Non-Surgical Transversal Dentoalveolar Compensation with Completely Customized Lingual Appliances versus Surgically Assisted Rapid Palatal Expansion in Adults—Tipping or Translation in Posterior Crossbite Correction?
Abstract
1. Introduction
2. Materials and Methods
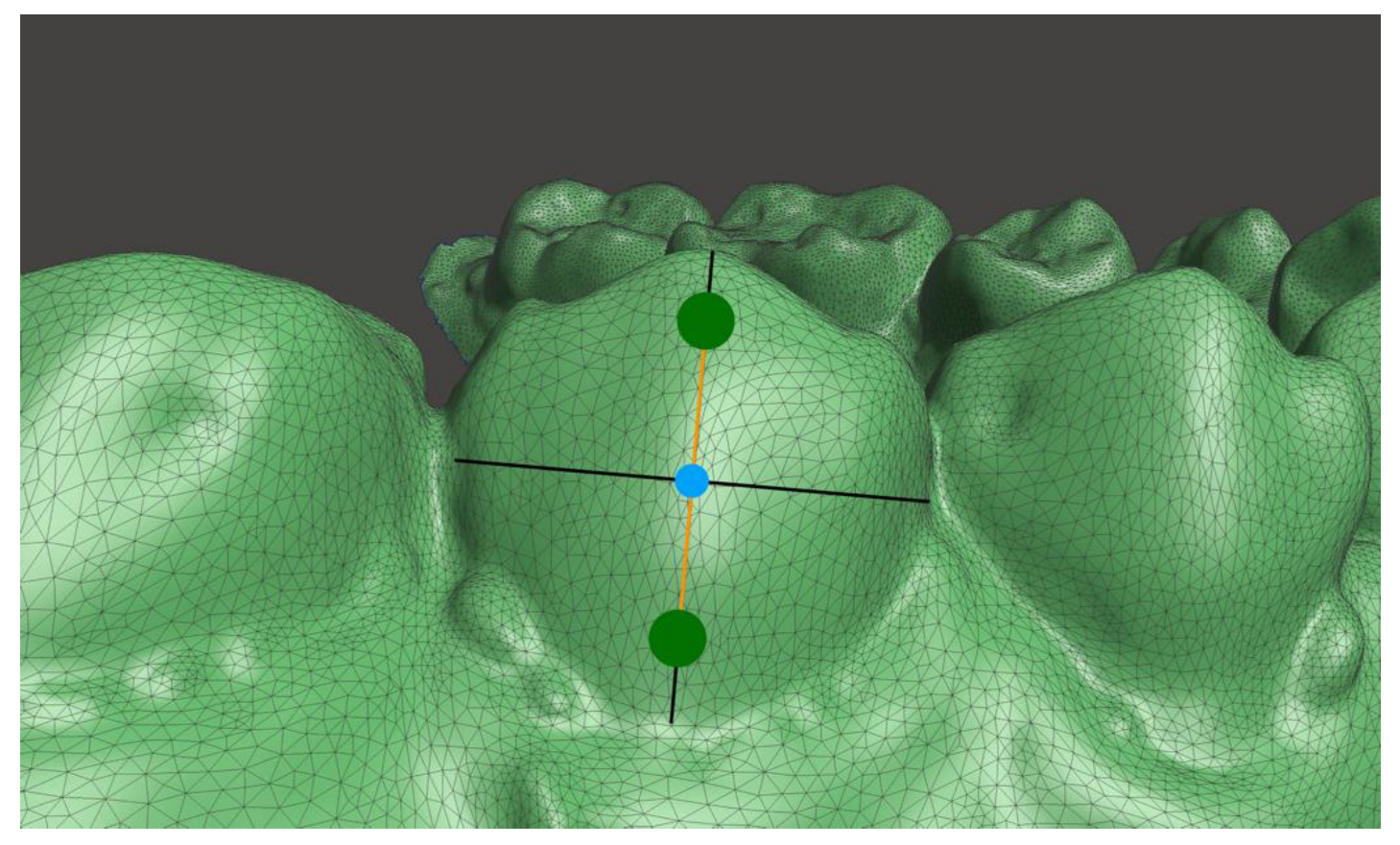
2.1. Measurement of the Buccolingual Inclination
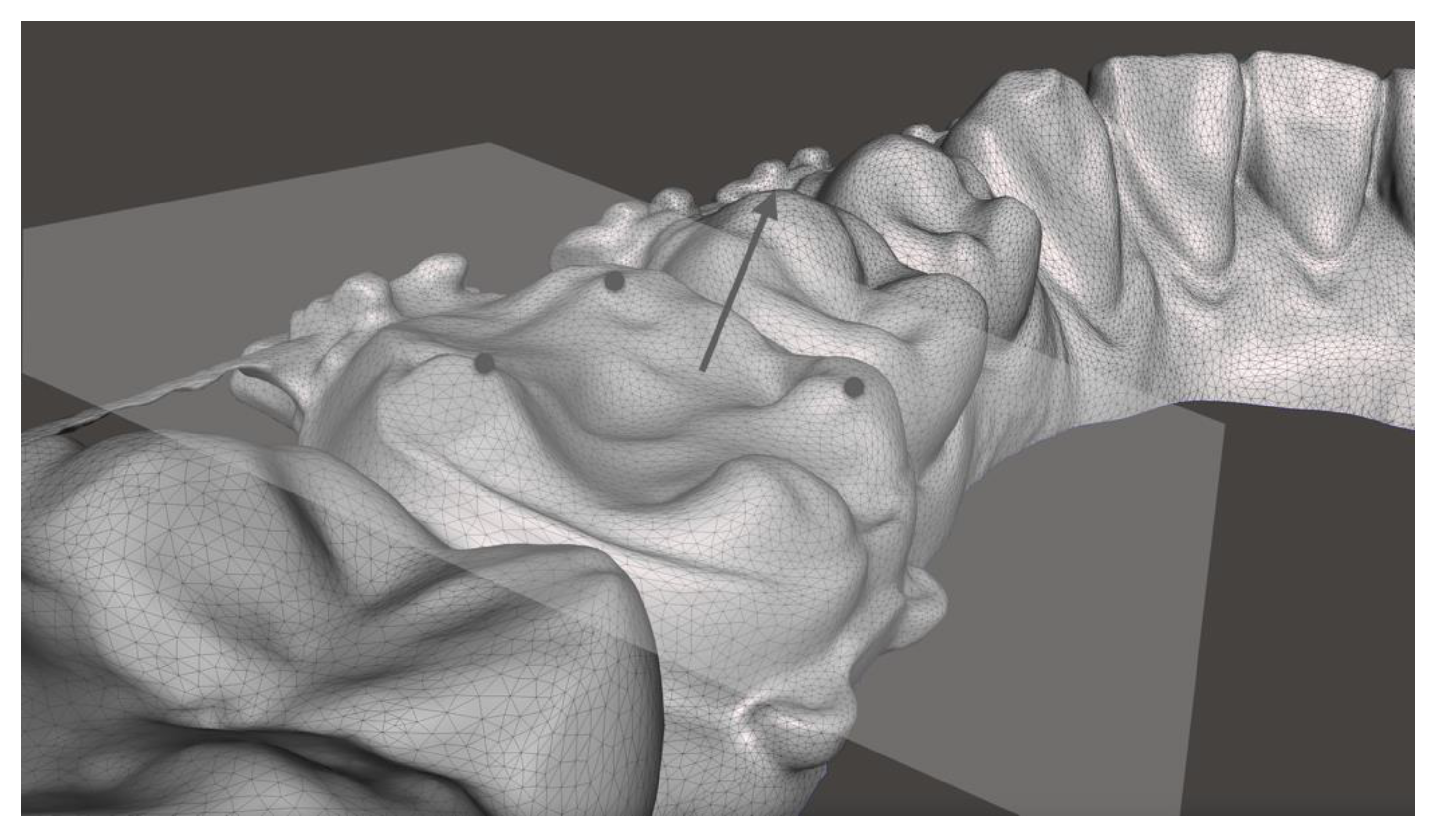
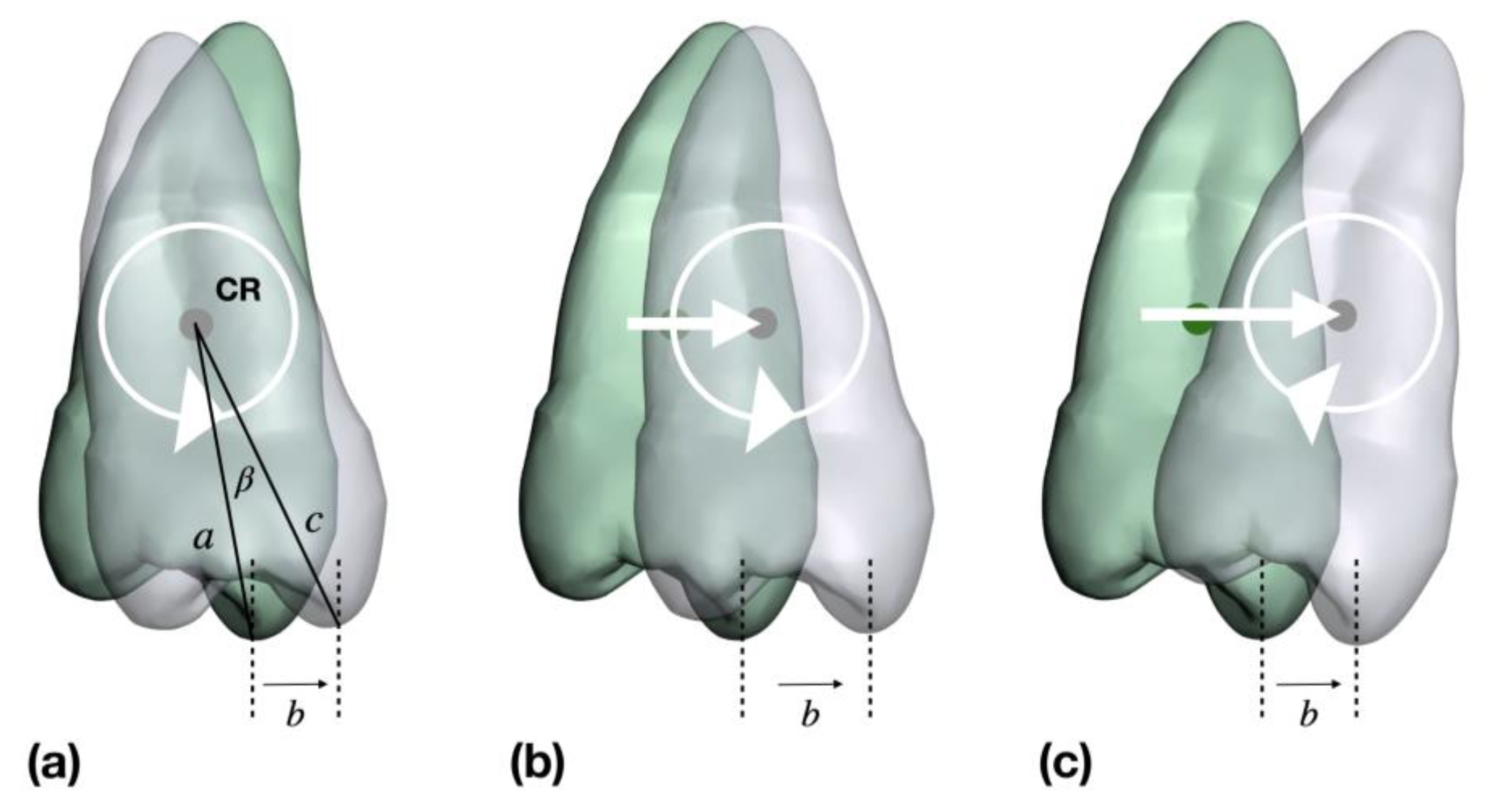
2.2. Analysis of Tooth Movements: Uncontrolled Tipping or Bodily Movements
2.3. Statistical Analysis
3. Results
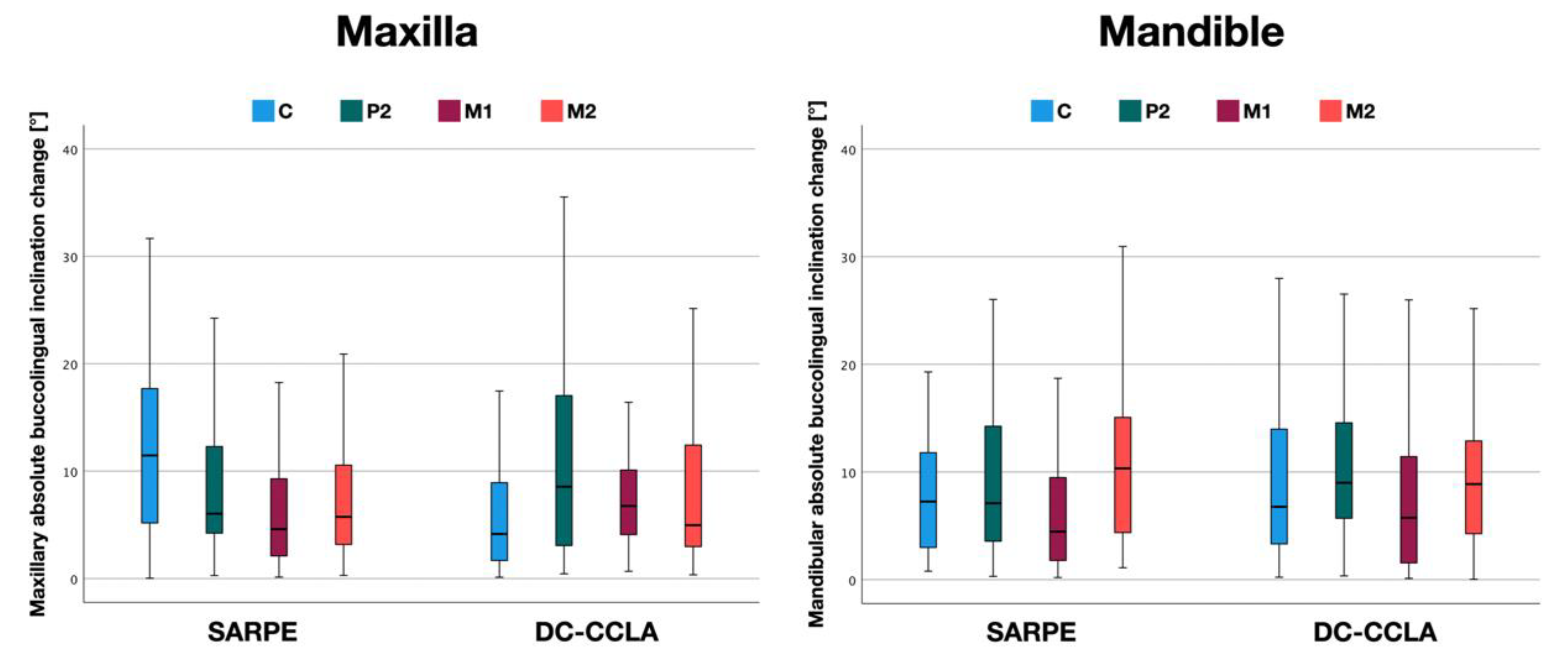
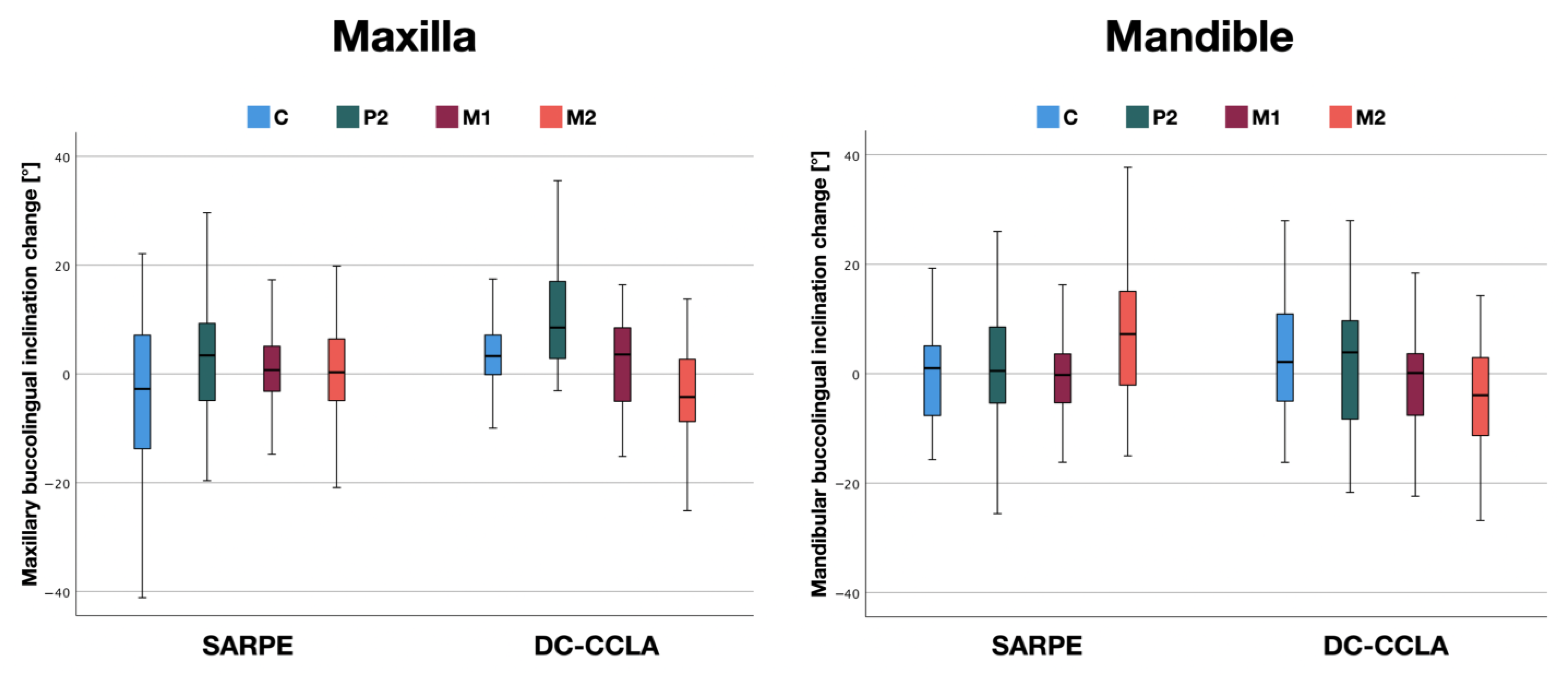
3.1. Buccolingual Inclination Change in the Maxilla
3.2. Buccolingual Inclination Change in the Mandible
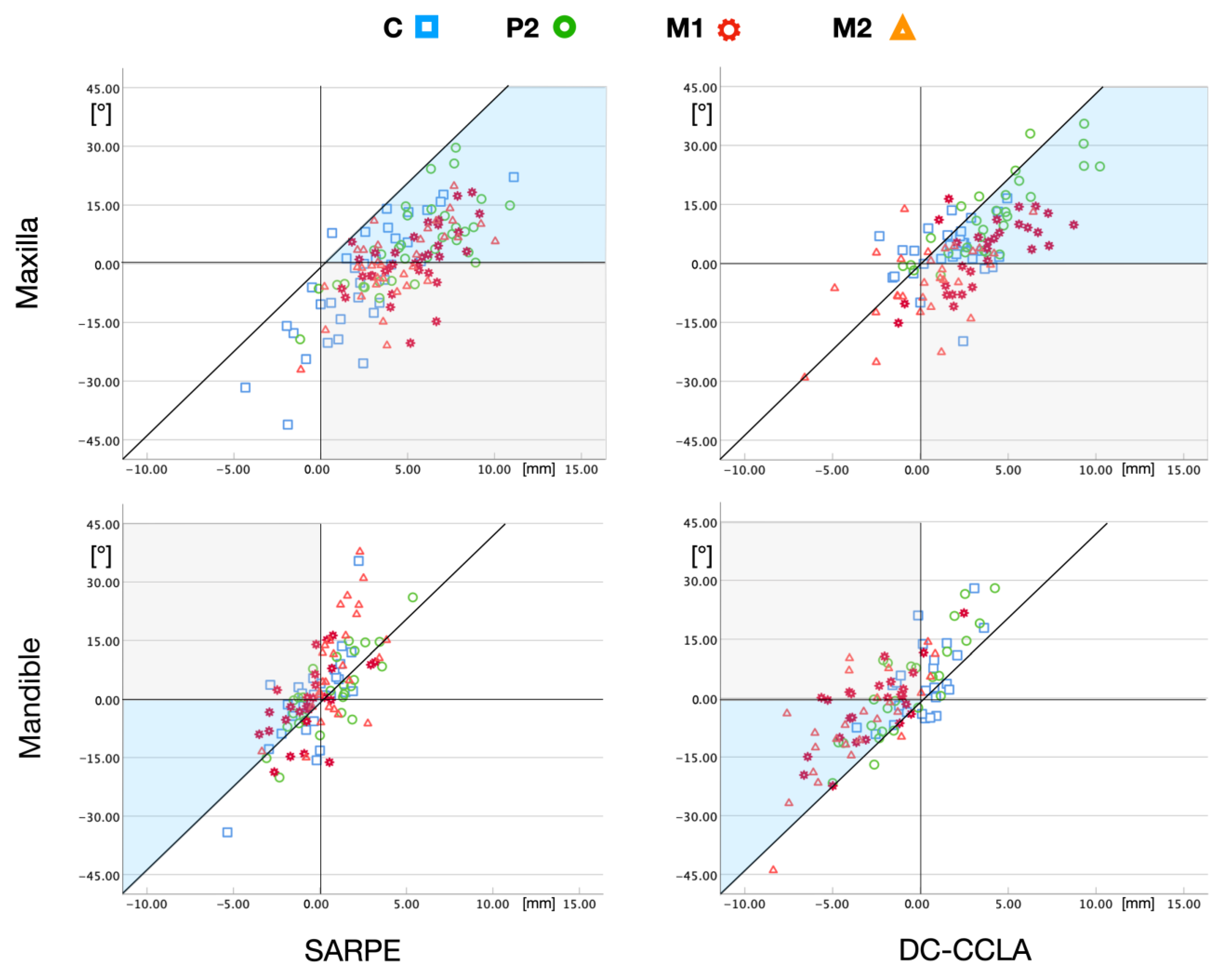
3.3. Description of Tooth Movements in the Maxilla
3.4. Description of Tooth Movements in the Mandible
4. Discussion
Strength and Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Holberg, C. Effects of Rapid Maxillary Expansion on the Cranial Base—An FEM-Analysis. J. Orofac. Orthop. 2005, 66, 54–66. [Google Scholar] [CrossRef] [PubMed]
- Suri, L.; Taneja, P. Surgically Assisted Rapid Palatal Expansion: A Literature Review. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 290–302. [Google Scholar] [CrossRef] [PubMed]
- Habersack, K.; Becker, J.; Ristow, O.; Paulus, G.W. Dental and Skeletal Effects of Two-Piece and Three-Piece Surgically Assisted Rapid Maxillary Expansion with Complete Mobilization: A Retrospective Cohort Study. J. Oral Maxillofac. Surg. 2014, 72, 2278–2288. [Google Scholar] [CrossRef] [PubMed]
- Hamedi Sangsari, A.; Sadr-Eshkevari, P.; Al-Dam, A.; Friedrich, R.E.; Freymiller, E.; Rashad, A. Surgically Assisted Rapid Palatomaxillary Expansion with or Without Pterygomaxillary Disjunction: A Systematic Review and Meta-Analysis. J. Oral Maxillofac. Surg. 2016, 74, 338–348. [Google Scholar] [CrossRef] [PubMed]
- Ferraro-Bezerra, M.; Tavares, R.N.; de Medeiros, J.R.; Nogueira, A.S.; Avelar, R.L.; Studart Soares, E.C. Effects of Pterygomaxillary Separation on Skeletal and Dental Changes After Surgically Assisted Rapid Maxillary Expansion: A Single-Center, Double-Blind, Randomized Clinical Trial. J. Oral Maxillofac. Surg. 2018, 76, 844–853. [Google Scholar] [CrossRef] [PubMed]
- Koudstaal, M.J.; Wolvius, E.B.; Schulten, A.J.M.; Hop, W.C.J.; van der Wal, K.G.H. Stability, Tipping and Relapse of Bone-Borne versus Tooth-Borne Surgically Assisted Rapid Maxillary Expansion; a Prospective Randomized Patient Trial. Int. J. Oral Maxillofac. Surg. 2009, 38, 308–315. [Google Scholar] [CrossRef]
- Blæhr, T.L.; Mommaerts, M.Y.; Kjellerup, A.D.; Starch-Jensen, T. Surgically Assisted Rapid Maxillary Expansion with Bone-Borne versus Tooth-Borne Distraction Appliances—A Systematic Review. Int. J. Oral Maxillofac. Surg. 2019, 48, 492–501. [Google Scholar] [CrossRef]
- Gogna, N.; Johal, A.S.; Sharma, P.k. The Stability of Surgically Assisted Rapid Maxillary Expansion (SARME): A Systematic Review. J. Cranio-Maxillofac. Surg. 2020, 48, 845–852. [Google Scholar] [CrossRef]
- Bortolotti, F.; Solidoro, L.; Bartolucci, M.L.; Incerti Parenti, S.; Paganelli, C.; Alessandri-Bonetti, G. Skeletal and Dental Effects of Surgically Assisted Rapid Palatal Expansion: A Systematic Review of Randomized Controlled Trials. Eur. J. Orthod. 2020, 42, 434–440. [Google Scholar] [CrossRef]
- Marchetti, C.; Pironi, M.; Bianchi, A.; Musci, A. Surgically Assisted Rapid Palatal Expansion vs. Segmental Le Fort I Osteotomy: Transverse Stability over a 2-Year Period. J. Cranio-Maxillofac. Surg. 2009, 37, 74–78. [Google Scholar] [CrossRef]
- Seeberger, R.; Gander, E.; Hoffmann, J.; Engel, M. Surgical Management of Cross-Bites in Orthognathic Surgery: Surgically Assisted Rapid Maxillary Expansion (SARME) versus Two-Piece Maxilla. J. Cranio-Maxillofac. Surg. 2015, 43, 1109–1112. [Google Scholar] [CrossRef]
- Phillips, C.; Medland, W.H.; Fields, H.W.; Proffit, W.R.; White, R.P. Stability of Surgical Maxillary Expansion. Int. J. Adult Orthodon. Orthognath. Surg. 1992, 7, 139–146. [Google Scholar] [PubMed]
- Brandtner, C.; Hachleitner, J.; Rippel, C.; Krenkel, C.; Gaggl, A. Long-Term Skeletal and Dental Stability after Orthognathic Surgery of the Maxillo-Mandibular Complex in Class II Patients with Transverse Discrepancies. J. Cranio-Maxillofac. Surg. 2015, 43, 1516–1521. [Google Scholar] [CrossRef]
- Proffit, W.R.; Turvey, T.A.; Phillips, C. The Hierarchy of Stability and Predictability in Orthognathic Surgery with Rigid Fixation: An Update and Extension. Head Face Med. 2007, 3, 21. [Google Scholar] [CrossRef] [PubMed]
- Haas Junior, O.L.; Guijarro-Martínez, R.; de Sousa Gil, A.P.; da Silva Meirelles, L.; de Oliveira, R.B.; Hernández-Alfaro, F. Stability and Surgical Complications in Segmental Le Fort I Osteotomy: A Systematic Review. Int. J. Oral Maxillofac. Surg. 2017, 46, 1071–1087. [Google Scholar] [CrossRef]
- Colak, O.; Paredes, N.A.; Elkenawy, I.; Torres, M.; Bui, J.; Jahangiri, S.; Moon, W. Tomographic Assessment of Palatal Suture Opening Pattern and Pterygopalatine Suture Disarticulation in the Axial Plane after Midfacial Skeletal Expansion. Prog. Orthod. 2020, 21, 21. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira, C.B.; Ayub, P.; Ledra, I.M.; Murata, W.H.; Suzuki, S.S.; Ravelli, D.B.; Santos-Pinto, A. Microimplant Assisted Rapid Palatal Expansion vs Surgically Assisted Rapid Palatal Expansion for Maxillary Transverse Discrepancy Treatment. Am. J. Orthod. Dentofac. Orthop. 2021, 159, 733–742. [Google Scholar] [CrossRef] [PubMed]
- Kapetanović, A.; Theodorou, C.I.; Bergé, S.J.; Schols, J.G.J.H.; Xi, T. Efficacy of Miniscrew-Assisted Rapid Palatal Expansion (MARPE) in Late Adolescents and Adults: A Systematic Review and Meta-Analysis. Eur. J. Orthod. 2021, 43, 313–323. [Google Scholar] [CrossRef]
- Betts, N.J.; Vanarsdall, R.L.; Barber, H.D.; Higgins-Barber, K.; Fonseca, R.J. Diagnosis and Treatment of Transverse Maxillary Deficiency. Int. J. Adult Orthodon. Orthognath. Surg. 1995, 10, 75–96. [Google Scholar]
- Silverstein, K.; Quinn, P.D. Surgically-Assisted Rapid Palatal Expansion for Management of Transverse Maxillary Deficiency. J. Oral Maxillofac. Surg. 1997, 55, 725–727. [Google Scholar] [CrossRef]
- Handelman, C.S.; Wang, L.; BeGole, E.A.; Haas, A.J. Nonsurgical Rapid Maxillary Expansion in Adults: Report on 47 Cases Using the Haas Expander. Angle Orthod. 2000, 70, 129–144. [Google Scholar] [CrossRef] [PubMed]
- Ghergu Jianu, A.; Chaqués-Asensi, J.; Llamas Carreras, J.M.; Perillo, L. Nonsurgical Maxillary Expansion in Adults: Report on Clinical Cases Using the Hyrax Expander. Minerva Stomatol. 2019, 68, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Habersack, K.; Karoglan, A.; Sommer, B.; Benner, K.U. High-Resolution Multislice Computerized Tomography with Multiplanar and 3-Dimensional Reformation Imaging in Rapid Palatal Expansion. Am. J. Orthod. Dentofac. Orthop. 2007, 131, 776–781. [Google Scholar] [CrossRef] [PubMed]
- Ugolini, A.; Agostino, P.; Silvestrini-Biavati, A.; Harrison, J.E.; Batista, K.B.S.L. Orthodontic Treatment for Posterior Crossbites. Cochrane Database Syst. Rev. 2021, 2021. [Google Scholar] [CrossRef]
- Little, R.M. Stability and Relapse of Mandibular Anterior Alignment: University of Washington Studies. Semin. Orthod. 1999, 5, 191–204. [Google Scholar] [CrossRef] [PubMed]
- Jung, S.K.; Kim, T.W. Treatment of Unilateral Posterior Crossbite with Facial Asymmetry in a Female Patient with Transverse Discrepancy. Am. J. Orthod. Dentofac. Orthop. 2015, 148, 154–164. [Google Scholar] [CrossRef]
- Liu, R.; Xiaoqing, M.; Wamalwa, P.; Zou, S.J. Nonsurgical Treatment of an Adult Patient with Bilateral Posterior Crossbite. Am. J. Orthod. Dentofac. Orthop. 2011, 140, 106–114. [Google Scholar] [CrossRef]
- Alexander, C.D.; Bloomquist, D.S.; Wallen, T.R. Stability of Mandibular Constriction with a Symphyseal Osteotomy. Am. J. Orthod. Dentofac. Orthop. 1993, 103, 15–23. [Google Scholar] [CrossRef]
- Schmid, J.Q.; Gerberding, E.; Hohoff, A.; Kleinheinz, J.; Stamm, T.; Middelberg, C. Non-Surgical Transversal Dentoalveolar Compensation with Completely Customized Lingual Appliances versus Surgically Assisted Rapid Palatal Expansion in Adults—The Amount of Posterior Crossbite Correction. J. Pers. Med. 2022, 12, 1893. [Google Scholar] [CrossRef]
- Andrews, L.F. The Six Keys to Normal Occlusion. Am. J. Orthod. 1972, 62, 296–309. [Google Scholar] [CrossRef]
- Dathe, H.; Nägerl, H.; Kubein-Meesenburg, D. A Caveat Concerning Center of Resistance. J. Dent. Biomech. 2013, 4, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Gandhi, V.; Luu, B.; Dresner, R.; Pierce, D.; Upadhyay, M. Where Is the Center of Resistance of a Maxillary First Molar? A 3-Dimensional Finite Element Analysis. Am. J. Orthod. Dentofac. Orthop. 2021, 160, 442–450.e1. [Google Scholar] [CrossRef] [PubMed]
- Burstone, C.J.; Pryputniewicz, R.J. Holographic Determination of Centers of Rotation Produced by Orthodontic Forces. Am. J. Orthod. 1980, 77, 396–409. [Google Scholar] [CrossRef] [PubMed]
- Tanne, K.; Koenig, H.A.; Burstone, C.J. Moment to Force Ratios and the Center of Rotation. Am. J. Orthod. Dentofac. Orthop. 1988, 94, 426–431. [Google Scholar] [CrossRef]
- Oh, M.B.; Mo, S.S.; Hwang, C.J.; Chung, C.; Kang, J.M.; Lee, K.J. The 3-Dimensional Zone of the Center of Resistance of the Mandibular Posterior Teeth Segment. Am. J. Orthod. Dentofac. Orthop. 2019, 156, 365–374. [Google Scholar] [CrossRef]
- Jiang, F.; Kula, K.; Chen, J. Estimating the Location of the Center of Resistance of Canines. Angle Orthod. 2016, 86, 365–371. [Google Scholar] [CrossRef]
- Volchansky, A.; Cleaton-Jones, P.; Fatti, L.P. A Technique for Computer Plotting of Clinical Crown Height Derived from Orthodontic Study Models. J. Dent. 1981, 9, 150–156. [Google Scholar] [CrossRef]
- Volchansky, A.; Cleaton-Jones, P. Clinical Crown Height (Length)—A Review of Published Measurements. J. Clin. Periodontol. 2001, 28, 1085–1090. [Google Scholar] [CrossRef]
- Kim, S.Y.; Lim, S.H.; Gang, S.N.; Kim, H.J. Crown and Root Lengths of Incisors, Canines, and Premolars Measured by Cone-Beam Computed Tomography in Patients with Malocclusions. Korean J. Orthod. 2013, 43, 271–278. [Google Scholar] [CrossRef]
- Xu, Y.Q.; Lin, J.Q.; Guan, W.Q. Cone-Beam Computed Tomography Study of the Incidence and Characteristics of the Second Mesiobuccal Canal in Maxillary Permanent Molars. Front. Physiol. 2022, 13, 1–9. [Google Scholar] [CrossRef]
- Hamasni, F.M.; El Hajj, F. Comparison of the Clinical Biological Width with the Published Standard Histologic Mean Values. J. Int. Soc. Prev. Community Dent. 2017, 7, 264–271. [Google Scholar] [CrossRef] [PubMed]
- Dahlberg, G. Statistical Methods for the Medical and Biological Students; Allen and Unwin: Sydney, Australia, 1940. [Google Scholar]
- Handelman, C. Palatal Expansion in Adults: The Nonsurgical Approach. Am. J. Orthod. Dentofac. Orthop. 2011, 140, 462–468. [Google Scholar] [CrossRef] [PubMed]
- Kayalar, E.; Schauseil, M.; Kuvat, S.V.; Emekli, U.; Firatli, S. Comparison of Tooth-Borne and Hybrid Devices in Surgically Assisted Rapid Maxillary Expansion: A Randomized Clinical Cone-Beam Computed Tomography Study. J. Cranio-Maxillofac. Surg. 2016, 44, 285–293. [Google Scholar] [CrossRef]
- Deeb, W.; Hansen, L.; Hotan, T.; Hietschold, V.; Harzer, W.; Tausche, E. Changes in Nasal Volume after Surgically Assisted Bone-Borne Rapid Maxillary Expansion. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 782–789. [Google Scholar] [CrossRef] [PubMed]
- Kunz, F.; Linz, C.; Baunach, G.; Böhm, H.; Meyer-Marcotty, P. Expansion Patterns in Surgically Assisted Rapid Maxillary Expansion: Transpalatal Distractor versus Hyrax Appliance. J. Orofac. Orthop. 2016, 77, 357–365. [Google Scholar] [CrossRef]
- Braun, S.; Hnat, W.P.; Leschinsky, R.; Legan, H.L. An Evaluation of the Shape of Some Popular Nickel Titanium Alloy Preformed Arch Wires. Am. J. Orthod. Dentofac. Orthop. 1999, 116, 1–12. [Google Scholar] [CrossRef]
- Bhowmik, S.G.; Hazare, P.V.; Bhowmik, H. Correlation of the Arch Forms of Male and Female Subjects with Those of Preformed Rectangular Nickel-Titanium Archwires. Am. J. Orthod. Dentofac. Orthop. 2012, 142, 364–373. [Google Scholar] [CrossRef]
- Cash, A.C.; Good, S.A.; Curtis, R.V.; McDonald, F. An Evaluation of Slot Size in Orthodontic Brackets—Are Standards as Expected? Angle Orthod. 2004, 74, 450–453. [Google Scholar] [CrossRef]
- De la Cruz, A.; Sampson, P.; Little, R.M.; Årtun, J.; Shapiro, P.A. Long-Term Changes in Arch Form after Orthodontic Treatment and Retention. Am. J. Orthod. Dentofac. Orthop. 1995, 107, 518–530. [Google Scholar] [CrossRef]
- Thilander, B.; Lennartsson, B. A Study of Children with Unilateral Posterior Crossbite, Treated and Untreated, in the Deciduous Dentition. Occlusal and Skeletal Characteristics of Significance in Predicting the Long-Term Outcome. J. Orofac. Orthop. 2002, 63, 371–383. [Google Scholar] [CrossRef]
- Bartzela, T.; Jonas, I. Long-Term Stability of Unilateral Posterior Crossbite Correction. Angle Orthod. 2007, 77, 237–243. [Google Scholar] [CrossRef] [PubMed]
- Bishara, S.E.; Jakobsen, J.R.; Treder, J.; Nowak, A. Arch Width Changes from 6 Weeks to 45 Years of Age. Am. J. Orthod. Dentofac. Orthop. 1997, 111, 401–409. [Google Scholar] [CrossRef] [PubMed]
- Cattaneo, P.M.; Treccani, M.; Carlsson, K.; Thorgeirsson, T.; Myrda, A.; Cevidanes, L.H.S.; Melsen, B. Transversal Maxillary Dento-Alveolar Changes in Patients Treated with Active and Passive Self-Ligating Brackets: A Randomized Clinical Trial Using CBCT-Scans and Digital Models. Orthod. Craniofacial Res. 2011, 14, 222–233. [Google Scholar] [CrossRef]
- Quinn, R.S.; Yoshikawa, D.K. A Reassessment of Force Magnitude in Orthodontics. Am. J. Orthod. 1985, 88, 252–260. [Google Scholar] [CrossRef] [PubMed]
- Kraus, C.D.; Campbell, P.M.; Spears, R.; Taylor, R.W.; Buschang, P.H. Bony Adaptation after Expansion with Light-to-Moderate Continuous Forces. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 655–666. [Google Scholar] [CrossRef]
- Capps, C.J.; Campbell, P.M.; Benson, B.; Buschang, P.H. Can Posterior Teeth of Patients Be Translated Buccally, and Does Bone Form on the Buccal Surface in Response? Angle Orthod. 2016, 86, 527–534. [Google Scholar] [CrossRef]
- Ruf, S.; Pancherz, H. Herbst/Multibracket Appliance Treatment of Class II Division 1 Malocclusions in Early and Late Adulthood. A Prospective Cephalometric Study of Consecutively Treated Subjects. Eur. J. Orthod. 2006, 28, 352–360. [Google Scholar] [CrossRef]
- Bock, N.C.; Ruf, S.; Wiechmann, D.; Jilek, T. Dentoskeletal Effects during Herbst-Multibracket Appliance Treatment: A Comparison of Lingual and Labial Approaches. Eur. J. Orthod. 2016, 38, 470–477. [Google Scholar] [CrossRef]


| SARPE | DC-CCLA | p | |
|---|---|---|---|
| Female | 19 (44%) | 25 (66%) | |
| Age (years) at T0 | 26.7 ± 9.7 | 32.1 ± 12.3 | 0.086 |
| Age (years) at T1 | 30.1 ± 9.6 | 34.4 ± 12.4 | 0.255 |
| Male | 24 (56%) | 13 (34%) | |
| Age (years) at T0 | 27.8 ± 9.8 | 27.0 ± 14.2 | 0.404 |
| Age (years) at T1 | 30.9 ± 9.5 | 30.0 ± 14.4 | 0.276 |
| Angle class I | 1 | 20 | |
| Angle class II | 14 | 13 | |
| Angle class III | 28 | 5 |
| Jaw | Tooth | SARPE | DC-CCLA | p | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | 95% CI | Min | Max | M | SD | 95% CI | Min | Max | ||||
| Mx | C | 12.21 | 9.40 | 9.21–15.21 | 0.03 | 41.13 | 6.40 | 5.91 | 4.45–8.34 | 0.12 | 23.74 | 0.005 | |
| P2 | 8.79 | 7.16 | 6.47–11.11 | 0.28 | 29.65 | 11.60 | 9.99 | 8.06–15.14 | 0.44 | 35.53 | 0.416 | ||
| M1 | 6.50 | 6.11 | 4.52–8.48 | 0.13 | 25.31 | 7.33 | 4.27 | 5.86–8.80 | 0.67 | 16.41 | 0.156 | ||
| M2 | 7.47 | 6.34 | 5.41–9.52 | 0.29 | 27.09 | 8.25 | 7.45 | 5.61–10.90 | 0.35 | 29.07 | 0.804 | ||
| Md | C | 8.24 | 7.69 | 5.81–10.67 | 0.78 | 35.37 | 8.57 | 6.76 | 6.35–10.80 | 0.22 | 27.99 | 0.573 | |
| P2 | 8.68 | 6.78 | 6.35–11.01 | 0.30 | 26.03 | 10.67 | 7.45 | 7.84–13.50 | 0.35 | 28.02 | 0.202 | ||
| M1 | 6.45 | 5.72 | 4.45–8.45 | 0.20 | 18.70 | 8.18 | 7.64 | 5.22–11.15 | 0.12 | 25.99 | 0.515 | ||
| M2 | 11.74 | 9.11 | 8.57–14.93 | 1.11 | 37.73 | 10.47 | 9.23 | 7.09–13.85 | 0.03 | 43.96 | 0.478 | ||
| Jaw | Tooth | SARPE | DC-CCLA | p | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | 95% CI | Min | Max | M | SD | 95% CI | Min | Max | ||||
| Mx | C | −4.47 | 14.86 | −9.22–0.28 | −41.13 | 22.14 | 3.99 | 7.78 | 1.43–6.55 | −19.80 | 23.74 | 0.006 | |
| P2 | 3.59 | 10.83 | 0.08–7.10 | −19.63 | 29.65 | 11.13 | 10.52 | 7.40–14.86 | −3.07 | 35.53 | 0.007 | ||
| M1 | 0.28 | 8.98 | −2.63–3.19 | −25.31 | 18.25 | 2.20 | 8.28 | −0.64–5.05 | −15.16 | 16.41 | 0.398 | ||
| M2 | −0.07 | 9.87 | −3.26–3.13 | −27.09 | 19.84 | −4.94 | 10.03 | −8.50–−1.39 | −29.07 | 13.79 | 0.029 | ||
| Md | C | −0.59 | 11.33 | −4.16–2.99 | −34.17 | 35.37 | 2.99 | 10.59 | −0.49–6.46 | −16.20 | 27.99 | 0.185 | |
| P2 | 1.01 | 11.07 | −2.79–4.81 | −25.55 | 26.03 | 3.06 | 12.80 | −1.81–7.93 | −21.68 | 28.02 | 0.651 | ||
| M1 | −0.74 | 8.66 | −3.77–2.28 | −18.70 | 16.26 | −0.41 | 11.30 | −4.79–3.98 | −22.39 | 25.99 | 0.944 | ||
| M2 | 7.92 | 12.67 | 3.50–12.34 | −14.99 | 37.73 | −4.86 | 13.19 | −9.69–−0.02 | −43.96 | 25.18 | <0.001 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schmid, J.Q.; Gerberding, E.; Hohoff, A.; Kleinheinz, J.; Stamm, T.; Middelberg, C. Non-Surgical Transversal Dentoalveolar Compensation with Completely Customized Lingual Appliances versus Surgically Assisted Rapid Palatal Expansion in Adults—Tipping or Translation in Posterior Crossbite Correction? J. Pers. Med. 2023, 13, 807. https://doi.org/10.3390/jpm13050807
Schmid JQ, Gerberding E, Hohoff A, Kleinheinz J, Stamm T, Middelberg C. Non-Surgical Transversal Dentoalveolar Compensation with Completely Customized Lingual Appliances versus Surgically Assisted Rapid Palatal Expansion in Adults—Tipping or Translation in Posterior Crossbite Correction? Journal of Personalized Medicine. 2023; 13(5):807. https://doi.org/10.3390/jpm13050807
Chicago/Turabian StyleSchmid, Jonas Q., Elena Gerberding, Ariane Hohoff, Johannes Kleinheinz, Thomas Stamm, and Claudius Middelberg. 2023. "Non-Surgical Transversal Dentoalveolar Compensation with Completely Customized Lingual Appliances versus Surgically Assisted Rapid Palatal Expansion in Adults—Tipping or Translation in Posterior Crossbite Correction?" Journal of Personalized Medicine 13, no. 5: 807. https://doi.org/10.3390/jpm13050807
APA StyleSchmid, J. Q., Gerberding, E., Hohoff, A., Kleinheinz, J., Stamm, T., & Middelberg, C. (2023). Non-Surgical Transversal Dentoalveolar Compensation with Completely Customized Lingual Appliances versus Surgically Assisted Rapid Palatal Expansion in Adults—Tipping or Translation in Posterior Crossbite Correction? Journal of Personalized Medicine, 13(5), 807. https://doi.org/10.3390/jpm13050807







