Serum LH Level on the Day of hCG Administration as a Predictor of the Reproductive Outcomes in Ovulation Induction Cycle Frozen–Thawed Embryo Transfer
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Population
2.2. Serum Hormonal and Ultrasound Assays
2.3. Treatment Protocol
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| LH | Luteinizing hormone |
| FET | Frozen embryo transfer |
| OI | Ovulation induction |
| hCG | Human chorionic gonadotropin |
| FSH | Follicle-stimulating hormone |
| E2 | Estradiol |
| AFC | Antral follicle count |
| ART | Assisted reproductive technology |
| PGD/PGS | Pre-implantation genetic diagnosis/screening |
| OHSS | Ovarian hyperstimulation syndrome |
| GnRH | Gonadotropin-releasing hormone |
References
- Mackens, S.; Santos-Ribeiro, S.; van de Vijver, A. Frozen embryo transfer: A review on the optimal endometrial preparation and timing. Hum. Reprod. 2017, 32, 2234–2242. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, N.; Enatsu, N.; Iwasaki, T.; Otsuki, J.; Matsumoto, Y.; Kokeguchi, S.; Shiotani, M. Predictive factors influencing pregnancy rate in frozen embryo transfer. Reprod. Med. Biol. 2020, 19, 182–188. [Google Scholar] [CrossRef]
- Sehring, J.; Beltsos, A.; Jeelani, R. Human implantation: The complex interplay between endometrial receptivity, inflammation, and the microbiome. Placenta 2021, 117, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Labarta, E.; Sebastian-Leon, P.; Devesa-Peiro, A.; Celada, P.; Vidal, C.; Giles, J.; Rodriguez-Varela, C.; Bosch, E.; Diaz-Gimeno, P. Analysis of serum and endometrial progesterone in determining endometrial receptivity. Hum. Reprod. 2021, 36, 2861–2870. [Google Scholar] [CrossRef] [PubMed]
- Casper, R.F.; Yanushpolsky, E.H. Optimal endometrial preparation for frozen embryo transfer cycles: Window of implantation and progesterone support. Fertil. Steril. 2016, 105, 867–872. [Google Scholar] [CrossRef]
- Lessey, B.A.; Young, S.L. What exactly is endometrial receptivity? Fertil. Steril. 2019, 111, 611–617. [Google Scholar] [CrossRef]
- Mumusoglu, S.; Polat, M.; Ozbek, I.Y.; Bozdag, G.; Papanikolaou, E.G.; Esteves, S.C.; Humaidan, P.; Yarali, H. Preparation of the Endometrium for Frozen Embryo Transfer: A Systematic Review. Front. Endocrinol. 2021, 12, 688237. [Google Scholar] [CrossRef]
- Paulson, R.J. Introduction: Endometrial receptivity: Evaluation, induction and inhibition. Fertil. Steril. 2019, 111, 609–610. [Google Scholar] [CrossRef]
- Zhang, W.B.; Li, Q.; Liu, H.; Chen, W.J.; Zhang, C.L.; Li, H.; Lu, X.; Chen, J.L.; Li, L.; Wu, H.; et al. Transcriptomic analysis of endometrial receptivity for a genomic diagnostics model of Chinese women. Fertil. Steril. 2021, 116, 157–164. [Google Scholar] [CrossRef]
- Yatsenko, S.A.; Rajkovic, A. Genetics of human female infertility. Biol. Reprod. 2019, 101, 549–566. [Google Scholar] [CrossRef]
- Siristatidis, C.; Arkoulis, T.; Christoforidis, N.; Salamalekis, G.; Koutlaki, N.; Karageorgiou, V.; Profer, D.; Vlahos, N.; Galazios, G. Investigating the impact of different strategies for endometrial preparation in frozen cycles considering normal responders undergoing IVF/ICSI cycles: A multicenter retrospective cohort study. Syst. Biol. Reprod. Med. 2021, 67, 201–208. [Google Scholar] [CrossRef] [PubMed]
- Eleftheriadou, A.; Francis, A.; Wilcox, M.; Jayaprakasan, K. Frozen Blastocyst Embryo Transfer: Comparison of Protocols and Factors Influencing Outcome. J. Clin. Med. 2022, 11, 737. [Google Scholar] [CrossRef] [PubMed]
- An, J.; Li, L.; Zhang, X.; Liu, L.; Wang, L.; Zhang, X. A clinical and basic study of optimal endometrial preparation protocols for patients with infertility undergoing frozen-thawed embryo transfer. Exp. Ther. Med. 2020, 20, 2191–2199. [Google Scholar] [CrossRef]
- Mann, O.N.; Kong, C.-S.; Lucas, E.S.; Brosens, J.J.; Hanyaloglu, A.C.; Brighton, P.J. Expression and function of the luteinizing hormone choriogonadotropin receptor in human endometrial stromal cells. Sci. Rep. 2022, 12, 8624. [Google Scholar] [CrossRef] [PubMed]
- Khoury, S.; Kadour-Peero, E.; Calderon, I. The effect of LH rise during artificial frozen-thawed embryo transfer (FET) cycles. Reprod. Fertil. 2021, 2, 231–235. [Google Scholar] [CrossRef] [PubMed]
- Zhou, R.; Zhang, X.; Dong, M.; Huang, L.; Zhu, X.; Wang, S.; Liu, F. Association between endogenous LH level prior to progesterone administration and live birth rate in artificial frozen-thawed blastocyst transfer cycles of ovulatory women. Hum. Reprod. 2021, 36, 2687–2696. [Google Scholar] [CrossRef] [PubMed]
- Thomsen, L.H.; Kesmodel, U.S.; Erb, K.; Bungum, L.; Pedersen, D.; Hauge, B.; Elbæk, H.O.; Povlsen, B.B.; Andersen, C.Y.; Humaidan, P. The impact of luteal serum progesterone levels on live birth rates—A prospective study of 602 IVF/ICSI cycles. Hum. Reprod. 2018, 33, 1506–1516. [Google Scholar] [CrossRef] [PubMed]
- Han, S.; Liu, M.H.; Lv, Y.S.; Ren, H.Y.; Guo, J.; Li, Y.; Liu, S. Effects of Low Luteinizing Hormone During Ovarian Stimulation on Endometrial Gene Expression and Function—Transcriptome Analysis During the Implantation Window. Reprod. Sci. 2022, 29, 1908–1920. [Google Scholar] [CrossRef]
- Vuong, L.N.; Ho, T.M.; Pham, T.D.; Ho, V.N.A.; Andersen, C.Y.; Humaidan, P. The early luteal hormonal profile in IVF patients triggered with hCG. Hum. Reprod. 2020, 35, 157–166. [Google Scholar] [CrossRef]
- Reichman, D.E.; Stewart, C.R.; Rosenwaks, Z. Natural frozen embryo transfer with hCG booster leads to improved cycle outcomes: A retrospective cohort study. J. Assist. Reprod. Genet. 2020, 37, 1177–1182. [Google Scholar] [CrossRef]
- Onogi, S.; Ezoe, K.; Nishihara, S.; Fukuda, J.; Kobayashi, T.; Kato, K. Endometrial thickness on the day of the LH surge: An effective predictor of pregnancy outcomes after modified natural cycle-frozen blastocyst transfer. Hum. Reprod. Open 2020, 2020, hoaa060. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Li, Z.; Ren, X.; Huang, B.; Zhu, G.; Yang, W.; Jin, L. Endometrial thickness as a predictor of the reproductive outcomes in fresh and frozen embryo transfer cycles. Medicine 2018, 97, e9689. [Google Scholar] [CrossRef] [PubMed]
- Martel, R.A.; Blakemore, J.K.; Grifo, J.A. The effect of endometrial thickness on live birth outcomes in women undergoing hormone-replaced frozen embryo transfer. Fertil. Steril. Rep. 2021, 2, 150–155. [Google Scholar] [CrossRef] [PubMed]
- Shalom-Paz, E.; Atia, N.; Atzmon, Y.; Hallak, M.; Shrim, A. The effect of endometrial thickness and pattern on the success of frozen embryo transfer cycles and gestational age accuracy. Gynecol. Endocrinol. 2021, 37, 428–432. [Google Scholar] [CrossRef] [PubMed]
| Clinical Parameters | Frozen-Thawed Enbryo Transfer (n = 250) |
|---|---|
| Age of woman (yr) | 34.29 ± 5.66 |
| LH on hCG day (mIU/mL) | 18.9 ± 23.86 |
| Endometrial thickness (mm) | 8.4 ± 1.58 |
| BMI (kg/m2) | 22.8 ± 2.90 |
| AFC (#) | 13.8 ± 6.47 |
| Basal FSH (MIU/mL) | 7.98 ± 3.23 |
| Basal LH (MIU/mL) | 4.87 ± 2.95 |
| Basal E2 (pg/nL) | 50.33 ± 32.67 |
| Duration of infertility(yr) | 4.37 ± 3.62 |
| E2 on hCG day (pg/mL) | 717.31 ± 549.55 |
| No. of embryos transferred | 1.74 ± 0.44 |
| Tine of HMG(d) | 9.41 ± 5.52 |
| No. of total retrieved oocytes | 11 ± 6.63 |
| Total HMG dose (IU) | 941.56 ± 879.44 |
| No. of total retrieved enbryos | 5.1 ± 3.47 |
| No. of ICSI cases | 25.2% (63/250) |
| Clinical pregnancy rate | 49.6% (124/250) |
| Live birth rate | 35.2% (88/250) |
| Primary infertility | 40.4% (101/250) |
| Secondary infertility | 59. 61 (149/250) |
| Pregnant Group (n = 124) | Non—Pregnant Group (n = 126) | p-Value | Live Birth (n = 87) | Nonlive Birth (n = 163) | p-Value | |
|---|---|---|---|---|---|---|
| Age of woman (yr) | 32.11 ± 4.39 | 36.44 ± 5.97 | 0 | 31.86 ± 4.26 | 35.59 ± 5.9 | 0 |
| LH on hCG day (mIU/mL) | 14.32 ± 15.88 | 23.42 ± 28.51 | 0.002 | 15.42 ± 16.6 | 20.45 ± 26.61 | NS |
| Endometrial thickness (mm) | 8.69 ± 1.83 | 8.11 ± 1.23 | 0.003 | 8.84 ± 1.77 | 8.17 ± 1.43 | 0.003 |
| BMI (kg/m2) | 22.8 ± 3.1 | 22.81 ± 2.71 | NS | 22.47 ± 2.94 | 22.95 ± 2.85 | NS |
| AFC (#) | 15.12 ± 6.48 | 12.54 ± 6.21 | 0.001 | 14.51 ± 6.33 | 13.45 ± 6.55 | NS |
| Basal FSH (mIU/mL) | 7.5 ± 2.99 | 8.45 ± 3.4 | NS | 7.69 ± 3.33 | 8.13 ± 3.17 | NS |
| Basal LH (mIU/mL) | 5.09 ± 3.09 | 4.64 ± 2.79 | NS | 4.91 ± 2.93 | 4.82 ± 2.96 | NS |
| Basal E2 (pg/mL) | 50.26 ± 30.7 | 50.39 ± 34.62 | NS | 50.18 ± 28.79 | 50.58 ± 34.68 | NS |
| Duration of infertility(yr) | 3.93 ± 2.65 | 4.8 ± 4.34 | NS | 4.16 ± 2.76 | 4.48 ± 4.0 | NS |
| E2 on hCG day (pg/mL) | 690.85 ± 588.45 | 717.31 ± 509.02 | NS | 640.3 ± 441.32 | 737.96 ± 597.87 | NS |
| No. of enbryos transferred | 1.85 ± 0.35 | 1.63 ± 0.49 | 0 | 1.86 ± 0.34 | 1.67 ± 0.46 | 0 |
| Time of HMG(d) | 9.71 ± 5.28 | 9.06 ± 5.8 | NS | 9.11 ± 4.35 | 9.53 ± 6.13 | NS |
| Total HMG dose (IU) | 995.8 ± 887.56 | 877.42 ± 870.12 | NS | 902.96 ± 626.02 | 957.13 ± 950.26 | NS |
| No. of total embryos | 6.02 ± 3.67 | 4.19 ± 3.02 | 0 | 6.18 ± 3.91 | 4.51 ± 3.06 | 0.001 |
| No. of IVF cases | 75.81% (94/124) | 73.81% (93/126) | NS | 78.16% (68/87) | 73% (119/163) | NS |
| Primary infertility | 42.74% (53/124) | 38.1% (48/126) | NS | 45.97 (40/87) | 37.42% (61/163) | NS |
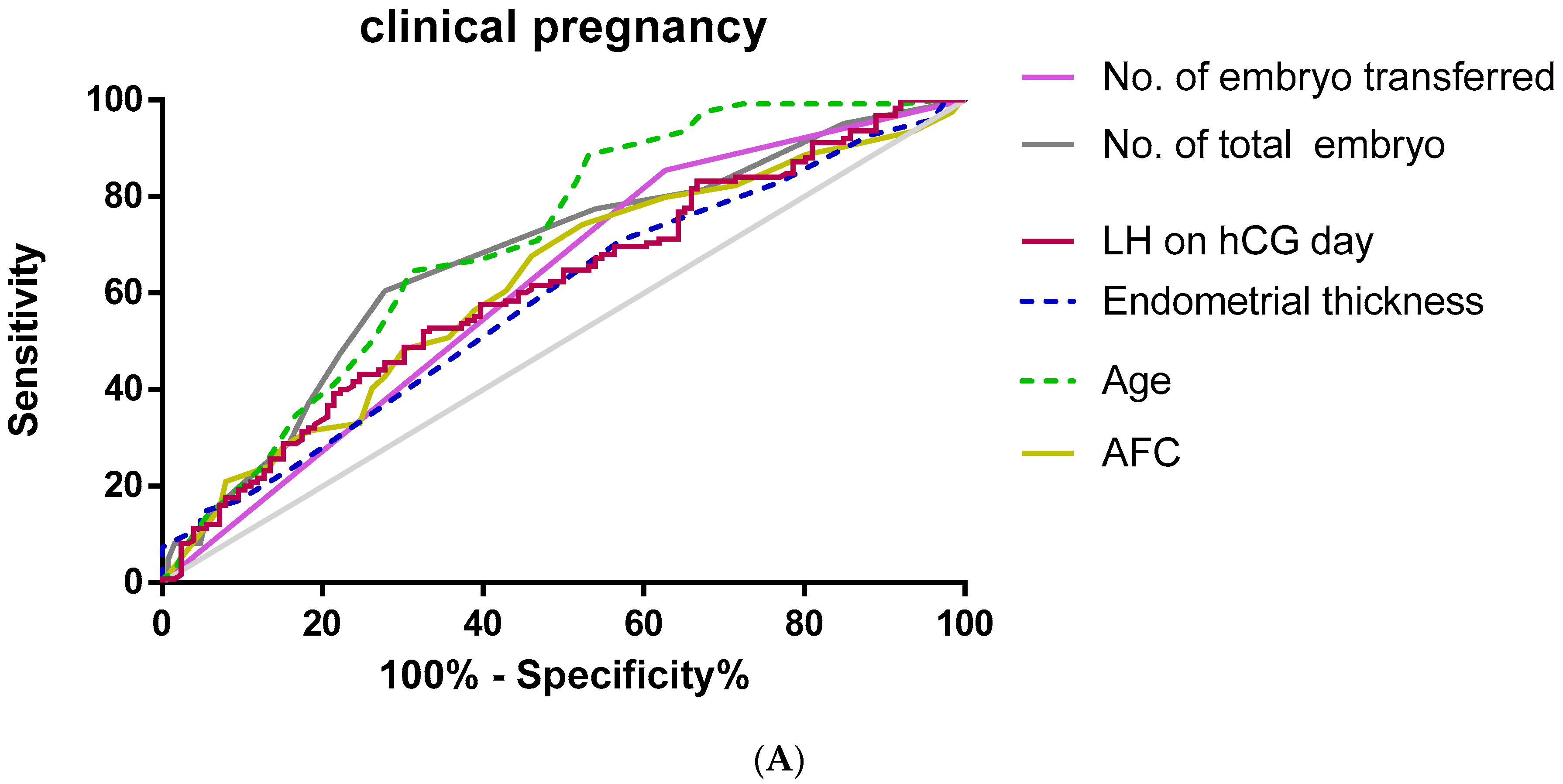
| Area under Curve | 95% CI | Cut-Off Value | Sensitivity | Specificity | p-Value | |
|---|---|---|---|---|---|---|
| LH on hCG day (mIU/mL) | 0.609 | 0.539–0.678 | 8.46 | 51.6 | 67.5 | 0.003 |
| Age of woman (yr) | 0.707 | 0.642–0.771 | 37.5 | 88.7 | 46.8 | 0 |
| Endometrial thickness (m) | 0.583 | 0.513–0.654 | 7.75 | 71 | 42.9 | 0.023 |
| AFC (#) | 0.619 | 0.549–0.689 | 10.5 | 74.2 | 47.6 | 0.001 |
| No. of enbryos transferred | 0.614 | 0.544–0.684 | 1.5 | 85.5 | 37.3 | 0.002 |
| No. of total enbryos | 0.67 | 0.603–0.737 | 4.5 | 60.5 | 72.7 | 0 |
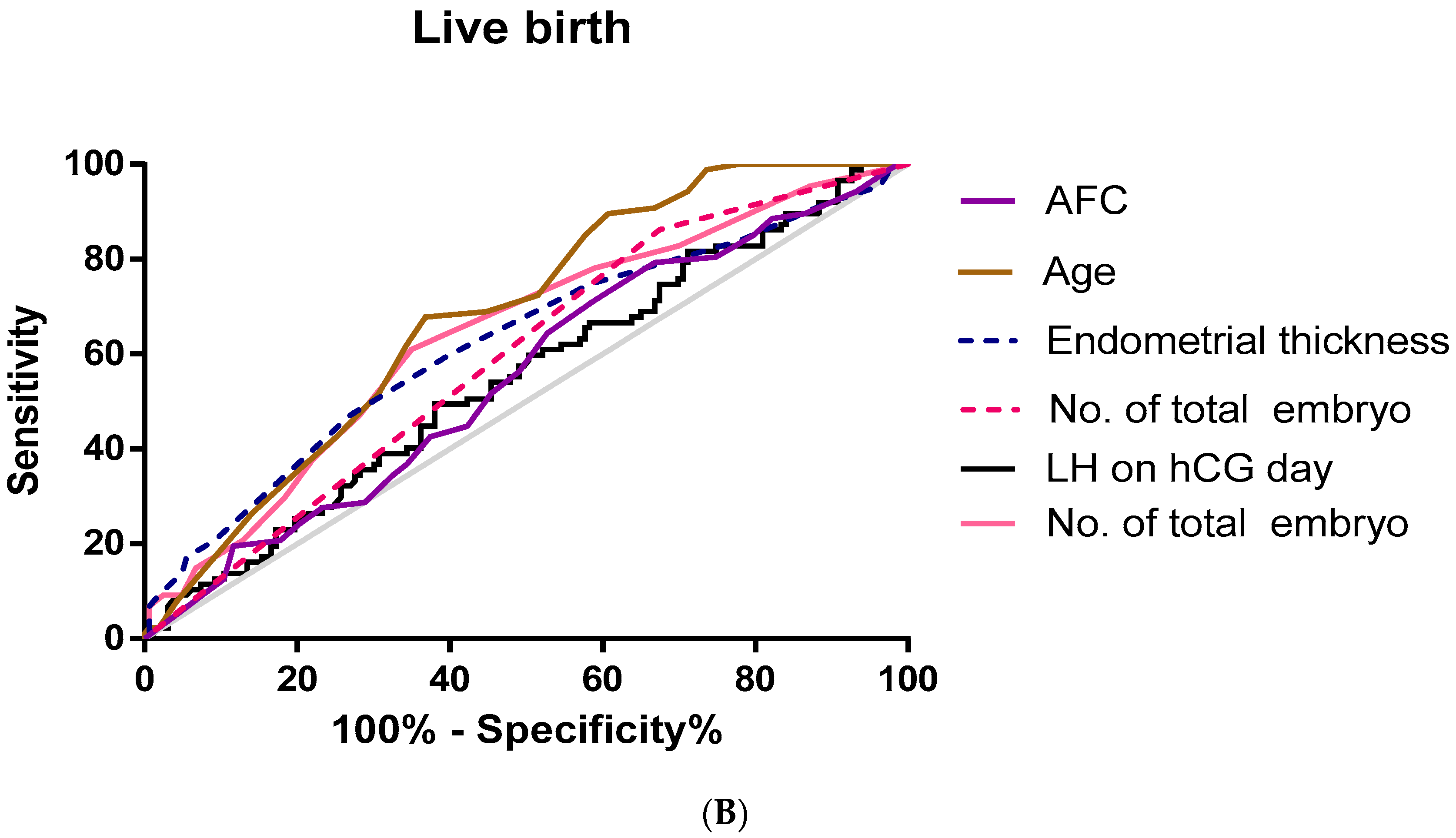
| Area under Curve | 95% CI | Cut-Off Value | Sensitivity | Specificity | p-Value | |
|---|---|---|---|---|---|---|
| LH on hCG day (mIU/mL) | 0.55 | 0.476–0.625 | 8.46 | 49.4 | 62 | 0.038 |
| Age of woman (yr) | 0.679 | 0.514–0.745 | 33.5 | 67.8 | 63.2 | 0 |
| Endometrial thickness (m) | 0.623 | 0.549–0.698 | 8.75 | 47.1 | 73 | 0.001 |
| AFC (#) | 0.552 | 0.478–0.626 | 10.5 | 71.3 | 41.1 | NS |
| No. of enbryos transferred | 0.594 | 0.522–0.665 | 1.5 | 86.2 | 32.5 | 0.015 |
| No. of total enbryos | 0.64 | 0.569–0.711 | 4.5 | 60.9 | 65 | 0 |
| Clinical Pregnancy | Live Birth | |||||
|---|---|---|---|---|---|---|
| p | OR | 95% CI | p | OR | 95% CI | |
| LH on hCG day (mIU/mL) | 0.02 | 1.02 | 1.0–1.03 | 0.241 | 0.992 | 0.978–1.006 |
| Age of woman (yr) | 0 | 1.13 | 1.07–1.2 | 0 | 0.884 | 0.830–0.942 |
| Endometrial thickness (mm) | 0.108 | 0.85 | 0.69–1.04 | 0.008 | 1.317 | 1.075–1.612 |
| AFC (#) | 0.3 | 1.03 | 0.98–1.09 | 0.005 | 0.92 | 0.867–0.975 |
| No. of enbryos transferred | 0.006 | 0.38 | 0.19–0.75 | 0.008 | 2.816 | 1.308–6.061 |
| No. of total enbryos | 0.04 | 0.86 | 0.78–0.95 | 0.001 | 1.183 | 1.072–1.306 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shi, Q.; Jiang, Y.; Kong, N.; Huang, C.; Liu, J.; Shen, X.; Sun, Y.; Lu, F.; Mei, J.; Zhou, J. Serum LH Level on the Day of hCG Administration as a Predictor of the Reproductive Outcomes in Ovulation Induction Cycle Frozen–Thawed Embryo Transfer. J. Pers. Med. 2023, 13, 52. https://doi.org/10.3390/jpm13010052
Shi Q, Jiang Y, Kong N, Huang C, Liu J, Shen X, Sun Y, Lu F, Mei J, Zhou J. Serum LH Level on the Day of hCG Administration as a Predictor of the Reproductive Outcomes in Ovulation Induction Cycle Frozen–Thawed Embryo Transfer. Journal of Personalized Medicine. 2023; 13(1):52. https://doi.org/10.3390/jpm13010052
Chicago/Turabian StyleShi, Qingqing, Yue Jiang, Na Kong, Chenyang Huang, Jingyu Liu, Xiaoyue Shen, Yanxin Sun, Feifei Lu, Jie Mei, and Jianjun Zhou. 2023. "Serum LH Level on the Day of hCG Administration as a Predictor of the Reproductive Outcomes in Ovulation Induction Cycle Frozen–Thawed Embryo Transfer" Journal of Personalized Medicine 13, no. 1: 52. https://doi.org/10.3390/jpm13010052
APA StyleShi, Q., Jiang, Y., Kong, N., Huang, C., Liu, J., Shen, X., Sun, Y., Lu, F., Mei, J., & Zhou, J. (2023). Serum LH Level on the Day of hCG Administration as a Predictor of the Reproductive Outcomes in Ovulation Induction Cycle Frozen–Thawed Embryo Transfer. Journal of Personalized Medicine, 13(1), 52. https://doi.org/10.3390/jpm13010052






