The Sinus Tract in Bone and Joint Infection: Minimally Invasive Salvation or Prolonged Suffering? A Multicenter Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Selection
2.2. Study Assessment
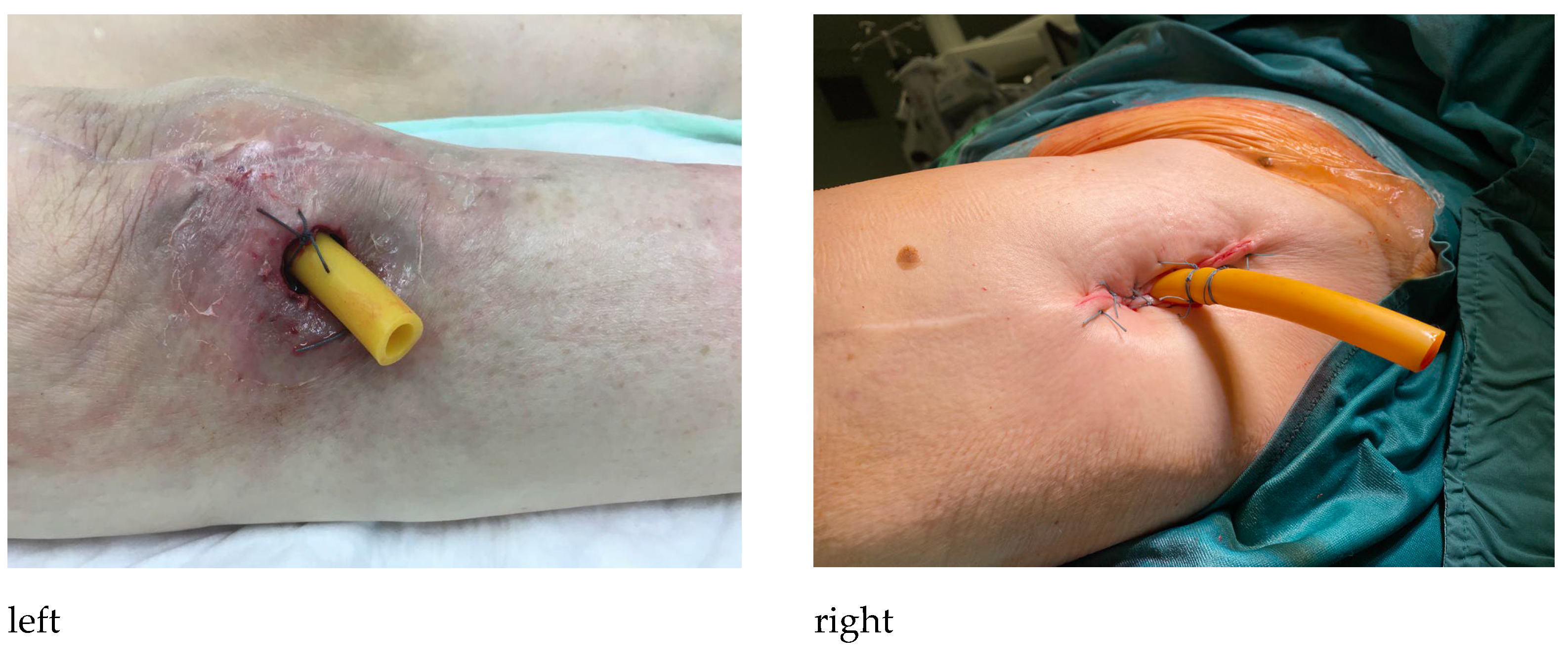
2.3. Iatrogenic Sinus Tract Treatment Technique
2.4. Statistical Analysis
3. Results
3.1. Daily Quality of Life
3.2. Microorganisms
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Born, P.; Ilchmann, T.; Zimmerli, W.; Zwicky, L.; Graber, P.; Ochsner, P.E.; Clauss, M. Eradication of infection, survival, and radiological results of uncemented revision stems in infected total hip arthroplasties. Acta Orthop. 2016, 87, 637–643. [Google Scholar] [CrossRef] [PubMed]
- Svensson, K.; Rolfson, O.; Kärrholm, J.; Mohaddes, M. Similar Risk of Re-Revision in Patients after One- or Two-Stage Surgical Revision of Infected Total Hip Arthroplasty: An Analysis of Revisions in the Swedish Hip Arthroplasty Register 1979–2015. J. Clin. Med. 2019, 8, 485. [Google Scholar] [CrossRef] [PubMed]
- Triantafyllopoulos, G.K.; Memtsoudis, S.G.; Zhang, W.; Ma, Y.; Sculco, T.P.; Poultsides, L.A. Periprosthetic Infection Recurrence after 2-Stage Exchange Arthroplasty: Failure or Fate? J. Arthroplast. 2017, 32, 526–531. [Google Scholar] [CrossRef]
- McNally, M.A.; Ferguson, J.Y.; Lau, A.C.K.; Diefenbeck, M.; Scarborough, M.; Ramsden, A.J.; Atkins, B.L. Single-stage treatment of chronic osteomyelitis with a new absorbable, gentamicin-loaded, calcium sulphate/hydroxyapatite biocomposite: A prospective series of 100 cases. Bone Jt. J. 2016, 98-B, 1289–1296. [Google Scholar] [CrossRef] [PubMed]
- Pincher, B.; Fenton, C.; Jeyapalan, R.; Barlow, G.; Sharma, H.K. A systematic review of the single-stage treatment of chronic osteomyelitis. J. Orthop. Surg. Res. 2019, 14, 393. [Google Scholar] [CrossRef]
- Kurtz, S.; Ong, K.; Lau, E.; Mowat, F.; Halpern, M. Projections of Primary and Revision Hip and Knee Arthroplasty in the United States from 2005 to 2030. J. Bone Jt. Surg. 2007, 89, 780–785. [Google Scholar] [CrossRef]
- Cochran, A.R.; Ong, K.L.; Lau, E.; Mont, M.A.; Malkani, A.L. Risk of Reinfection after Treatment of Infected Total Knee Arthroplasty. J. Arthroplast. 2016, 31 (Suppl. 9), 156–161. [Google Scholar] [CrossRef] [PubMed]
- Kremers, H.M.; Nwojo, M.E.; Ransom, J.E.; Wood-Wentz, C.M.; Melton, L.J.; Huddleston, P.M. Trends in the Epidemiology of Osteomyelitis: A population-based study, 1969 to 2009. J. Bone Jt. Surg. 2015, 97, 837–845. [Google Scholar] [CrossRef] [PubMed]
- Leitner, L.; Posch, F.; Amerstorfer, F.; Sadoghi, P.; Leithner, A.; Glehr, M. The Dark Side of Arthroplasty: Competing Risk Analysis of Failed Hip and Knee Arthroplasty with Periprosthetic Joint Infection. J. Arthroplast. 2020, 35, 2601–2606.e1. [Google Scholar] [CrossRef]
- Carr, J.B., II; Werner, B.; Browne, J.A. Trends and Outcomes in the Treatment of Failed Septic Total Knee Arthroplasty: Comparing Arthrodesis and Above-Knee Amputation. J. Arthroplast. 2016, 31, 1574–1577. [Google Scholar] [CrossRef] [PubMed]
- Vincenten, C.M.; Den, B.L.; Bos, P.K.; Bolder, S.B.; Gosens, T. Quality of life and health status after Girdlestone resection arthroplasty in patients with an infected total hip prosthesis. J. Bone Jt. Infect. 2019, 4, 10–15. [Google Scholar] [CrossRef]
- Troendlin, F.; Frieler, S.; Hanusrichter, Y.; Yilmaz, E.; Schildhauer, T.A.; Baecker, H. Persistent Fistula for Treatment of a Failed Periprosthetic Joint Infection: Relic from the Past or a Viable Salvage Procedure? J. Arthroplast. 2020, 35, 544–549. [Google Scholar] [CrossRef]
- Cierny, G.; Mader, J.T.; Penninck, J.J. A Clinical Staging System for Adult Osteomyelitis. Clin. Orthop. Relat. Res. 2003, 414, 7–24. [Google Scholar] [CrossRef]
- McPherson, E.J.; Tontz, W., Jr.; Patzakis, M.; Woodsome, C.; Holtom, P.; Norris, L.; Shufelt, C. Outcome of infected total knee utilizing a staging system for prosthetic joint infection. Am. J. Orthop. 1999, 28, 161–165. [Google Scholar]
- Ware, J.E., Jr.; Gandek, B.; Kosinski, M.; Aaronson, N.K.; Apolone, G.; Brazier, J.; Bullinger, M.; Kaasa, S.; Leplège, A.; Prieto, L.; et al. The Equivalence of SF-36 Summary Health Scores Estimated Using Standard and Country-Specific Algorithms in 10 Countries: Results from the IQOLA Project. International Quality of Life Assessment. J. Clin. Epidemiol. 1998, 51, 1167–1170. [Google Scholar] [CrossRef] [PubMed]
- Breeman, S.; Cotton, S.; Fielding, S.; Jones, G.T. Normative data for the Hospital Anxiety and Depression Scale. Qual. Life Res. 2015, 24, 391–398. [Google Scholar] [CrossRef] [PubMed]
- Walter, N.; Rupp, M.; Hierl, K.; Koch, M.; Kerschbaum, M.; Worlicek, M.; Alt, V. Long-Term Patient-Related Quality of Life after Knee Periprosthetic Joint Infection. J. Clin. Med. 2021, 10, 907. [Google Scholar] [CrossRef] [PubMed]
- Helwig, P.; Morlock, J.; Oberst, M.; Hauschild, O.; Hübner, J.; Borde, J.; Südkamp, N.P.; Konstantinidis, L. Periprosthetic joint infection—Effect on quality of life. Int. Orthop. 2014, 38, 1077–1081. [Google Scholar] [CrossRef] [PubMed]
- Hotchen, A.; Dudareva, M.; Corrigan, R.; Faggiani, M.; Ferguson, J.; McNally, M.A. Quality of life in patients with chronic osteomyelitis referred to a tertiary bone infection centre. In Proceedings of the The European Bone and Joint Infection Society (EBJIS), Ljubljana, Slovenia, 7–9 October 2021. [Google Scholar]
- Ong, K.L.; Lau, E.; Suggs, J.; Kurtz, S.M.; Manley, M.T. Risk of Subsequent Revision after Primary and Revision Total Joint Arthroplasty. Clin. Orthop. Relat. Res. 2010, 468, 3070–3076. [Google Scholar] [CrossRef]
- Kheir, M.; Tan, T.L.; Gomez, M.M.; Chen, A.F.; Parvizi, J. Patients with Failed Prior Two-Stage Exchange Have Poor Outcomes after Further Surgical Intervention. J. Arthroplast. 2017, 32, 1262–1265. [Google Scholar] [CrossRef]
- Wouthuyzen-Bakker, M.; Nijman, J.M.; Kampinga, G.A.; van Assen, S.; Jutte, P.C. Efficacy of Antibiotic Suppressive Therapy in Patients with a Prosthetic Joint Infection. J. Bone Jt. Infect. 2017, 2, 77–83. [Google Scholar] [CrossRef] [PubMed]
- Escudero-Sanchez, R.; Senneville, E.; Digumber, M.; Soriano, A.; del Toro, M.; Bahamonde, A.; del Pozo, J.; Guio, L.; Murillo, O.; Rico, A.; et al. Suppressive antibiotic therapy in prosthetic joint infections: A multicentre cohort study. Clin. Microbiol. Infect. 2020, 26, 499–505. [Google Scholar] [CrossRef] [PubMed]
- Chen, A.F.; Kinback, N.C.; Heyl, A.E.; McClain, E.J.; Klatt, B.A. Better Function for Fusions Versus Above-the-knee Amputations for Recurrent Periprosthetic Knee Infection. Clin. Orthop. Relat. Res. 2012, 470, 2737–2745. [Google Scholar] [CrossRef]
- Orfanos, A.V.; Michael, R.J.; Keeney, B.J.; Moschetti, W.E. Patient-reported outcomes after above-knee amputation for prosthetic joint infection. Knee 2020, 27, 1101–1105. [Google Scholar] [CrossRef]
- Schwartz, A.J.; Trask, D.J.; Bews, K.A.; Hanson, K.T.; Etzioni, D.A.; Habermann, E.B. Hip Disarticulation for Periprosthetic Joint Infection: Frequency, Outcome, and Risk Factors. J. Arthroplast. 2020, 35, 3269–3273.e3. [Google Scholar] [CrossRef] [PubMed]
- Kavanagh, N.; Ryan, E.J.; Widaa, A.; Sexton, G.; Fennell, J.; O’Rourke, S.; Cahill, K.C.; Kearney, C.J.; O’Brien, F.J.; Kerrigan, S.W. Staphylococcal Osteomyelitis: Disease Progression, Treatment Challenges, and Future Directions. Clin. Microbiol. Rev. 2018, 31, e00084-17. [Google Scholar] [CrossRef]
- Ferguson, J.; Alexander, M.; Bruce, S.; O’Connell, M.; Beecroft, S.; McNally, M. A retrospective cohort study comparing clinical outcomes and healthcare resource utilisation in patients undergoing surgery for osteomyelitis in England: A case for reorganising orthopaedic infection services. J. Bone Jt. Infect. 2021, 6, 151–163. [Google Scholar] [CrossRef] [PubMed]
- Chan, J.K.K.; Ferguson, J.Y.; Scarborough, M.; McNally, M.A.; Ramsden, A.J. Management of Post-Traumatic Osteomyelitis in the Lower Limb: Current State of the Art. Indian J. Plast. Surg. 2019, 52, 062–072. [Google Scholar] [CrossRef]
- Jiang, N.; Zhao, X.-Q.; Wang, L.; Lin, Q.-R.; Hu, Y.-J.; Yu, B. Single-stage debridement with implantation of antibiotic-loaded calcium sulphate in 34 cases of localized calcaneal osteomyelitis. Acta Orthop. 2020, 91, 353–359. [Google Scholar] [CrossRef] [PubMed]

| Total, N = 48 | McPherson Host Classification (n = 25) | Cierny–Mader Host Classification (n = 23) | |||
|---|---|---|---|---|---|
| Age (years), mean (range) | 63.6 (22.5–92.5) | IA1 | n = 1 | 3A | n = 1 |
| Female, n (%) | 16 (33%) | IA2 | n = 2 | 3B | n = 2 |
| Right side, n (%) | 22 (46%) | IA3 | n = 1 | 3Bl | n = 9 |
| BMI, mean (SD) | 27.4 (±4.9) | IB2 | n = 2 | 3Bls | n = 6 |
| PJI/osteomyelitis cases, n (%) | 25 (52%)/23 (48%) | IIIA1 | n = 1 | 3Bs | n = 1 |
| Cause of sinus tract (surgical/natural), n (%) | 7 (15%)/41 (85%) | IIIA2 | n = 5 | 4Bls | n= 1 |
| Localization of the sinus tract, n (%) | IIIA3 | n = 1 | |||
| Hip joint | 10 (20%) | IIIB1 | n = 1 | ||
| Knee joint | 14 (29%) | IIIB2 | n = 6 | ||
| Shoulder Joint | 2 (4%) | IIIB3 | n = 3 | ||
| Femur | 7 (15%) | IIIC2 | n = 2 | ||
| Tibia | 11 (23%) | ||||
| Foot | 1 (2%) | ||||
| Forearm | 1 (2%) | ||||
| Humerus | 2 (4%) | ||||
| Scores | Scores at Follow-Up, Mean (SD) | SF-36 Subscales | SF-36 Subscales at Follow-Up Mean (SD) |
|---|---|---|---|
| SF-36 MCS | 50.2 (±12.3) | PF | 43.3 (±32.3) |
| SF-36 PCS | 33.9 (±11.3) | RP | 29.6 (±22.8) |
| HADS-D | 6.6 (±4.4) | BP | 51.1 (±28.5) |
| HADS-A | 6.2 (±4.6) | GH | 52.9 (±20.9) |
| VAS | 3.4 (±2.6) | VT | 44.8 (±23.1) |
| Oxford Hip Score | 21.3 (±5.3) | SF | 61.7 (±20.9) |
| Oxford Knee Score | 15.6 (±7.3) | RE | 47.1 (±29.7) |
| MH | 68.2 (±25.3) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Klim, S.M.; Amerstorfer, F.; McNally, M.A.; Trebse, R.; Slokar, U.; Sigmund, I.K.; Hecker, A.; Reinbacher, P.; Leitner, L.; Bernhardt, G.A.; et al. The Sinus Tract in Bone and Joint Infection: Minimally Invasive Salvation or Prolonged Suffering? A Multicenter Study. J. Pers. Med. 2023, 13, 737. https://doi.org/10.3390/jpm13050737
Klim SM, Amerstorfer F, McNally MA, Trebse R, Slokar U, Sigmund IK, Hecker A, Reinbacher P, Leitner L, Bernhardt GA, et al. The Sinus Tract in Bone and Joint Infection: Minimally Invasive Salvation or Prolonged Suffering? A Multicenter Study. Journal of Personalized Medicine. 2023; 13(5):737. https://doi.org/10.3390/jpm13050737
Chicago/Turabian StyleKlim, Sebastian Martin, Florian Amerstorfer, Martin A. McNally, Rihard Trebse, Urban Slokar, Irene Katharina Sigmund, Andrzej Hecker, Patrick Reinbacher, Lukas Leitner, Gerwin Alexander Bernhardt, and et al. 2023. "The Sinus Tract in Bone and Joint Infection: Minimally Invasive Salvation or Prolonged Suffering? A Multicenter Study" Journal of Personalized Medicine 13, no. 5: 737. https://doi.org/10.3390/jpm13050737
APA StyleKlim, S. M., Amerstorfer, F., McNally, M. A., Trebse, R., Slokar, U., Sigmund, I. K., Hecker, A., Reinbacher, P., Leitner, L., Bernhardt, G. A., Leithner, A., Wanko, S., & Glehr, M. (2023). The Sinus Tract in Bone and Joint Infection: Minimally Invasive Salvation or Prolonged Suffering? A Multicenter Study. Journal of Personalized Medicine, 13(5), 737. https://doi.org/10.3390/jpm13050737







