Prognostic Serum Biomarkers of Inflammaging in Patients Undergoing Emergency Laparotomy
Abstract
1. Introduction
2. Materials and Methods
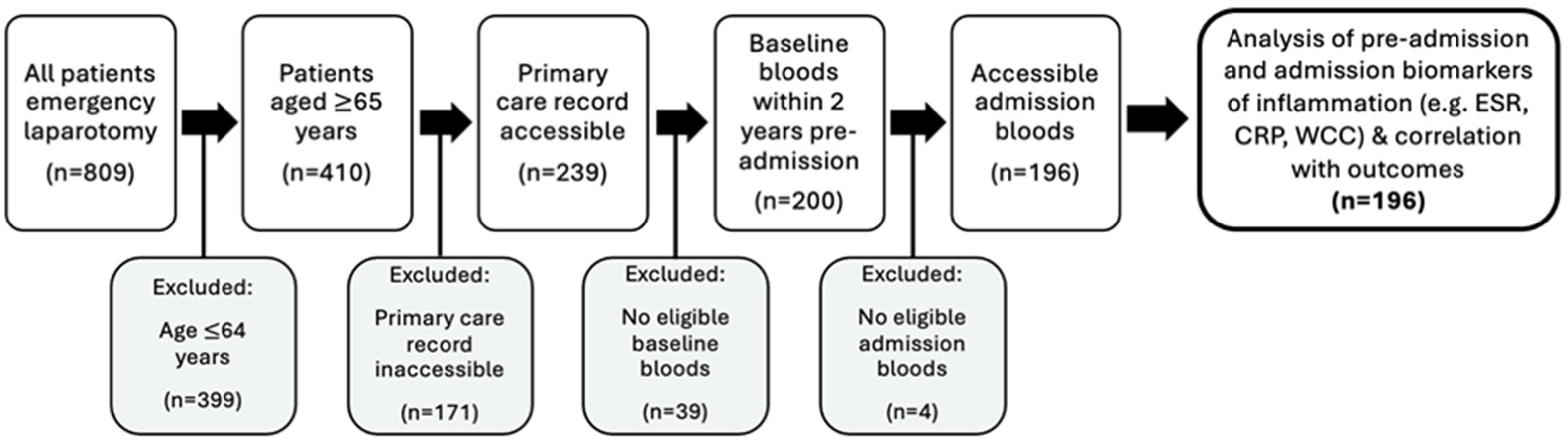
2.1. Participant Selection
2.2. Data Collection and Handling
2.3. Statistical Analysis
2.4. Ethical Statement
3. Results
3.1. Participant Characteristics
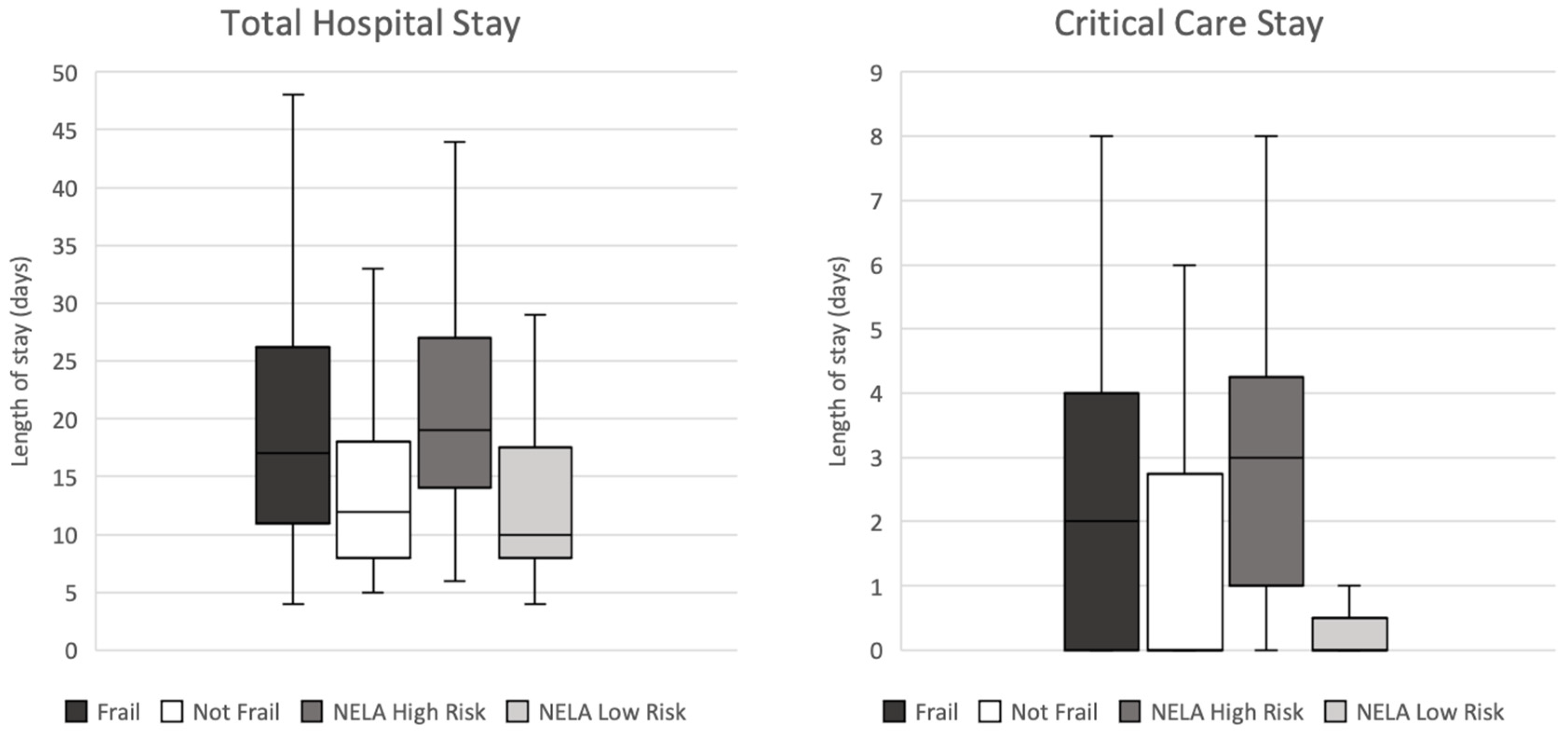
3.2. Clinical Frailty Scale, NELA Risk of Mortality and Actual Mortality
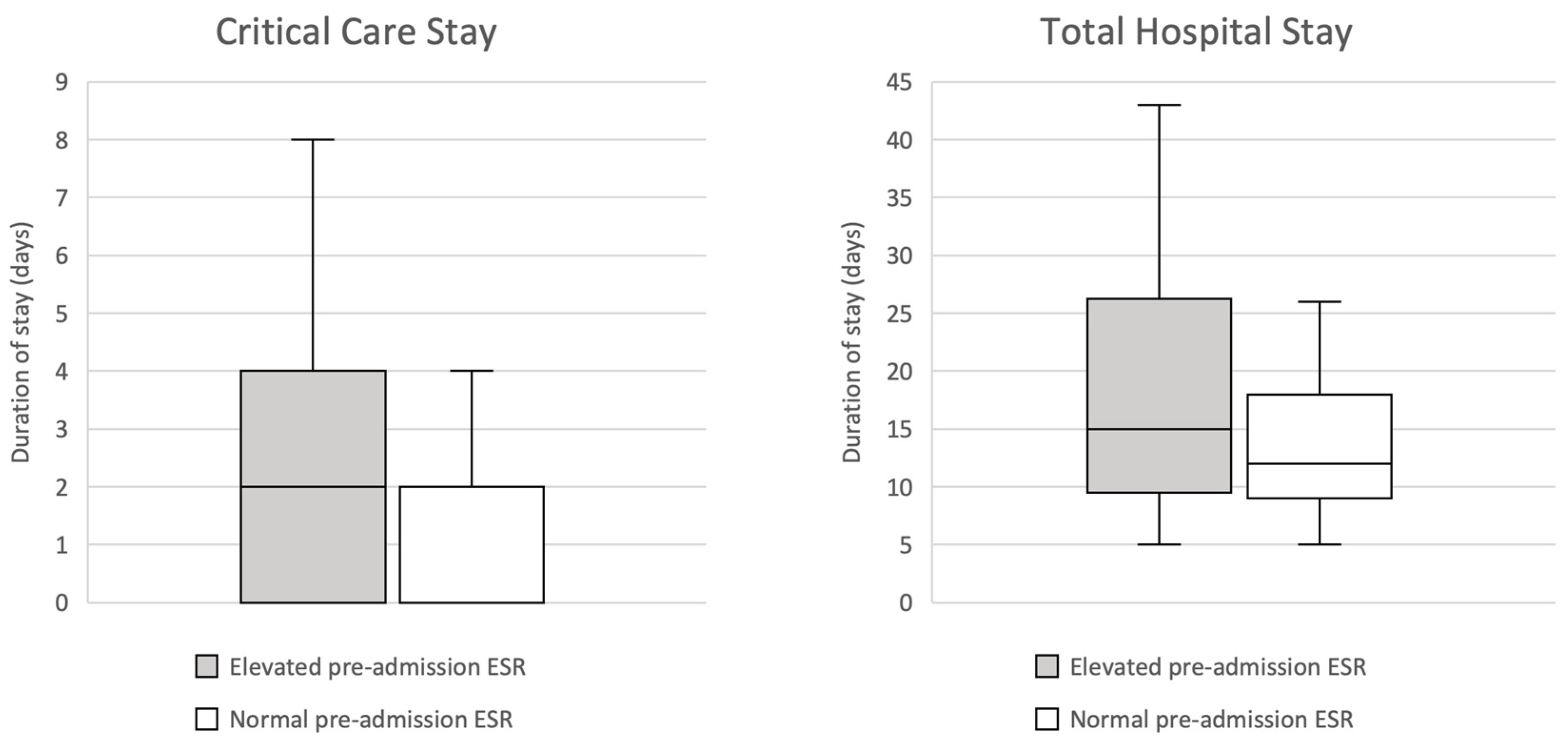
3.3. Erythrocyte Sedimentation Rate
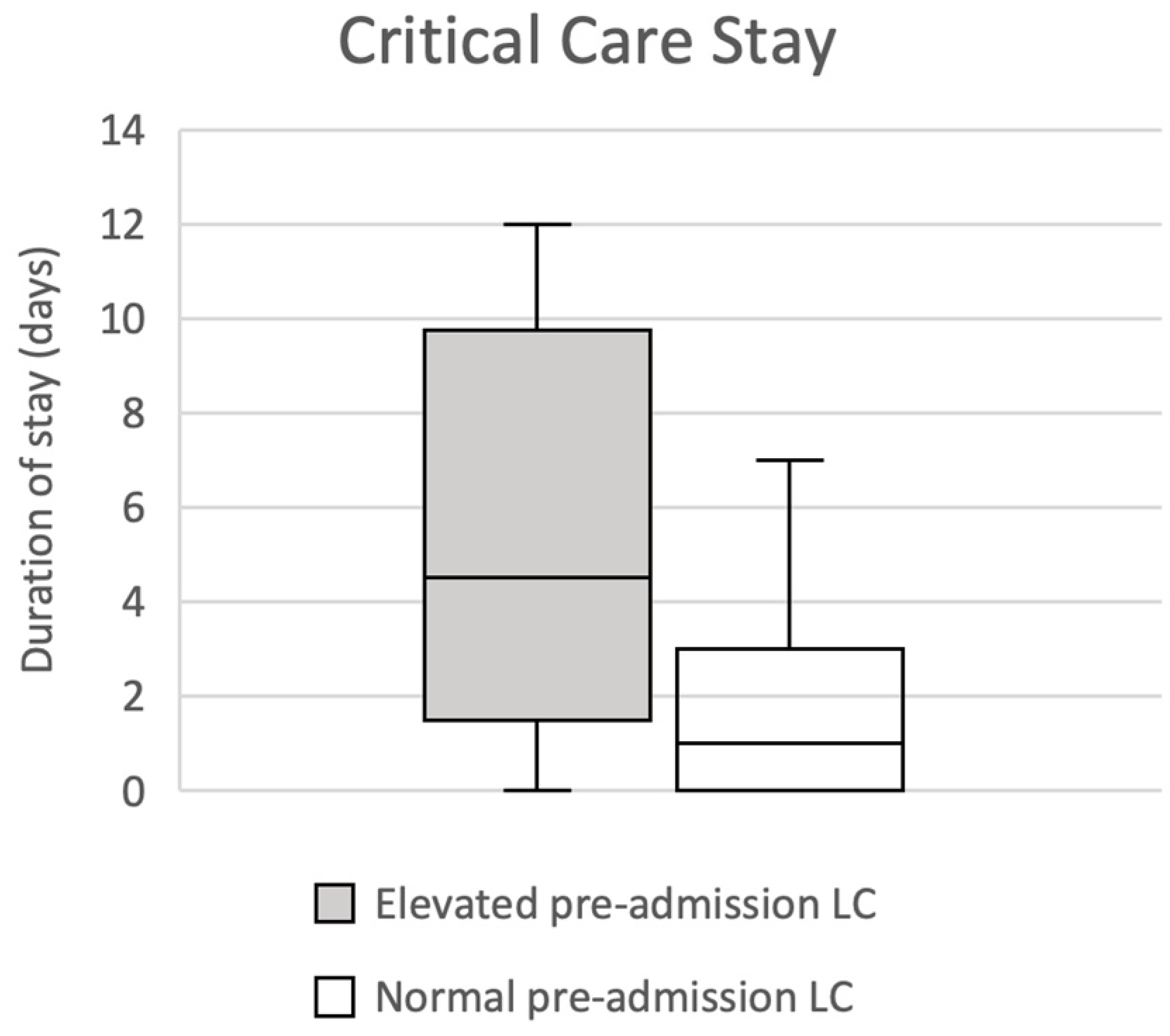
3.4. Lymphocyte Count
3.5. C-Reaction Protein, Total White Cell Count and Neutrophil Count
4. Discussion
4.1. Overview
4.2. Clinical Relevance and Future Application
4.3. C-Reactive Protein and Erythrocyte Sedimentation Rate
4.4. Inflammaging in Surgery
4.5. Limitations and Further Considerations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Xue, Q.-L. The frailty syndrome: Definition and natural history. Clin. Geriatr. Med. 2011, 27, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Parmar, K.L.; Law, J.; Carter, B.; Hewitt, J.; Boyle, J.M.; Casey, P.; Maitra, I.; Farrell, I.S.; Pearce, L.; Moug, S.J.; et al. Frailty in Older Patients Undergoing Emergency Laparotomy: Results From the UK Observational Emergency Laparotomy and Frailty (ELF) Study. Ann. Surg. 2021, 273, 709–718. [Google Scholar] [CrossRef] [PubMed]
- Green, G.; Shaikh, I.; Fernandes, R.; Wegstapel, H. Emergency laparotomy in octogenarians: A 5-year study of morbidity and mortality. World J. Gastrointest Surg 2013, 5, 216–221. [Google Scholar] [CrossRef] [PubMed]
- Church, S.; Rogers, E.; Rockwood, K.; Theou, O. A scoping review of the Clinical Frailty Scale. BMC Geriatr. 2020, 20, 393. [Google Scholar] [CrossRef] [PubMed]
- Thahir, A.; Pinto-Lopes, R.; Madenlidou, S.; Daby, L.; Halahakoon, C. Mortality risk scoring in emergency general surgery: Are we using the best tool? J. Perioper. Pract. 2021, 31, 153–158. [Google Scholar] [CrossRef]
- Eugene, N.; Oliver, C.M.; Bassett, M.G.; Poulton, T.E.; Kuryba, A.; Johnston, C.; Anderson, I.D.; Moonesinghe, S.R.; Grocott, M.P.; Murray, D.M.; et al. Development and internal validation of a novel risk adjustment model for adult patients undergoing emergency laparotomy surgery: The National Emergency Laparotomy Audit risk model. Br. J. Anaesth. 2018, 121, 739–748. [Google Scholar] [CrossRef]
- Darbyshire, A.R.; Kostakis, I.; Pucher, P.H.; Prytherch, D.; Mercer, S.J. P-POSSUM and the NELA Score Overpredict Mortality for Laparoscopic Emergency Bowel Surgery: An Analysis of the NELA Database. World J. Surg. 2022, 46, 552–560. [Google Scholar] [CrossRef]
- Ferrucci, L.; Fabbri, E. Inflammageing: Chronic inflammation in ageing, cardiovascular disease, and frailty. Nat. Rev. Cardiol. 2018, 15, 505–522. [Google Scholar] [CrossRef]
- Franceschi, C.; Campisi, J. Chronic Inflammation (Inflammaging) and Its Potential Contribution to Age-Associated Diseases. J. Gerontol. Ser. A 2014, 69, S4–S9. [Google Scholar] [CrossRef]
- Yende, S.; Kellum, J.A.; Talisa, V.B.; Peck Palmer, O.M.; Chang, C.-C.H.; Filbin, M.R.; Shapiro, N.I.; Hou, P.C.; Venkat, A.; LoVecchio, F.; et al. Long-term Host Immune Response Trajectories Among Hospitalized Patients with Sepsis. JAMA Netw. Open 2019, 2, e198686. [Google Scholar] [CrossRef]
- Simpson, G.; Saunders, R.; Wilson, J.; Magee, C. The role of the neutrophil:lymphocyte ratio (NLR) and the CRP:albumin ratio (CAR) in predicting mortality following emergency laparotomy in the over 80 age group. Eur. J. Trauma Emerg. Surg. 2018, 44, 877–882. [Google Scholar] [CrossRef]
- Man, W.; Lin, H.; Liu, Z.; Jin, L.; Wang, J.; Zhang, J.; Bai, Z.; Yao, H.; Zhang, Z.; Deng, W. Usefulness of Inflammation-Based Prognostic Scores for Predicting the Risk of Complications after Radical Resection of Colorectal Carcinoma. Cancer Manag. Res. 2020, 12, 1029–1038. [Google Scholar] [CrossRef]
- Microsoft. Microsoft Excel; Microsoft Corp.: Washington, WA, USA, 2018; Available online: https://office.microsoft.com/excel (accessed on 6 January 2023).
- IBM. SPSS Statistics, Version 28; IBM Corp.: New York, NY, USA, 2021; Available online: https://www.ibm.com/uk-en/spss (accessed on 6 January 2023).
- Ahmed, A.; Azim, A. Emergency Laparotomies: Causes, Pathophysiology, and Outcomes. Indian J. Crit. Care Med. 2020, 24, S183–S189. [Google Scholar]
- Watson, J.; Round, A.; Hamilton, W. Raised inflammatory markers. BMJ 2012, 344, e454. [Google Scholar] [CrossRef]
- Salazar, J.; Martínez, M.S.; Chávez-Castillo, M.; Núñez, V.; Añez, R.; Torres, Y.; Toledo, A.; Chacín, M.; Silva, C.; Pacheco, E.; et al. C-Reactive Protein: An In-Depth Look into Structure, Function, and Regulation. Int. Sch. Res. Not. 2014, 2014, 653045. [Google Scholar] [CrossRef]
- Sproston, N.R.; Ashworth, J.J. Role of C-Reactive Protein at Sites of Inflammation and Infection. Front. Immunol. 2018, 9, 754. [Google Scholar] [CrossRef]
- Harrison, M. Erythrocyte sedimentation rate and C-reactive protein. Aust Prescr 2015, 38, 93–94. [Google Scholar] [CrossRef]
- Bray, C.; Bell, L.N.; Liang, H.; Haykal, R.; Kaiksow, F.; Mazza, J.J.; Yale, S.H. Erythrocyte Sedimentation Rate and C-reactive Protein Measurements and Their Relevance in Clinical Medicine. Wmj 2016, 115, 317–321. [Google Scholar]
- Tishkowski, K.; Gupta, V. Erythrocyte Sedimentation Rate. Available online: https://www.ncbi.nlm.nih.gov/books/NBK557485/ (accessed on 18 March 2023).
- Lapić, I.; Padoan, A.; Bozzato, D.; Plebani, M. Erythrocyte Sedimentation Rate and C-Reactive Protein in Acute Inflammation. Am. J. Clin. Pathol. 2020, 153, 14–29. [Google Scholar] [CrossRef]
- Petring Hasselager, R.; Bang Foss, N.; Andersen, O.; Cihoric, M.; Bay-Nielsen, M.; Nielsen, H.J.; Camilla Andresen, L.; Toft Tengberg, L. Mortality and major complications after emergency laparotomy: A pilot study of risk prediction model development by preoperative blood-based immune parameters. Acta Anaesthesiol. Scand. 2021, 65, 151–161. [Google Scholar] [CrossRef]
- Vaughan-Shaw, P.G.; Rees, J.R.; King, A.T. Neutrophil lymphocyte ratio in outcome prediction after emergency abdominal surgery in the elderly. Int. J. Surg. 2012, 10, 157–162. [Google Scholar] [CrossRef] [PubMed]
- Achanta, A.; Nordestgaard, A.; Kongkaewpaisan, N.; Han, K.; Mendoza, A.; Saillant, N.; Rosenthal, M.; Fagenholz, P.; Velmahos, G.; Kaafarani, H.M.A. Most of the variation in length of stay in emergency general surgery is not related to clinical factors of patient care. J. Trauma Acute Care Surg. 2019, 87, 408–412. [Google Scholar] [CrossRef] [PubMed]
- Ward, T.L.; Raybould, S.J.; Mondal, A.; Lambert, J.; Patel, B. Predicting the length of stay at admission for emergency general surgery patients a cohort study. Ann. Med. Surg. 2021, 62, 127–130. [Google Scholar] [CrossRef] [PubMed]
- Toptas, M.; Sengul Samanci, N.; Akkoc, İ.; Yucetas, E.; Cebeci, E.; Sen, O.; Can, M.M.; Ozturk, S. Factors Affecting the Length of Stay in the Intensive Care Unit: Our Clinical Experience. Biomed. Res. Int. 2018, 2018, 9438046. [Google Scholar] [CrossRef]
- Gholson, J.J.; Noiseux, N.O.; Otero, J.E.; Gao, Y.; Shah, A.S. Patient Factors Systematically Influence Hospital Length of Stay in Common Orthopaedic Procedures. Iowa Orthop. J. 2017, 37, 233–237. [Google Scholar]
| Characteristic | Frequency (Percentage of Total) |
|---|---|
| Gender | |
| Male | 83 (42.3%) |
| Female | 113 (57.7%) |
| Age (years) | |
| 65–74 | 98 (50.0%) |
| 75–84 | 73 (37.2%) |
| 85–94 | 25 (12.8%) |
| Primary clinical feature(s) | |
| Abdominal pain | 148 (75.5%) |
| Nausea +/− vomiting | 72 (36.7%) |
| Constipation | 47 (21.4%) |
| Non-specifically unwell | 15 (7.7%) |
| Abdominal distension | 12 (6.1%) |
| Diarrhoea | 10 (5.1%) |
| Haematochezia or melaena | 6 (3.1%) |
| Diagnosis | |
| Small bowel obstruction | 84 (41.8%) |
| Perforation | 34 (17.3%) |
| Complicated hernia | 29 (14.8%) |
| Large bowel obstruction | 23 (11.7%) |
| Ischaemic colitis | 6 (3.1%) |
| Diverticular disease | 6 (3.1%) |
| Unknown | 5 (2.6%) |
| Volvulus | 2 (1.0%) |
| Appendicitis | 2 (1.0%) |
| Anastomotic leak (following previous surgery) | 2 (1.0%) |
| Colorectal cancer | 2 (1.0%) |
| Bile duct injury (following previous surgery) | 1 (0.5%) |
| Past medical history | |
| Chronic respiratory disease (COPD or asthma) | 52 (26.5%) |
| Hypertension | 101 (51.5%) |
| Ischaemic heart disease | 31 (15.8%) |
| Atrial fibrillation | 28 (14.3%) |
| Inflammatory bowel disease | 9 (4.6%) |
| Diabetes mellitus | 35 (17.9%) |
| Chronic kidney disease | 21 (10.7%) |
| Cerebrovascular disease (stroke or TIA) | 23 (11.7%) |
| Serological Parameter | Outcome | p-Value | Median (Elevated/Non-Elevated) |
|---|---|---|---|
| CRP > 5 | Critical care stay | p = 0.638 | 2 days:2 days |
| Total hospital stay | p = 0.561 | 17 days:17 days | |
| WCC > 11 | Critical care stay | p = 0.115 | 0 days:2 days |
| Total hospital stay | p = 0.065 | 11 days:15 days | |
| NC > 7.5 | Critical care stay | p = 0.325 | 0 days:2 days |
| Total hospital stay | p = 0.336 | 11 days:15 days |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
George, M.; Mukherjee, R. Prognostic Serum Biomarkers of Inflammaging in Patients Undergoing Emergency Laparotomy. J. Pers. Med. 2023, 13, 769. https://doi.org/10.3390/jpm13050769
George M, Mukherjee R. Prognostic Serum Biomarkers of Inflammaging in Patients Undergoing Emergency Laparotomy. Journal of Personalized Medicine. 2023; 13(5):769. https://doi.org/10.3390/jpm13050769
Chicago/Turabian StyleGeorge, Michael, and Rajarshi Mukherjee. 2023. "Prognostic Serum Biomarkers of Inflammaging in Patients Undergoing Emergency Laparotomy" Journal of Personalized Medicine 13, no. 5: 769. https://doi.org/10.3390/jpm13050769
APA StyleGeorge, M., & Mukherjee, R. (2023). Prognostic Serum Biomarkers of Inflammaging in Patients Undergoing Emergency Laparotomy. Journal of Personalized Medicine, 13(5), 769. https://doi.org/10.3390/jpm13050769







