Alternatively Spliced Isoforms of MUC4 and ADAM12 as Biomarkers for Colorectal Cancer Metastasis
Abstract
1. Introduction
2. Materials and Methods
2.1. Cell Culture
2.2. RNA Extraction and cDNA Synthesis
2.3. Primer Design
2.4. Semi-Quantitative Endpoint PCR
2.5. Gel Extraction and Purification of Amplified PCR Products
2.6. Sanger Sequencing
2.7. Quantitative Real-Time PCR
2.8. RNA Sequencing
2.9. Western Blotting
2.10. Statistical Analysis
2.11. Survival Analysis
3. Results
3.1. Expression of ADAM12 and MUC4 in Human CRC
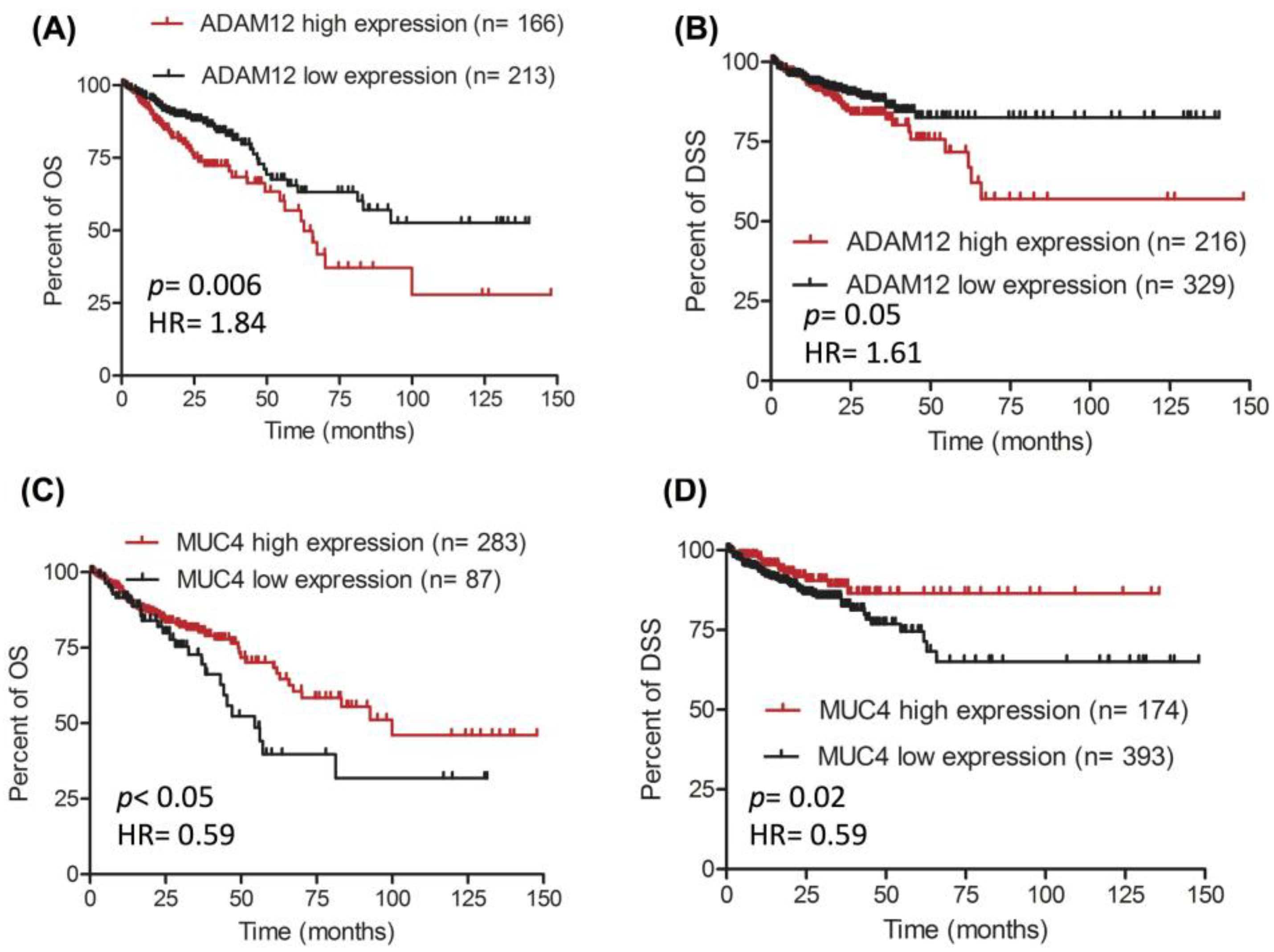
3.2. Potential of ADAM12 and MUC4 as Biomarkers in CRC
3.3. In Silico Identification of ADAM12 Isoforms
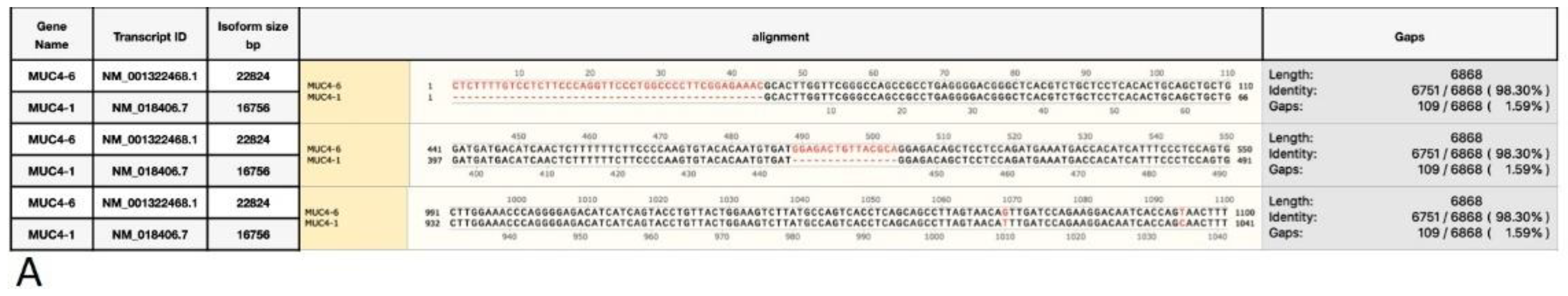
3.4. In Silico Identification of MUC4 Isoforms
3.5. Amplification of ADAM12 and MUC4 Isoforms
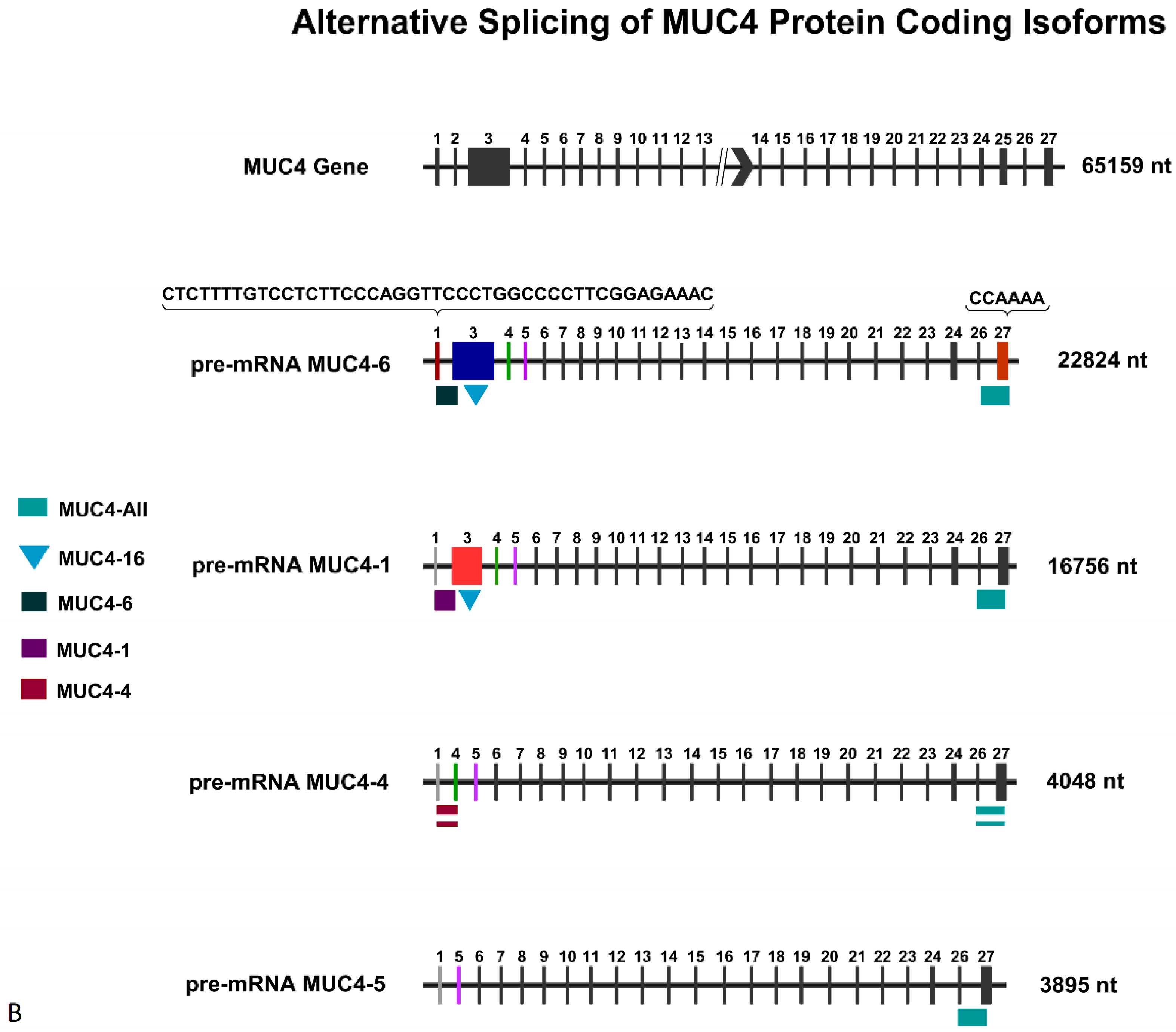
3.6. Quantitative Assessment of the Expression of ADAM12 and MUC4 Isoforms
3.7. Effect of 5-Fluorouracil on the Expression of ADAM12 and MUC4 Isoforms
3.8. RNA-Seq Isoform Analysis
3.9. Detection of ADAM12 and MUC4 Isoforms at the Protein Level
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Acknowledgments
Conflicts of Interest
References
- Raji, N.; Zadeh, T.M.; Babheidarian, P.; Houshmand, M. Detection of microsatellite instability by high-resolution melting analysis in colorectal cancer. Iran. Biomed. J. 2022, 26, 70–76. [Google Scholar] [PubMed]
- Alsanea, N.; Abduljabbar, A.S.; Alhomoud, S.; Ashari, L.H.; Hibbert, D.; Bazarbashi, S. Colorectal cancer in Saudi Arabia: Incidence, survival, demographics and implications for national policies. Ann. Saudi Med. 2015, 35, 196–202. [Google Scholar] [CrossRef] [PubMed]
- Armaghany, T.; Wilson, J.D.; Chu, Q.; Mills, G. Genetic alterations in colorectal cancer. Gastrointest. Cancer Res. 2012, 5, 19–27. [Google Scholar] [PubMed]
- Haggar, F.A.; Boushey, R.P. Colorectal cancer epidemiology: Incidence, mortality, survival, and risk factors. Clin. Colon Rectal Surg. 2009, 22, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Strum, W.B. Colorectal Adenomas. N. Engl. J. Med. 2016, 375, 389–390. [Google Scholar] [CrossRef]
- Sawicki, T.; Ruszkowska, M.; Danielewicz, A.; Niedźwiedzka, E.; Arłukowicz, T.; Przybyłowicz, K.E. A review of colorectal cancer in terms of epidemiology, risk factors, development, symptoms and diagnosis. Cancers 2021, 13, 2025. [Google Scholar] [CrossRef]
- Pino, M.S.; Chung, D.C. The chromosomal instability pathway in colon cancer. Gastroenterology 2010, 138, 2059–2072. [Google Scholar] [CrossRef]
- Vaughn, C.P.; ZoBell, S.D.; Furtado, L.V.; Baker, C.L.; Samowitz, W.S. Frequency of KRAS, BRAF, and NRAS mutations in colorectal cancer. Genes Chromosome Cancer 2011, 50, 307–312. [Google Scholar] [CrossRef]
- Müller, M.F.; Ibrahim, A.E.K.; Arends, M.J. Molecular pathological classification of colorectal cancer. Virchows Arch. 2016, 469, 129–134. [Google Scholar] [CrossRef]
- Aziz, M.A.; Yousef, Z.; Saleh, A.M.; Mohammad, S.; Al Knawy, B. Towards personalized medicine of colorectal cancer. Crit. Rev. Oncol. Hematol. 2017, 118, 70–78. [Google Scholar] [CrossRef]
- Alhumaid, A.; Alyousef, Z.; Bakhsh, H.A.; Alghamdi, S.; Aziz, M.A. Emerging paradigms in the treatment of liver metastases in colorectal cancer. Crit. Rev. Oncol. Hematol. 2018, 132, 39–50. [Google Scholar] [CrossRef]
- Bonnal, S.C.; López-Oreja, I.; Valcárcel, J. Roles and mechanisms of alternative splicing in cancer—Implications for care. Nat. Rev. Clin. Oncol. 2020, 17, 457–474. [Google Scholar] [CrossRef]
- Lander, E.S.; Linton, L.M.; Birren, B. Initial sequencing and analysis of the human genome. Nature 2001, 409, 860–921. [Google Scholar]
- Tazi, J.; Bakkour, N.; Stamm, S. Alternative splicing and disease. Biochim. Biophys. Acta 2009, 1792, 14–26. [Google Scholar] [CrossRef]
- Hagen, R.M.; Ladomery, M.R. Role of splice variants in the metastatic progression of prostate cancer. Biochem. Soc. Trans. 2012, 40, 870–874. [Google Scholar] [CrossRef]
- Chen, Y.; Huang, M.; Liu, X. Alternative splicing of mRNA in colorectal cancer: New strategies for tumor diagnosis and treatment. Cell Death Dis. 2021, 12, 752. [Google Scholar] [CrossRef]
- Yang, Q.; Zhao, J.; Zhang, W.; Chen, D.; Wang, Y. Aberrant alternative splicing in breast cancer. J. Mol. Cell Biol. 2019, 11, 920–929. [Google Scholar] [CrossRef]
- Ye, Z.; Bing, A.; Zhao, S. Comprehensive analysis of spliceosome genes and their mutants across 27 cancer types in 9070 patients: Clinically relevant outcomes in the context of 3P medicine. EPMA J. 2022, 13, 335–350. [Google Scholar] [CrossRef]
- Golubnitschaja, O.; Baban, B.; Boniolo, G. Medicine in the early twenty-first century: Paradigm and anticipation—EPMA position paper 2016. EPMA J. 2016, 7, 23. [Google Scholar] [CrossRef]
- Mardis, E.R. The emergence of cancer genomics in diagnosis and precision medicine. Nat. Cancer 2021, 2, 1263–1264. [Google Scholar] [CrossRef]
- Supplitt, S.; Karpinski, P.; Sasiadek, M.; Laczmanska, I. Current Achievements and Applications of Transcriptomics in Personalized Cancer Medicine. Int. J. Mol. Sci. 2021, 22, 1422. [Google Scholar] [CrossRef] [PubMed]
- Kwon, Y.W.; Jo, H.S.; Bae, S.; Seo, Y.; Song, P.; Song, M.; Yoon, J.H. Application of proteomics in cancer: Recent trends and approaches for biomarkers discovery. Front. Med. 2021, 8. [Google Scholar] [CrossRef] [PubMed]
- Santos, G.C.; Saldanha-Gama, R.; Brito, N.M.D.; Renovato-Martins, M.; Barja-Fidalgo, C. Metabolomics in cancer and cancer-associated inflammatory cells. J. Cancer Metastasis Treat. 2021, 7, 1. [Google Scholar] [CrossRef]
- Cheng, T.; Zhan, X. Pattern recognition for predictive, preventive, and personalized medicine in cancer. EPMA J. 2017, 8, 51–60. [Google Scholar] [CrossRef] [PubMed]
- Yoo, B.C.; Kim, K.H.; Woo, S.M.; Myung, J.K. Clinical multi-omics strategies for the effective cancer management. J. Proteom. 2018, 188, 97–106. [Google Scholar] [CrossRef]
- Lu, M.; Zhan, X. The crucial role of multiomic approach in cancer research and clinically relevant outcomes. EPMA J. 2018, 9, 77–102. [Google Scholar] [CrossRef]
- Aziz, M.A.; Periyasamy, S.; Al Yousef, Z.; AlAbdulkarim, I.; Al Otaibi, M.; Alfahed, A.; Alasiri, G. Integrated exon level expression analysis of driver genes explain their role in colorectal cancer. PLoS ONE 2014, 9, e110134. [Google Scholar] [CrossRef]
- Eldai, H.; Periyasamy, S.; Al Qarni, S.; Al Rodayyan, M.; Muhammed Mustafa, S.; Deeb, A.; Al Sheikh, E.; Afzal Khan, M.; Johani, M.; Yousef, Z.; et al. Novel genes associated with colorectal cancer are revealed by high resolution cytogenetic analysis in a patient specific manner. PLoS ONE 2013, 8, e76251. [Google Scholar] [CrossRef]
- Nilsen, T.W.; Graveley, B.R. Expansion of the eukaryotic proteome by alternative splicing. Nature 2010, 463, 457–463. [Google Scholar] [CrossRef]
- Pan, Q.; Shai, O.; Lee, L.J.; Frey, B.J.; Blencowe, B.J. Deep surveying of alternative splicing complexity in the human transcriptome by high-throughput sequencing. Nat. Genet. 2008, 40, 1413–1415. [Google Scholar] [CrossRef]
- Wang, E.T.; Sandberg, R.; Luo, S.; Khrebtukova, I.; Zhang, L.; Mayr, C.; Kingsmore, S.F.; Schroth, G.P.; Burge, C.B. Alternative isoform regulation in human tissue transcriptomes. Nature 2008, 456, 470–476. [Google Scholar] [CrossRef]
- Nyren-Erickson, E.K.; Jones, J.M.; Srivastava, D.; Mallik, S. A disintegrin and metalloproteinase-12 (ADAM12): Function, roles in disease progression, and clinical implications. Biochim. Biophys. Acta Gen. Subj. 2013, 1830, 4445–4455. [Google Scholar] [CrossRef]
- Du, S.; Sun, L.; Wang, Y.; Zhu, W.; Gao, J.; Pei, W.; Zhang, Y. ADAM12 is an independent predictor of poor prognosis in liver cancer. Sci. Rep. 2022, 12, 1–15. [Google Scholar] [CrossRef]
- Zhu, H.; Jiang, W.; Zhu, H.; Hu, J.; Tang, B.; Zhou, Z.; He, X. Elevation of ADAM12 facilitates tumor progression by enhancing metastasis and immune infiltration in gastric cancer. Int. J. Oncol. 2022, 60, 1–13. [Google Scholar] [CrossRef]
- Munkley, J.; Livermore, K.; Rajan, P.; Elliott, D.J. RNA splicing and splicing regulator changes in prostate cancer pathology. Hum. Genet. 2017, 136, 1143–1154. [Google Scholar] [CrossRef]
- Le, K.Q.; Prabhakar, B.S.; Hong, W.J.; Li, L.C. Alternative splicing as a biomarker and potential target for drug discovery. Acta Pharmacol. Sin. 2015, 36, 1212–1218. [Google Scholar] [CrossRef]
- Gardina, P.J.; Clark, T.A.; Shimada, B.; Staples, M.K.; Yang, Q.; Veitch, J.; Schweitzer, A.; Awad, T.; Sugnet, C.; Dee, S.; et al. Alternative splicing and differential gene expression in colon cancer detected by a whole genome exon array. BMC Genom. 2006, 7, 325. [Google Scholar] [CrossRef]
- Tripathi, V.; Shin, J.H.; Stuelten, C.H. TGF-β-induced alternative splicing of TAK1 promotes EMT and drug resistance. Oncogene 2019, 38, 3185–3200. [Google Scholar] [CrossRef]
- Oltean, S.; Bates, D.O. Hallmarks of alternative splicing in cancer. Oncogene 2014, 33, 5311–5318. [Google Scholar] [CrossRef]
- Martinez-Montiel, N.; Rosas-Murrieta, N.H.; Ruiz, M.A.; Monjaraz-Guzman, E.; Martinez-Contreras, R. Alternative Splicing as a Target for Cancer Treatment. Int. J. Mol. Sci. 2018, 19, 545. [Google Scholar] [CrossRef]
- Lefave, C.V.; Squatrito, M.; Vorlova, S.; Rocco, G.L.; Brennan, C.W.; Holland, E.C.; Pan, Y.X.; Cartegni, L. Splicing factor hnRNPH drives an oncogenic splicing switch in gliomas. EMBO J. 2011, 30, 4084–4097. [Google Scholar] [CrossRef] [PubMed]
- Xiong, Y.; Deng, Y.; Wang, K.; Zhou, H.; Zheng, X.; Si, L.; Fu, Z. Profiles of alternative splicing in colorectal cancer and their clinical significance: A study based on large-scale sequencing data. EBioMedicine 2018, 36, 183–195. [Google Scholar] [CrossRef] [PubMed]
- Venables, J.P.; Klinck, R.; Bramard, A.; Inkel, L.; Dufresne-Martin, G.; Koh, C.; Gervais-Bird, J.; Lapointe, E.; Froehlich, U.; Durand, M. Identification of alternative splicing markers for breast cancer. Cancer Res. 2008, 68, 9525–9531. [Google Scholar] [CrossRef] [PubMed]
- Thorsen, K.; Sorensen, K.D.; Brems-Eskildsen, A.S.; Modin, C.; Gaustadnes, M.; Hein, A.M.; Kruhoffer, M.; Laurberg, S.; Borre, M.; Wang, K. Alternative splicing in colon, bladder, and prostate cancer identified by exon array analysis. Mol. Cell. Proteom. 2008, 7, 1214–1224. [Google Scholar] [CrossRef] [PubMed]
- Yi, Q.; Tang, L. Alternative spliced variants as biomarkers of colorectal cancer. Curr. Drug Metab. 2011, 12, 966–974. [Google Scholar] [CrossRef]
- Huang, X.; Liu, J.; Mo, X.; Liu, H.; Wei, C.; Huang, L.; Chen, J.; Tian, C.; Meng, Y.; Wu, G. Systematic profiling of alternative splicing events and splicing factors in left- and right-sided colon cancer. Aging 2019, 11, 8270–8293. [Google Scholar] [CrossRef]
- Buxbaum, J.D.; Liu, K.N.; Luo, Y.; Slack, J.L.; Stocking, K.L.; Peschon, J.J.; Johnson, R.S.; Castner, B.J.; Cerretti, D.P.; Black, R.A. Evidence that tumor necrosis factor alpha converting enzyme is involved in regulated alpha-secretase cleavage of the Alzheimer amyloid protein precursor. J. Biol. Chem. 1998, 273, 27765–27767. [Google Scholar] [CrossRef]
- Aziz, M.A.; AlOtaibi, M.; AlAbdulrahman, A.; AlDrees, M.; AlAbdulkarim, I. Mucin Family Genes are Downregulated in Colorectal Cancer Patients. J. Carcinog. Mutagen. 2014, S10, 009. Available online: https://www.readcube.com/articles/10.4172%2F2157-2518.s10-009 (accessed on 20 December 2022). [CrossRef]




| Gene Isoform | Transcript ID | Primer Sequence | Amplicon Size (bp) |
|---|---|---|---|
| ADAM12- All | F-GTAGCTGTCAAATGGCG R-CCACAAATCTGTTCCCAC | 198 bp | |
| ADAM12-1 | ENST00000368679.4 * NM_003474.6 ** | F-CCAACTCGTATAGCATGCATC | 197 bp |
| ADAM12-3 | ENST00000448723.1 * NM_001288973.2 ** | R-CAATGCCCACGTAATGCAC | |
| ADAM12-2 | ENST00000368676.4 * NM_021641.5 ** | F-CTGCTCCTGAGAGAGTAGC | |
| ADAM12-4 | NM_001288974.2 ** | 205 bp | |
| ADAM12-5 | NM_001288975.2 ** | R-CAGAGCATTAAGTTGCAGCC | |
| ADAM12-4 | NM_001288974.2 ** | F-GAAAGAAGCAAGGCAGGA R-CGTTTCCATGACAACAGAC | 231 bp |
| GAPDH | ENSG00000111640 * NG_007073.2 ** | F-ACCCAGAAGACTGTG R-CAGTGAGCTTCCCGTTCAG | 139 bp |
| ACTNB | ENSG00000075624 * NG_007992.1 ** | F-TGACGTGGACATCCGCAAAG R-CTGGAAGGTGGACAGCGAGG | 205 bp |
| Transcript ID | SW620 | SW480 | Fold Change |
|---|---|---|---|
| (SW480/SW620) | |||
| ADAM12_ENSG00000148848.10 | 0.0245429 | 0.0241492 | 0.983958701 |
| ADAM12_ENST00000368679.4 | 0.00916641 | 0.000339521 | 0.037039692 |
| ADAM12_ENST00000368676.4 | 0.0273946 | 0.0424578 | 1.549860191 |
| ADAM12_ENST00000467145.1 | 0 | 5.45E-05 | |
| ADAM12_ENST00000482291.1 | 0.0861337 | 9.29E-05 | 0.001079091 |
| ADAM12_ENST00000485388.2 | 0.010143 | 0 | 0 |
| ADAM12_ENST00000448723.1 | 0.0269748 | 0.00363765 | 0.134853641 |
| ADAM12_ENST00000494661.1 | 0 | 1.44E-18 | |
| MUC4_ENST00000415455.1 | 4.40E-06 | 4.54E-10 | 1.03E-04 |
| MUC4_ENST00000308466.8 | 7.57E-09 | 1.71E-12 | 2.26E-04 |
| MUC4_ENST00000392407.2 | 0.112782 | 0.0177344 | 1.57E-01 |
| MUC4_ENST00000339251.5 | 8.73E-06 | 0.0596096 | 6.83E+03 |
| MUC4_ENST00000448861.1 | 0.00120339 | 0.00127307 | 1.06E+00 |
| MUC4_ENST00000349607.4 | 2.30E-07 | 4.93E-13 | 2.14E-06 |
| MUC4_ENST00000346145.4 | 6.92E-12 | 2.68E-07 | 3.87E+04 |
| MUC4_ENST00000478156.1 | 1.28E-91 | 1.11E-25 | 8.67E+65 |
| MUC4_ENSG00000145113.17 | 0.0510692 | 0.0332947 | 6.52E-01 |
| MUC4_ENST00000463781.3 | 1.02E-66 | 5.30E-23 | 5.20E+43 |
| MUC4_ENST00000479406.1 | 2.42E-93 | 6.33E-30 | 2.62E+63 |
| MUC4_ENST00000462323.1 | 3.35E-94 | 2.96E-32 | 8.84E+61 |
| MUC4_ENST00000475231.1 | 9.90E-95 | 1.02E-32 | 1.03E+62 |
| MUC4_ENST00000470451.1 | 5.26E-94 | 4.40E-32 | 8.37E+61 |
| MUC4_ENST00000480843.1 | 1.55E-94 | 1.51E-32 | 9.74E+61 |
| MUC4_ENST00000477086.1 | 3.49E-90 | 2.11E-30 | 6.05E+59 |
| MUC4_ENST00000466475.1 | 8.35E-91 | 6.02E-31 | 7.21E+59 |
| MUC4_ENST00000477756.1 | 1.63E-90 | 1.08E-30 | 6.63E+59 |
| MUC4_ENST00000464234.1 | 1.63E-56 | 1.69E-12 | 1.04E+44 |
| MUC4_ENST00000467235.1 | 0.0118175 | 0.0397415 | 3.36E+00 |
| MUC4_ENST00000469992.1 | 2.94E-76 | 0.153917 | 5.24E+74 |
| MUC4_ENST00000486425.1 | 2.02E-234 | 6.08E-94 | 3.01E+140 |
| MUC4_ENST00000478685.1 | 2.08E-76 | 0.11691 | 5.62E+74 |
| Gene | SW620 | SW480 | Fold Change (SW480/SW620) |
|---|---|---|---|
| SF3B1 | 287.3 | 242.6 | 1.18 |
| U2Af1 | 91.08 | 109.47 | 0.83 |
| U2AF1L4 | 1.228 | 2.64 | 0.47 |
| SRSF2 | 225.8 | 200.5 | 1.12 |
| RBM10 | 124.05 | 89.05 | 1.39 |
| FUBP1 | 157.3 | 104.5 | 1.5 |
| SRPK1 | 123.48 | 118.4 | 1.04 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Althenayyan, S.; AlMuhanna, M.H.; AlAbdulrahman, A.; Alghanem, B.; Alsagaby, S.A.; Alfahed, A.; Alasiri, G.; Aziz, M.A. Alternatively Spliced Isoforms of MUC4 and ADAM12 as Biomarkers for Colorectal Cancer Metastasis. J. Pers. Med. 2023, 13, 135. https://doi.org/10.3390/jpm13010135
Althenayyan S, AlMuhanna MH, AlAbdulrahman A, Alghanem B, Alsagaby SA, Alfahed A, Alasiri G, Aziz MA. Alternatively Spliced Isoforms of MUC4 and ADAM12 as Biomarkers for Colorectal Cancer Metastasis. Journal of Personalized Medicine. 2023; 13(1):135. https://doi.org/10.3390/jpm13010135
Chicago/Turabian StyleAlthenayyan, Saleh, Mohammed H. AlMuhanna, Abdulkareem AlAbdulrahman, Bandar Alghanem, Suliman A. Alsagaby, Abdulaziz Alfahed, Glowi Alasiri, and Mohammad Azhar Aziz. 2023. "Alternatively Spliced Isoforms of MUC4 and ADAM12 as Biomarkers for Colorectal Cancer Metastasis" Journal of Personalized Medicine 13, no. 1: 135. https://doi.org/10.3390/jpm13010135
APA StyleAlthenayyan, S., AlMuhanna, M. H., AlAbdulrahman, A., Alghanem, B., Alsagaby, S. A., Alfahed, A., Alasiri, G., & Aziz, M. A. (2023). Alternatively Spliced Isoforms of MUC4 and ADAM12 as Biomarkers for Colorectal Cancer Metastasis. Journal of Personalized Medicine, 13(1), 135. https://doi.org/10.3390/jpm13010135







