Patient Satisfaction and Impact on Oral Health after Maxillary Rehabilitation Using a Personalized Additively Manufactured Subperiosteal Jaw Implant (AMSJI)
Abstract
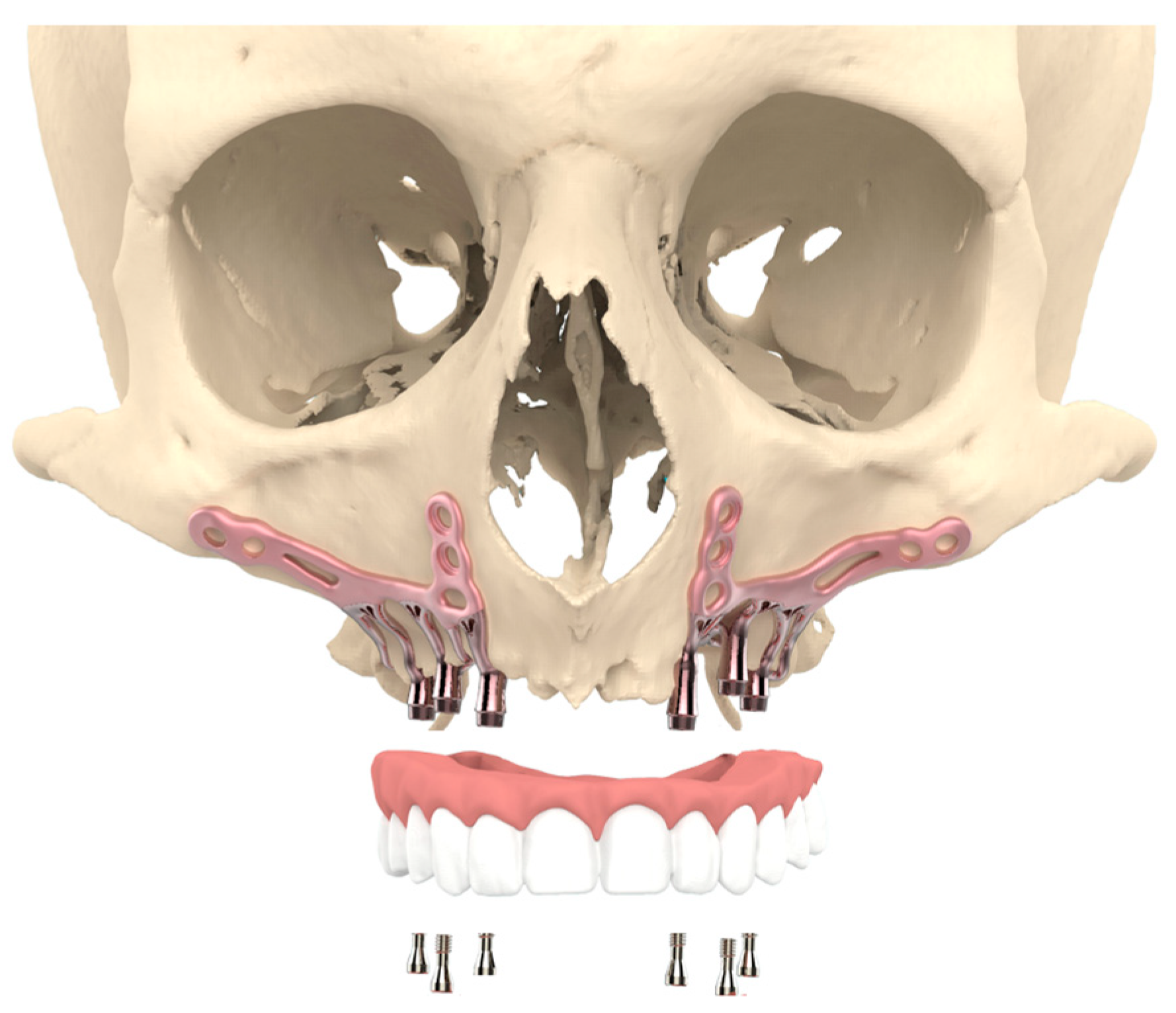
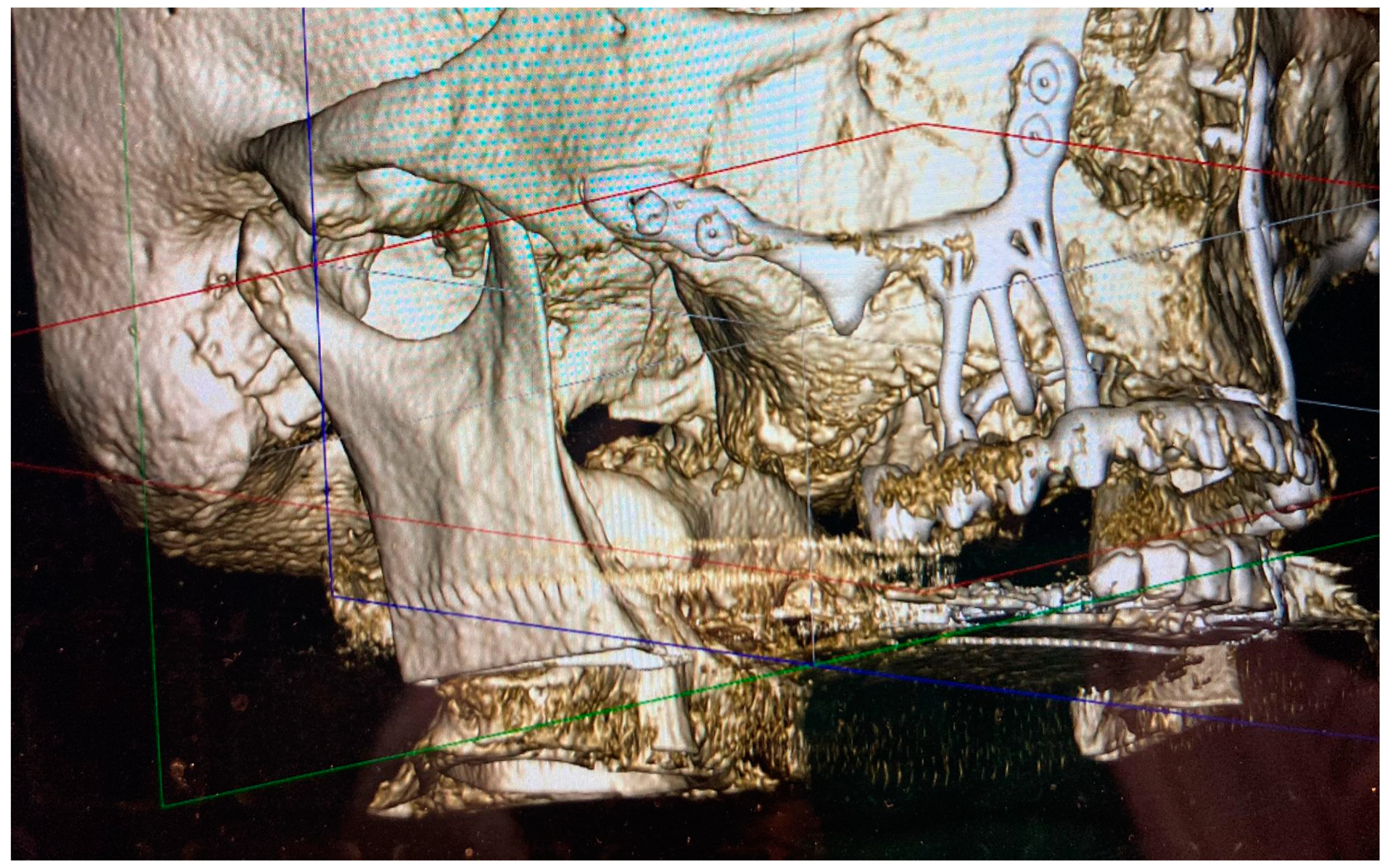
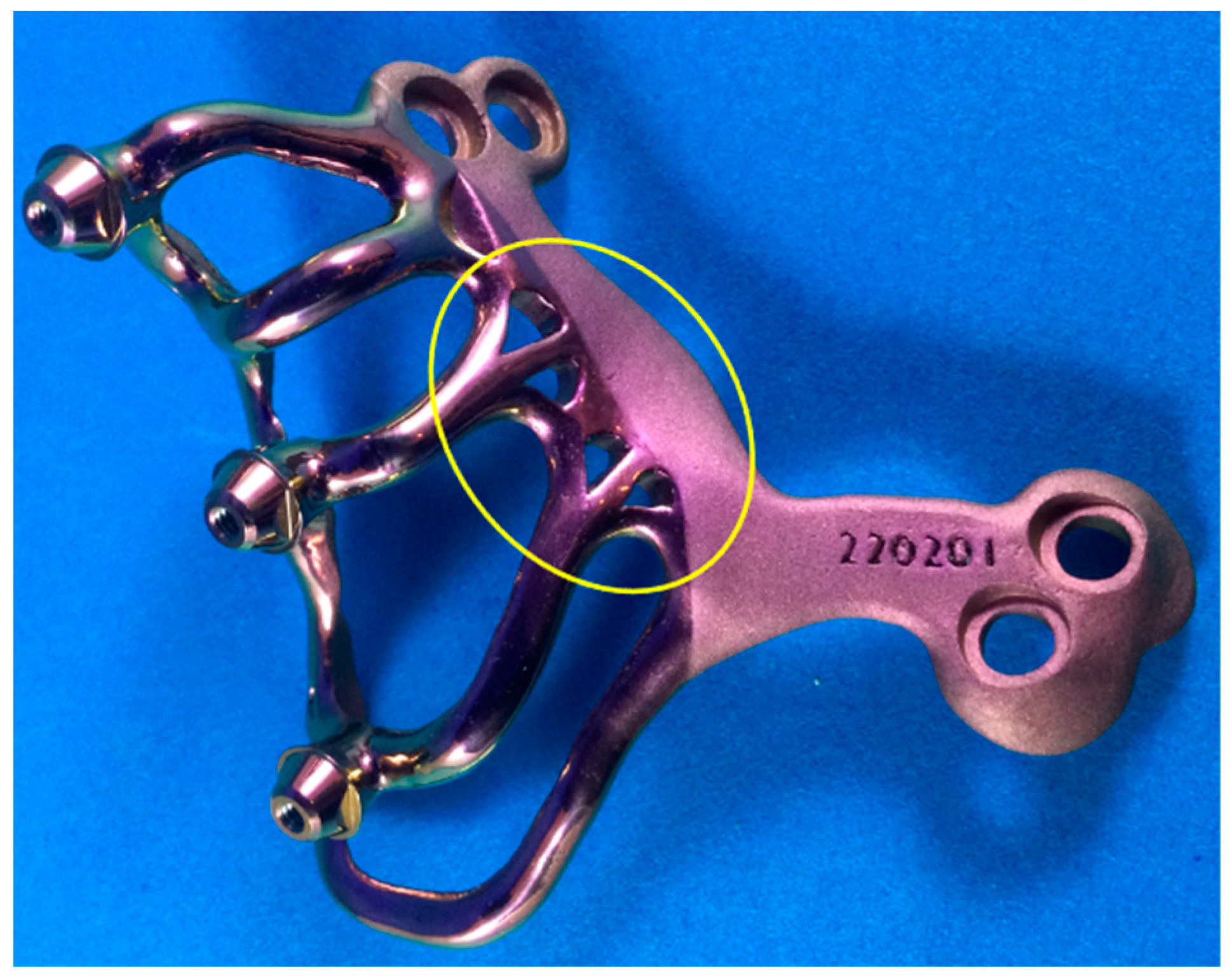
1. Introduction
2. Materials and Methods
- A.
- The Oral Health Impact Profile-14 (OHIP-14)
- B.
- Numerical Rating Scale (NRS)
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dahl, S.G.A. Om möjligheten för implantation i käken av metallskelett som bas eller retention för fasta eller avtagbara protester Särtryck ur Odontologisk Tidskrift häfte. Odontol. Tidskr. 1943, 52, 440–446. [Google Scholar]
- Obwegeser, H.L. Experiences with subperiosteal implants. Oral Surg. Oral Med. Oral Pathol. 1959, 12, 777–786. [Google Scholar] [CrossRef]
- Mommaerts, M.Y. Additively manufactured sub-periosteal jaw implants. Int. J. Oral Maxillofac. Surg. 2017, 46, 938–940. [Google Scholar] [CrossRef]
- Mommaerts, M.Y. Evolutionary steps in the design and biofunctionalization of the additively manufactured sub-periosteal jaw implant ‘AMSJI’ for the maxilla. Int. J. Oral Maxillofac. Surg. 2019, 48, 108–114. [Google Scholar] [CrossRef]
- Korn, P.; Gellrich, N.C.; Spalthoff, S.; Jehn, P.; Eckstein, F.; Lentge, F.; Zeller, A.N.; Rahlf, B. Managing the severely atrophic maxilla: Farewell to zygomatic implants and extensive augmentations? J. Stomatol. Oral Maxillofac. Surg. 2022, 123, 562–565. [Google Scholar] [CrossRef]
- Gellrich, N.C.; Zimmerer, R.M.; Spalthoff, S.; Jehn, P.; Pott, P.C.; Rana, M.; Rahlf, B. A customised digitally engineered solution for fixed dental rehabilitation in severe bone deficiency: A new innovative line extension in implant dentistry. J. Cranio-Maxillofac. Surg. 2017, 45, 1632–1638. [Google Scholar] [CrossRef]
- Dimitroulis, G.; Gupta, B.; Wilson, I.; Hart, C. The atrophic edentulous alveolus. A preliminary study on a new generation of subperiosteal implants. Oral Maxillofac. Surg. 2022, 1–10. [Google Scholar] [CrossRef]
- Bodine, R.L.; Yanase, R.T.; Bodine, A. Forty years of experience with subperiosteal implant dentures in 41 edentulous patients. J. Prosthet. Dent. 1996, 75, 33–44. [Google Scholar] [CrossRef]
- Yanase, R.T.; Bodine, R.L.; Tom, J.F.; White, S.N. The mandibular subperiosteal implant denture: A prospective survival study. J. Prosthet. Dent. 1994, 71, 369–374. [Google Scholar] [CrossRef]
- Van den Borre, C.; Rinaldi, M.; De Neef, B.; Loomans, N.A.J.; Nout, E.; Van Doorne, L.; Naert, I.; Politis, C.; Schouten, H.; Klomp, G.; et al. Patient- and clinician-reported outcomes for the additively manufactured sub-periosteal jaw implant (AMSJI) in the maxilla: A prospective multicentre one-year follow-up study. Int. J. Oral Maxillofac. Surg. 2022, 51, 243–250. [Google Scholar] [CrossRef]
- Cunha-Cruz, J.; Hujoel, P.P.; Nadanovsky, P. Secular trends in socio-economic disparities in edentulism: USA, 1972–2001. J. Dent. Res. 2007, 86, 131–136. [Google Scholar] [CrossRef] [PubMed]
- Douglass, C.W.; Shih, A.; Ostry, L. Will there be a need for complete dentures in the United States in 2020? J. Prosthet. Dent. 2002, 87, 5–8. [Google Scholar] [CrossRef] [PubMed]
- Laurito, D.; Lamazza, L.; Spink, M.J.; De Biase, A. Tissue-supported dental implant prosthesis (overdenture): The search for the ideal protocol. A literature review. Ann. Stomatol. 2012, 3, 2–10. [Google Scholar]
- Mapkar, M.; Syed, R. Revisiting the maxillary subperiosteal implant prosthesis: A case study. J. Dent. Implant. 2015, 5, 113–119. [Google Scholar]
- Emami, E.; de Souza, R.F.; Kabawat, M.; Feine, J.S. The impact of edentulism on oral and general health. Int. J. Dent. 2013, 2013, 498305. [Google Scholar] [CrossRef]
- Gjerde, C.G.; Shanbhag, S.; Neppelberg, E. Patient experience following iliac crest-derived alveolar bone grafting and implant placement. Int. J. Implant Dent. 2020, 6, 4. [Google Scholar] [CrossRef] [PubMed]
- Wortmann, D.E.; van Minnen, B.; Delli, K.; Schortinghuis, J.; Raghoebar, G.M.; Vissink, A. Harvesting anterior iliac crest or calvarial bone grafts to augment severely resorbed edentulous jaws: A systematic review and meta-analysis of patient-reported outcomes. Int. J. Oral Maxillofac. Surg. 2022, 12. Epub ahead of print. [Google Scholar] [CrossRef]
- Solà Pérez, A.; Pastorino, D.; Aparicio, C.; Pegueroles Neyra, M.; Khan, R.S.; Wright, S.; Ucer, C. Success Rates of Zygomatic Implants for the Rehabilitation of Severely Atrophic Maxilla: A Systematic Review. Dent. J. 2022, 12, 151. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Ruiz, J.A.; Sánchez-Siles, M.; Guerrero-Sánchez, Y.; Pato-Mourelo, J.; Camacho-Alonso, F. Evaluation of Quality of Life and Satisfaction in Patients with Fixed Prostheses on Zygomatic Implants Compared with the All-on-Four Concept: A Prospective Randomized Clinical Study. Int. J. Environ. Res. Public Health 2021, 25, 3426. [Google Scholar] [CrossRef]
- Ramezanzade, S.; Yates, J.; Tuminelli, F.J. Zygomatic implants placed in atrophic maxilla: An overview of current systematic reviews and meta-analysis. Maxillofac. Plast. Reconstr. Surg. 2021, 43, 1. [Google Scholar] [CrossRef]
- Sartori, E.M.; Padovan, L.E.; de Mattias Sartori, I.A.; Ribeiro, P.D., Jr.; Gomes de Souza Carvalho, A.C.; Goiato, M.C. Evaluation of satisfaction of patients rehabilitated with zygomatic fixtures. J. Oral Maxillofac. Surg. 2012, 70, 314–319. [Google Scholar] [CrossRef] [PubMed]
- Abd El Salam, S.E.; El Khashab, M.A. Zygomatic implants may improve quality of life and satisfaction in patients with atrophied maxilla. J. Evid. Based Dent. Pract. 2022, 22, 101729. [Google Scholar] [CrossRef] [PubMed]
- Dahl, K.E.; Wang, N.J.; Skau, I.; Ohrn, K. Oral health-related quality of life and associated factors in Norwegian adults. Acta Odontol. Scand. 2011, 69, 208–214. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Bäumer, D.; Ozga, A.K.; Körner, G.; Bäumer, A. Patient satisfaction and oral health-related quality of life 10 years after implant placement. BMC Oral Health 2021, 21, 30. [Google Scholar] [CrossRef]
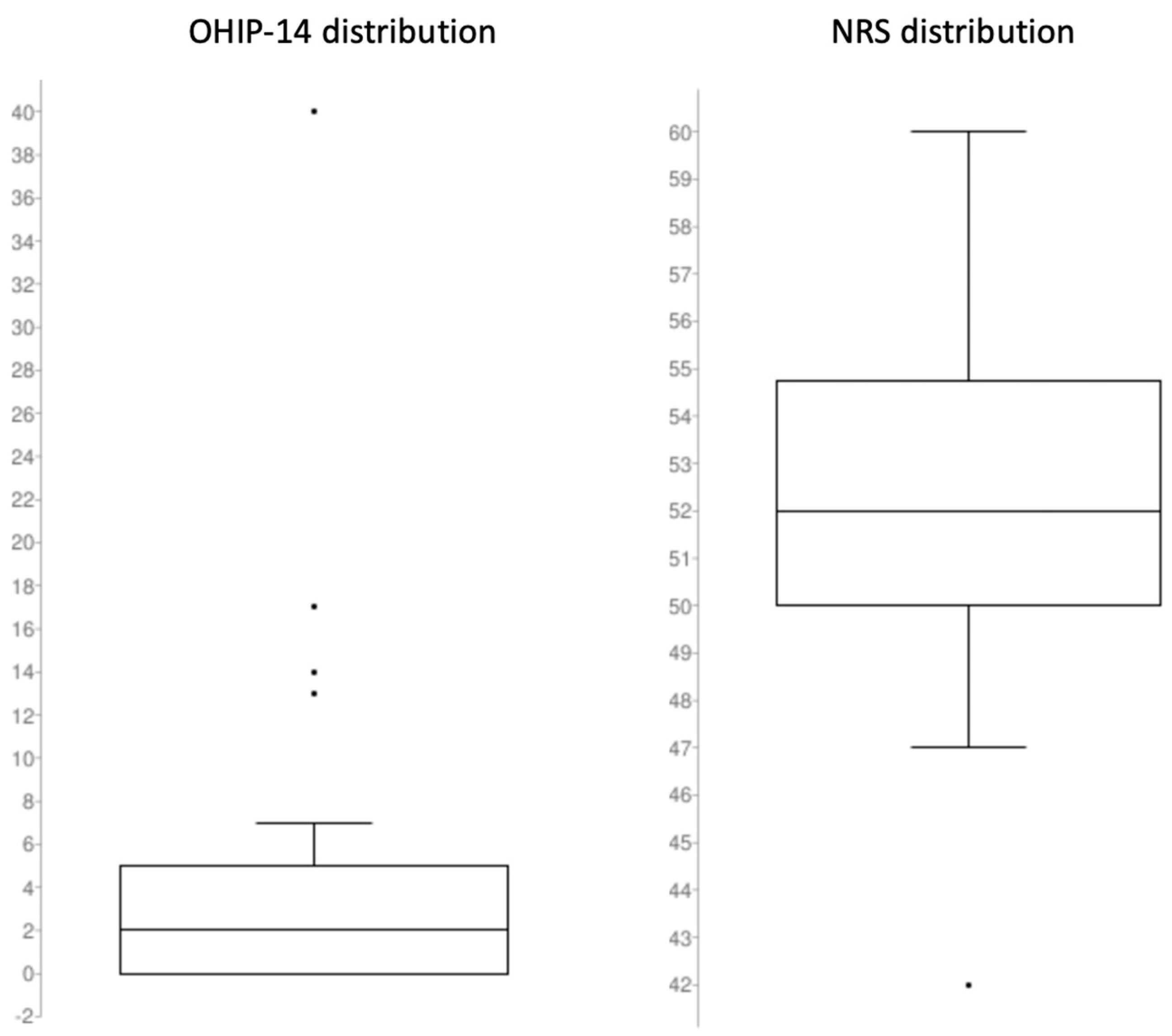
| Domain | Mean | SD |
|---|---|---|
| Overall OHIP-14 | 4.20 | 7.09 |
| 1.08 | 1.51 |
| 1.00 | 1.75 |
| 0.75 | 1.45 |
| 0.53 | 1.20 |
| 0.38 | 1.13 |
| 0.25 | 0.84 |
| 0.23 | 0.73 |
| Question | Mean | SD |
|---|---|---|
| Overall NRS | 52.25 | 4.00 |
| 9.03 | 0.92 |
| 8.83 | 1.11 |
| 8.63 | 1.29 |
| 8.48 | 1.38 |
| 8.73 | 1.28 |
| 8.58 | 1.11 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Van den Borre, C.; De Neef, B.; Loomans, N.A.J.; Rinaldi, M.; Nout, E.; Bouvry, P.; Naert, I.; Mommaerts, M.Y. Patient Satisfaction and Impact on Oral Health after Maxillary Rehabilitation Using a Personalized Additively Manufactured Subperiosteal Jaw Implant (AMSJI). J. Pers. Med. 2023, 13, 297. https://doi.org/10.3390/jpm13020297
Van den Borre C, De Neef B, Loomans NAJ, Rinaldi M, Nout E, Bouvry P, Naert I, Mommaerts MY. Patient Satisfaction and Impact on Oral Health after Maxillary Rehabilitation Using a Personalized Additively Manufactured Subperiosteal Jaw Implant (AMSJI). Journal of Personalized Medicine. 2023; 13(2):297. https://doi.org/10.3390/jpm13020297
Chicago/Turabian StyleVan den Borre, Casper, Björn De Neef, Natalie A. J. Loomans, Marco Rinaldi, Erik Nout, Peter Bouvry, Ignace Naert, and Maurice Y. Mommaerts. 2023. "Patient Satisfaction and Impact on Oral Health after Maxillary Rehabilitation Using a Personalized Additively Manufactured Subperiosteal Jaw Implant (AMSJI)" Journal of Personalized Medicine 13, no. 2: 297. https://doi.org/10.3390/jpm13020297
APA StyleVan den Borre, C., De Neef, B., Loomans, N. A. J., Rinaldi, M., Nout, E., Bouvry, P., Naert, I., & Mommaerts, M. Y. (2023). Patient Satisfaction and Impact on Oral Health after Maxillary Rehabilitation Using a Personalized Additively Manufactured Subperiosteal Jaw Implant (AMSJI). Journal of Personalized Medicine, 13(2), 297. https://doi.org/10.3390/jpm13020297







