Effectiveness of Cement Augmentation on Early Postoperative Mobility in Patients Treated for Trochanteric Fractures with Cephalomedullary Nailing: A Prospective Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
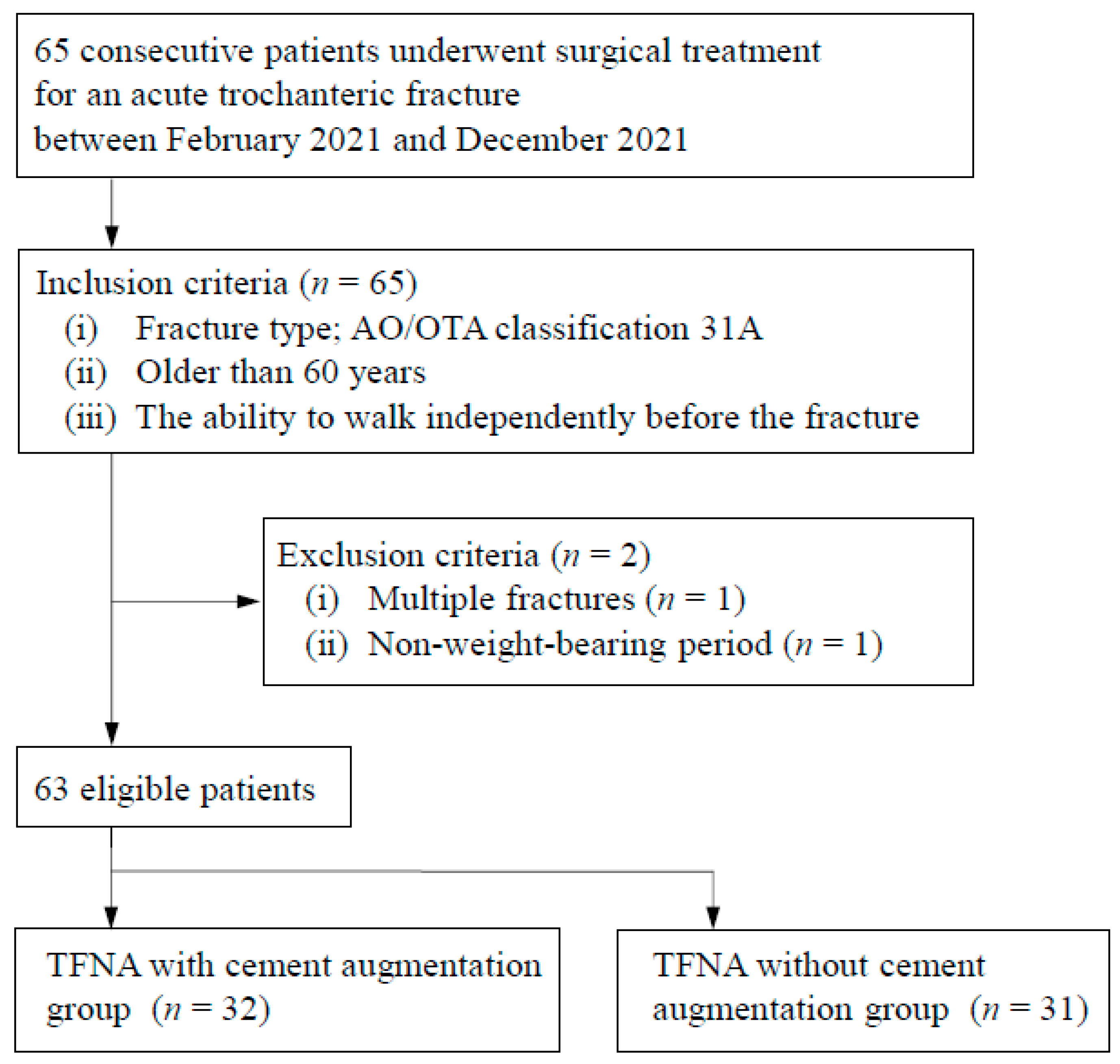
2.2. Patient Selection
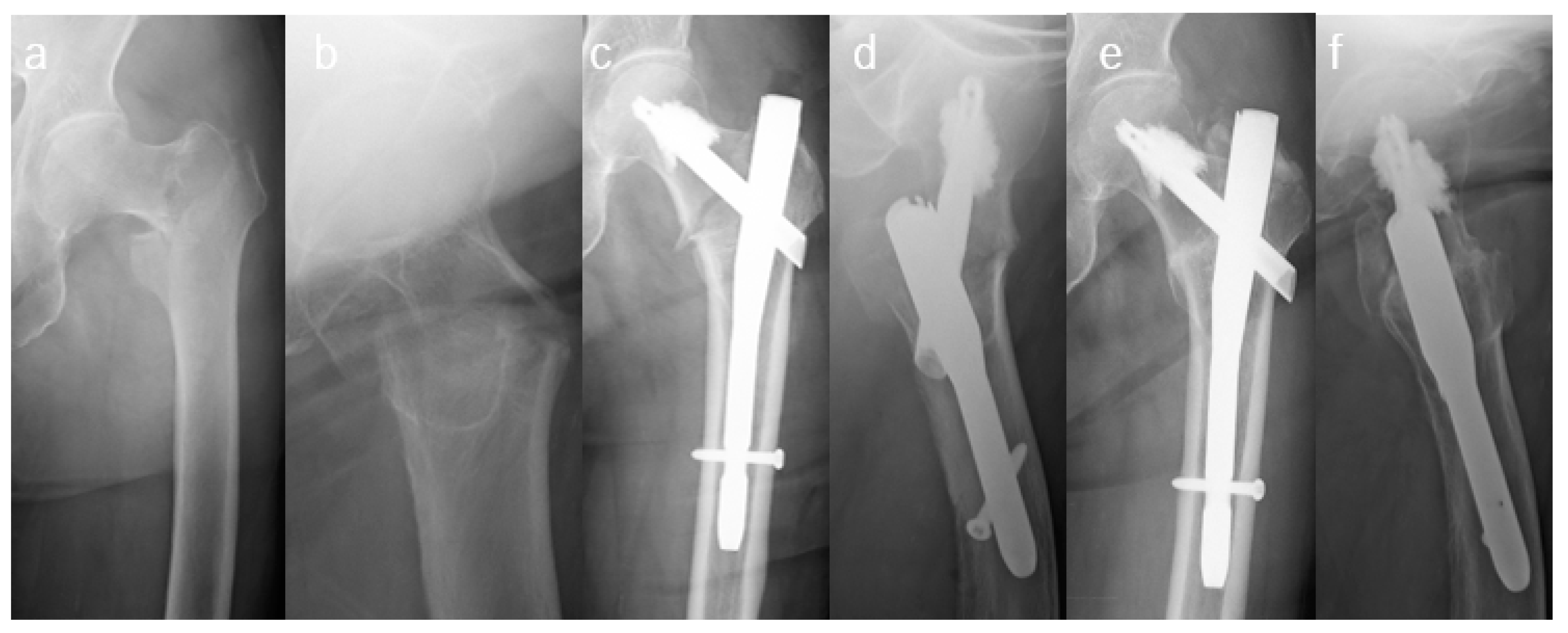
2.3. Surgical Procedures and Rehabilitation Plan
2.4. Main Exposure
2.5. Outcomes
2.6. Preoperative Variables
2.7. Postoperative Variables
2.8. Statistical Analyses
3. Results
4. Discussion
4.1. Strengths
4.2. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chen, I.J.; Chiang, C.Y.; Li, Y.H.; Chang, C.H.; Hu, C.C.; Chen, D.W.; Chang, Y.; Yang, W.E.; Shih, H.N.; Ueng, S.W.; et al. Nationwide Cohort Study of Hip Fractures: Time Trends in the Incidence Rates and Projections up to 2035. Osteoporos. Int. 2015, 26, 681–688. [Google Scholar] [CrossRef] [PubMed]
- Dhanwal, D.K.; Dennison, E.M.; Harvey, N.C.; Cooper, C. Epidemiology of Hip Fracture: Worldwide Geographic Variation. Indian J. Orthop. 2011, 45, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Turgut, A.; Kalenderer, Ö.; Karapınar, L.; Kumbaracı, M.; Akkan, H.A.; Ağuş, H. Which Factor Is Most Important for Occurrence of Cutout Complications in Patients Treated With Proximal Femoral Nail Antirotation? Retrospective Analysis of 298 Patients. Arch. Orthop. Trauma Surg. 2016, 136, 623–630. [Google Scholar] [CrossRef] [PubMed]
- Pascarella, R.; Fantasia, R.; Maresca, A.; Bettuzzi, C.; Amendola, L.; Violini, S.; Cuoghi, F.; Sangiovanni, P.; Cerbasi, S.; Boriani, S.; et al. How Evolution of the Nailing System Improves Results and Reduces Orthopedic Complications: More Than 2000 Cases of Trochanteric Fractures Treated With the Gamma Nail System. Musculoskelet. Surg. 2016, 100, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Heini, P.F.; Franz, T.; Fankhauser, C.; Gasser, B.; Ganz, R. Femoroplasty-Augmentation of Mechanical Properties in the Osteoporotic Proximal Femur: A Biomechanical Investigation of PMMA Reinforcement in Cadaver Bones. Clin. Biomech. 2004, 19, 506–512. [Google Scholar] [CrossRef] [PubMed]
- Stoffel, K.K.; Leys, T.; Damen, N.; Nicholls, R.L.; Kuster, M.S. A New Technique for Cement Augmentation of the Sliding Hip Screw in Proximal Femur Fractures. Clin. Biomech. 2008, 23, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Yee, D.K.H.; Lau, W.; Tiu, K.L.; Leung, F.; Fang, E.; Pineda, J.P.S.; Fang, C. Cementation: For Better or Worse? Interim Results of a Multi-centre Cohort Study Using a Fenestrated Spiral Blade Cephalomedullary Device for Pertrochanteric Fractures in the Elderly. Arch. Orthop. Trauma Surg. 2020, 140, 1957–1964. [Google Scholar] [CrossRef]
- Goodnough, L.H.; Wadhwa, H.; Tigchelaar, S.S.; DeBaun, M.R.; Chen, M.J.; Bishop, J.A.; Gardner, M.J. Trochanteric Fixation Nail Advanced With Helical Blade and Cement Augmentation: Early Experience With a Retrospective Cohort. Eur. J. Orthop. Surg. Traumatol. 2021, 31, 259–264. [Google Scholar] [CrossRef]
- Kammerlander, C.; Hem, E.S.; Klopfer, T.; Gebhard, F.; Sermon, A.; Dietrich, M.; Bach, O.; Weil, Y.; Babst, R.; Blauth, M. Cement Augmentation of the Proximal Femoral Nail Antirotation (PFNA)-a Multicentre Randomized Controlled Trial. Injury 2018, 49, 1436–1444. [Google Scholar] [CrossRef]
- Yamamoto, N.; Ogawa, T.; Banno, M.; Watanabe, J.; Noda, T.; Schermann, H.; Ozaki, T. Cement Augmentation of Internal Fixation for Trochanteric Fracture: A Systematic Review and Meta-analysis. Eur. J. Trauma Emerg. Surg. 2022, 48, 1699–1709. [Google Scholar] [CrossRef]
- Kristensen, M.T.; Öztürk, B.; Röck, N.D.; Ingeman, A.; Palm, H.; Pedersen, A.B. Regaining Pre-fracture Basic Mobility Status After Hip Fracture and Association With Post-discharge Mortality and Readmission—A Nationwide Register Study in Denmark. Age Ageing 2019, 48, 278–284. [Google Scholar] [CrossRef] [PubMed]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef] [PubMed]
- Mochizuki, Y.; Yamamoto, N.; Fujii, T.; Noda, T.; Ozaki, T. Effect of Cement Augmentation on Early Postoperative ADL Score in Patients Treated with Cephalomedullary Nailing for Trochanteric Fractures. Available online: https://www.protocols.io/view/effect-of-cement-augmentation-on-early-postoperati-btmbnk2n (accessed on 27 June 2022).
- Meinberg, E.G.; Agel, J.; Roberts, C.S.; Karam, M.D.; Kellam, J.F. Fracture and Dislocation Classification Compendium-2018. J. Orthop. Trauma 2018, 32 (Suppl. S1), S1–S170. [Google Scholar] [CrossRef]
- Chang, S.M.; Zhang, Y.Q.; Ma, Z.; Li, Q.; Dargel, J.; Eysel, P. Fracture Reduction With Positive Medial Cortical Support: A Key Element in Stability Reconstruction for the Unstable Pertrochanteric Hip Fractures. Arch. Orthop. Trauma Surg. 2015, 135, 811–818. [Google Scholar] [CrossRef] [PubMed]
- Foss, N.B.; Kristensen, M.T.; Kehlet, H. Prediction of Postoperative Morbidity, Mortality and Rehabilitation in Hip Fracture Patients: The Cumulated Ambulation Score. Clin. Rehabil. 2006, 20, 701–708. [Google Scholar] [CrossRef]
- Aagesen, M.; Kristensen, M.T.; Vinther, A. The Cumulated Ambulation Score Is Superior to the New Mobility Score and the de Morton Mobility Index in Predicting Discharge Destination of Patients Admitted to an Acute Geriatric Ward; a 1-Year Cohort Study of 491 Patients. Disabil. Rehabil. 2022, 44, 1481–1488. [Google Scholar] [CrossRef] [PubMed]
- Hulsbæk, S.; Larsen, R.F.; Rosthøj, S.; Kristensen, M.T. The Barthel Index and the Cumulated Ambulation Score Are Superior to the de Morton Mobility Index for the Early Assessment of Outcome in Patients With a Hip Fracture Admitted to an Acute Geriatric Ward. Disabil. Rehabil. 2019, 41, 1351–1359. [Google Scholar] [CrossRef] [PubMed]
- Sink, E.L.; Leunig, M.; Zaltz, I.; Gilbert, J.C.; Clohisy, J.; Academic Network for Conservational Hip Outcomes Research Group. Reliability of a Complication Classification System for Orthopaedic Surgery. Clin. Orthop. Relat. Res. 2012, 470, 2220–2226. [Google Scholar] [CrossRef] [PubMed]
- Inouye, S.K.; van Dyck, C.H.; Alessi, C.A.; Balkin, S.; Siegal, A.P.; Horwitz, R.I. Clarifying Confusion: The Confusion Assessment Method. A New Method for Detection of Delirium. Ann. Intern. Med. 1990, 113, 941–948. [Google Scholar] [CrossRef] [PubMed]
- Quan, H.; Li, B.; Couris, C.M.; Fushimi, K.; Graham, P.; Hider, P.; Januel, J.M.; Sundararajan, V. Updating and Validating the Charlson Comorbidity Index and Score for Risk Adjustment in Hospital Discharge Abstracts Using Data From 6 Countries. Am. J. Epidemiol. 2011, 173, 676–682. [Google Scholar] [CrossRef] [Green Version]
- Tomita, Y.; Yamamoto, N.; Inoue, T.; Noda, T.; Kawasaki, K.; Ozaki, T. Clinical Prediction Model for Postoperative Ambulatory Ability Outcomes in Patients With Trochanteric Fractures. Injury 2021, 52, 1826–1832. [Google Scholar] [CrossRef] [PubMed]
- Baumgaertner, M.R.; Curtin, S.L.; Lindskog, D.M.; Keggi, J.M. The Value of the Tip-Apex Distance in Predicting Failure of Fixation of Peritrochanteric Fractures of the Hip. J. Bone Jt. Surg. Am. 1995, 77, 1058–1064. [Google Scholar] [CrossRef] [PubMed]
- Ito, J.; Takakubo, Y.; Sasaki, K.; Sasaki, J.; Owashi, K.; Takagi, M. Prevention of Excessive Postoperative Sliding of the Short Femoral Nail in Femoral Trochanteric Fractures. Arch. Orthop. Trauma Surg. 2015, 135, 651–657. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, N.; Tamura, R.; Inoue, T.; Noda, T.; Nagano, H.; Ozaki, T. Radiological Findings and Outcomes of Anterior Wall Fractures in Pertrochanteric Fractures. J. Orthop. Sci. 2021, 26, 247–253. [Google Scholar] [CrossRef] [PubMed]
- Cleveland, M.; Bosworth, D.M.; Thompson, F.R.; Wilson, H.J., Jr.; Ishizuka, T. A Ten-Year Analysis of Intertrochanteric Fractures of the Femur. J. Bone Jt. Surg. Am. 1959, 41–A, 1399–1408. [Google Scholar] [CrossRef]
- Ogawa, T.; Aoki, T.; Shirasawa, S. Effect of Hip Fracture Surgery Within 24 Hours on Short-Term Mobility. J. Orthop. Sci. 2019, 24, 469–473. [Google Scholar] [CrossRef]
- Kulachote, N.; Sa-Ngasoongsong, P.; Sirisreetreerux, N.; Chulsomlee, K.; Thamyongkit, S.; Wongsak, S. Predicting Factors for Return to Prefracture Ambulatory Level in High Surgical Risk Elderly Patients Sustained Intertrochanteric Fracture and Treated with Proximal Femoral Nail Antirotation (PFNA) with and Without Cement Augmentation. Geriatr. Orthop. Surg. Rehabil. 2020, 11, 2151459320912121. [Google Scholar] [CrossRef]
- Keppler, A.M.; Pfeufer, D.; Kau, F.; Linhart, C.; Zeckey, C.; Neuerburg, C.; Böcker, W.; Kammerlander, C. Cement Augmentation of the Proximal Femur Nail Antirotation (PFNA) Is Associated With Enhanced Weight-Bearing in Older Adults. Injury 2021, 52, 3042–3046. [Google Scholar] [CrossRef]
- Dall’Oca, C.; Maluta, T.; Moscolo, A.; Lavini, F.; Bartolozzi, P. Cement Augmentation of Intertrochanteric Fractures Stabilised With Intramedullary Nailing. Injury 2010, 41, 1150–1155. [Google Scholar] [CrossRef]
- Kim, S.J.; Park, H.S.; Lee, D.W.; Lee, J.W. Is Calcium Phosphate Augmentation a Viable Option for Osteoporotic Hip Fractures? Osteoporos. Int. 2018, 29, 2021–2028. [Google Scholar] [CrossRef]
- Mitsuzawa, S.; Matsuda, S. Cement Distribution and Initial Fixability of Trochanteric Fixation Nail Advanced (TFNA) Helical Blades. Injury 2022, 53, 1184–1189. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Zhang, K.; Jia, Y.; Yu, B.; Feng, W. InterTan Nail Versus Proximal Femoral Nail Antirotation-Asia in the Treatment of Unstable Trochanteric Fractures. Orthopedics 2013, 36, e288–e294. [Google Scholar] [CrossRef] [PubMed]
- Erhart, S.; Schmoelz, W.; Blauth, M.; Lenich, A. Biomechanical effect of bone cement augmentation on rotational stability and pull-out strength of the Proximal Femur Nail Antirotation™. Injury 2011, 42, 1322–1327. [Google Scholar] [CrossRef] [PubMed]
| Total (n = 63) | Cement Augmented Group (n = 32) | Control Group (n = 31) | p-Value | |
|---|---|---|---|---|
| Mean age, years (range) | 87.0 (65–104) | 87.0 (65–99) | 87.0 (66–104) | 0.98 |
| Men, n (%) | 14 (22.2) | 3 (9.4) | 11 (35.5) | 0.01 |
| Height, cm (SD) | 150.6 (9.3) | 149.2 (8.9) | 152.1 (9.7) | 0.22 |
| Weight, kg (SD) | 47.5 (9.6) | 46.9 (9.8) | 48.2 (9.5) | 0.59 |
| BMI, kg/m2 (SD) | 20.8 (2.9) | 21.0 (3.2) | 20.7 (2.6) | 0.71 |
| ASA classification 1, n (%) | 13 (20.6) | 7 (21.9) | 6 (19.4) | 1.00 |
| ASA classification 2, n (%) | 50 (79.4) | 25 (78.2) | 25 (80.6) | 1.00 |
| Charlson comorbidity index, median (IQR) | 2 (0–2) | 2 (0–2) | 2 (0–2) | 0.51 |
| Preoperative laboratory value | ||||
| Hemoglobin, g/dL (SD) | 10.7 (1.8) | 10.6 (1.6) | 10.9 (2.1) | 0.61 |
| Albumin, g/dL (SD) | 3.3 (0.5) | 3.3 (0.4) | 3.3 (0.5) | 0.91 |
| Pre-fracture ambulatory level | ||||
| IA without gait aids, n (%) | 32 (50.8) | 17 (53.1) | 15 (48.4) | 0.70 |
| Pre-fracture resistance (single- and co-residence), n (%) | 52 (82.5) | 25 (78.2) | 27 (87.1) | 0.34 |
| Treatment for osteoporosis, n (%) | 6 (9.5) | 4 (12.5) | 2 (6.5) | 0.41 |
| Dementia, n (%) | 37 (58.7) | 20 (62.5) | 17 (54.8) | 0.54 |
| Fracture type A1, n (%) (A1.2/1.3) | 48 (76.2) | 23 (71.9) | 25 (80.6) | 0.41 |
| Fracture type A2, n (%) (A2.2/2.3) | 15 (23.8) | 9 (28.1) | 6 (19.4) | 0.41 |
| Time to surgery, day (SD) | 3.3 (1.8) | 3.2 (1.9) | 3.4 (1.8) | 0.45 |
| Total (n = 63) | Cement Augmented Group (n = 32) | Control Group (n = 31) | p-Value | |
|---|---|---|---|---|
| TAD, mm (SD) | 20.2 (4.8) | 21.1 (4.5) | 19.3 (5.1) | 0.15 |
| Center-center blade position, n (%) | 55 (87.3) | 29 (90.6) | 26 (83.9) | 0.42 |
| Adequate reduction with AP Xp, n (%) | 63 (100) | 32 (100) | 31 (100) | 1.00 |
| Adequate reduction with lateral Xp, n (%) | 58 (92.1) | 30 (93.8) | 28 (90.3) | 0.61 |
| Baumgaertner criteria, good, n (%) | 60 (95.2) | 30 (93.8) | 30 (96.8) | 0.57 |
| Surgical time, min (SD) | 47.5 (21.7) | 46.0 (22.7) | 49.0 (20.9) | 0.59 |
| Intraoperative blood loss, cc, median (IQR) | 50 (45–50) | 50 (47.5–100) | 50 (45–50) | 0.52 |
| Total (n = 63) | Cement Augmented Group (n = 32) | Control Group (n = 31) | p-Value | |
|---|---|---|---|---|
| CAS at day 1–3, median (IQR) | 4.0 (2–6) | 5.0 (3.8–6.3) | 3.0 (1.0–4.5) | 0.004 |
| VAS at rest day 1, median (IQR) | 2.0 (0–5.3) | 0.09 (0–2.3) | 4.6 (0–7.3) | 0.003 |
| VAS at rest day 2, median (IQR) | 0 (0–2.2) | 0 (0–2.0) | 0.7 (0–2.7) | 0.183 |
| VAS at rest day 3, median (IQR) | 0 (0–1.9) | 0 (0–0.71) | 0 (0–3.0) | 0.060 |
| VAS during movement day 1, median (IQR) | 8.0 (5.9–9.3) | 8.0 (6.0–8.3) | 8.0 (5.7–10) | 0.241 |
| VAS during movement day 2, median (IQR) | 5.7 (4.0–8.0) | 5.0 (4.0–7.0) | 6.0 (4.3–8.0) | 0.225 |
| VAS during movement day 3, median (IQR) | 5.0 (3.0–7.2) | 4.0 (2.3–5.3) | 7.0 (3.6–8.4) | 0.004 |
| Barthel index at 1 week, median (IQR) | 40 (15–52.5) | 45.0 (20–51.3) | 35.0 (10–52.5) | 0.247 |
| RPAL at 1 week, n (%) | 2 (3.2) | 2 (6.3) | 0 (0) | 0.150 |
| Sink classification 1/2, n (%) | 50/13 (79.4) | 23/9 (71.9) | 27/4 (87.1) | 0.136 |
| Complications during postoperative week 1, n (%) | 42 (66.7) | 19 (59.4) | 23 (74.2) | 0.212 |
| Adjusted R2 | Beta (95% CI) | Adjusted Beta (95% CI) | p-Value | |
|---|---|---|---|---|
| 0.121 | 0.01 | |||
| Constant | 3.95 (−5.66 to 13.55) | 0.42 | ||
| Age | 0.01 (−0.11 to 0.12) | 0.01 (−0.26, 0.28) | 0.95 | |
| CCI | −0.22 (−0.75 to 0.31) | −0.12 (−0.39, 0.16) | 0.40 | |
| Dementia | −0.55 (−1.51 to 0.42) | −0.17 (−0.48, 0.13) | 0.26 | |
| Cement augmentation | 2.05 (0.51 to 3.59) | 0.33 (0.08, 0.59) | 0.01 |
| Authors | Study Design | CA Cases (n) | Control Cases (n) | Implant | Timing of Evaluation (Post Operation) | Clinical Outcomes |
|---|---|---|---|---|---|---|
| Dall’Oca et al. (2010) [30] | RCT | 40 | 40 | Gamma nail 3 | 1,3,6,12 months | Harris hip score; without a certain tendency |
| Kammerlander et al. (2018) [9] | RCT | 85 | 115 | PFNA | 3,6,12 months | There were no significant differences in time taken to walk 3 m and RPAL. |
| Kim.et al. (2018) [31] | Retrospective cohort study | 40 | 42 | PFN | 6 months | The CA group had higher Harris hip scores and lower VAS pain scores. |
| Keppler et al. (2021) [29] | Prospective cohort study | 24 | 24 | PFNA | 5 days | The CA group had higher Barthel index values and loading rates. |
| Mitsuzawa et al. (2021) [32] | Prospective cohort study | 9 | 9 | TFNA | 2 weeks | The CA group had lower VAS scores in full load walking and higher Parker mobility scores. |
| Kulachote et al. (2021) [28] | Retrospective cohort study | 68 | 67 | PFNA | 1 year | The CA group had higher RPALs. |
| Our study (2022) | Prospective cohort study | 32 | 32 | TFNA | 1–3 days, 1 week | The CA group had higher CASs after multiple linear regression analysis. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mochizuki, Y.; Yamamoto, N.; Fujii, T.; Tomita, Y. Effectiveness of Cement Augmentation on Early Postoperative Mobility in Patients Treated for Trochanteric Fractures with Cephalomedullary Nailing: A Prospective Cohort Study. J. Pers. Med. 2022, 12, 1392. https://doi.org/10.3390/jpm12091392
Mochizuki Y, Yamamoto N, Fujii T, Tomita Y. Effectiveness of Cement Augmentation on Early Postoperative Mobility in Patients Treated for Trochanteric Fractures with Cephalomedullary Nailing: A Prospective Cohort Study. Journal of Personalized Medicine. 2022; 12(9):1392. https://doi.org/10.3390/jpm12091392
Chicago/Turabian StyleMochizuki, Yusuke, Norio Yamamoto, Tatsuya Fujii, and Yosuke Tomita. 2022. "Effectiveness of Cement Augmentation on Early Postoperative Mobility in Patients Treated for Trochanteric Fractures with Cephalomedullary Nailing: A Prospective Cohort Study" Journal of Personalized Medicine 12, no. 9: 1392. https://doi.org/10.3390/jpm12091392
APA StyleMochizuki, Y., Yamamoto, N., Fujii, T., & Tomita, Y. (2022). Effectiveness of Cement Augmentation on Early Postoperative Mobility in Patients Treated for Trochanteric Fractures with Cephalomedullary Nailing: A Prospective Cohort Study. Journal of Personalized Medicine, 12(9), 1392. https://doi.org/10.3390/jpm12091392






