Leary, M.; Fonseca-Becker, F.; Rosario, E.; Burguess, I.; Aguilar, M.; Fickes, C.; West, S.K. Knowledge of Diabetic Eye Disease and Vision Care Guidelines Among Hispanic Individuals in Baltimore With and Without Diabetes. Arch. Ophthalmol. 2008, 126, 968–974. [Google Scholar] [CrossRef] [PubMed]
- Muñoz, B.; West, S.K.; Rubin, G.S.; Schein, O.D.; Quigley, H.A.; Bressler, S.B.; Bandeen-Roche, K.; and the SEE Study Team. Causes of Blindness and Visual Impairment in a Population of Older Americans: The Salisbury Eye Evaluation Study. Arch. Ophthalmol. 2000, 118, 819–825. [Google Scholar] [CrossRef] [PubMed]
- Soares, R.R.; Huang, C.; Sharpe, J.; Cobbs, L.; Gopal, A.; Rao, W.; Samuelson, A.; Parikh, D.; Zhang, Q.; Bailey, R.; et al. Geographic and Socioeconomic Access Disparities to Phase 3 Clinical Trials in Ophthalmology in the United States. Eye 2022. [Google Scholar] [CrossRef]
- Baxter, S.L. Representation Matters—Diversity in Retina Clinical Trials. JAMA Ophthalmol. 2022, 140, 1103–1104. [Google Scholar] [CrossRef] [PubMed]
- Berkowitz, S.T.; Groth, S.L.; Gangaputra, S.; Patel, S. Racial/Ethnic Disparities in Ophthalmology Clinical Trials Resulting in US Food and Drug Administration Drug Approvals from 2000 to 2020|Ophthalmology|JAMA Ophthalmology|JAMA Network. Available online: https://jamanetwork-com.ezproxy.med.cornell.edu/journals/jamaophthalmology/fullarticle/2778782 (accessed on 1 March 2023).
- Kaakour, A.-H.; Hua, H.-U.; Rachitskaya, A. Representation of Race and Ethnicity in Randomized Clinical Trials of Diabetic Macular Edema and Retinal Vein Occlusion Compared to 2010 US Census Data. JAMA Ophthalmol. 2022, 140, 1096–1102. [Google Scholar] [CrossRef]
- Soares, R.R.; Gopal, A.D.; Parikh, D.; Shields, C.N.; Patel, S.; Hinkle, J.; Sharpe, J.; Ho, A.C.; Regillo, C.D.; Haller, J.; et al. Geographic Access Disparities of Clinical Trials in Neovascular Age-Related Macular Degeneration in the United States. Am. J. Ophthalmol. 2021, 229, 160–168. [Google Scholar] [CrossRef]
- Soares, R.R.; Parikh, D.; Shields, C.N.; Peck, T.; Gopal, A.; Sharpe, J.; Yonekawa, Y. Geographic Access Disparities to Clinical Trials in Diabetic Eye Disease in the United States. Ophthalmol. Retin. 2021, 5, 879–887. [Google Scholar] [CrossRef]
- National Academies of Sciences, Engineering, and Medicine; Policy and Global Affairs; Committee on Women in Science, Engineering, and Medicine; Committee on Improving the Representation of Women and Underrepresented Minorities in Clinical Trials and Research; Bibbins-Domingo, K.; Helman, A. Why Diverse Representation in Clinical Research Matters and the Current State of Representation within the Clinical Research Ecosystem; National Academies Press (US): Washington, DC, USA, 2022. [Google Scholar] [CrossRef]
- Ramamoorthy, A.; Pacanowski, M.; Bull, J.; Zhang, L. Racial/Ethnic Differences in Drug Disposition and Response: Review of Recently Approved Drugs. Clin. Pharmacol. Ther. 2015, 97, 263–273. [Google Scholar] [CrossRef]
- Baca, E.; Garcia-Garcia, M.; Porras-Chavarino, A. Gender Differences in Treatment Response to Sertraline versus Imipramine in Patients with Nonmelancholic Depressive Disorders. Prog. Neuropsychopharmacol. Biol. Psychiatry 2004, 28, 57–65. [Google Scholar] [CrossRef] [PubMed]
- Bano, S.; Akhter, S.; Afridi, M.I. Gender Based Response to Fluoxetine Hydrochloride Medication in Endogenous Depression. J. Coll. Physicians Surg.-Pak. JCPSP 2004, 14, 161–165. [Google Scholar]
- Melotte, S.; Kejriwal, M. A Geo-Tagged COVID-19 Twitter Dataset for 10 North American Metropolitan Areas over a 255-Day Period. Data 2021, 6, 64. [Google Scholar] [CrossRef]
- Oliphant, S.N. Examining Time-Variant Spatial Dependence of Urban Places and Shootings. J. Urban Health 2021, 98, 777–790. [Google Scholar] [CrossRef] [PubMed]
- Camacho, K.; Portelli, R.; Shortridge, A.; Takahashi, B. Sentiment Mapping: Point Pattern Analysis of Sentiment Classified Twitter Data. Cartogr. Geogr. Inf. Sci. 2021, 48, 241–257. [Google Scholar] [CrossRef]
- Herrera, A.P.; Snipes, S.A.; King, D.W.; Torres-Vigil, I.; Goldberg, D.S.; Weinberg, A.D. Disparate Inclusion of Older Adults in Clinical Trials: Priorities and Opportunities for Policy and Practice Change. Am. J. Public Health 2010, 100, S105–S112. [Google Scholar] [CrossRef] [PubMed]
- Ludmir, E.B.; Mainwaring, W.; Lin, T.A.; Miller, A.B.; Jethanandani, A.; Espinoza, A.F.; Mandel, J.J.; Lin, S.H.; Smith, B.D.; Smith, G.L.; et al. Factors Associated With Age Disparities Among Cancer Clinical Trial Participants. JAMA Oncol. 2019, 5, 1769–1773. [Google Scholar] [CrossRef]
- Zulman, D.M.; Sussman, J.B.; Chen, X.; Cigolle, C.T.; Blaum, C.S.; Hayward, R.A. Examining the Evidence: A Systematic Review of the Inclusion and Analysis of Older Adults in Randomized Controlled Trials. J. Gen. Intern. Med. 2011, 26, 783–790. [Google Scholar] [CrossRef]
- Florisson, S.; Aagesen, E.K.; Bertelsen, A.S.; Nielsen, L.P.; Rosholm, J.-U. Are Older Adults Insufficiently Included in Clinical Trials?—An Umbrella Review. Basic Clin. Pharmacol. Toxicol. 2021, 128, 213–223. [Google Scholar] [CrossRef]
- Buffenstein, I.; Kaneakua, B.; Taylor, E.; Matsunaga, M.; Choi, S.Y.; Carrazana, E.; Viereck, J.; Liow, K.K.; Ghaffari-Rafi, A. Demographic Recruitment Bias of Adults in United States Randomized Clinical Trials by Disease Categories between 2008 to 2019: A Systematic Review and Meta-Analysis. Sci. Rep. 2023, 13, 42. [Google Scholar] [CrossRef]
- Staples, J.N.; Lester, J.; Li, A.; Walsh, C.; Cass, I.; Karlan, B.Y.; Bresee, C.; Rimel, B.J. Language as a Barrier to Cancer Clinical Trial Accrual: Assessing Consenting Team Knowledge and Practices for Cancer Clinical Trial Consent among Low English Fluency Patients. Appl. Cancer Res. 2018, 38, 14. [Google Scholar] [CrossRef]
- Mudie, L.I.; Patnaik, J.L.; Gill, Z.; Wagner, M.; Christopher, K.L.; Seibold, L.K.; Ifantides, C. Disparities in Eye Clinic Patient Encounters among Patients Requiring Language Interpreter Services. BMC Ophthalmol. 2023, 23, 82. [Google Scholar] [CrossRef]
- Nipp, R.D.; Hong, K.; Paskett, E.D. Overcoming Barriers to Clinical Trial Enrollment. Am. Soc. Clin. Oncol. Educ. Book 2019, 39, 105–114. [Google Scholar] [CrossRef] [PubMed]
- Sohn, H. Racial and Ethnic Disparities in Health Insurance Coverage: Dynamics of Gaining and Losing Coverage over the Life-Course. Popul. Res. Policy Rev. 2017, 36, 181–201. [Google Scholar] [CrossRef] [PubMed]
- Diaz, G.A.; Crowe, J.; Hopkin, J. Health Insurance Literacy and Health Services Access Barriers in Niemann–Pick Disease: The Patient and Caregiver Voice. Orphanet J. Rare Dis. 2022, 17, 332. [Google Scholar] [CrossRef]
- Venkatesh, A.K.; Chou, S.-C.; Li, S.-X.; Choi, J.; Ross, J.S.; D’Onofrio, G.; Krumholz, H.M.; Dharmarajan, K. Association Between Insurance Status and Access to Hospital Care in Emergency Department Disposition. JAMA Intern. Med. 2019, 179, 686–693. [Google Scholar] [CrossRef]
- Unger, J.M.; Gralow, J.R.; Albain, K.S.; Ramsey, S.D.; Hershman, D.L. Patient Income Level and Cancer Clinical Trial Participation: A Prospective Survey Study. JAMA Oncol. 2016, 2, 137–139. [Google Scholar] [CrossRef] [PubMed]
- Sanjiv, N.; Osathanugrah, P.; Harrell, M.; Siegel, N.H.; Ness, S.; Chen, X.; Cabral, H.; Subramanian, M.L. Race and Ethnic Representation among Clinical Trials for Diabetic Retinopathy and Diabetic Macular Edema within the United States: A Review. J. Natl. Med. Assoc. 2022, 114, 123–140. [Google Scholar] [CrossRef]
- Hamel, L.M.; Penner, L.A.; Albrecht, T.L.; Heath, E.; Gwede, C.K.; Eggly, S. Barriers to Clinical Trial Enrollment in Racial and Ethnic Minority Patients With Cancer. Cancer Control J. Moffitt Cancer Cent. 2016, 23, 327–337. [Google Scholar] [CrossRef]
- Scharff, D.P.; Mathews, K.J.; Jackson, P.; Hoffsuemmer, J.; Martin, E.; Edwards, D. More than Tuskegee: Understanding Mistrust about Research Participation. J. Health Care Poor. Underserved 2010, 21, 879–897. [Google Scholar] [CrossRef]
- Berkowitz, S.A.; Traore, C.Y.; Singer, D.E.; Atlas, S.J. Evaluating Area-Based Socioeconomic Status Indicators for Monitoring Disparities within Health Care Systems: Results from a Primary Care Network. Health Serv. Res. 2015, 50, 398–417. [Google Scholar] [CrossRef]
- Thomas, A.J.; Eberly, L.E.; Davey Smith, G.; Neaton, J.D.; for the Multiple Risk Factor Intervention Trial (MRFIT) Research Group. ZIP-Code-Based versus Tract-Based Income Measures as Long-Term Risk-Adjusted Mortality Predictors. Am. J. Epidemiol. 2006, 164, 586–590. [Google Scholar] [CrossRef]


| Characteristic | n 1 | All Patients | Enrolled | Declined | Communication | DNQ | |
|---|---|---|---|---|---|---|---|
| Total | 1477 | 1477 | 635 | 232 | 290 | 320 | |
| Average Age (SD) | 1476 | 68.5 (13.9) | 67.9 (14.2) | 70.3 (13.8) | 66.5 (14.3) | 70.0 (12.6) | |
| Gender (%) | Male | 1475 | 647 (43.9) | 300 (47.3) | 101 (43.5) | 113 (39.1) | 133 (41.6) |
| Female | 828 (56.1) | 334 (52.7) | 131 (56.5) | 176 (60.9) | 187 (58.4) | ||
| Race (%) | White | 1459 | 900 (61.7) | 368 (59.1) | 147 (64.2) | 165 (57.5) | 220 (68.8) |
| Black | 139 (9.5) | 67 (10.8) | 18 (7.9) | 36 (12.5) | 18 (5.6) | ||
| Asian | 54 (3.8) | 27 (4.3) | 13 (5.7) | 11 (3.9) | 4 (1.2) | ||
| Other | 365 (25.0) | 161 (25.8) | 51 (22.2) | 75 (26.1) | 78 (24.4) | ||
| Ethnicity (%) | Hispanic | 1472 | 275 (18.7) | 102 (16.1) | 42 (18.4) | 67 (23.2) | 64 (20.0) |
| Not Hispanic | 1083 (73.6) | 466 (73.4) | 177 (77.6) | 196 (67.8) | 244 (76.3) | ||
| Other | 114 (7.7) | 67 (10.5) | 9 (4.0) | 26 (9.0) | 12 (3.7) | ||
| Preferred Language (%) | English | 1442 | 1306 (90.6) | 573 (92.7) | 202 (89.4) | 248 (87.9) | 283 (90.4) |
| Spanish | 126 (8.8) | 39 (6.3) | 23 (10.2) | 33 (11.7) | 29 (9.3) | ||
| Other | 9 (0.6) | 6 (1.0) | 1 (0.4) | 1 (0.4) | 1 (0.3) |
| Characteristic | All Patients | Enrolled | Declined | Communication | DNQ | |
|---|---|---|---|---|---|---|
| Total | 1477 | 635 | 232 | 290 | 320 | |
| Insurance Status (%) | Yes | 1358 (91.9) | 600 (94.5) | 261 (90.0) | 204 (87.9) | 293 (91.6) |
| No/not provided | 119 (8.1) | 35 (5.5) | 28 (10.0) | 28 (12.1) | 27 (8.4) | |
| SSN (%) | Yes | 1273 (86.2) | 593 (93.4) | 233 (80.3) | 179 (77.2) | 268 (83.8) |
| No/not provided | 204 (13.8) | 42 (6.6) | 57 (19.7) | 53 (22.8) | 52 (16.3) | |
| Characteristic | Odds Ratio | Standard Error | z | p | [95% Confidence Interval] | ||
|---|---|---|---|---|---|---|---|
| Age | 0.98 | 0.007 | −2.47 | 0.01 | 0.97 | 1.00 | |
| Gender | Female | 0.86 | 0.14 | −0.95 | 0.34 | 0.62 | 1.18 |
| Race | Black | 1.23 | 0.36 | 0.69 | 0.49 | 0.69 | 2.20 |
| Asian | 1.14 | 0.27 | 0.57 | 0.57 | 0.72 | 1.81 | |
| Other | 0.62 | 0.23 | −1.27 | 0.20 | 0.30 | 1.29 | |
| Ethnicity | Not Hispanic | 0.80 | 0.24 | −0.75 | 0.45 | 0.44 | 1.44 |
| Other | 2.34 | 1.19 | 1.66 | 0.10 | 0.86 | 6.36 | |
| Preferred language | Spanish | 0.35 | 0.13 | −2.86 | 0.00 | 0.17 | 0.72 |
| Other | 3.1 | 3.43 | 1.01 | 0.32 | 0.34 | 27.35 | |
| Baseline Odds | 11.18 | 5.61 | 4.81 | 0.00 | 4.18 | 29.89 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cao, J.A.; Patel, S.B.; Wong, C.W.; Garcia, D.; Munoz, J.; Cone, C.; Zamora, D.; Reagan, M.; Nguyen, T.V.; Pearce, W.; et al. Demographic and Socioeconomic Factors in Prospective Retina-Focused Clinical Trial Screening and Enrollment. J. Pers. Med. 2023, 13, 880. https://doi.org/10.3390/jpm13060880
Cao JA, Patel SB, Wong CW, Garcia D, Munoz J, Cone C, Zamora D, Reagan M, Nguyen TV, Pearce W, et al. Demographic and Socioeconomic Factors in Prospective Retina-Focused Clinical Trial Screening and Enrollment. Journal of Personalized Medicine. 2023; 13(6):880. https://doi.org/10.3390/jpm13060880
Chicago/Turabian StyleCao, Jessica A., Sagar B. Patel, Calvin W. Wong, David Garcia, Jose Munoz, Cassandra Cone, Deneva Zamora, Mary Reagan, Tieu V. Nguyen, Will Pearce, and et al. 2023. "Demographic and Socioeconomic Factors in Prospective Retina-Focused Clinical Trial Screening and Enrollment" Journal of Personalized Medicine 13, no. 6: 880. https://doi.org/10.3390/jpm13060880
APA StyleCao, J. A., Patel, S. B., Wong, C. W., Garcia, D., Munoz, J., Cone, C., Zamora, D., Reagan, M., Nguyen, T. V., Pearce, W., Fish, R. H., Brown, D. M., Chaudhary, V., Wykoff, C. C., & Fan, K. C. (2023). Demographic and Socioeconomic Factors in Prospective Retina-Focused Clinical Trial Screening and Enrollment. Journal of Personalized Medicine, 13(6), 880. https://doi.org/10.3390/jpm13060880






