Using the C-Read as a Portable Device to Evaluate Reading Ability in Young Chinese Adults: An Observational Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Screen Time and Visual QoL
2.4. C-Read Device and Smartphone-Based App
2.5. Data Collection and Statistical Analysis
3. Results
3.1. Demographics
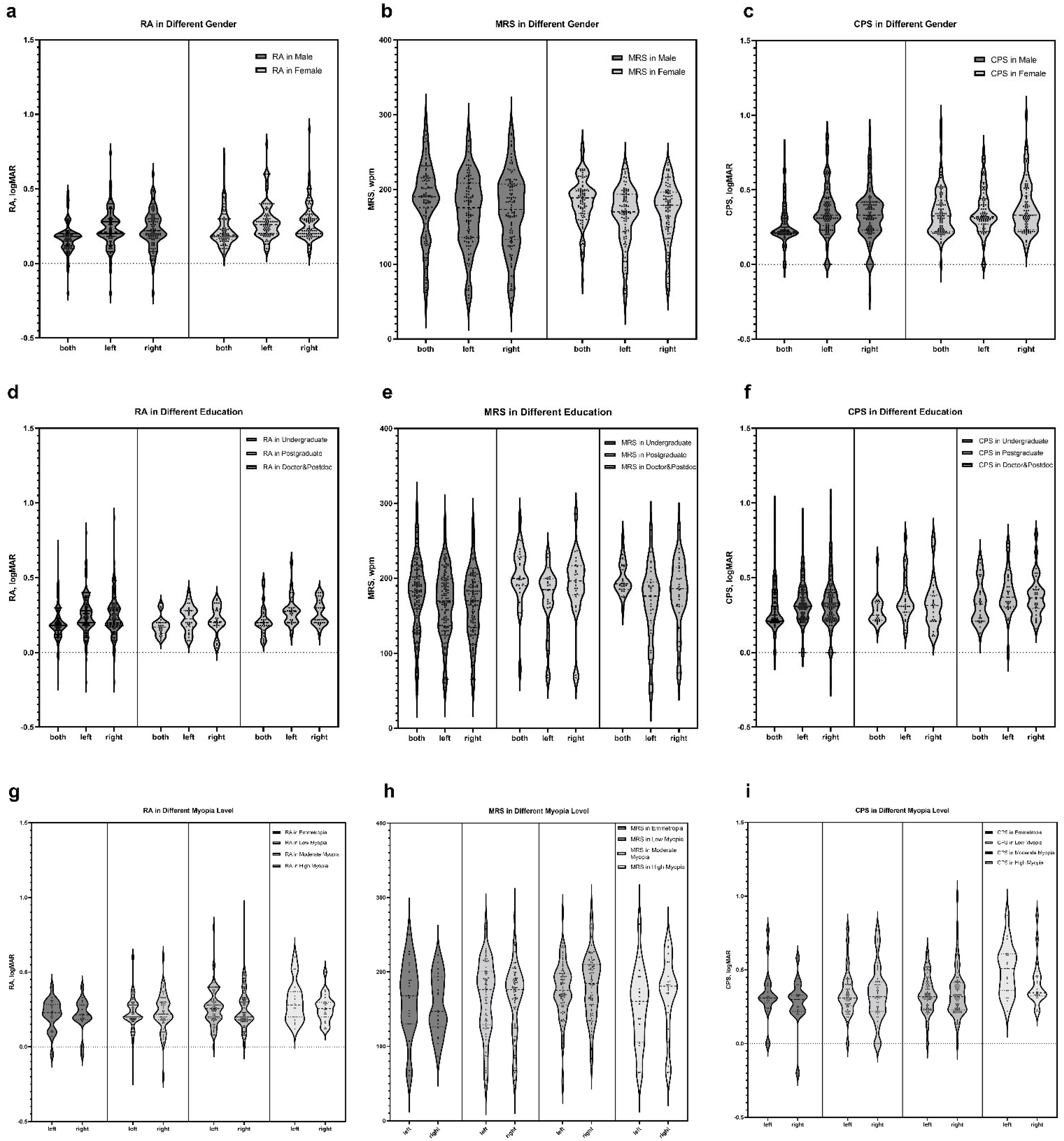
3.2. Characteristics of Reading Speed
3.3. Effect of Age, Myopia, and Screen Time on Reading Ability
3.4. Effect of Reading Ability on VFQ-25 Score Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cieza, A.; Causey, K.; Kamenov, K.; Hanson, S.W.; Chatterji, S.; Vos, T. Global estimates of the need for rehabilitation based on the Global Burden of Disease study 2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2021, 396, 2006–2017. [Google Scholar] [CrossRef] [PubMed]
- Radner, W.; Diendorfer, G.; Kainrath, B.; Kollmitzer, C. The accuracy of reading speed measurement by stopwatch versus measurement with an automated computer program (rad-rd©). Acta Ophthalmol. 2017, 95, 211–216. [Google Scholar] [CrossRef] [PubMed]
- Shah, P.; Schwartz, S.G.; Gartner, S.; Scott, I.U.; Flynn, H.W. Low vision services: A practical guide for the clinician. Ther. Adv. Ophthalmol. 2018, 10, 2515841418776264. [Google Scholar] [CrossRef] [PubMed]
- Kandel, H.; Khadka, J.; Goggin, M.; Pesudovs, K. Impact of refractive error on quality of life: A qualitative study. Clin. Exp. Ophthalmol. 2017, 45, 677–688. [Google Scholar] [CrossRef] [PubMed]
- Elliott, D.B.; Trukolo-Ilic, M.; Strong, J.G.; Pace, R.; Plotkin, A.; Bevers, P. Demographic characteristics of the vision-disabled elderly. Investig. Ophthalmol. Vis. Sci. 1997, 38, 2566–2575. [Google Scholar]
- Hawkins, B.; Miskala, P.; Bass, E.; Bressler, N.; Childs, A.; Mangione, C.; Marsh, M. Submacular Surgery Trials Research Group Surgical removal vs. observation for subfoveal choroidal neovascularization, either associated with the ocular histoplasmosis syndrome or idiopathic: II. Quality-of-life findings from a randomized clinical trial: SST Group H Trial: SST Report No. 10. Arch Ophthalmol. 2004, 122, 1616–1628. [Google Scholar] [PubMed]
- Ghazi, N.G. Bevacizumab for neovascular age-related macular degeneration (ABC trial): Multicenter randomized double-masked study. Expert Rev. Clin. Pharmacol. 2010, 3, 747–752. [Google Scholar] [CrossRef]
- Akutsu, H.; Legge, G.E.; Showalter, M.; Lindstrom, R.L.; Zabel, R.W.; Kirby, V.M. Contrast sensitivity and reading through multifocal intraocular lenses. Arch. Ophthalmol. 1992, 110, 1076–1080. [Google Scholar] [CrossRef]
- Legge, G.E.; Ross, J.A.; Luebker, A.; Lamay, J.M. Psychophysics of reading. VIII. The Minnesota low-vision reading test. Optom. Vis. Sci. 1989, 66, 843–853. [Google Scholar] [CrossRef]
- Mansfield, J.S.; Ahn, S.J.; Legge, G.E.; Luebker, A. A new reading-acuity chart for normal and low vision. In Noninvasive Assessment of the Visual System; paper NSuD. 3; Optica Publishing Group: Washington, DC, USA, 1993. [Google Scholar]
- Radner, W.; Willinger, U.; Obermayer, W.; Mudrich, C.; Velikay-Parel, M.; Eisenwort, B. A new reading chart for simultaneous determination of reading vision and reading speed. Klin. Monbl. Augenheilkd. 1998, 213, 174–181. [Google Scholar] [CrossRef]
- Radner, W. Standardization of reading charts: A review of recent developments. Optom. Vis. Sci. 2019, 96, 768–779. [Google Scholar] [CrossRef]
- Mansfield, J.S.; Legge, G.E.; Bane, M.C. Psychophysics of reading. XV: Font effects in normal and low vision. Investig. Ophthalmol. Vis. Sci. 1996, 37, 1492–1501. [Google Scholar]
- Han, Q.M.; Cong, L.J.; Yu, C.; Liu, L. Developing a Logarithmic Chinese Reading Acuity Chart. Optom. Vis. Sci. 2017, 94, 714–724. [Google Scholar] [CrossRef] [PubMed]
- Radner, W.; Obermayer, W.; Richter-Mueksch, S.; Willinger, U.; Velikay-Parel, M.; Eisenwort, B. The validity and reliability of short German sentences for measuring reading speed. Graefes. Arch. Clin. Exp. Ophthalmol. 2002, 240, 461–467. [Google Scholar] [CrossRef]
- Hahn, G.A.; Penka, D.; Gehrlich, C.; Messias, A.; Weismann, M.; Hyvärinen, L.; Leinonen, M.; Feely, M.; Rubin, G.; Dauxerre, C.; et al. New standardised texts for assessing reading performance in four European languages. Br. J. Ophthalmol. 2006, 90, 480–484. [Google Scholar] [CrossRef] [PubMed]
- Sultana, A.; Tasnim, S.; Hossain, M.M.; Bhattacharya, S.; Purohit, N. Digital screen time during the COVID-19 pandemic: A public health concern. F1000Research 2021, 10, 81. [Google Scholar] [CrossRef]
- Liu, Z. Reading behavior in the digital environment: Changes in reading behavior over the past ten years. J. Doc. 2005, 61, 700–712. [Google Scholar] [CrossRef]
- Legge, G.E. Reading digital with low vision. Visible Lang. 2016, 50, 102. [Google Scholar]
- Kingsnorth, A.; Wolffsohn, J.S. Mobile app reading speed test. Br. J. Ophthalmol. 2015, 99, 536–539. [Google Scholar] [CrossRef]
- Calabrèse, A.; To, L.; He, Y.; Berkholtz, E.; Rafian, P.; Legge, G.E. Comparing performance on the MNREAD iPad application with the MNREAD acuity chart. J. Vis. 2018, 18, 8. [Google Scholar] [CrossRef]
- Calabrese, A.; Gamam, S.; Mansfield, J.S.; Legge, G.E. Implementing the MNREAD Reading Acuity Test on an ipad3. READING 2014, 200, 300. [Google Scholar]
- Murro, V.; Sodi, A.; Giacomelli, G.; Mucciolo, D.P.; Pennino, M.; Virgili, G.; Rizzo, S. Reading Ability and Quality of Life in Stargardt Disease. Eur. J. Ophthalmol. 2017, 27, 740–745. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Hopewell, S.; Schulz, K.F.; Montori, V.; Gøtzsche, P.C.; Devereaux, P.J.; Elbourne, D.; Egger, M.; Altman, D.G. CONSORT 2010 explanation and elaboration: Updated guidelines for reporting parallel group randomised trials. BMJ 2010, 340, c869. [Google Scholar] [CrossRef]
- Mangione, C.M.; Lee, P.P.; Gutierrez, P.R.; Spritzer, K.; Berry, S.; Hays, R.D. Development of the 25-item National Eye Institute Visual Function Questionnaire. Arch. Ophthalmol. 2001, 119, 1050–1058. [Google Scholar] [PubMed]
- Broman, A.T.; Munoz, B.; West, S.K.; Rodriguez, J.; Sanchez, R.; Snyder, R.; Klein, R. Psychometric properties of the 25-item NEI-VFQ in a Hispanic population: Proyecto VER. Investig. Ophthalmol. Vis. Sci. 2001, 42, 606–613. [Google Scholar]
- Globe, D.; Varma, R.; Azen, S.P.; Paz, S.; Yu, E.; Preston-Martin, S. Psychometric performance of the NEI VFQ-25 in visually normal Latinos: The Los Angeles Latino Eye Study. Investig. Ophthalmol. Vis. Sci. 2003, 44, 1470–1478. [Google Scholar] [CrossRef]
- Suzukamo, Y.; Oshika, T.; Yuzawa, M.; Tokuda, Y.; Tomidokoro, A.; Oki, K.; Mangione, C.M.; Green, J.; Fukuhara, S. Psychometric properties of the 25-item National Eye Institute Visual Function Questionnaire (NEI VFQ-25), Japanese version. Health Qual. Life Outcomes 2005, 3, 65. [Google Scholar] [CrossRef]
- Labiris, G.; Katsanos, A.; Fanariotis, M.; Tsirouki, T.; Pefkianaki, M.; Chatzoulis, D.; Tsironi, E. Psychometric properties of the Greek version of the NEI-VFQ 25. BMC Ophthalmol. 2008, 8, 4. [Google Scholar] [CrossRef]
- Chan, C.W.; Wong, D.; Lam, C.L.; McGhee, S.; Lai, W.W. Development of a Chinese version of the National Eye Institute Visual Function Questionnaire (CHI-VFQ-25) as a tool to study patients with eye diseases in Hong Kong. Br. J. Ophthalmol. 2009, 93, 1431–1436. [Google Scholar] [CrossRef]
- Grosvenor, T. A review and a suggested classification system for myopia on the basis of age-related prevalence and age of onset. Am. J. Optom. Physiol. Opt. 1987, 64, 545–554. [Google Scholar] [CrossRef]
- Rubin, G.S. Measuring reading performance. Vis. Res. 2013, 90, 43–51. [Google Scholar] [CrossRef] [PubMed]
- Lovie-Kitchin, J.E.; Bowers, A.R.; Woods, R.L. Oral and silent reading performance with macular degeneration. Ophthalmic Physiol. Opt. 2000, 20, 360–370. [Google Scholar] [CrossRef] [PubMed]
- Runge, P.E. Eduard Jaeger’s Test-Types (Schrift-Scalen) and the historical development of vision tests. Trans. Am. Ophthalmol. Soc. 2000, 98, 375–438. [Google Scholar] [PubMed]
- Trauzettel-Klosinski, S.; Dietz, K.; Group, I.S. Standardized assessment of reading performance: The new international reading speed texts IReST. Investig. Ophthalmol. Vis. Sci. 2012, 53, 5452–5461. [Google Scholar] [CrossRef]
- Cheung, J.P.; Liu, D.S.; Lam, C.C.; Cheong, A.M. Development and validation of a new Chinese reading chart for children. Ophthalmic Physiol. Opt. 2015, 35, 514–521. [Google Scholar] [CrossRef]
- Zhang, J.Y.; Zhang, T.; Xue, F.; Liu, L.; Yu, C. Legibility variations of Chinese characters and implications for visual acuity measurement in Chinese reading population. Investig. Ophthalmol. Vis. Sci. 2007, 48, 2383–2390. [Google Scholar] [CrossRef]
- West, S.K.; Rubin, G.S.; Munoz, B.; Abraham, D.; Fried, L.P.; The Salisbury Eye Evaluation Project T. Assessing Functional Status: Correlation Between Performance on Tasks Conducted in a Clinic Setting and Performance on the Same Task Conducted at Home. J. Gerontol. Ser. A 1997, 52A, M209–M217. [Google Scholar] [CrossRef]
- Fried, L.P.; Herdman, S.J.; Kuhn, K.E.; Rubin, G.; Turano, K. Preclinical disability: Hypotheses about the bottom of the iceberg. J. Aging Health 1991, 3, 285–300. [Google Scholar] [CrossRef]
- Pan, C.W.; Ramamurthy, D.; Saw, S.M. Worldwide prevalence and risk factors for myopia. Ophthalmic Physiol. Opt. 2012, 32, 3–16. [Google Scholar] [CrossRef]
- Huang, L.; Kawasaki, H.; Liu, Y.; Wang, Z. The prevalence of myopia and the factors associated with it among university students in Nanjing: A cross-sectional study. Medicine 2019, 98, e14777. [Google Scholar] [CrossRef]
- Hu, Y.; Zhao, F.; Ding, X.; Zhang, S.; Li, Z.; Guo, Y.; Feng, Z.; Tang, X.; Li, Q.; Guo, L.; et al. Rates of Myopia Development in Young Chinese Schoolchildren During the Outbreak of COVID-19. JAMA Ophthalmol. 2021, 139, 1115–1121. [Google Scholar] [CrossRef] [PubMed]
- Balhara, Y.P.S.; Bhargava, R. Screen time and COVID-19: Observations from among the college students in India. J. Behav. Addict. 2022, 11, 182. [Google Scholar]
- Seresirikachorn, K.; Thiamthat, W.; Sriyuttagrai, W.; Soonthornworasiri, N.; Singhanetr, P.; Yudtanahiran, N.; Theeramunkong, T. Effects of digital devices and online learning on computer vision syndrome in students during the COVID-19 era: An online questionnaire study. BMJ Paediatr. Open 2022, 6, e001429. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.F.; Liao, M.Q.; Cai, W.L.; Yu, X.X.; Li, S.N.; Ke, X.Y.; Tan, S.X.; Luo, Z.Y.; Cui, Y.F.; Wang, Q.; et al. Physical activity, screen exposure and sleep among students during the pandemic of COVID-19. Sci. Rep. 2021, 11, 8529. [Google Scholar] [CrossRef] [PubMed]
- Lissak, G. Adverse physiological and psychological effects of screen time on children and adolescents: Literature review and case study. Environ. Res. 2018, 164, 149–157. [Google Scholar] [CrossRef]
- Wong, C.W.; Tsai, A.; Jonas, J.B.; Ohno-Matsui, K.; Chen, J.; Ang, M.; Ting, D.S.W. Digital Screen Time During the COVID-19 Pandemic: Risk for a Further Myopia Boom? Am. J. Ophthalmol. 2021, 223, 333–337. [Google Scholar] [CrossRef] [PubMed]
- Mu, J.; Zhong, H.; Liu, M.; Jiang, M.; Shuai, X.; Chen, Y.; Long, W.; Zhang, S. Trends in Myopia Development Among Primary and Secondary School Students During the COVID-19 Pandemic: A Large-Scale Cross-Sectional Study. Front. Public Health 2022, 10, 859285. [Google Scholar] [CrossRef]
- Liu, J.; Chen, Q.; Dang, J. Examining risk factors related to digital learning and social isolation: Youth visual acuity in COVID-19 pandemic. J. Glob. Health. 2021, 11, 05020. [Google Scholar] [CrossRef]
- Calabrèse, A.; Cheong, A.M.; Cheung, S.H.; He, Y.; Kwon, M.; Mansfield, J.S.; Subramanian, A.; Yu, D.; Legge, G.E. Baseline MNREAD Measures for Normally Sighted Subjects From Childhood to Old Age. Investig. Ophthalmol. Vis. Sci. 2016, 57, 3836–3843. [Google Scholar] [CrossRef]
- Chan, C.W.; Wong, J.C.; Chan, K.S.; Wong, W.K.; Tam, K.C.; Chau, P.S. Evaluation of quality of life in patients with cataract in Hong Kong. J. Cataract. Refract. Surg. 2003, 29, 1753–1760. [Google Scholar]
- Zhu, M.; Yu, J.; Zhang, J.; Yan, Q.; Liu, Y. Evaluating vision-related quality of life in preoperative age-related cataract patients and analyzing its influencing factors in China: A cross-sectional study. BMC Ophthalmol. 2015, 15, 160. [Google Scholar] [CrossRef] [PubMed]
- Hernandez Trillo, A.; Dickinson, C.M. The impact of visual and nonvisual factors on quality of life and adaptation in adults with visual impairment. Investig. Ophthalmol. Vis. Sci. 2012, 53, 4234–4241. [Google Scholar] [CrossRef] [PubMed]



| Characteristic | No. (%) |
|---|---|
| Healthy Group (n = 207) | |
| Age, mean (SD), y | 22.46 (4.01) |
| Gender | |
| Male | 116 (56.04) |
| Female | 91 (43.96) |
| Education | |
| Undergraduate | 146 (71.22) |
| Postgraduate | 26 (12.68) |
| Doctor and Postdoc | 33 (16.10) |
| Myopia, eyes | |
| No | 40 (9.66) |
| Low | 144 (34.78) |
| Moderate | 187 (45.17) |
| High | 43 (10.39) |
| Screen time, mean (SD), h | |
| Phone | 4.55 (1.37) |
| Personal computer | 4.32 (1.65) |
| Pad | 2.55 (1.71) |
| Total | 5.06 (1.50) |
| VFQ-25, mean (SD) | 86.26 (9.11) |
| Characteristic | Mean (SD) |
|---|---|
| Healthy Group (n = 191) | |
| RA, logMAR | |
| both eyes | 0.193 (0.104) |
| right eye | 0.242 (0.124) |
| left eye | 0.249 (0.120) |
| MRS, wpm | |
| both eyes | 185.16 (44.93) |
| right eye | 171.65 (46.27) |
| left eye | 168.59 (45.68) |
| CPS, logMAR | |
| both eyes | 0.419 (1.05) |
| right eye | 0.412 (0.647) |
| left eye | 0.371 (0.229) |
| RA | MRS | CPS | ||
|---|---|---|---|---|
| Gender | Male (n = 105) | 0.17 (0.10) | 184.95 (52.74) | 0.27 (0.13) |
| Female (n = 86) | 0.22 (0.11) | 185.42 (33.29) | 0.34 (0.15) | |
| p value | 0.005 | 0.685 | 0.025 | |
| Education | Undergraduate (n = 133) | 0.19 (0.11) | 178.57 (48.40) | 0.30 (0.15) |
| Postgraduate (n = 26) | 0.17 (0.06) | 203.76 (39.07) | 0.27 (0.09) | |
| Doctor and Postdoc (n = 30) | 0.21 (0.10) | 199.64 (21.80) | 0.33 (0.14) | |
| p value | 0.217 | 0.002 | 0.093 | |
| Myopia | No (n = 37) | 0.16 (0.08) | 162.4 (42.9) | 0.29 (0.10) |
| Low (n = 136) | 0.19 (0.11) | 163.2 (46.1) | 0.34 (0.15) | |
| Moderate (n = 166) | 0.19 (0.11) | 178.6 (43.4) | 0.34 (0.14) | |
| High (n = 43) | 0.22 (0.08) | 162.9 (44.7) | 0.44 (0.18) | |
| p value | 0.772 | 0.049 | < 0.001 |
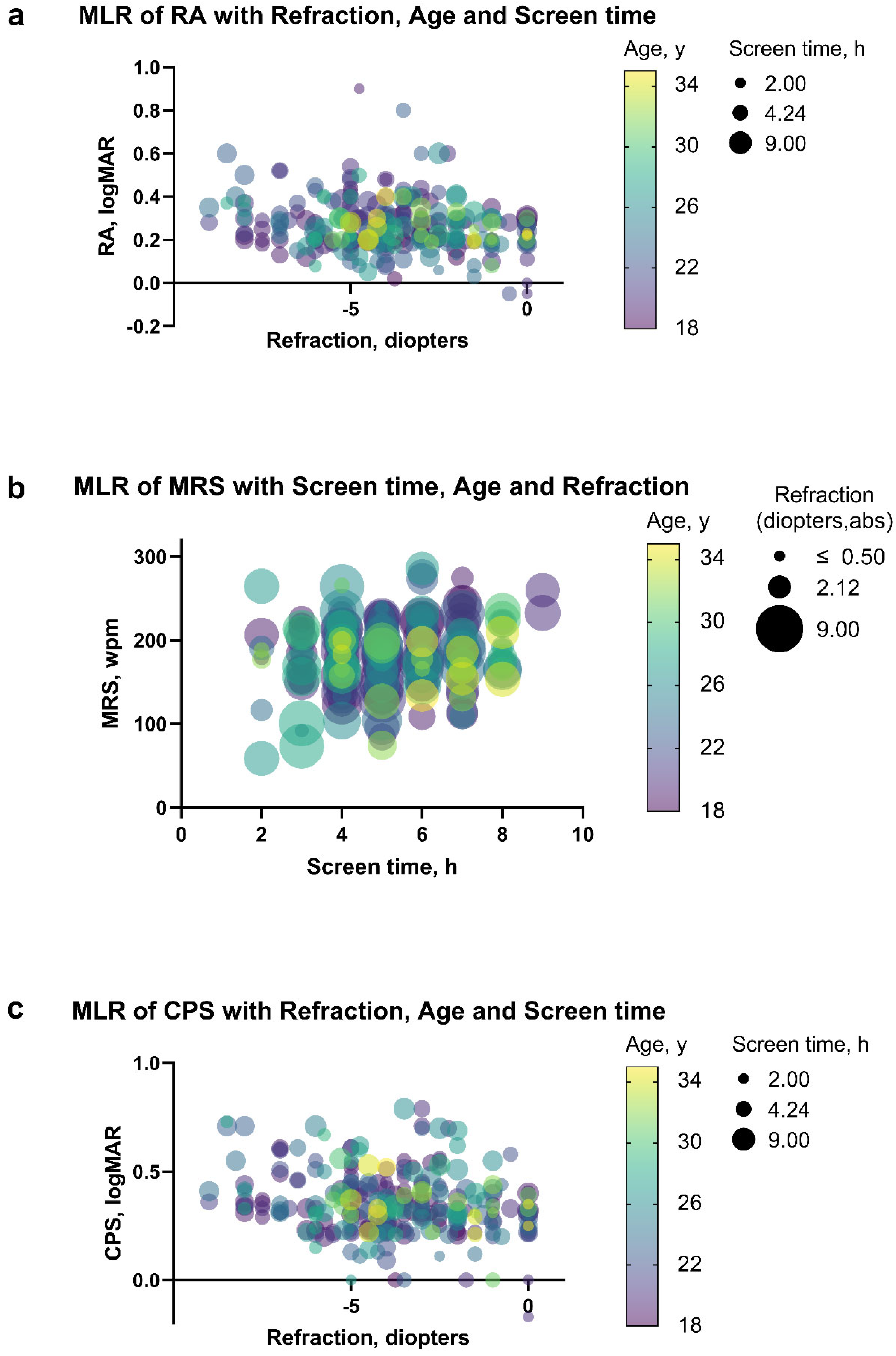
| Measure | Multivariate Linear Regression | Stepwise Regression (p value = 0.05) | |||
|---|---|---|---|---|---|
| β (95% CI) | p Value | β (95% CI) | p Value | ||
| RA | Intercept | 0.213 (0.128 to 0.297) | <0.001 | 0.22 (0.19 to 0.24) | <0.001 |
| Age, y | −0.00074 (−0.00387 to 0.00239) | 0.642 | |||
| Screen time, h | 0.0044 (−0.0045 to 0.0133) | 0.331 | |||
| Myopia, D | −0.012 (−0.018 to −0.006) | <0.001 | −0.012 (−0.018 to −0.006) | <0.001 | |
| MRS | Intercept | 179.77 (152.39 to 207.15) | <0.001 | 166.0 (150.9 to 181.1) | <0.001 |
| Age, y | −0.55 (−1.56 to 0.47) | 0.289 | |||
| Screen time, h | 3.45 (0.57 to 6.33) | 0.019 | 3.19 (0.34 to 6.04) | 0.028 | |
| Myopia, D | 0.68 (−1.33 to 2.69) | 0.507 | |||
| CPS | Intercept | 0.19 (0.09 to 0.30) | <0.001 | 0.23 (0.16 to 0.29) | <0.001 |
| Age, y | −0.0014 (−0.024 to 0.005) | 0.467 | |||
| Screen time, h | 0.015 (0.004 to 0.026) | 0.010 | 0.015 (0.004 to 0.026) | 0.007 | |
| Myopia, D | −0.013 (−0.021 to −0.006) | <0.001 | −0.013 (−0.021 to −0.006) | <0.001 | |
| Measure | Multivariate Linear Regression | Stepwise Regression (p Value = 0.05) | |||
|---|---|---|---|---|---|
| β (95% CI) | p Value | β (95% CI) | p Value | ||
| Right eye | Intercept | 109.76 (99.15 to 120.38) | <0.001 | 100.82 (94.78 to 106.86) | <0.001 |
| Age, y | −0.17 (−0.50 to 0.15) | 0.298 | |||
| Total screen time, h | −0.86 (−1.30 to −0.42) | <0.001 | −0.86 (−1.29 to −0.42) | <0.001 | |
| Refraction, D | 0.42 (−0.17 to 1.01) | 0.164 | |||
| RA, logMAR | −16.60 (−32.19 to −1.00) | 0.037 | −18.65 (−30.88 to −6.43) | 0.003 | |
| MRS, wpm | −0.017 (−0.046 to 0.012) | 0.240 | |||
| CPS, logMAR | −2.75 (−14.36 to 8.86) | 0.640 | |||
| Left eye | Intercept | 105.58 (95.57 to 115.60) | <0.001 | 100.68 (95.15 to 106.21) | <0.001 |
| Age, y | −0.08 (−0.37 to 0.21) | 0.598 | |||
| Total screen time, h | −0.64 (−1.05 to −0.23) | 0.002 | −0.63 (−1.04 to −0.23) | 0.002 | |
| Refraction, D | 0.11 (−0.43 to 0.65) | 0.683 | |||
| RA, logMAR | −21.31 (−35.69 to −6.92) | 0.004 | −26.83 (−37.84 to −15.83) | <0.001 | |
| MRS, wpm | −0.01 (−0.04 to 0.02) | 0.429 | |||
| CPS, logMAR | −6.28 (−17.37 to 4.82) | 0.266 | |||
| Both eyes * | Intercept | 107.25 (96.62 to 117.89) | <0.001 | 100.24 (94.59 to 105.89) | <0.001 |
| Age, y | −0.12 (−0.44 to 0.20) | 0.451 | |||
| Total screen time, h | −0.88 (−1.32 to −0.44) | <0.001 | −0.86 (−1.29 to −0.43) | <0.001 | |
| RA, logMAR | −15.61 (−30.70 to −0.52) | 0.043 | −21.41 (−33.74 to −9.08) | 0.001 | |
| MRS, wpm | −0.015 (−0.045 to 0.015) | 0.330 | |||
| CPS, logMAR | −7.59 (−18.30 to 3.12) | 0.164 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cheng, T.; Yao, T.; Xu, B.; Dai, W.; Qin, X.; Ye, J.; Suo, L.; Zhang, C. Using the C-Read as a Portable Device to Evaluate Reading Ability in Young Chinese Adults: An Observational Study. J. Pers. Med. 2023, 13, 463. https://doi.org/10.3390/jpm13030463
Cheng T, Yao T, Xu B, Dai W, Qin X, Ye J, Suo L, Zhang C. Using the C-Read as a Portable Device to Evaluate Reading Ability in Young Chinese Adults: An Observational Study. Journal of Personalized Medicine. 2023; 13(3):463. https://doi.org/10.3390/jpm13030463
Chicago/Turabian StyleCheng, Tian, Taikang Yao, Boxuan Xu, Wanwei Dai, Xuejiao Qin, Juan Ye, Lingge Suo, and Chun Zhang. 2023. "Using the C-Read as a Portable Device to Evaluate Reading Ability in Young Chinese Adults: An Observational Study" Journal of Personalized Medicine 13, no. 3: 463. https://doi.org/10.3390/jpm13030463
APA StyleCheng, T., Yao, T., Xu, B., Dai, W., Qin, X., Ye, J., Suo, L., & Zhang, C. (2023). Using the C-Read as a Portable Device to Evaluate Reading Ability in Young Chinese Adults: An Observational Study. Journal of Personalized Medicine, 13(3), 463. https://doi.org/10.3390/jpm13030463








