The Short-Term Efficacy of Large-Focused and Controlled-Unfocused (Radial) Extracorporeal Shock Wave Therapies in the Treatment of Hip Osteoarthritis
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Considerations
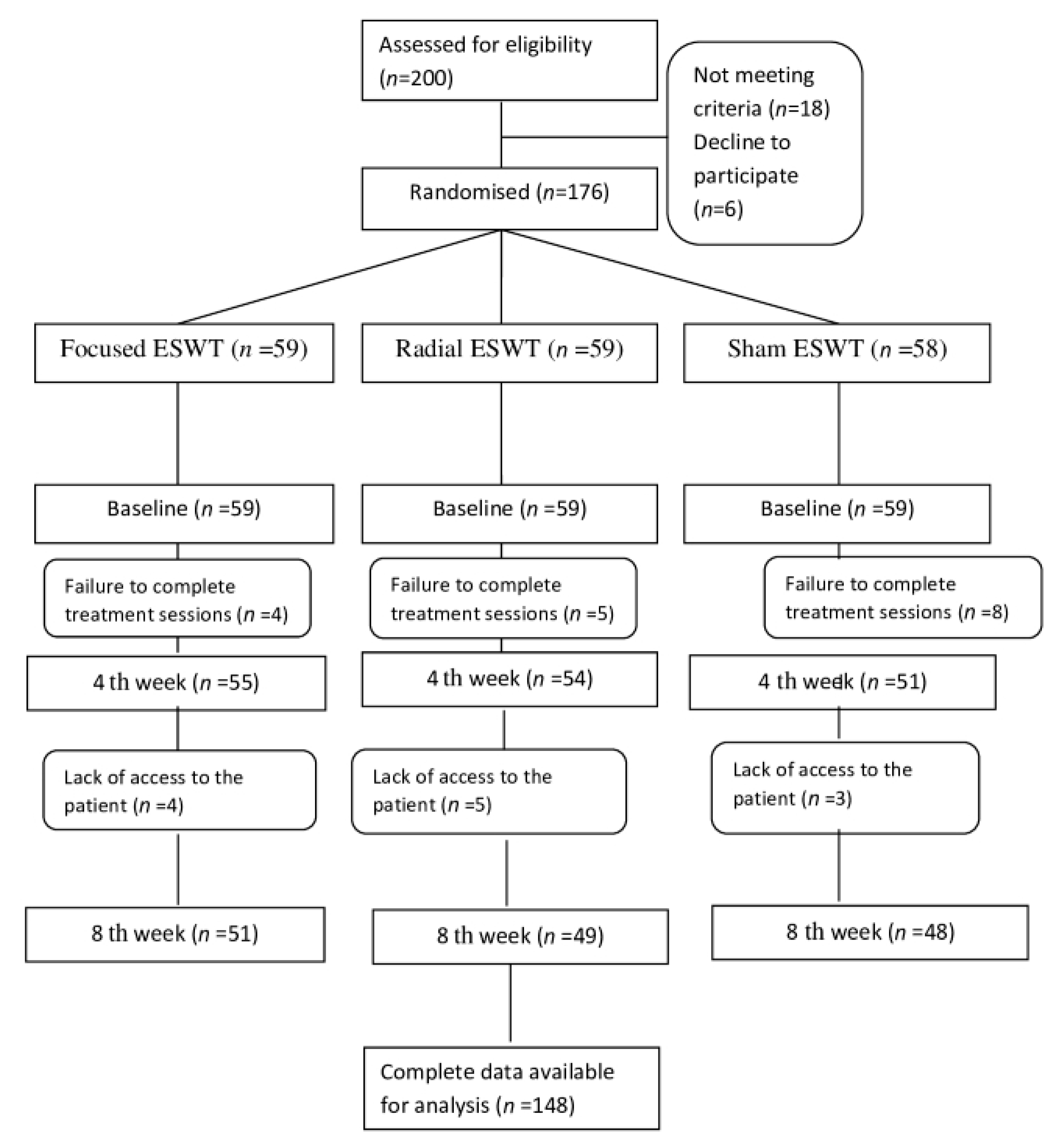
2.2. Study Design
2.3. Estimation of Sample Size and Study Power
2.4. Blinding
2.5. Participants
2.6. Inclusion/Exclusion Criteria
2.7. Randomization
2.8. Interventions
2.9. Outcome Measures
2.10. Statistical Analysis
- In the f-ESWT Group: VAS (baseline–4th week) and WOMAC stiffness (baseline–4th week);
- In the r-ESWT Group: VAS (baseline–8th week), WOMAC stiffness (baseline–4th week), and WOMAC stiffness (baseline–8th week);
- In the s-ESWT Group: VAS (baseline–4th week), VAS (baseline–8th week), WOMAC pain (baseline–4th week), WOMAC pain (baseline–8th week), WOMAC stiffness (baseline–8th week), WOMAC function (baseline–8th week), and WOMAC total (baseline–8th week).
3. Results
4. Discussion
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Katz, J.N.; Arant, K.R.; Loeser, R.F. Diagnosis and Treatment of Hip and Knee Osteoarthritis: A Review. JAMA—J. Am. Med. Assoc. 2021, 325, 568–578. [Google Scholar] [CrossRef] [PubMed]
- Bijlsma, J.W.J.; Knahr, K. Strategies for the Prevention and Management of Osteoarthritis of the Hip and Knee. Best Pract. Res. Clin. Rheumatol. 2007, 21, 59–76. [Google Scholar] [CrossRef]
- Jordan, J.M.; Helmick, C.G.; Renner, J.B.; Luta, G.; Dragomir, A.D.; Woodard, J.; Fang, F.; Schwartz, T.A.; Nelson, A.E.; Abbate, L.M.; et al. Prevalence of Hip Symptoms and Radiographic and Symptomatic Hip Osteoarthritis in African Americans and Caucasians: The Johnston County Osteoarthritis Project. J. Rheumatol. 2009, 36, 809–815. [Google Scholar] [CrossRef] [PubMed]
- Brown, T.D.; Johnston, R.C.; Saltzman, C.L.; Marsh, J.L.; Buckwalter, J.A. Posttraumatic Osteoarthritis: A First Estimate of Incidence, Prevalence, and Burden of Disease. J. Orthop. Trauma 2006, 20, 739–744. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.C.; Choudhry, N.; Franklin, J.M.; Bykov, K.; Eikermann, M.; Lii, J.; Fischer, M.A.; Bateman, B.T. Patterns and Predictors of Persistent Opioid Use Following Hip or Knee Arthroplasty. Osteoarthr. Cartil. 2017, 25, 1399–1406. [Google Scholar] [CrossRef] [PubMed]
- Losina, E.; Walensky, R.P.; Kessler, C.L.; Emrani, P.S.; Reichmann, W.M.; Wright, E.A.; Holt, H.L.; Solomon, D.H.; Yelin, E.; Paltiel, A.D.; et al. Cost-Effectiveness of Total Knee Arthroplasty in the United States: Patient Risk and Hospital Volume. Arch. Intern. Med. 2009, 169, 1113–1121. [Google Scholar] [CrossRef]
- Rhon, D. Re: Zhang W, Moskowitz RW, Nuki G; et al. OARSI Recommendations for the Management of Hip and Knee Osteoarthritis, Part II: OARSI Evidence-Based, Expert Consensus Guidelines. Osteoarthritis Cartilage 2008;16:137-62. Osteoarthr. Cartil. 2008, 16, 1585. [Google Scholar] [CrossRef]
- Sofat, N.; Ejindu, V.; Kiely, P. What Makes Osteoarthritis Painful? The Evidence for Local and Central Pain Processing. Rheumatology 2011, 50, 2157–2165. [Google Scholar] [CrossRef]
- Wang, C.; Wang, F.; Yang, K.D.; Weng, L.; Hsu, C.; Huang, C.; Yang, L. Shock Wave Therapy Induces Neovascularization at the Tendon–Bone Junction. A Study in Rabbits. J. Orthop. Res. 2003, 21, 984–989. [Google Scholar] [CrossRef]
- Buchbinder, R.; Forbes, A.; Ptasznik, R.; Rompe, J.D. Shock-Wave Therapy for Plantar Fasciitis/JA Ogden, RG Alvarez, and RL Levitt Reply. J. Bone Jt. Surg. 2005, 87, 680. [Google Scholar] [CrossRef]
- Sems, A.; Dimeff, R.; Iannotti, J.P. Extracorporeal Shock Wave Therapy in the Treatment of Chronic Tendinopathies. JAAOS-J. Am. Acad. Orthop. Surg. 2006, 14, 195–204. [Google Scholar] [CrossRef] [PubMed]
- Lizis, P.; Kobza, W.; Manko, G. Extracorporeal Shockwave Therapy vs. Kinesiotherapy for Osteoarthritis of the Knee: A Pilot Randomized Controlled Trial. J. Back Musculoskelet. Rehabil. 2017, 30, 1121–1128. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Kim, J.Y.; Choi, C.M.; Lee, J.K.; Kee, H.S.; Jung, K.I.; Yoon, S.R. The Dose-Related Effects of Extracorporeal Shock Wave Therapy for Knee Osteoarthritis. Ann. Rehabil. Med. 2015, 39, 616–623. [Google Scholar] [CrossRef] [PubMed]
- Moya, D.; Ramón, S.; Schaden, W.; Wang, C.J.; Guiloff, L.; Cheng, J.H. The Role of Extracorporeal Shockwave Treatment in Musculoskeletal Disorders. J. Bone Jt. Surg.-Am. Vol. 2018, 100, 251–263. [Google Scholar] [CrossRef]
- Xu, J.; Chen, H.; Li, X.; Huang, Z.; Xu, H.; Yang, H.; Hu, J. Optimal Intensity Shock Wave Promotes the Adhesion and Migration of Rat Osteoblasts via Integrin Β1-Mediated Expression of Phosphorylated Focal Adhesion Kinase. J. Biol. Chem. 2012, 287, 26200–26212. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.-J.; Hsu, S.-L.; Weng, L.-H.; Sun, Y.-C.; Wang, F.-S. Extracorporeal Shockwave Therapy Shows a Number of Treatment Related Chondroprotective Effect in Osteoarthritis of the Knee in Rats. BMC Musculoskelet. Disord. 2013, 14, 44. [Google Scholar] [CrossRef]
- Chen, P.-Y.; Cheng, J.-H.; Wu, Z.-S.; Chuang, Y.-C. New Frontiers of Extracorporeal Shock Wave Medicine in Urology from Bench to Clinical Studies. Biomedicines 2022, 10, 675. [Google Scholar] [CrossRef]
- Fu, M.; Sun, C.-K.; Lin, Y.-C.; Wang, C.-J.; Wu, C.-J.; Ko, S.-F.; Chua, S.; Sheu, J.-J.; Chiang, C.-H.; Shao, P.-L.; et al. Extracorporeal Shock Wave Therapy Reverses Ischemia-Related Left Ventricular Dysfunction and Remodeling: Molecular-Cellular and Functional Assessment. PLoS ONE 2011, 6, e24342. [Google Scholar] [CrossRef]
- Dias dos Santos, P.R.; De Medeiros, V.P.; Freire Martins de Moura, J.P.; da Silveira Franciozi, C.E.; Nader, H.B.; Faloppa, F. Effects of Shock Wave Therapy on Glycosaminoglycan Expression during Bone Healing. Int. J. Surg. 2015, 24, 120–123. [Google Scholar] [CrossRef]
- Avendaño-Coy, J.; Comino-Suárez, N.; Grande-Muñoz, J.; Avendaño-López, C.; Gómez-Soriano, J. Extracorporeal Shockwave Therapy Improves Pain and Function in Subjects with Knee Osteoarthritis: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Int. J. Surg. 2020, 82, 64–75. [Google Scholar] [CrossRef] [PubMed]
- Ko, N.; Chang, C.; Cheng, C.; Yu, H.; Hu, G. Comparative Effectiveness of Focused Extracorporeal versus Radial Extracorporeal Shockwave Therapy for Knee Osteoarthritis-Randomized Controlled Study. Int. J. Environ. Res. Public Health 2022, 19, 9001. [Google Scholar] [CrossRef] [PubMed]
- Mueller, M.; Bockstahler, B.; Skalicky, M.; Mlacnik, E.; Lorinson, D. Effects of Radial Shockwave Therapy on the Limb Function of Dogs with Hip Osteoarthritis. Vet. Rec. 2007, 160, 762–765. [Google Scholar] [CrossRef] [PubMed]
- Altman, R.; Alarcón, G.; Appelrouth, D.; Bloch, D.; Borenstein, D.; Brandt, K.; Brown, C.; Cooke, T.D.; Daniel, W.; Feldman, D. The American College of Rheumatology Criteria for the Classification and Reporting of Osteoarthritis of the Hip. Arthritis Rheum. 1991, 34, 505–514. [Google Scholar] [CrossRef] [PubMed]
- Kellgren, J.H.; Lawrence, J.S. Radiological Assessment of Osteo-Arthrosis. Ann. Rheum. Dis. 1957, 16, 494–502. [Google Scholar] [CrossRef]
- Freyd, M. The Graphic Rating Scale. J. Educ. Psychol. 1923, 14, 83. [Google Scholar] [CrossRef]
- Bellamy, N.; Buchanan, W.W. Outcome Measurement in Osteoarthritis Clinical Trials: The Case for Standardisation. Clin. Rheumatol. 1984, 3, 293–303. [Google Scholar] [CrossRef]
- Tüzün, E.H.; Eker, L.; Aytar, A.; Daşkapan, A.; Bayramoğlu, M. Acceptability, Reliability, Validity and Responsiveness of the Turkish Version of WOMAC Osteoarthritis Index. Osteoarthr. Cartil. 2005, 13, 28–33. [Google Scholar] [CrossRef]
- Xie, X.; Zhu, J.; Zhang, H. Effects of Extracorporeal Shock Wave Therapy in Patients with Knee Osteoarthritis: A Cohort Study Protocol. Medicine 2020, 99, e21749. [Google Scholar] [CrossRef]
- Lee, S.; Lee, D.; Park, J. Effects of Extracorporeal Shockwave Therapy on Patients with Chronic Low Back Pain and Their Dynamic Balance Ability. J. Phys. Ther. Sci. 2014, 26, 7–10. [Google Scholar] [CrossRef]
- Zhao, Z.; Jing, R.; Shi, Z.; Zhao, B.; Ai, Q.; Xing, G. Efficacy of Extracorporeal Shockwave Therapy for Knee Osteoarthritis: A Randomized Controlled Trial. J. Surg. Res. 2013, 185, 661–666. [Google Scholar] [CrossRef]
- Chen, T.W.; Lin, C.W.; Lee, C.L.; Chen, C.H.; Chen, Y.J.; Lin, T.Y.; Huang, M.H. The Efficacy of Shock Wave Therapy in Patients with Knee Osteoarthritis and Popliteal Cyamella. Kaohsiung J. Med. Sci. 2014, 30, 362–370. [Google Scholar] [CrossRef] [PubMed]
- Imamura, M.; Alamino, S.; Hsing, W.T.; Alfieri, F.M.; Schmitz, C.; Battistella, L.R. Radial Extracorporeal Shock Wave Therapy for Disabling Pain Due to Severe Primary Knee Osteoarthritis. J. Rehabil. Med. 2017, 49, 54–62. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.; Gao, F.; Han, J.; Mao, T.; Sun, W.; Wang, B.; Guo, W.; Cheng, L.; Li, Z. Extracorporeal Shock Wave Treatment Can Normalize Painful Bone Marrow Edema in Knee Osteoarthritis. Medicine 2018, 97, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Zhong, Z.; Liu, B.; Liu, G.; Chen, J.; Li, Y.; Chen, J.; Liu, X.; Hu, Y. A Randomized Controlled Trial on the Effects of Low-Dose Extracorporeal Shockwave Therapy in Patients with Knee Osteoarthritis. Arch. Phys. Med. Rehabil. 2019, 100, 1695–1702. [Google Scholar] [CrossRef] [PubMed]
- Uysal, A.; Yildizgoren, M.T.; Guler, H.; Turhanoglu, A.D. Effects of Radial Extracorporeal Shock Wave Therapy on Clinical Variables and Isokinetic Performance in Patients with Knee Osteoarthritis: A Prospective, Randomized, Single-Blind and Controlled Trial. Int. Orthop. 2020, 44, 1311–1319. [Google Scholar] [CrossRef]
- Zhang, Y.F.; Liu, Y.; Chou, S.W.; Weng, H. Dose-Related Effects of Radial Extracorporeal Shock Wave Therapy for Knee Osteoarthritis: A Randomized Controlled Trial. J. Rehabil. Med. 2021, 53, 2742. [Google Scholar] [CrossRef]
- Ioppolo, F.; Saracino, F.; Rizzo, R.S.; Monacelli, G.; Lanni, D.; Di Sante, L.; Cacchio, A.; Santilli, V.; Venditto, T. Comparison between Extracorporeal Shock Wave Therapy and Intra-Articular Hyaluronic Acid Injections in the Treatment of First Carpometacarpal Joint Osteoarthritis. Ann. Rehabil. Med. 2018, 42, 92–100. [Google Scholar] [CrossRef]
| Focused ESWT (n = 51) | Radial ESWT (n = 49) | Sham ESWT (n = 48) | P1 | |
|---|---|---|---|---|
| Age (years) | 63.7 ± 5.9 (51.5–75.0) | 64.2 ± 6.8 (53.2–75.5) | 63.4 ± 6.0 (54.1–75.3) | 0.832 |
| Gender (F/M) | 33/18 | 33/16 | 32/16 | 0.959 |
| BMI (kg/m2) | 27.0 ± 1.7 (24.0–31.6) | 26.8 ± 1.9 (23.0–31.5) | 26.4 ± 2.7 (22.8–37.3) | 0.389 |
| Grade (II/III) | 22/29 | 26/23 | 28/20 | 0.306 |
| Pain duration (years) | 2.8 ± 1.6 (0.5–8.2) | 2.9 ± 1.7 (0.5–8.5) | 2.7 ± 1.5 (0.6–7.8) | 0.913 |
| VAS | Focused ESWT (n = 51) | Radial ESWT (n = 49) | Sham ESWT (n = 48) | P1 |
|---|---|---|---|---|
| (baseline) | 7.4 ± 1.9 (4–10) | 7.3 ± 1.9 (4–10) | 7.2 ± 1.9 (4–10) | 0.933 |
| (4th week ) | 5.3 ± 2.1 (1–9) | 6.3 ± 1.8 (3–10) | 7.3 ± 2.1 (2–10) | |
| (8th week) | 3.8 ± 1.9 (0–8) | 5.5 ± 1.8 (2–10) | 7.5 ± 1.9 (3–10) | |
| P2 (baseline vs. 4th week) | <0.001 | <0.001 | 0.828 | |
| P2 (baseline vs. 8th week) | <0.001 | <0.001 | 0.070 | |
| Change (baseline–4th week) | 2.0 ± 1.7 (−1–8) | 1.0 ± 1.1 (−2–3) | −0.0 ± 1.3 (−2–5) | 0.002 ‡ <0.001 †,§ |
| Change (baseline—8th week) | 3.6 ± 1.7 (0–8) | 1.8 ± 1.3 (−2–5) | −0.3 ± 1.1 (−3–2) | <0.001 ‡,†,§ |
| WOMAC Pain | Focused ESWT (n = 51) | Radial ESWT (n = 49) | Sham ESWT (n = 48) | P1 |
|---|---|---|---|---|
| (baseline) | 14.8 ± 4.1 (7–20) | 14.6 ± 3.8 (7–20) | 14.4 ± 4.0 (7–20) | 0.877 |
| (4th week) | 10.5 ± 4.0 (3–17) | 12.7 ± 3.3 (6–20) | 14.3 ± 4.3 (4–20) | |
| (8th week) | 7.5 ± 3.7 (1–15) | 11.4 ± 3.8 (3–20) | 15.0 ± 3.8 (7–20) | |
| P2 (baseline vs. 4th week) | <0.001 | <0.001 | 0.862 | |
| P2 (baseline vs. 8th week) | <0.001 | <0.001 | 0.021 | |
| Change (baseline–4th week) | 4.3 ± 3.3 (0–14) | 2.0 ± 1.7 (−2–6) | 0.1 ± 2.5 (−3–10) | <0.001 ‡,†,§ |
| Change (baseline–8th week) | 7.3 ± 3.5 (0–16) | 3.2 ± 2.5 (−3–10) | −0.6 ± 1.8 (−5–4) | <0.001 ‡,†,§ |
| WOMAC Stiffness | Focused ESWT (n = 51) | Radial ESWT (n = 49) | Sham ESWT (n = 48) | P1 |
|---|---|---|---|---|
| (baseline) | 5.4 ± 1.8 (2–8) | 5.6 ± 1.7 (2–8) | 5.3 ± 2.0 (2–8) | 0.754 |
| (4th week) | 3.9 ± 1.9 (1–8) | 4.7 ± 1.6 (2–8) | 5.4 ± 2.3 (1–9) | |
| (8th week) | 2.5 ± 1.6 (1–15) | 4.0 ± 1.7 (1–8) | 5.6 ± 2.0 (1–8) | |
| P2 (baseline vs. 4th week) | <0.001 | <0.001 | 0.513 | |
| P2 (baseline vs. 8th week) | <0.001 | <0.001 | 0.031 | |
| Change (baseline–4th week) | 1.5 ± 1.6 (−4–5) | 0.9 ± 1.0 (−2–3) | −0.1 ± 1.3 (−2–4) | 0.002 ‡ <0.001 †,§ |
| Change (baseline–8th week) | 2.9 ± 1.4 (0–7) | 1.6 ± 1.2 (−2–4) | −0.3 ± 1.0 (−3–2) | <0.001 ‡,†,§ |
| WOMAC Function | Focused ESWT (n = 51) | Radial ESWT (n = 49) | Sham ESWT (n = 48) | P1 |
|---|---|---|---|---|
| (baseline) | 48.7 ± 14.8 (19–68) | 48.4 ± 14.2 (23–68) | 48.0 ± 14.2 (23–68) | 0.972 |
| (4th week) | 36.0 ± 14.4 (12–66) | 43.1 ± 12.1 (22–62) | 46.5 ± 14.3 (14–66) | |
| (8th week) | 24.2 ± 11.6 (4–52) | 38.1 ± 12.4 (10–60) | 48.2 ± 14.6 (18–68) | |
| P2 (baseline vs. 4th week) | <0.001 | <0.001 | 0.190 | |
| P2 (baseline vs. 8th week) | <0.001 | <0.001 | 0.850 | |
| Change (baseline–4th week) | 12.7 ± 10.5 (−5–49) | 5.2 ± 4.3 (−3–15) | 1.5 ± 8.0 (−11–34) | <0.001 ‡,† <0.077 § |
| Change (baseline–8th week) | 24.5 ± 11.4 (1–44) | 10.2 ± 7.5 (−2–32) | −0.2 ± 6.1 (−13–21) | <0.001 ‡,†,§ |
| WOMAC Total | Focused ESWT (n = 51) | Radial ESWT (n = 49) | Sham ESWT (n = 48) | P1 |
|---|---|---|---|---|
| (baseline) | 68.9 ± 20.3 (31–96) | 68.7 ± 19.3 (34–96) | 67.7 ± 20.0 (33–96) | 0.949 |
| (4th week) | 50.5 ± 19.2 (18–84) | 60.5 ± 16.4 (33–85) | 66.5 ± 20.1 (19–94) | |
| (8th week) | 24.2 ± 11.6 (4–52) | 53.8 ± 17.8 (16–86) | 68.8 ± 20.3 (27–96) | |
| P2 (baseline vs. 4th week) | <0.001 | <0.001 | 0.448 | |
| P2 (baseline vs. 8th week) | <0.001 | <0.001 | 0.375 | |
| Change (baseline–4th week) | 18.5 ± 14.5 (−6–68) | 8.2 ± 5.9 (−5–20) | 1.3 ± 11.3 (−14–47) | <0.001 ‡,†,§ |
| Change (baseline–8th week) | 35.2 ± 15.8 (2–65) | 14.9 ± 10.8 (−5–45) | −1.1 ± 8.4 (−18–26) | <0.001 ‡,†,§ |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Şah, V. The Short-Term Efficacy of Large-Focused and Controlled-Unfocused (Radial) Extracorporeal Shock Wave Therapies in the Treatment of Hip Osteoarthritis. J. Pers. Med. 2023, 13, 48. https://doi.org/10.3390/jpm13010048
Şah V. The Short-Term Efficacy of Large-Focused and Controlled-Unfocused (Radial) Extracorporeal Shock Wave Therapies in the Treatment of Hip Osteoarthritis. Journal of Personalized Medicine. 2023; 13(1):48. https://doi.org/10.3390/jpm13010048
Chicago/Turabian StyleŞah, Volkan. 2023. "The Short-Term Efficacy of Large-Focused and Controlled-Unfocused (Radial) Extracorporeal Shock Wave Therapies in the Treatment of Hip Osteoarthritis" Journal of Personalized Medicine 13, no. 1: 48. https://doi.org/10.3390/jpm13010048
APA StyleŞah, V. (2023). The Short-Term Efficacy of Large-Focused and Controlled-Unfocused (Radial) Extracorporeal Shock Wave Therapies in the Treatment of Hip Osteoarthritis. Journal of Personalized Medicine, 13(1), 48. https://doi.org/10.3390/jpm13010048






