The Relationship between Preoperative Urine Culture and Post-Percutaneous Nephrostolithotomy Systemic Inflammatory Response Syndrome: A Single-Center Retrospective Study
Abstract
1. Introduction
2. Materials and Methods
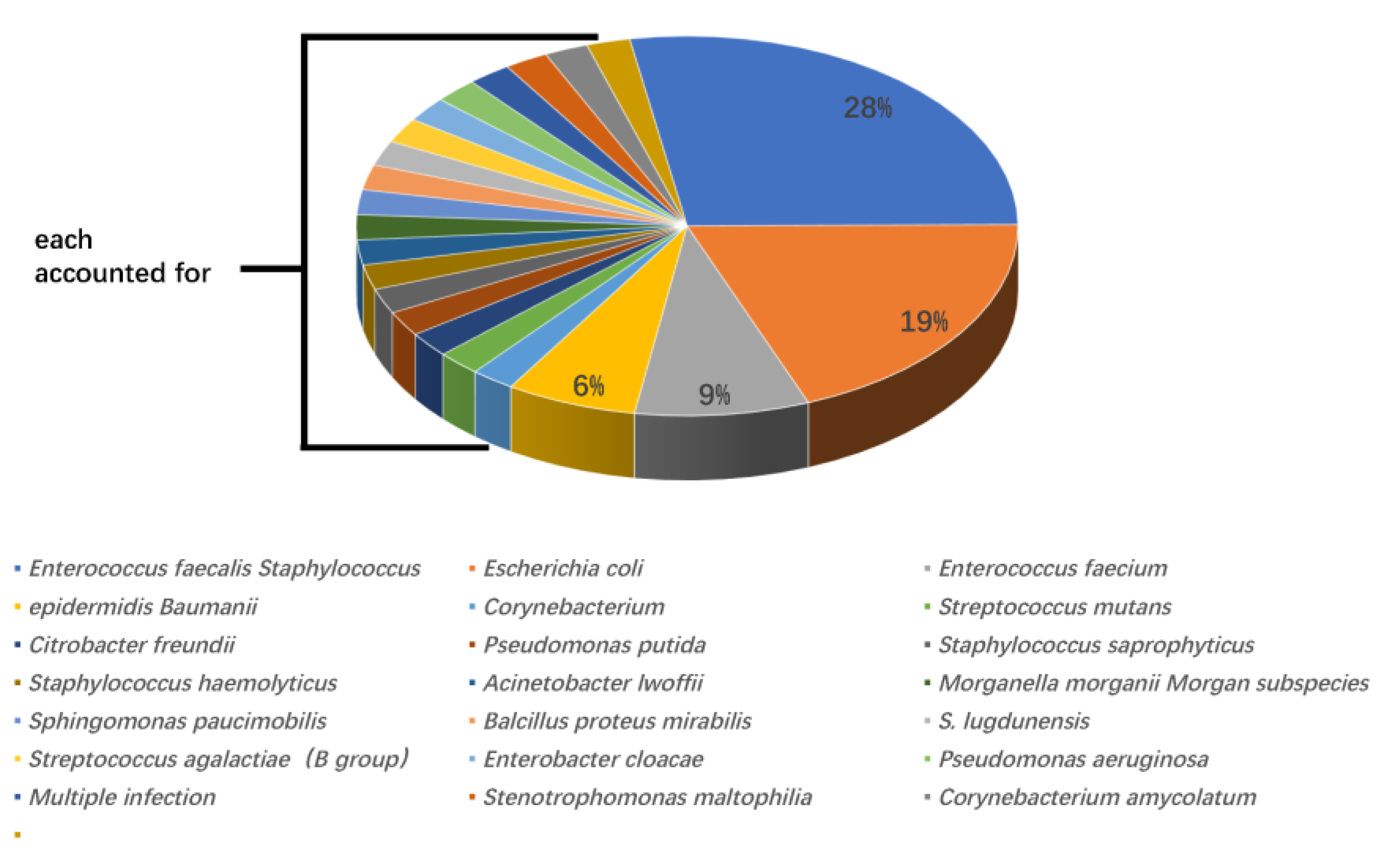
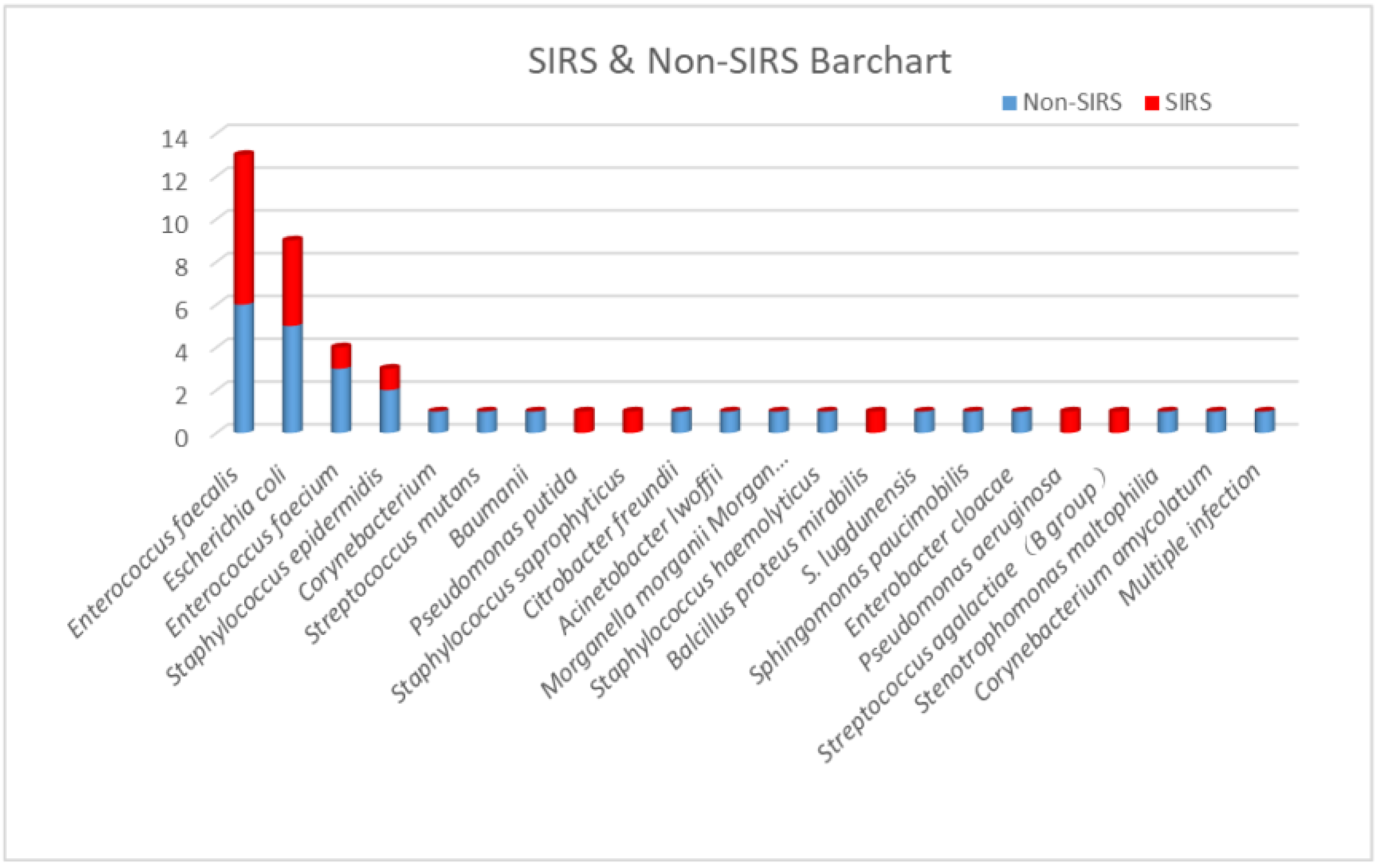
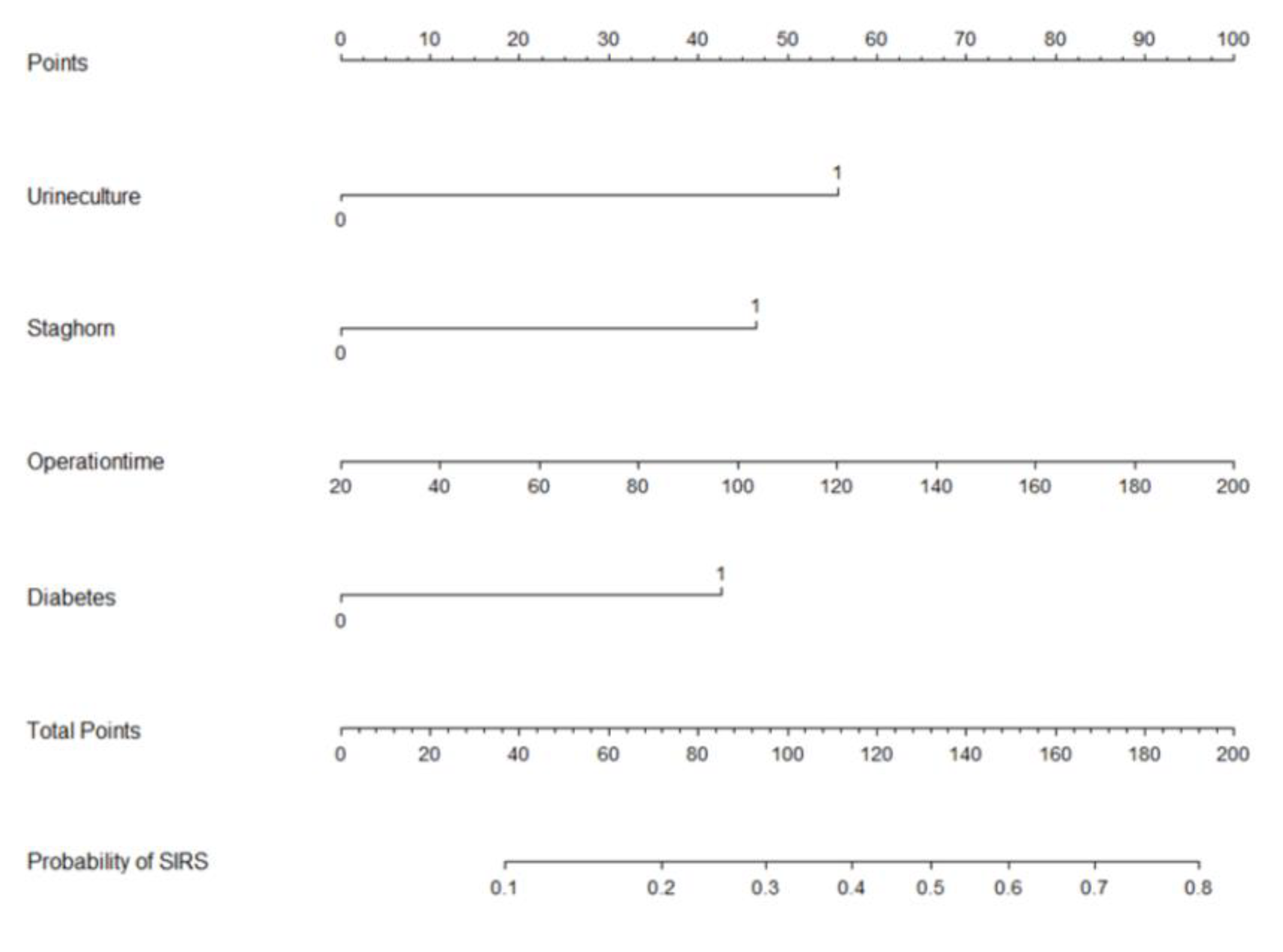
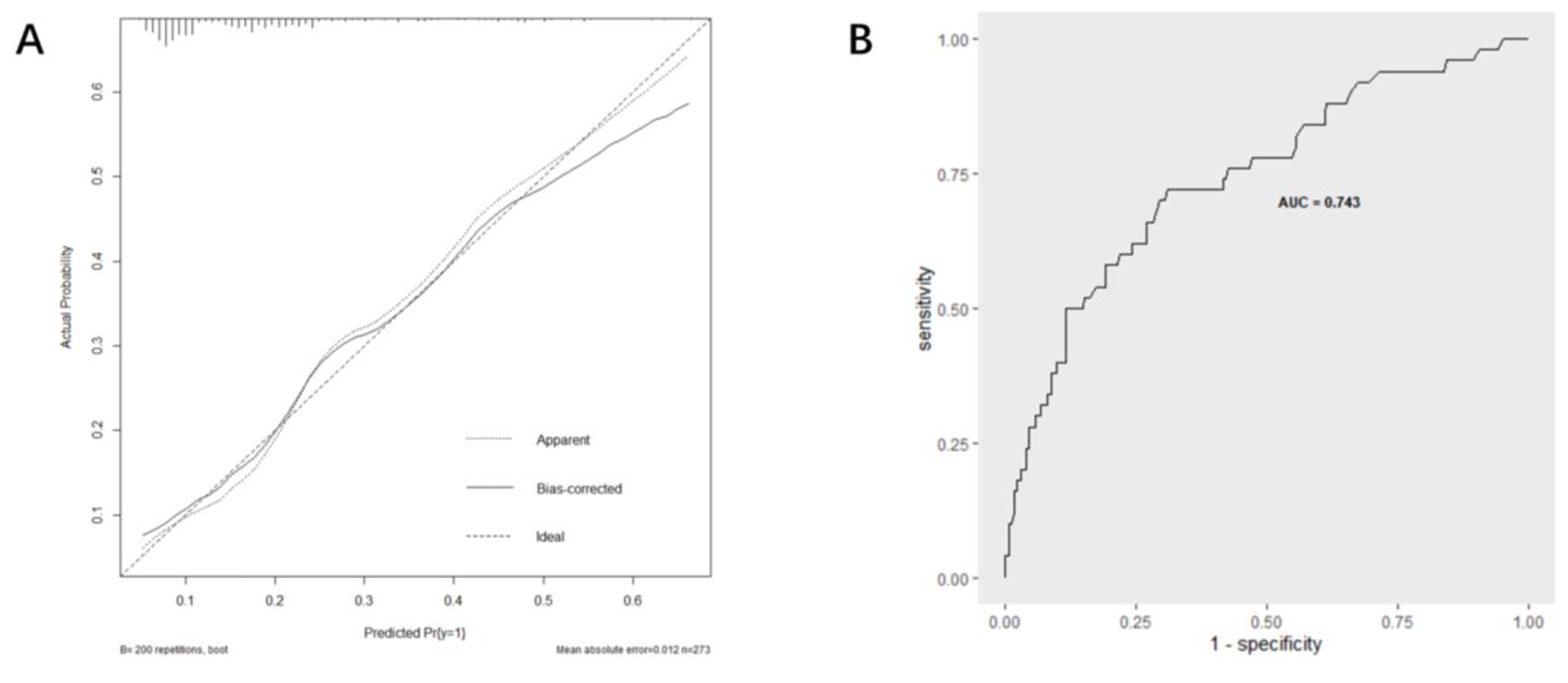
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fernström, I.; Johansson, B. Percutaneous Pyelolithotomy: A new extraction technique. Scand. J. Urol. Nephrol. 1976, 10, 257–259. [Google Scholar] [CrossRef]
- Pradère, B.; Doizi, S.; Proietti, S.; Brachlow, J.; Traxer, O. Evaluation of Guidelines for Surgical Management of Urolithiasis. J. Urol. 2017, 199, 1267–1271. [Google Scholar] [CrossRef]
- Türk, C.; Petřík, A.; Sarica, K.; Seitz, C.; Skolarikos, A.; Straub, M.; Knoll, T. EAU Guidelines on Interventional Treatment for Urolithiasis. Eur. Urol. 2016, 69, 475–482. [Google Scholar] [CrossRef]
- Jiang, Y.; Zhang, J.; Kang, N.; Niu, Y.; Li, Z.; Yu, C.; Zhang, J. Current Trends in Percutaneous Nephrolithotomy in China: A Spot Survey. Risk Manag. Heal. Policy 2021, 14, 2507–2515. [Google Scholar] [CrossRef]
- Maghsoudi, R.; Etemadian, M.; Kashi, A.H.; Mehravaran, K. Management of Colon Perforation During Percutaneous Nephro-lithotomy: 12 Years of Experience in a Referral Center. J. Endourol. 2017, 31, 1032–1036. [Google Scholar] [CrossRef] [PubMed]
- Gamal, W.M.; Hussein, M.; Aldahshoury, M.; Hammady, A.; Osman, M.; Moursy, E.; Abuzeid, A. Solo ultrasonography-guided percuta-nous nephrolithotomy for single stone pelvis. J. Endourol. 2011, 25, 593–596. [Google Scholar] [CrossRef] [PubMed]
- Jiang, E.; Guo, H.; Yang, B.; Li, P.; Mishra, P.; Yang, T.; Li, Y.; Wang, H. Predicting and comparing postoperative infections in different strati-fication following PCNL based on nomograms. Sci. Rep. 2020, 10, 11337. [Google Scholar] [CrossRef]
- Yang, T.; Liu, S.; Hu, J.; Wang, L.; Jiang, H. The Evaluation of Risk Factors for Postoperative Infectious Complications after Per-cutaneous Nephrolithotomy. Biomed. Res. Int. 2017, 2017, 4832051. [Google Scholar]
- Gutierrez, J.; Smith, A.; Geavlete, P.; Shah, H.; Kural, A.R.; de Sio, M.; Sesmero, J.H.A.; Hoznek, A.; de la Rosette, J. Urinary tract infections and post-operative fever in percutaneous nephrolithotomy. World J. Urol. 2012, 31, 1135–1140. [Google Scholar] [CrossRef]
- Liu, J.; Zhou, C.; Gao, W.; Huang, H.; Jiang, X.; Zhang, D. Does preoperative urine culture still play a role in predicting post-PCNL SIRS? A retrospective cohort study. Urolithiasis 2019, 48, 251–256. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Mi, Y.; Wu, S.; Shao, H.; Zhu, L.; Dai, F. Impact Factors and an Efficient Nomogram for Predicting the Occurrence of Sepsis after Percutaneous Nephrolithotomy. BioMed Res. Int. 2020, 2020, 6081768. [Google Scholar] [CrossRef]
- Erdil, T.; Bostanci, Y.; Ozden, E.; Atac, F.; Yakupoglu, Y.K.; Yilmaz, A.F.; Sarikaya, S. Risk factors for systemic inflammatory response syndrome following percutaneous nephrolithotomy. Urolithiasis 2013, 41, 395–401. [Google Scholar] [CrossRef]
- Korets, R.; Graversen, J.A.; Kates, M.; Mues, A.C.; Gupta, M. Post-Percutaneous Nephrolithotomy Systemic Inflammatory Response: A Prospective Analysis of Preoperative Urine, Renal Pelvic Urine and Stone Cultures. J. Urol. 2011, 186, 1899–1903. [Google Scholar] [CrossRef]
- Paonessa, J.E.; Gnessin, E.; Bhojani, N.; Williams, J.C., Jr.; Lingeman, J.E. Preoperative Bladder Urine Culture as a Predictor of In-traoperative Stone Culture Results: Clinical Implications and Relationship to Stone Composition. J. Urol. 2016, 196, 769–774. [Google Scholar] [CrossRef] [PubMed]
- Eswara, J.R.; Shariftabrizi, A.; Sacco, D. Positive stone culture is associated with a higher rate of sepsis after endourological procedures. Urolithiasis 2013, 41, 411–414. [Google Scholar] [CrossRef] [PubMed]
- Mariappan, P.; Smith, G.; Bariol, S.V.; Moussa, S.A.; Tolley, D.A. Stone and pelvic urine culture and sensitivity are better than bladder urine as predictors of urosepsis following percutaneous nephrolithotomy: A prospective clinical study. J. Urol. 2005, 173, 1610–1614. [Google Scholar] [CrossRef] [PubMed]
- Christaki, E.; Marcou, M.; Tofarides, A. Antimicrobial Resistance in Bacteria: Mechanisms, Evolution, and Persistence. J. Mol. Evol. 2019, 88, 26–40. [Google Scholar] [CrossRef]
- Liu, J.; Yang, Q.; Lan, J.; Hong, Y.; Huang, X.; Yang, B. Risk factors and prediction model of urosepsis in patients with diabetes after percutaneous nephrolithotomy. BMC Urol. 2021, 21, 74. [Google Scholar] [CrossRef]
- Chan, J.Y.; Wong, V.K.; Wong, J.; Paterson, R.F.; Lange, D.; Chew, B.H.; Scotland, K.B. Predictors of urosepsis in struvite stone patients after percutaneous nephrolithotomy. Investig. Clin. Urol. 2021, 62, 201–209. [Google Scholar] [CrossRef]
- Jiang, G.; Li, J.; Long, H.; Qiulin, C.; Jin, R.; Yaodong, Y.; Xingyou, D.; Jiang, Z.; Zhenyang, Z. Study on risk factors, bacterial species, and drug resistance of acute pyelonephritis associated with ureteral stent after percutaneous nephrolithotomy. Eur. J. Clin. Microbiol. Infect. Dis. 2020, 40, 707–713. [Google Scholar] [CrossRef]
- Gadzhiev, N.; Malkhasyan, V.; Akopyan, G.; Petrov, S.; Jefferson, F.; Okhunov, Z. Percutaneous nephrolithotomy for staghorn calculi: Troubleshooting and managing complications. Asian J. Urol. 2019, 7, 139–148. [Google Scholar] [CrossRef]
- Chen, D.; Jiang, C.; Liang, X.; Zhong, F.; Huang, J.; Lin, Y.; Zhao, Z.; Duan, X.; Zeng, G.; Wu, W. Early and rapid prediction of postoperative infections following percutaneous nephrolithotomy in patients with complex kidney stones. BJU Int. 2018, 123, 1041–1047. [Google Scholar] [CrossRef]
- Yang, Z.; Lin, D.; Hong, Y.; Hu, M.; Cai, W.; Pan, H.; Li, Q.; Lin, J.; Ye, L. The effect of preoperative urine culture and bacterial species on infection after percutaneous nephrolithotomy for patients with upper urinary tract stones. Sci. Rep. 2022, 12, 4833. [Google Scholar] [CrossRef] [PubMed]
- Chibelean, C.B.; Petca, R.-C.; Mareș, C.; Popescu, R.-I.; Enikő, B.; Mehedințu, C.; Petca, A. A Clinical Perspective on the Antimicrobial Resistance Spectrum of Uropathogens in a Romanian Male Population. Microorganisms 2020, 8, 848. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Jiang, F.; Xie, A.; Jiang, Y. Analysis of the Distribution and Drug Resistance of Pathogens in Patients with Urinary Tract Infection in the Eastern Chongming Area of Shanghai from 2018 to 2020. Infect. Drug Resist. 2022, 15, 6413–6422. [Google Scholar] [CrossRef] [PubMed]
- Gajdács, M.; Ábrók, M.; Lázár, A.; Burián, K. Increasing relevance of Gram-positive cocci in urinary tract infections: A 10-year analysis of their prevalence and resistance trends. Sci. Rep. 2020, 10, 17658. [Google Scholar] [CrossRef]
| Variables | UC (−) | UC (+) | p |
|---|---|---|---|
| Age (years) | 56 (47–64) | 60 (49–68) | 0.214 |
| Gender | 0.028 | ||
| Male, n (%) | 162 (86.2%) | 26 (13.8%) | |
| Female, n (%) | 64 (75.3%) | 21 (24.7%) | |
| BMI (Kg/m2) | 24.6 (22.5–27.0) | 23.4 (22.0–27.2) | 0.240 |
| Diabetes, n (%) | 44 (19.5%) | 4 (8.5%) | 0.091 |
| Hypertension, n (%) | 88 (38.9%) | 20 (42.6%) | 0.645 |
| Body temperature >37.5 °C | 11 (4.9%) | 5 (10.6%) | 0.125 |
| Number of stones | 0.205 | ||
| Solitary, n (%) | 47 (20.8%) | 6 (12.8%) | |
| Multiple, n (%) | 179 (79.2%) | 41 (87.2%) | |
| Staghorn calculi, n (%) | 49 (21.7%) | 21 (44.7%) | 0.001 |
| Hydronephrosis, n (%) | 195 (86.3%) | 39 (83.0%) | 0.556 |
| Largest stone size (cm) | 2.0 (1.5–2.5) | 2.5 (2.0–3.5) | 0.002 |
| Urine WBC ≥ 100, n (%) | 43 (19.0%) | 32 (68.1%) | <0.001 |
| Leukocyte esterase 3+ or higher, n (%) | 17 (7.5%) | 27 (57.4%) | <0.001 |
| Positive urine nitrite, n (%) | 5 (2.2%) | 10 (21.3%) | <0.001 |
| Preoperative neutrophile (109/L) | 4.0 (3.3–5.0) | 4.1 (3.2–5.5) | 0.549 |
| Preoperative lymphocyte (109/L) | 1.8 (1.5–2.2) | 2.0 (1.4–2.4) | 0.559 |
| Preoperative neutrophile-lymphocyte ratio | 2.2 (1.7–2.9) | 2.2 (1.6–3.1) | 0.922 |
| Elevated CRP, n (%) | 48 (21.2%) | 16 (34.0%) | 0.059 |
| AGR < 1.5, n (%) | 155 (68.6%) | 31 (66.0%) | 0.725 |
| Serum creatinine | 0.190 | ||
| Normal, n (%) | 170 (75.2%) | 31 (66.0%) | |
| Abnormal, n (%) | 56 (24.8%) | 16 (34.0%) | |
| Operation time (min) | 70 (53–85) | 65 (53–86) | 0.877 |
| SIRS, n (%) | 32 (14.2%) | 18 (38.3%) | <0.001 |
| Variables | Non-SIRS | SIRS | p |
|---|---|---|---|
| Age (years) | 57 (47–65) | 55 (48–62) | 0.443 |
| Gender | 0.411 | ||
| Male, n (%) | 156 (70.0%) | 32 (64.0%) | |
| Female, n (%) | 67 (30.0%) | 18 (36.0%) | |
| BMI (Kg/m2) | 24.5 (22.2–27.2) | 22.9 (22.6–25.8) | 0.509 |
| Diabetes, n (%) | 35 (15.7%) | 13 (26.0%) | 0.084 |
| Hypertension, n (%) | 87 (39.0%) | 21 (42.0%) | 0.696 |
| Body temperature >37.5 °C | 13 (5.8%) | 3 (6.0%) | 0.963 |
| Number of stones | 0.284 | ||
| Solitary, n (%) | 46 (20.6%) | 7 (14.0%) | |
| Multiple, n (%) | 177 (79.4%) | 43 (86.0%) | |
| Staghorn calculi, n (%) | 46 (20.6%) | 24 (48.0%) | <0.001 |
| Hydronephrosis, n (%) | 191 (85.7%) | 43 (86.0%) | 0.949 |
| Largest stone size (cm) | 2.0 (1.5–2.5) | 2.5 (2.0–3.5) | <0.001 |
| Urine WBC ≥ 100, n (%) | 54 (24.2%) | 21 (42.0%) | 0.011 |
| Leukocyte esterase 3+ or higher, n (%) | 29 (13.0%) | 15 (30.0%) | 0.003 |
| Positive urine nitrite, n (%) | 8 (3.6%) | 7 (14.0%) | 0.009 |
| Preoperative neutrophile (109/L) | 4.1 (3.3–5.1) | 4.0 (3.2–5.0) | 0.484 |
| Preoperative lymphocyte (109/L) | 1.8 (1.5–2.2) | 2.0 (1.6–2.7) | 0.021 |
| Preoperative NLR | 2.2 (1.8–3.0) | 2.0 (1.4–2.5) | 0.022 |
| Elevated CRP, n (%) | 52 (23.3%) | 12 (24.0%) | 0.918 |
| AGR < 1.5, n (%) | 151 (67.7%) | 35 (70.0%) | 0.754 |
| Serum creatinine | 0.437 | ||
| Normal, n (%) | 162 (72.6%) | 39 (78.0%) | |
| Abnormal, n (%) | 61 (27.4%) | 11 (22.0%) | |
| Operation time (min) | 64 (53–84) | 78 (64–90) | 0.007 |
| Positive urine culture, n (%) | 29 (13.0%) | 18 (36.0%) | <0.001 |
| Variables | Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | |
| Age | 0.992 | 0.967–1.017 | 0.519 | |||
| Gender | 0.764 | 0.401–1.455 | 0.412 | |||
| Male/female | ||||||
| BMI | 0.970 | 0.893–1.054 | 0.477 | |||
| Diabetes | 1.887 | 0.912–3.907 | 0.087 | 2.666 | 1.193–5.954 | 0.017 |
| Hypertension | 1.132 | 0.607–2.110 | 0.696 | |||
| Body temperature >37.5 °C | 1.031 | 0.283–3.763 | 0.963 | |||
| Number of stones | 1.596 | 0.674–3.781 | 0.288 | |||
| Multiple/solitary | ||||||
| Staghorn calculi | 3.552 | 1.868–6.754 | <0.001 | 2.924 | 1.467–5.830 | 0.002 |
| Hydronephrosis | 1.029 | 0.426–2.487 | 0.949 | |||
| Largest stone size | 1.925 | 1.360–2.723 | <0.001 | |||
| Urine WBC ≥ 100 | 2.266 | 1.195–4.297 | 0.012 | |||
| Leukocyte esterase 3+ or higher | 2.867 | 1.396–5.889 | 0.004 | |||
| Positive urine nitrite | 4.375 | 1.507–12.703 | 0.007 | |||
| Preoperative neutrophile | 1.056 | 0.967–1.153 | 0.224 | |||
| Preoperative lymphocyte | 1.060 | 0.905–1.243 | 0.470 | |||
| Preoperative NLR | 0.966 | 0.837–1.116 | 0.639 | |||
| Elevated CRP | 1.018 | 0.506–2.132 | 0.918 | |||
| AGR < 1.5 | 1.113 | 0.571–2.167 | 0.754 | |||
| Serum creatinine | 0.749 | 0.361–1.556 | 0.439 | |||
| Abnormal/normal | ||||||
| Operation time (min) | 1.014 | 1.003–1.025 | 0.015 | 1.013 | 1.001–1.025 | 0.036 |
| Positive urine culture | 3.763 | 1.874–7.554 | <0.001 | 3.607 | 1.680–7.741 | 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhou, H.; Xie, T.; Gao, Y.; Yao, X.; Xu, Y. The Relationship between Preoperative Urine Culture and Post-Percutaneous Nephrostolithotomy Systemic Inflammatory Response Syndrome: A Single-Center Retrospective Study. J. Pers. Med. 2023, 13, 187. https://doi.org/10.3390/jpm13020187
Zhou H, Xie T, Gao Y, Yao X, Xu Y. The Relationship between Preoperative Urine Culture and Post-Percutaneous Nephrostolithotomy Systemic Inflammatory Response Syndrome: A Single-Center Retrospective Study. Journal of Personalized Medicine. 2023; 13(2):187. https://doi.org/10.3390/jpm13020187
Chicago/Turabian StyleZhou, Hongmin, Tiancheng Xie, Yuchen Gao, Xudong Yao, and Yunfei Xu. 2023. "The Relationship between Preoperative Urine Culture and Post-Percutaneous Nephrostolithotomy Systemic Inflammatory Response Syndrome: A Single-Center Retrospective Study" Journal of Personalized Medicine 13, no. 2: 187. https://doi.org/10.3390/jpm13020187
APA StyleZhou, H., Xie, T., Gao, Y., Yao, X., & Xu, Y. (2023). The Relationship between Preoperative Urine Culture and Post-Percutaneous Nephrostolithotomy Systemic Inflammatory Response Syndrome: A Single-Center Retrospective Study. Journal of Personalized Medicine, 13(2), 187. https://doi.org/10.3390/jpm13020187







