Effect of the Duration of Restrictive Fluid Therapy on Acute Kidney Injury in Robot-Assisted Laparoscopic Prostatectomy
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethics Approval
2.2. Trial Registration
2.3. Patients
2.4. Study Protocol
2.4.1. Anesthesia
2.4.2. Fluid Administration
2.4.3. Surgery
2.4.4. Hemodynamic Monitoring
2.4.5. Additional Recorded Parameters
2.5. Statistical Analysis
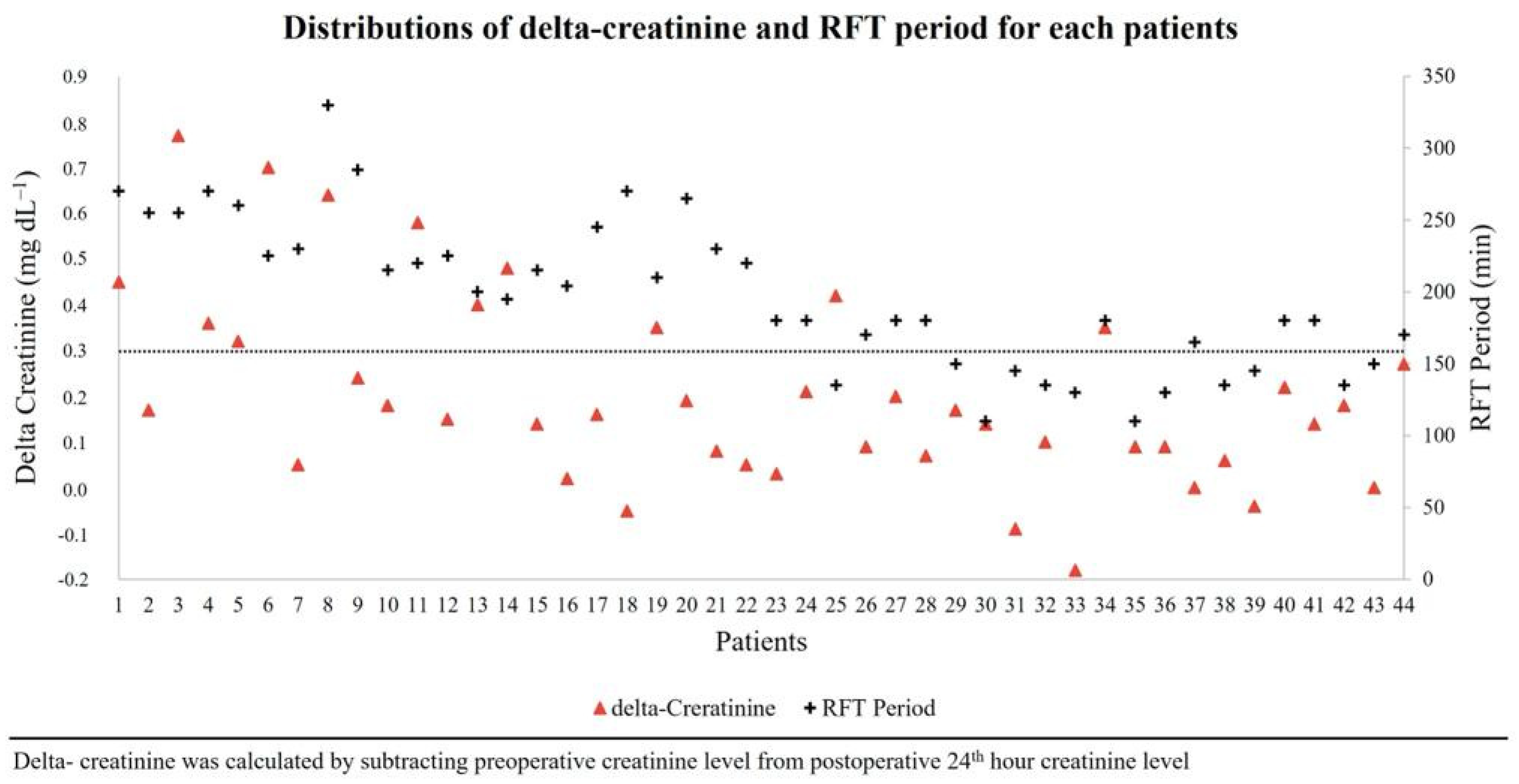
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ren, S.; Nathan, S.; Pavan, N.; Gu, D.; Sridhar, A.; Autorino, R. Robot-Assisted Radical Prostatectomy: Advanced Surgical Techniques; Springer Nature: Berlin/Heidelberg, Germany, 2022; ISBN 9783031058554. [Google Scholar]
- Chiumello, D.; Fratti, I.; Coppola, S. The Intraoperative Management of Robotic-Assisted Laparoscopic Prostatectomy. Curr. Opin. Anaesthesiol. 2023, 36, 657–665. [Google Scholar] [CrossRef]
- Awad, H.; Walker, C.M.; Shaikh, M.; Dimitrova, G.T.; Abaza, R.; O’Hara, J. Anesthetic Considerations for Robotic Prostatectomy: A Review of the Literature. J. Clin. Anesth. 2012, 24, 494–504. [Google Scholar] [CrossRef] [PubMed]
- Seo, D.Y.; Cho, H.J.; Cho, J.M.; Kang, J.Y.; Yoo, T.K. Experience with Robot-Assisted Laparoscopic Radical Prostatectomy at a Secondary Training Hospital: Operation Time, Treatment Outcomes, and Complications with the Accumulation of Experience. Korean J. Urol. 2013, 54, 522–526. [Google Scholar] [CrossRef] [PubMed]
- Wiesenthal, J.D.; Fazio, L.M.; Perks, A.E.; Blew, B.D.M.; Mazer, D.; Hare, G.; Honey, R.J.D.; Pace, K.T. Effect of Pneumoperitoneum on Renal Tissue Oxygenation and Blood Flow in a Rat Model. Urology 2011, 77, 1508.e9–1508.e15. [Google Scholar] [CrossRef] [PubMed]
- Sato, H.; Narita, S.; Saito, M.; Yamamoto, R.; Koizumi, A.; Nara, T.; Kanda, S.; Numakura, K.; Inoue, T.; Satoh, S.; et al. Acute Kidney Injury and Its Impact on Renal Prognosis after Robot-Assisted Laparoscopic Radical Prostatectomy. Int. J. Med. Robot. 2020, 16, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Mori, C.; Iwasaki, H.; Sato, I.; Takahoko, K.; Inaba, Y.; Kawasaki, Y.; Tamaki, G.; Kakizaki, H. Impact of Intraoperative Fluid Restriction on Renal Outcomes in Patients Undergoing Robotic-Assisted Laparoscopic Prostatectomy. J. Robot. Surg. 2023, 17, 1989–1993. [Google Scholar] [CrossRef] [PubMed]
- Khwaja, A. KDIGO Clinical Practice Guidelines for Acute Kidney Injury. Nephron 2012, 120, c179–c184. [Google Scholar] [CrossRef]
- Wrzosek, A.; Jakowicka-Wordliczek, J.; Zajaczkowska, R.; Serednicki, W.T.; Jankowski, M.; Bala, M.M.; Swierz, M.J.; Polak, M.; Wordliczek, J. Perioperative Restrictive versus Goal-Directed Fluid Therapy for Adults Undergoing Major Non-Cardiac Surgery. Cochrane Database Syst. Rev. 2019, 12, CD012767. [Google Scholar] [CrossRef]
- Zarbock, A.; Weiss, R.; Albert, F.; Rutledge, K.; Kellum, J.A.; Bellomo, R.; Grigoryev, E.; Candela-Toha, A.M.; Demir, Z.A.; Legros, V.; et al. Epidemiology of Surgery Associated Acute Kidney Injury (EPIS-AKI): A Prospective International Observational Multi-Center Clinical Study. Intensive Care Med. 2023. [Google Scholar] [CrossRef]
- Gainsburg, D.M. Anesthetic Concerns for Robotic-Assisted Laparoscopic Radical Prostatectomy. Minerva Anestesiol. 2012, 78, 596–604. [Google Scholar]
- Bishara, B.; Karram, T.; Khatib, S.; Ramadan, R.; Schwartz, H.; Hoffman, A.; Abassi, Z. Impact of Pneumoperitoneum on Renal Perfusion and Excretory Function: Beneficial Effects of Nitroglycerine. Surg. Endosc. 2009, 23, 568–576. [Google Scholar] [CrossRef]
- Abassi, Z.; Bishara, B.; Karram, T.; Khatib, S.; Winaver, J.; Hoffman, A. Adverse Effects of Pneumoperitoneum on Renal Function: Involvement of the Endothelin and Nitric Oxide Systems. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2008, 294, R842–R850. [Google Scholar] [CrossRef] [PubMed]
- Hirvonen, E.A.; Nuutinen, L.S.; Kauko, M. Hemodynamic Changes due to Trendelenburg Positioning and Pneumoperitoneum during Laparoscopic Hysterectomy. Acta Anaesthesiol. Scand. 1995, 39, 949–955. [Google Scholar] [CrossRef] [PubMed]
- Watt, D.G.; Horgan, P.G.; McMillan, D.C. Routine Clinical Markers of the Magnitude of the Systemic Inflammatory Response after Elective Operation: A Systematic Review. Surgery 2015, 157, 362–380. [Google Scholar] [CrossRef] [PubMed]
- Essber, H.; Cohen, B.; Artis, A.S.; Leung, S.M.; Maheshwari, K.; Khan, M.Z.; Sessler, D.I.; Turan, A.; Ruetzler, K. Renal Injury after Open versus Laparoscopic Non-Cardiac Surgery: A Retrospective Cohort Analysis. Braz. J. Anesthesiol. 2021, 71, 50–57. [Google Scholar] [CrossRef] [PubMed]
- Nishio, S.; Takeda, H.; Yokoyama, M. Changes in Urinary Output during Laparoscopic Adrenalectomy. BJU Int. 1999, 83, 944–947. [Google Scholar] [CrossRef]
- Ahn, J.H.; Lim, C.H.; Chung, H.I.; Choi, S.U.; Youn, S.Z.; Lim, H.J. Postoperative Renal Function in Patients Is Unaltered after Robotic-Assisted Radical Prostatectomy. Korean J. Anesthesiol. 2011, 60, 192–197. [Google Scholar] [CrossRef]
- Naito, A.; Taguchi, S.; Suzuki, M.; Kawai, T.; Uchida, K.; Fujimura, T.; Fukuhara, H.; Kume, H. Transient Acute Kidney Injury Observed Immediately after Robot-assisted Radical Prostatectomy but Not after Open Radical Prostatectomy. Mol. Clin. Oncol. 2020, 13, 18. [Google Scholar] [CrossRef]
- Katayama, S.; Mori, K.; Pradere, B.; Yanagisawa, T.; Mostafaei, H.; Quhal, F.; Motlagh, R.S.; Laukhtina, E.; Grossmann, N.C.; Rajwa, P.; et al. Influence of Steep Trendelenburg Position on Postoperative Complications: A Systematic Review and Meta-Analysis. J. Robot. Surg. 2022, 16, 1233–1247. [Google Scholar] [CrossRef]
- Pawlik, M.T.; Prasser, C.; Zeman, F.; Harth, M.; Burger, M.; Denzinger, S.; Blecha, S. Pronounced Haemodynamic Changes during and after Robotic-Assisted Laparoscopic Prostatectomy: A Prospective Observational Study. BMJ Open 2020, 10, e038045. [Google Scholar] [CrossRef]
- Hofer, C.K.; Zalunardo, M.P.; Klaghofer, R.; Spahr, T.; Pasch, T.; Zollinger, A. Changes in Intrathoracic Blood Volume Associated with Pneumoperitoneum and Positioning. Acta Anaesthesiol. Scand. 2002, 46, 303–308. [Google Scholar] [CrossRef] [PubMed]
- Haas, S.; Haese, A.; Goetz, A.E.; Kubitz, J.C. Haemodynamics and Cardiac Function during Robotic-Assisted Laparoscopic Prostatectomy in Steep Trendelenburg Position. Int. J. Med. Robot. 2011, 7, 408–413. [Google Scholar] [CrossRef] [PubMed]

| RFT Period ≤ 3 h (n = 22) | RFT Period > 3 h (n = 22) | p | |
|---|---|---|---|
| Age, years | 66 (61–72) | 66 (62–70) | 0.860 |
| BMI, kg m−2 | 27.1 ± 3.0 | 28.1 ± 4.5 | 0.393 |
| ASA | 2 (2–2) | 2 (2–2) | 0.780 |
| Comorbidities, n (%) | |||
| HT | 15 (68.2) | 16 (72.7) | 1.000 |
| DM | 5 (22.7) | 3 (13.6) | 0.698 |
| CAD | 3 (13.6) | 4 (18.2) | 1.000 |
| COPD | 3 (13.6) | 2 (9.1) | 1.000 |
| CVD | 0 (0.0) | 1 (4.5) | 1.000 |
| Preoperative laboratories | |||
| Hb, g dL−1 | 14.0 ± 1.5 | 14.0 ± 1.3 | 0.958 |
| Hct, % | 41.6 ± 4.2 | 42.0 ± 3.7 | 0.732 |
| Urea, mg dL−1 | 28 ± 11 | 31 ± 14 | 0.485 |
| Creatinine, mg dL−1 | 0.91 ± 0.11 | 0.96 ± 0.13 | 0.174 |
| Fasting, hour | 11 (10–14) | 10 (10–12) | 0.169 |
| Colonic cleansing, n (%) | 21 (95.5) | 21 (95.5) | 1.000 |
| RFT Period ≤ 3 h (n = 22) | RFT Period > 3 h (n = 22) | p | |
|---|---|---|---|
| Baseline hemodynamic parameters | |||
| HR, bpm | 69 (62–76) | 72 (66–79) | 0.221 |
| SAP, mmHg | 154 ± 13 | 156 ± 17 | 0.282 |
| DAP, mmHg | 79 ± 8 | 77 ± 10 | 0.241 |
| MAP, mmHg | 100 ± 11 | 103 ± 11 | 0.189 |
| SVI, ml/m2 | 48 ± 10 | 46 ± 13 | 0.610 |
| CI, L/min/m2 | 3.0 (2.8–3.5) | 3.0 (2.6–4.2) | 0.851 |
| Ea, L/min/m2 | 1.13 ± 0.27 | 1.09 ± 0.35 | 0.713 |
| dp/dt, mmHg/msn | 1.32 (1.22–1.56) | 1.30 (1.11–1.80) | 0.769 |
| CPO, watt | 1.40 (1.20–1.62) | 1.56 (1.08–2.00) | 0.690 |
| CCE, unit | 0.29 (0.10–0.44) | 0.27 (0.07–0.51) | 0.742 |
| Surgery time, min | 232 ± 42 | 293 ± 31 | <0.001 |
| Trendelenburg time, min | 201 (169–210) | 240 (223–256) | <0.001 |
| Console time, min | 150 (135–180) | 230 (215–266) | <0.001 |
| Intraoperative fluid administration, | |||
| pre-anastomosis, mL kg−1 h−1 | 1.2 ± 0.3 | 1.0 ± 0.4 | 0.434 |
| post-anastomosis, mL kg−1 h−1 | 9.7 (7.6–13.5) | 10.7 (8.2–14.6) | 0.091 |
| Total, mL kg−1 h−1 | 4.3 ± 1.0 | 3.0 ± 0.9 | <0.001 |
| The usage of drugs during the intraoperative period, n (%) | |||
| Ephedrine | 18 (81.8) | 17 (77.3) | 1.000 |
| Ephedrine (mg kg−1) | 0.13 (0.06–0.38) | 0.13 (0.05–0.27) | 0.795 |
| Norepinephrine | 1 (4.5) | 5 (22.7) | 0.185 |
| Norepinephrine (mcg kg−1) | 0.0 (0.0–0.0) | 0.0 (0.0–0.04) | 0.103 |
| Diuretics | 21 (95.5) | 21 (95.5) | 1.000 |
| Intraoperative cardiac events, n (%) | |||
| Hypotension (MAP < 60 mmg) | 8 (36.4) | 8 (36.4) | 1.000 |
| Arrhythmia | 0 (0.0) | 1 (4.5) | 1.000 |
| Ischemic changes in ECG | 0 (0.0) | 0 (0.0) | NS |
| Postoperative laboratories test results at 24th hour | |||
| Hb, g dL−1 | 12.8 (11.2–13.6) | 11.9 (10.9–12.9) | 0.323 |
| Hct, % | 36.6 (33.1–38.6) | 35.3 (32.0–37.9) | 0.459 |
| Urea, mg dL−1 | 28 ± 10 | 37 ± 11 | 0.006 |
| Creatinine, mg dL−1 | 1.0 ± 0.2 | 1.3 ± 0.3 | 0.007 |
| Troponin-I, ng mL−1 | 0.006(0.004–0.06) | 0.006 (0.004–0.011) | 0.728 |
| Total fluid intake at the end of the first 72 h after surgery, mL | 8155 ± 1328 | 8038 ± 846 | 0.730 |
| AKI, n (%) | 2 (9.1) | 10 (45.5) | 0.016 |
| Hemodynamic Parameters | RFT Period ≤ 3 h (n = 22) | RFT Period > 3 h (n = 22) | p |
|---|---|---|---|
| After anesthesia induction | |||
| HR, min−1 | 61 ± 10 | 65 ± 12 | 0.271 |
| SAP, mmHg | 105 ± 18 | 104 ± 18 | 0.843 |
| DAP, mmHg | 60 ± 10 | 59 ± 8 | 0.815 |
| MAP, mmHg | 74 ± 14 | 73 ± 11 | 0.624 |
| SVI, mL/m2 | 40 ± 9 | 36 ± 8 | 0.090 |
| CI, L/min/m2 | 2.3 (2.2–2.6) | 2.1 (2.0–2.4) | 0.078 |
| PPV, % | 8 (7–12) | 10 (8–16) | 0.168 |
| SVV, % | 8 (7–9) | 10 (6–13) | 0.137 |
| Ea, L/min/m2 | 0.95 (0.79–1.17) | 1.03 (0.92–1.30) | 0.366 |
| dP/dt, mmHg/msn | 0.76 (0.53–0.85) | 0.72 (0.52–0.93) | 0.869 |
| CPO, watt | 0.75 (0.67–0.94) | 0.74 (0.60–0.80) | 0.348 |
| CCE, unit | 0.06 ± 0.26 | 0.02 ± 0.28 | 0.580 |
| After 1 h in the Td position | |||
| HR, min−1 | 53 (49–59) | 55 (52–62) | 0.166 |
| SAP, mmHg | 96 ± 13 | 100 ± 15 | 0.271 |
| DAP, mmHg | 61 ± 8 | 66 ± 10 | 0.095 |
| MAP, mmHg | 73 ± 9 | 77 ± 12 | 0.175 |
| SVI, mL/m2 | 45 ± 10 | 39 ± 8 | 0.074 |
| CI, L/min/m2 | 2.4 ± 0.3 | 2.3 ± 0.3 | 0.320 |
| PPV, % | 11 ± 4 | 13 ± 5 | 0.156 |
| SVV, % | 9 ± 4 | 8 ± 3 | 0.512 |
| Ea, L/min/m2 | 0.73 (0.68–0.98) | 0.79 (0.76–1.01) | 0.326 |
| dP/dt, mmHg/msn | 0.43 (0.28–0.58) | 0.44 (0.31–0.50) | 0.879 |
| CPO, watt | 0.77 ± 0.15 | 0.80 ± 0.16 | 0.451 |
| CCE, unit | −0.21 ± 0.34 | −0.30 ± 0.35 | 0.391 |
| At the end of the console period | |||
| HR, min−1 | 60 (51–67) | 65 (59–71) | 0.041 |
| SAP, mmHg | 92 ± 19 | 102 ± 20 | 0.105 |
| DAP, mmHg | 54 ± 12 | 60 ± 12 | 0.125 |
| MAP, mmHg | 67 ± 16 | 73 ± 14 | 0.134 |
| SVI, ml/m2 | 38 ± 8 | 32 ± 8 | 0.016 |
| CI, L/min/m2 | 2.2 ± 0.3 | 2.1 ± 0.4 | 0.232 |
| PPV, % | 8 (6–10) | 9 (6–16) | 0.494 |
| SVV, % | 11 (7–12) | 8 (5–14) | 0.160 |
| Ea, L/min/m2 | 0.86 (0.70–0.99) | 1.07 (0.94–1.23) | <0.001 |
| dp/dt, mmHg/msn | 0.46 (0.39–0.63) | 0.48 (0.40–0.76) | 0.372 |
| CPO, watt | 0.68 ± 0.20 | 0.69 ± 0.21 | 0.810 |
| CCE, unit | −0.09 (−0.28, 0.22) | −0.27 (−0.40, 0.07) | 0.197 |
| Relative Risk (CI 95%) | p | |
|---|---|---|
| RFT ≤ 3 h plus | Ref | - |
| Total fluid > 3.3 mL/kg/h plus | ||
| SVI at the end of the console period ≥ 32 mL/m2 | ||
| RFT period > 3 h plus | 1.1 (0.1–22.7) | 0.972 |
| Total fluid > 3.3 mL/kg/h plus | ||
| SVI at the end of the console period ≥ 32 mL/m2 | ||
| RFT period > 3 h plus | 10.8 (1.4–82.6) | 0.022 |
| Total fluid ≤ 3.3 mL/kg/h plus | ||
| SVI at the end of the console period ≥ 32 mL/m2 | ||
| RFT period > 3 h plus | 12.0 (1.7–85.2) | 0.013 |
| Total fluid ≤ 3.3 mL/kg/h plus | ||
| SVI at the end of the console period < 32 mL/m2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aktas Yildirim, S.; Sarikaya, Z.T.; Dogan, L.; Gucyetmez, B.; Turkeri, L.; Toraman, F. Effect of the Duration of Restrictive Fluid Therapy on Acute Kidney Injury in Robot-Assisted Laparoscopic Prostatectomy. J. Pers. Med. 2023, 13, 1666. https://doi.org/10.3390/jpm13121666
Aktas Yildirim S, Sarikaya ZT, Dogan L, Gucyetmez B, Turkeri L, Toraman F. Effect of the Duration of Restrictive Fluid Therapy on Acute Kidney Injury in Robot-Assisted Laparoscopic Prostatectomy. Journal of Personalized Medicine. 2023; 13(12):1666. https://doi.org/10.3390/jpm13121666
Chicago/Turabian StyleAktas Yildirim, Serap, Zeynep Tugce Sarikaya, Lerzan Dogan, Bulent Gucyetmez, Levent Turkeri, and Fevzi Toraman. 2023. "Effect of the Duration of Restrictive Fluid Therapy on Acute Kidney Injury in Robot-Assisted Laparoscopic Prostatectomy" Journal of Personalized Medicine 13, no. 12: 1666. https://doi.org/10.3390/jpm13121666
APA StyleAktas Yildirim, S., Sarikaya, Z. T., Dogan, L., Gucyetmez, B., Turkeri, L., & Toraman, F. (2023). Effect of the Duration of Restrictive Fluid Therapy on Acute Kidney Injury in Robot-Assisted Laparoscopic Prostatectomy. Journal of Personalized Medicine, 13(12), 1666. https://doi.org/10.3390/jpm13121666






