Structured Reporting in Radiological Settings: Pitfalls and Perspectives
Abstract
:1. Introduction
2. Method
3. Description
- I.
- At the first level, a SR is subdivided into sections and subheadings. Now, all radiological reports have these forms, including sections for clinical data, study protocols, radiological findings, and conclusions to emphasize the main radiological features.
- II.
- At the second level, the report is organized, explaining all the relevant specific disease findings.
- III.
- At the third level, the report includes a standard lexicon.
4. Perspectives and Clinical Settings
5. Open Questions: Radiologists and SR
6. Pitfalls
7. Educational: Resident and Structured Report
8. Discussion and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- European Society of Radiology (ESR). ESR paper on structured reporting in radiology. Insights Imaging 2018, 9, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- American Recovery and Reinvestment Act of 2009 Title XIII: Health Information Technology: Health Information Technology for Economic and Clinical Health Act (HITECH Act), 112–164. US Government. Available online: https://www.healthit.gov/sites/default/files/hitech_act_excerpt_from_arra_with_index.pdf (accessed on 6 June 2022).
- Sobez, L.M.; Kim, S.H.; Angstwurm, M.; Störmann, S.; Pförringer, D.; Schmidutz, F.; Prezzi, D.; Kelly-Morland, C.; Sommer, W.H.; Sabel, B.; et al. Creating high-quality radiology reports in foreign languages through multilingual structured reporting. Eur. Radiol. 2019, 29, 6038–6048. [Google Scholar] [CrossRef] [PubMed]
- Segrelles, J.D.; Medina, R.; Blanquer, I.; Martí-Bonmatí, L. Increasing the Efficiency on Producing Radiology Reports for Breast Cancer Diagnosis by Means of Structured Reports. A Comparative Study. Methods Inf. Med. 2017, 56, 248–260. [Google Scholar]
- Ierardi, A.M.; Wood, B.J.; Arrichiello, A.; Bottino, N.; Bracchi, L.; Forzenigo, L.; Andrisani, M.C.; Vespro, V.; Bonelli, C.; Amalou, A.; et al. Preparation of a radiology department in an Italian hospital dedicated to COVID-19 patients. Radiol. Med. 2020, 125, 894–901. [Google Scholar] [CrossRef]
- Caranci, F.; Leone, G.; Ponsiglione, A.; Muto, M.; Tortora, F.; Muto, M.; Cirillo, S.; Brunese, L.; Cerase, A. Imaging findings in hypophysitis: A review. Radiol. Med. 2020, 125, 319–328. [Google Scholar] [CrossRef]
- Bécares-Martínez, C.; López-Llames, A.; Martín-Pagán, A.; Cores-Prieto, A.E.; Arroyo-Domingo, M.; Marco-Algarra, J.; Morales-Suárez-Varela, M. Cervical spine radiographs in patients with vertigo and dizziness. Radiol. Med. 2020, 125, 272–279. [Google Scholar] [CrossRef] [PubMed]
- Pinto Dos Santos, D.; Hempel, J.M.; Mildenberger, P.; Klöckner, R.; Persigehl, T. Structured Reporting in Clinical Routine. Rofo 2019, 191, 33–39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Larson, D.B.; Towbin, A.J.; Pryor, R.M.; Donnelly, L.F. Improving consistency in radiology reporting through the use of department-wide standardized structured reporting. Radiology 2013, 267, 240–250. [Google Scholar] [CrossRef] [Green Version]
- Brook, O.R.; Brook, A.; Vollmer, C.M.; Kent, T.S.; Sanchez, N.; Pedrosa, I. Structured reporting of multiphasic CT for pancreatic cancer: Potential effect on staging and surgical planning. Radiology 2015, 274, 464–472. [Google Scholar] [CrossRef]
- Lee, M.C.; Chuang, K.S.; Hsu, T.C.; Lee, C.D. Enhancement of Structured Reporting—An Integration Reporting Module with Radiation Dose Collection Supporting. J. Med. Syst. 2016, 40, 250. [Google Scholar] [CrossRef]
- Pediconi, F.; Galati, F.; Bernardi, D.; Belli, P.; Brancato, B.; Calabrese, M.; Camera, L.; Carbonaro, L.A.; Caumo, F.; Clauser, P.; et al. Breast imaging and cancer diagnosis during the COVID-19 pandemic: Recommendations from the Italian College of Breast Radiologists by SIRM. Radiol. Med. 2020, 125, 926–930. [Google Scholar] [CrossRef] [PubMed]
- Gurgitano, M.; Angileri, S.A.; Rodà, G.M.; Liguori, A.; Pandolfi, M.; Ierardi, A.M.; Wood, B.J.; Carrafiello, G. Interventional Radiology ex-machina: Impact of Artificial Intelligence on practice. Radiol. Med. 2021, 126, 998–1006. [Google Scholar] [CrossRef] [PubMed]
- Deandrea, S.; Cavazzana, L.; Principi, N.; Luconi, E.; Campoleoni, M.; Bastiampillai, A.J.; Bracchi, L.; Bucchi, L.; Pedilarco, S.; Piscitelli, A.; et al. Screening of women with aesthetic prostheses in dedicated sessions of a population-based breast cancer screening programme. Radiol. Med. 2021, 126, 946–955. [Google Scholar] [CrossRef] [PubMed]
- Eghtedari, M.; Chong, A.; Rakow-Penner, R.; Ojeda-Fournier, H. Current Status and Future of BI-RADS in Multimodality Imaging, From the AJR Special Series on Radiology Reporting and Data Systems. AJR Am. J. Roentgenol. 2021, 216, 860–873. [Google Scholar] [CrossRef]
- Bimonte, S.; Leongito, M.; Barbieri, A.; Del Vecchio, V.; Barbieri, M.; Albino, V.; Piccirillo, M.; Amore, A.; Di Giacomo, R.; Nasto, A.; et al. Inhibitory effect of (-)-epigallocatechin-3-gallate and bleomycin on human pancreatic cancer MiaPaca-2 cell growth. Infect. Agents Cancer 2015, 10, 22. [Google Scholar] [CrossRef]
- Granata, V.; Fusco, R.; Catalano, O.; Piccirillo, M.; De Bellis, M.; Izzo, F.; Petrillo, A. Percutaneous ablation therapy of hepatocellular carcinoma with irreversible electroporation: MRI findings. AJR Am. J. Roentgenol. 2015, 204, 1000–1007. [Google Scholar] [CrossRef]
- D’Agostino, V.; Caranci, F.; Negro, A.; Piscitelli, V.; Tuccillo, B.; Fasano, F.; Sirabella, G.; Marano, I.; Granata, V.; Grassi, R.; et al. A Rare Case of Cerebral Venous Thrombosis and Disseminated Intravascular Coagulation Temporally Associated to the COVID-19 Vaccine Administration. J. Pers. Med. 2021, 11, 285. [Google Scholar] [CrossRef]
- di Giacomo, V.; Trinci, M.; van der Byl, G.; Catania, V.D.; Calisti, A.; Miele, V. Ultrasound in newborns and children suffering from non-traumatic acute abdominal pain: Imaging with clinical and surgical correlation. J. Ultrasound 2014, 18, 385–393. [Google Scholar] [CrossRef] [Green Version]
- Miele, V.; Di Giampietro, I. Diagnostic Imaging in Emergency. Salut. Soc. 2014, 2EN, 127–138. [Google Scholar]
- Granata, V.; Grassi, R.; Fusco, R.; Izzo, F.; Brunese, L.; Delrio, P.; Avallone, A.; Pecori, B.; Petrillo, A. Current status on response to treatment in locally advanced rectal cancer: What the radiologist should know. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 12050–12062. [Google Scholar]
- Park, S.H.; Kim, Y.S.; Choi, J. Dosimetric analysis of the effects of a temporary tissue expander on the radiotherapy technique. Radiol. Med. 2021, 126, 437–444. [Google Scholar] [CrossRef] [PubMed]
- Karmazanovsky, G.; Gruzdev, I.; Tikhonova, V.; Kondratyev, E.; Revishvili, A. Computed tomography-based radiomics approach in pancreatic tumors characterization. Radiol. Med. 2021. [Google Scholar] [CrossRef] [PubMed]
- Bertocchi, E.; Barugola, G.; Nicosia, L.; Mazzola, R.; Ricchetti, F.; Dell’Abate, P.; Alongi, F.; Ruffo, G. A comparative analysis between radiation dose intensification and conventional fractionation in neoadjuvant locally advanced rectal cancer: A monocentric prospective observational study. Radiol. Med. 2020, 125, 990–998. [Google Scholar] [CrossRef] [PubMed]
- Bracci, S.; Dolciami, M.; Trobiani, C.; Izzo, A.; Pernazza, A.; D’Amati, G.; Manganaro, L.; Ricci, P. Quantitative CT texture analysis in predicting PD-L1 expression in locally advanced or metastatic NSCLC patients. Radiol. Med. 2021, 126, 1425–1433. [Google Scholar] [CrossRef]
- Caruso, D.; Pucciarelli, F.; Zerunian, M.; Ganeshan, B.; De Santis, D.; Polici, M.; Rucci, C.; Polidori, T.; Guido, G.; Bracci, B.; et al. Chest CT texture-based radiomics analysis in differentiating COVID-19 from other interstitial pneumonia. Radiol. Med. 2021, 126, 1415–1424. [Google Scholar] [CrossRef]
- Avallone, A.; Pecori, B.; Bianco, F.; Aloj, L.; Tatangelo, F.; Romano, C.; Granata, V.; Marone, P.; Leone, A.; Botti, G.; et al. Critical role of bevacizumab scheduling in combination with pre-surgical chemo-radiotherapy in MRI-defined high-risk locally advanced rectal cancer: Results of the BRANCH trial. Oncotarget 2015, 6, 30394–303407. [Google Scholar] [CrossRef] [Green Version]
- Petralia, G.; Zugni, F.; Summers, P.E.; Colombo, A.; Pricolo, P.; Grazioli, L.; Colagrande, S.; Giovagnoni, A.; Padhani, A.R.; Italian Working Group on Magnetic Resonance. Whole-body magnetic resonance imaging (WB-MRI) for cancer screening: Recommendations for use. Radiol. Med. 2021, 126, 1434–1450. [Google Scholar] [CrossRef]
- Petralia, G.; Summers, P.E.; Agostini, A.; Ambrosini, R.; Cianci, R.; Cristel, G.; Calistri, L.; Colagrande, S. Dynamic contrast-enhanced MRI in oncology: How we do it. Radiol. Med. 2020, 125, 1288–1300. [Google Scholar] [CrossRef]
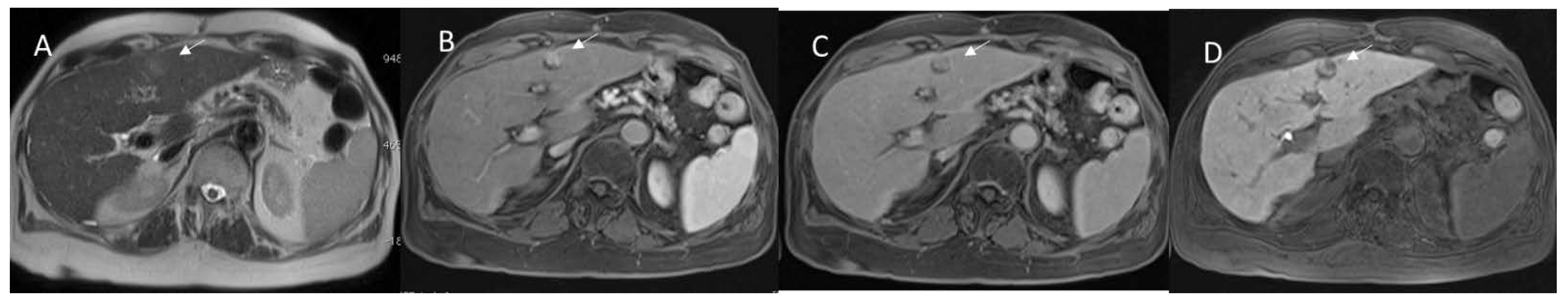
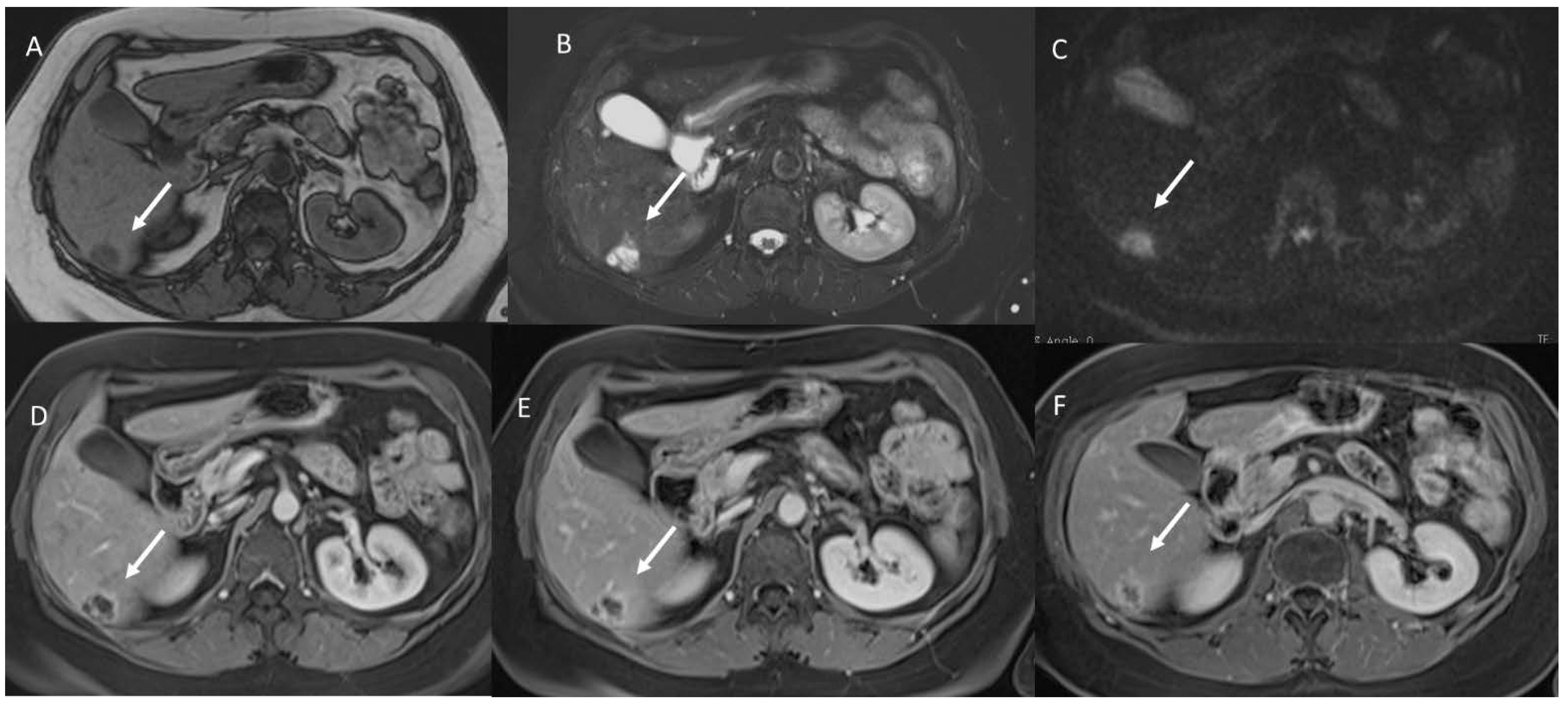
- Granata, V.; Grassi, R.; Fusco, R.; Setola, S.V.; Belli, A.; Ottaiano, A.; Nasti, G.; La Porta, M.; Danti, G.; Cappabianca, S.; et al. Intrahepatic cholangiocarcinoma and its differential diagnosis at MRI: How radiologist should assess MR features. Radiol. Med. 2021, 126, 1584–1600. [Google Scholar] [CrossRef]
- Weiss, D.L.; Bolos, P.R. Reporting and dictation. In Branstetter IV BF: Practical Imaging Informatics: Foundations and Applications for PACS Professionals; Springer: Berlin/Heidelberg, Germany, 2019. [Google Scholar]
- De Muzio, F.; Cutolo, C.; Granata, V.; Fusco, R.; Ravo, L.; Maggialetti, N.; Brunese, M.C.; Grassi, R.; Grassi, F.; Bruno, F.; et al. CT study protocol optimization in acute non-traumatic abdominal settings. Eur. Rev. Med. Pharmacol. Sci. 2022, 26, 860–878. [Google Scholar]
- Granata, V.; Fusco, R.; Venanzio Setola, S.; Barretta, M.L.; Iasevoli, D.M.A.; Palaia, R.; Belli, A.; Patrone, R.; Tatangelo, F.; Grazzini, G.; et al. Diagnostic performance of LI-RADS in adult patients with rare hepatic tumors. Eur. Rev. Med. Pharmacol. Sci. 2022, 26, 399–414. [Google Scholar] [PubMed]
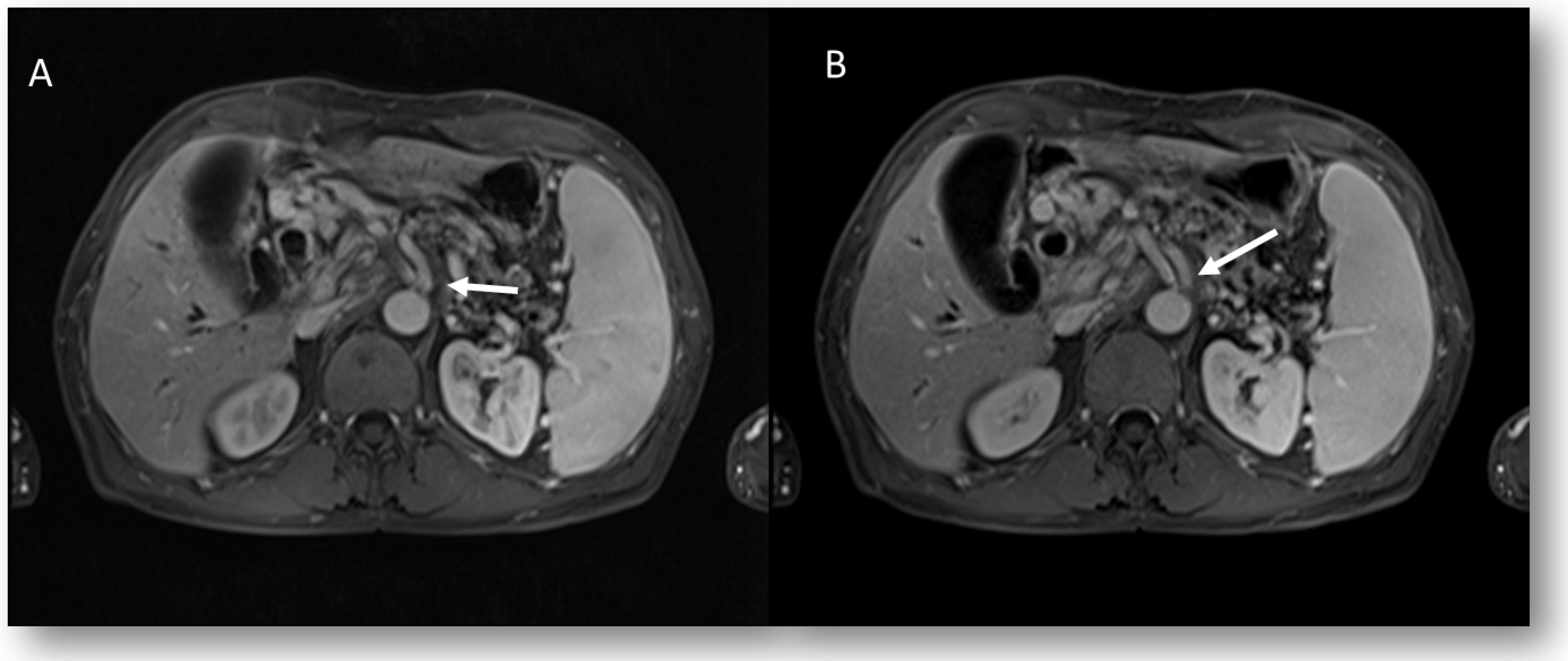
- Granata, V.; Fusco, R.; Setola, S.V.; Piccirillo, M.; Leongito, M.; Palaia, R.; Granata, F.; Lastoria, S.; Izzo, F.; Petrillo, A. Early radiological assessment of locally advanced pancreatic cancer treated with electrochemotherapy. World J. Gastroenterol. 2017, 23, 4767–4778. [Google Scholar] [CrossRef] [PubMed]
- Granata, V.; Fusco, R.; Bicchierai, G.; Cozzi, D.; Grazzini, G.; Danti, G.; De Muzio, F.; Maggialetti, N.; Smorchkova, O.; D’Elia, M.; et al. Diagnostic protocols in oncology: Workup and treatment planning. Part 1: The optimitation of CT protocol. Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 6972–6994. [Google Scholar]
- Granata, V.; Bicchierai, G.; Fusco, R.; Cozzi, D.; Grazzini, G.; Danti, G.; De Muzio, F.; Maggialetti, N.; Smorchkova, O.; D’Elia, M.; et al. Diagnostic protocols in oncology: Workup and treatment planning. Part 2: Abbreviated MR protocol. Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 6499–6528. [Google Scholar] [PubMed]
- Liu, J.; Wang, C.; Guo, W.; Zeng, P.; Liu, Y.; Lang, N.; Yuan, H. A preliminary study using spinal MRI-based radiomics to predict high-risk cytogenetic abnormalities in multiple myeloma. Radiol. Med. 2021, 126, 1226–1235. [Google Scholar] [CrossRef] [PubMed]
- Bilreiro, C.; Soler, J.C.; Ayuso, J.R.; Caseiro-Alves, F.; Ayuso, C. Diagnostic value of morphological enhancement patterns in the hepatobiliary phase of gadoxetic acid-enhanced MRI to distinguish focal nodular hyperplasia from hepatocellular adenoma. Radiol. Med. 2021, 126, 1379–1387. [Google Scholar] [CrossRef] [PubMed]
- Esposito, A.; Buscarino, V.; Raciti, D.; Casiraghi, E.; Manini, M.; Biondetti, P.; Forzenigo, L. Characterization of liver nodules in patients with chronic liver disease by MRI: Performance of the Liver Imaging Reporting and Data System (LI-RADS v.2018) scale and its comparison with the Likert scale. Radiol. Med. 2020, 125, 15–23. [Google Scholar] [CrossRef]
- Qin, H.; Que, Q.; Lin, P.; Li, X.; Wang, X.R.; He, Y.; Chen, J.Q.; Yang, H. Magnetic resonance imaging (MRI) radiomics of papillary thyroid cancer (PTC): A comparison of predictive performance of multiple classifiers modeling to identify cervical lymph node metastases before surgery. Radiol. Med. 2021; 126, 1312–1327. [Google Scholar] [CrossRef]
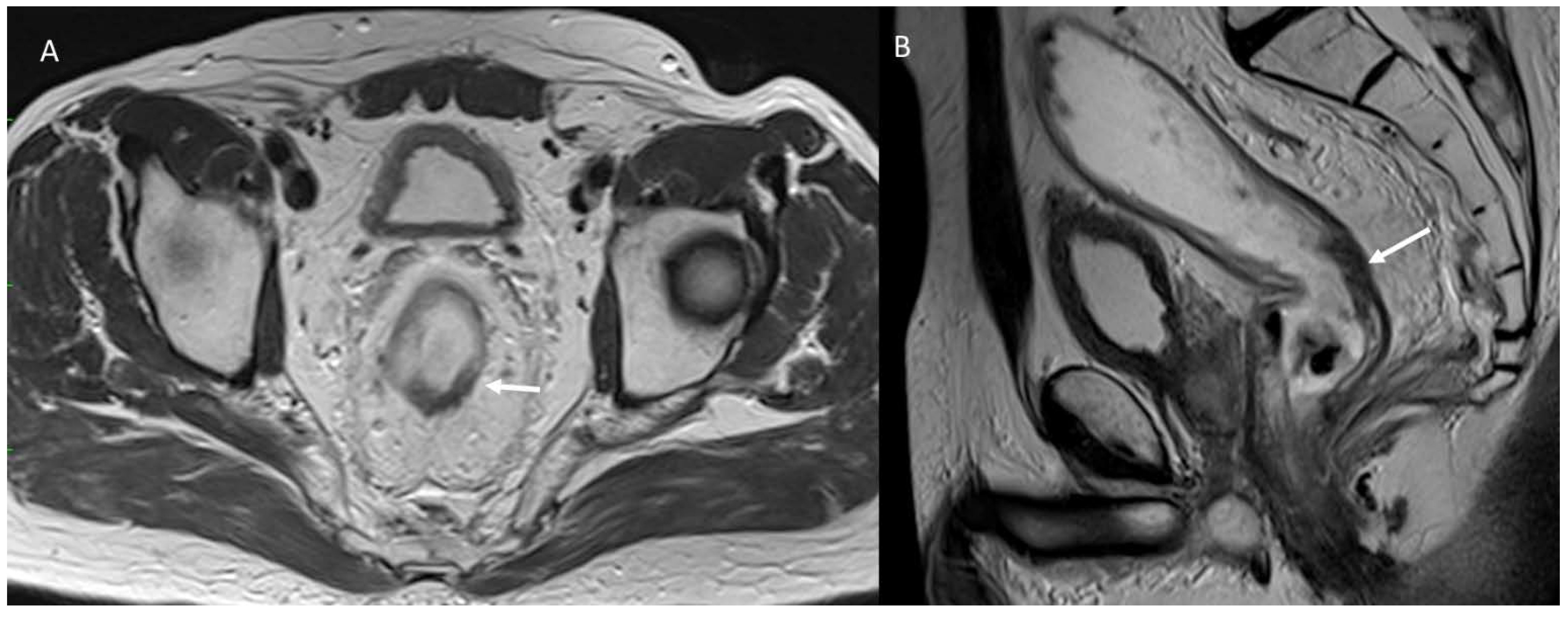
- Santone, A.; Brunese, M.C.; Donnarumma, F.; Guerriero, P.; Mercaldo, F.; Reginelli, A.; Miele, V.; Giovagnoni, A.; Brunese, L. Radiomic features for prostate cancer grade detection through formal verification. Radiol. Med. 2021, 126, 688–697. [Google Scholar] [CrossRef]
- Fusco, R.; Petrillo, M.; Granata, V.; Filice, S.; Sansone, M.; Catalano, O.; Petrillo, A. Magnetic Resonance Imaging Evaluation in Neoadjuvant Therapy of Locally Advanced Rectal Cancer: A Systematic Review. Radiol. Oncol. 2017, 51, 252–262. [Google Scholar] [CrossRef]
- Agazzi, G.M.; Ravanelli, M.; Roca, E.; Medicina, D.; Balzarini, P.; Pessina, C.; Vermi, W.; Berruti, A.; Maroldi, R.; Farina, D. CT texture analysis for prediction of EGFR mutational status and ALK rearrangement in patients with non-small cell lung cancer. Radiol. Med. 2021, 126, 786–794. [Google Scholar] [CrossRef]
- Fusco, R.; Granata, V.; Mazzei, M.A.; Meglio, N.D.; Roscio, D.D.; Moroni, C.; Monti, R.; Cappabianca, C.; Picone, C.; Neri, E.; et al. Quantitative imaging decision support (QIDSTM) tool consistency evaluation and radiomic analysis by means of 594 metrics in lung carcinoma on chest CT scan. Cancer Control. 2021, 28, 1073274820985786. [Google Scholar] [CrossRef] [PubMed]
- Kirienko, M.; Ninatti, G.; Cozzi, L.; Voulaz, E.; Gennaro, N.; Barajon, I.; Ricci, F.; Carlo-Stella, C.; Zucali, P.; Sollini, M.; et al. Computed tomography (CT)-derived radiomic features differentiate prevascular mediastinum masses as thymic neoplasms versus lymphomas. Radiol. Med. 2020, 125, 951–960. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Kang, L.; Li, G.; Zhang, X.; Ren, J.; Shi, Z.; Li, J.; Yu, S. Computed tomography-based radiomics model for discriminating the risk stratification of gastrointestinal stromal tumors. Radiol. Med. 2020, 125, 465–473. [Google Scholar] [CrossRef] [PubMed]
- Scapicchio, C.; Gabelloni, M.; Barucci, A.; Cioni, D.; Saba, L.; Neri, E. A deep look into radiomics. Radiol. Med. 2021, 126, 1296–1311. [Google Scholar] [CrossRef]
- Benedetti, G.; Mori, M.; Panzeri, M.M.; Barbera, M.; Palumbo, D.; Sini, C.; Muffatti, F.; Andreasi, V.; Steidler, S.; Doglioni, C.; et al. CT-derived radiomic features to discriminate histologic characteristics of pancreatic neuroendocrine tumors. Radiol. Med. 2021, 126, 745–760. [Google Scholar] [CrossRef]
- Laurelli, G.; Falcone, F.; Gallo, M.S.; Scala, F.; Losito, S.; Granata, V.; Cascella, M.; Greggi, S. Long-Term Oncologic and Reproductive Outcomes in Young Women With Early Endometrial Cancer Conservatively Treated: A Prospective Study and Literature Update. Int. J. Gynecol. Cancer 2016, 26, 1650–1657. [Google Scholar] [CrossRef]
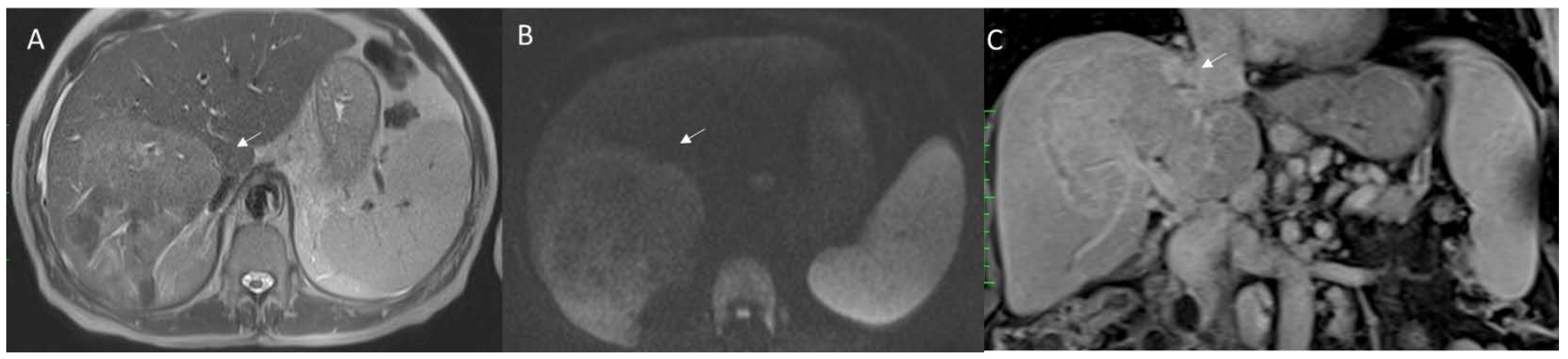
- Granata, V.; Petrillo, M.; Fusco, R.; Setola, S.V.; de Lutio di Castelguidone, E.; Catalano, O.; Piccirillo, M.; Albino, V.; Izzo, F.; Petrillo, A. Surveillance of HCC Patients after Liver RFA: Role of MRI with Hepatospecific Contrast versus Three-Phase CT Scan-Experience of High Volume Oncologic Institute. Gastroenterol. Res. Pract. 2013, 2013, 469097. [Google Scholar] [CrossRef]
- Granata, V.; Fusco, R.; Venanzio Setola, S.; Mattace Raso, M.; Avallone, A.; De Stefano, A.; Nasti, G.; Palaia, R.; Delrio, P.; Petrillo, A.; et al. Liver radiologic findings of chemotherapy-induced toxicity in liver colorectal metastases patients. Eur. Rev. Med. Pharmacol. Sci. 2019, 23, 9697–9706. [Google Scholar]
- Nardone, V.; Reginelli, A.; Grassi, R.; Boldrini, L.; Vacca, G.; D’Ippolito, E.; Annunziata, S.; Farchione, A.; Belfiore, M.P.; Desideri, I.; et al. Delta radiomics: A systematic review. Radiol. Med. 2021, 126, 1571–1583. [Google Scholar] [CrossRef]
- Masci, G.M.; Iafrate, F.; Ciccarelli, F.; Pambianchi, G.; Panebianco, V.; Pasculli, P.; Ciardi, M.R.; Mastroianni, C.M.; Ricci, P.; Catalano, C.; et al. Tocilizumab effects in COVID-19 pneumonia: Role of CT texture analysis in quantitative assessment of response to therapy. Radiol. Med. 2021, 126, 1170–1180. [Google Scholar] [CrossRef]
- Cicero, G.; Ascenti, G.; Albrecht, M.H.; Blandino, A.; Cavallaro, M.; D’Angelo, T.; Carerj, M.L.; Vogl, T.J.; Mazziotti, S. Extra-abdominal dual-energy CT applications: A comprehensive overview. Radiol. Med. 2020, 125, 384–397. [Google Scholar] [CrossRef] [PubMed]
- Ohashi, Y.; Takashima, H.; Ohmori, G.; Harada, K.; Chiba, A.; Numasawa, K.; Imai, T.; Hayasaka, S.; Itoh, A. Efficacy of non-rigid registration technique for misregistration in 3D-CTA fusion imaging. Radiol. Med. 2020, 125, 618–624. [Google Scholar] [CrossRef] [PubMed]
- Michallek, F.; Nakamura, S.; Ota, H.; Ogawa, R.; Shizuka, T.; Nakashima, H.; Wang, Y.N.; Ito, T.; Sakuma, H.; Dewey, M.; et al. Fractal analysis of 4D dynamic myocardial stress-CT perfusion imaging differentiates micro- and macrovascular ischemia in a multi-center proof-of-concept study. Sci. Rep. 2022, 12, 5085. [Google Scholar] [CrossRef] [PubMed]
- Gatti, M.; Calandri, M.; Bergamasco, L.; Darvizeh, F.; Grazioli, L.; Inchingolo, R.; Ippolito, D.; Rousset, S.; Veltri, A.; Fonio, P.; et al. Characterization of the arterial enhancement pattern of focal liver lesions by multiple arterial phase magnetic resonance imaging: Comparison between hepatocellular carcinoma and focal nodular hyperplasia. Radiol. Med. 2020, 125, 348–355. [Google Scholar] [CrossRef]
- Granata, V.; Fusco, R.; Filice, S.; Catalano, O.; Piccirillo, M.; Palaia, R.; Izzo, F.; Petrillo, A. The current role and future prospectives of functional parameters by diffusion weighted imaging in the assessment of histologic grade of HCC. Infect. Agents Cancer 2018, 13, 23. [Google Scholar] [CrossRef] [Green Version]
- Fusco, R.; Sansone, M.; Granata, V.; Setola, S.V.; Petrillo, A. A systematic review on multiparametric MR imaging in prostate cancer detection. Infect. Agents Cancer 2017, 12, 57. [Google Scholar] [CrossRef] [Green Version]
- Gholizadeh, N.; Greer, P.B.; Simpson, J.; Goodwin, J.; Fu, C.; Lau, P.; Siddique, S.; Heerschap, A.; Ramadan, S. Diagnosis of transition zone prostate cancer by multiparametric MRI: Added value of MR spectroscopic imaging with sLASER volume selection. J. Biomed. Sci. 2021, 28, 54. [Google Scholar] [CrossRef]
- Gholizadeh, N.; Simpson, J.; Ramadan, S.; Denham, J.; Lau, P.; Siddique, S.; Dowling, J.; Welsh, J.; Chalup, S.; Greer, P.B. Voxel-based supervised machine learning of peripheral zone prostate cancer using noncontrast multiparametric MRI. J. Appl. Clin. Med. Phys. 2020, 21, 179–191. [Google Scholar] [CrossRef]
- Petrillo, A.; Fusco, R.; Petrillo, M.; Granata, V.; Delrio, P.; Bianco, F.; Pecori, B.; Botti, G.; Tatangelo, F.; Caracò, C.; et al. Standardized Index of Shape (DCE-MRI) and Standardized Uptake Value (PET/CT): Two quantitative approaches to discriminate chemo-radiotherapy locally advanced rectal cancer responders under a functional profile. Oncotarget 2017, 8, 8143–8153. [Google Scholar] [CrossRef] [Green Version]
- Higashi, M.; Tanabe, M.; Okada, M.; Furukawa, M.; Iida, E.; Ito, K. Influence of fat deposition on T1 mapping of the pancreas: Evaluation by dual-flip-angle MR imaging with and without fat suppression. Radiol. Med. 2020, 125, 1–6. [Google Scholar] [CrossRef]
- Li, J.; Cao, B.; Bi, X.; Chen, W.; Wang, L.; Du, Z.; Zhang, X.; Yu, X. Evaluation of liver function in patients with chronic hepatitis B using Gd-EOB-DTPA-enhanced T1 mapping at different acquisition time points: A feasibility study. Radiol. Med. 2021, 126, 1149–1158. [Google Scholar] [CrossRef] [PubMed]
- Granata, V.; Caruso, D.; Grassi, R.; Cappabianca, S.; Reginelli, A.; Rizzati, R.; Masselli, G.; Golfieri, R.; Rengo, M.; Regge, D.; et al. Structured Reporting of Rectal Cancer Staging and Restaging: A Consensus Proposal. Cancers 2021, 13, 2135. [Google Scholar] [CrossRef] [PubMed]
- Beets-Tan, R.G.H.; Lambregts, D.M.J.; Maas, M.; Bipat, S.; Barbaro, B.; Curvo-Semedo, L.; Fenlon, H.M.; Gollub, M.J.; Gourtsoyianni, S.; Halligan, S.; et al. Magnetic resonance imaging for clinical management of rectal cancer: Updated recommendations from the 2016 European Society of Gastrointestinal and Abdominal Radiology (ESGAR) consensus meeting. Eur. Radiol. 2018, 28, 1465–1475. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rega, D.; Granata, V.; Petrillo, A.; Pace, U.; Sassaroli, C.; Di Marzo, M.; Cervone, C.; Fusco, R.; D’Alessio, V.; Nasti, G.; et al. Organ Sparing for Locally Advanced Rectal Cancer after Neoadjuvant Treatment Followed by Electrochemotherapy. Cancers 2021, 13, 3199. [Google Scholar] [CrossRef]
- Rega, D.; Granata, V.; Romano, C.; D’Angelo, V.; Pace, U.; Fusco, R.; Cervone, C.; Ravo, V.; Tatangelo, F.; Avallone, A.; et al. Watch and Wait Approach for Rectal Cancer Following Neoadjuvant Treatment: The Experience of a High Volume Cancer Center. Diagnostics 2021, 11, 1507. [Google Scholar] [CrossRef]
- Altinmakas, E.; Dogan, H.; Taskin, O.C.; Ozoran, E.; Bugra, D.; Adsay, V.; Balik, E.; Gurses, B. Extramural venous invasion (EMVI) revisited: A detailed analysis of various characteristics of EMVI and their role as a predictive imaging biomarker in the neoadjuvant treatment response in rectal cancer. Abdom. Radiol. 2022, 47, 1975–1987. [Google Scholar] [CrossRef]
- Zhang, D.; Duan, Y.; Guo, J.; Wang, Y.; Yang, Y.; Li, Z.; Wang, K.; Wu, L.; Yu, M. Using Multi-Scale Convolutional Neural Network Based on Multi-Instance Learning to Predict the Efficacy of Neoadjuvant Chemoradiotherapy for Rectal Cancer. IEEE J. Transl. Eng. Health Med. 2022, 10, 4300108. [Google Scholar] [CrossRef]
- Crimì, F.; Capelli, G.; Spolverato, G.; Bao, Q.R.; Florio, A.; Milite Rossi, S.; Cecchin, D.; Albertoni, L.; Campi, C.; Pucciarelli, S.; et al. MRI T2-weighted sequences-based texture analysis (TA) as a predictor of response to neoadjuvant chemo-radiotherapy (nCRT) in patients with locally advanced rectal cancer (LARC). Radiol. Med. 2020, 125, 1216–1224. [Google Scholar] [CrossRef]
- Ale Ali, H.; Kirsch, R.; Razaz, S.; Jhaveri, A.; Thipphavong, S.; Kennedy, E.D.; Jhaveri, K.S. Extramural venous invasion in rectal cancer: Overview of imaging, histopathology, and clinical implications. Abdom. Radiol. 2019, 44, 1–10. [Google Scholar] [CrossRef]
- Cusumano, D.; Meijer, G.; Lenkowicz, J.; Chiloiro, G.; Boldrini, L.; Masciocchi, C.; Dinapoli, N.; Gatta, R.; Casà, C.; Damiani, A.; et al. A field strength independent MR radiomics model to predict pathological complete response in locally advanced rectal cancer. Radiol. Med. 2021, 126, 421–429. [Google Scholar] [CrossRef]
- Dinapoli, N.; Barbaro, B.; Gatta, R.; Chiloiro, G.; Casà, C.; Masciocchi, C.; Damiani, A.; Boldrini, L.; Gambacorta, M.A.; Dezio, M.; et al. Magnetic Resonance, Vendor-independent, Intensity Histogram Analysis Predicting Pathologic Complete Response After Radiochemotherapy of Rectal Cancer. Int. J. Radiat. Oncol. Biol. Phys. 2018, 102, 765–774. [Google Scholar] [CrossRef] [PubMed]
- Granata, V.; Morana, G.; D’Onofrio, M.; Fusco, R.; Coppola, F.; Grassi, F.; Cappabianca, S.; Reginelli, A.; Maggialetti, N.; Buccicardi, D.; et al. Structured Reporting of Computed Tomography and Magnetic Resonance in the Staging of Pancreatic Adenocarcinoma: A Delphi Consensus Proposal. Diagnostics 2021, 11, 2033. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.K.; Park, M.S.; Choi, M.; Shin, J.; Lee, S.S.; Jeong, W.K.; Hwang, S.H.; Choi, S.H. Systematic review and meta-analysis of diagnostic performance of CT imaging for assessing resectability of pancreatic ductal adenocarcinoma after neoadjuvant therapy: Importance of CT criteria. Abdom. Radiol. 2021, 46, 5201–5217. [Google Scholar] [CrossRef]
- Granata, V.; Grassi, R.; Fusco, R.; Setola, S.V.; Palaia, R.; Belli, A.; Miele, V.; Brunese, L.; Grassi, R.; Petrillo, A.; et al. Assessment of Ablation Therapy in Pancreatic Cancer: The Radiologist’s Challenge. Front. Oncol. 2020, 10, 560952. [Google Scholar] [CrossRef] [PubMed]
- Al-Hawary, M.M.; Francis, I.R.; Chari, S.T.; Fishman, E.K.; Hough, D.M.; Lu, D.S.; Macari, M.; Megibow, A.J.; Miller, F.H.; Mortele, K.J.; et al. Pancreatic ductal adenocarcinoma radiology reporting template: Consensus statement of the society of abdominal radiology and the american pancreatic association. Gastroenterology 2014, 146, 291–304.e1. [Google Scholar] [CrossRef]
- Neri, E.; Granata, V.; Montemezzi, S.; Belli, P.; Bernardi, D.; Brancato, B.; Caumo, F.; Calabrese, M.; Coppola, F.; Cossu, E.; et al. Structured reporting of X-ray mammography in the first diagnosis of breast cancer: A Delphi consensus proposal. Radiol. Med. 2022, 127, 471–483. [Google Scholar] [CrossRef]
- Granata, V.; Coppola, F.; Grassi, R.; Fusco, R.; Tafuto, S.; Izzo, F.; Reginelli, A.; Maggialetti, N.; Buccicardi, D.; Frittoli, B.; et al. Structured Reporting of Computed Tomography in the Staging of Neuroendocrine Neoplasms: A Delphi Consensus Proposal. Front. Endocrinol. 2021, 12, 748944. [Google Scholar] [CrossRef]
- Granata, V.; Faggioni, L.; Grassi, R.; Fusco, R.; Reginelli, A.; Rega, D.; Maggialetti, N.; Buccicardi, D.; Frittoli, B.; Rengo, M.; et al. Structured reporting of computed tomography in the staging of colon cancer: A Delphi consensus proposal. Radiol. Med. 2022, 127, 21–29. [Google Scholar] [CrossRef]
- Granata, V.; Grassi, R.; Miele, V.; Larici, A.R.; Sverzellati, N.; Cappabianca, S.; Brunese, L.; Maggialetti, N.; Borghesi, A.; Fusco, R.; et al. Structured Reporting of Lung Cancer Staging: A Consensus Proposal. Diagnostics 2021, 11, 1569. [Google Scholar] [CrossRef]
- Granata, V.; Pradella, S.; Cozzi, D.; Fusco, R.; Faggioni, L.; Coppola, F.; Grassi, R.; Maggialetti, N.; Buccicardi, D.; Lacasella, G.V.; et al. Computed Tomography Structured Reporting in the Staging of Lymphoma: A Delphi Consensus Proposal. J. Clin. Med. 2021, 10, 4007. [Google Scholar] [CrossRef]
- Neri, E.; Coppola, F.; Larici, A.R.; Sverzellati, N.; Mazzei, M.A.; Sacco, P.; Dalpiaz, G.; Feragalli, B.; Miele, V.; Grassi, R. Structured reporting of chest CT in COVID-19 pneumonia: A consensus proposal. Insights Imaging 2020, 11, 92. [Google Scholar] [CrossRef] [PubMed]
- Granata, V.; Fusco, R.; Avallone, A.; Filice, F.; Tatangelo, F.; Piccirillo, M.; Grassi, R.; Izzo, F.; Petrillo, A. Critical analysis of the major and ancillary imaging features of LI-RADS on 127 proven HCCs evaluated with functional and morphological MRI: Lights and shadows. Oncotarget 2017, 8, 51224–51237. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Granata, V.; Fusco, R.; Avallone, A.; Catalano, O.; Filice, F.; Leongito, M.; Palaia, R.; Izzo, F.; Petrillo, A. Major and ancillary magnetic resonance features of LI-RADS to assess HCC: An overview and update. Infect. Agents Cancer 2017, 12, 23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, D.H.; Kim, B.; Lee, E.S.; Kim, H.J.; Min, J.H.; Lee, J.M.; Choi, M.H.; Seo, N.; Choi, S.H.; Kim, S.H.; et al. Radiologic Evaluation and Structured Reporting Form for Extrahepatic Bile Duct Cancer: 2019 Consensus Recommendations from the Korean Society of Abdominal Radiology. Korean J. Radiol. 2021, 22, 41–62. [Google Scholar] [CrossRef]
- Francone, M.; Budde, R.P.J.; Bremerich, J.; Dacher, J.N.; Loewe, C.; Wolf, F.; Natale, L.; Pontone, G.; Redheuil, A.; Vliegenthart, R.; et al. CT and MR imaging prior to transcatheter aortic valve implantation: Standardisation of scanning protocols, measurements and reporting-a consensus document by the European Society of Cardiovascular Radiology (ESCR). Eur. Radiol. 2020, 30, 2627–2650. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kotter, E.; Pinto Dos Santos, D. Strukturierte Befundung in der Radiologie: Sicht der deutschen und europäischen Fachgesellschaften [Structured reporting in radiology: German and European radiology societies’ point of view]. Radiologe 2021, 61, 979–985. [Google Scholar] [CrossRef]
- Available online: www.sirm.org (accessed on 6 June 2022).
- Faggioni, L.; Coppola, F.; Ferrari, R.; Neri, E.; Regge, D. Usage of structured reporting in radiological practice: Results from an Italian online survey. Eur. Radiol. 2017, 27, 1934–1943. [Google Scholar] [CrossRef]
- Brady, A.P. Radiology reporting-from Hemingway to HAL? Insights Imaging 2018, 9, 237–246. [Google Scholar] [CrossRef] [Green Version]
- Berretta, M.; Di Francia, R.; Cazzavillan, S.; Rossi, P.; Scorba, A.; Sciacca, P.G.; Santagà, D. Integrative Medicine in Oncology, Milan October 19th, 2019. WCRJ 2019, 6, e1400. [Google Scholar]
- Del Buono, A.; D’orta, A.; Tarro, G.; Rossi, P.; Papa, S.; Iodice, L.; Abbadessa, A.; Montano, L.; Portale, G.; Berretta, M.; et al. Terra dei fuochi, the starting point. The role of prevention and complementary medicine in the clinical practice. WCRJ 2018, 5, e1112. [Google Scholar]
- Di Franco, R.; Borzillo, V.; Falivene, S.; Giugliano, F.M.; Cammarota, F.; Ametrano, G.; Muto, M.; Ravo, V.; Romano, F.J.; Rossetti, S.; et al. Radiosurgery of brain metastases with CyberKnife® system: Role of image. WCRJ 2017, 4, e987. [Google Scholar]
- Kumarappan, C.T.; Cini, M.J. In vitro cytotoxicity and in vivo acute oral toxicity evaluation of coptis chinensis aqueous extract. WCRJ 2021, 8, e1971. [Google Scholar]
- Ramezani, M.; Aalami Aleagha, Z.; Almasi, A.; Khazaei, S.; Oltulu, P.; Sadeghi, M. Expression of MSH-6 immunohistochemistry marker in colorectal cancer. WCRJ 2021, 8, e1989. [Google Scholar]
- Pialago, E.L.; Comuelo, R.E.; Tidon, D.; Guzman, J.P. Prognostic value of serum alpha fetoprotein response during pre-operative chemotherapy in hepatoblastoma: A meta-analysis. WCRJ 2021, 8, e1921. [Google Scholar]
- Viganò, L.; Bellini, D.; Caruso, F.; Mucllari, S.; Paglioli, E.; Tintori, L.; Viganò, V.; Taibi, R.; Casu, C. Multiple myeloma-oral radiological evidences. WCRJ 2021, 8, e1852. [Google Scholar]
- Licito, A.; Marotta, G.; Battaglia, M.; Ottaiano, M.P.; Morra, G.; De Lucia, V.; Daria, R.; Cafiero, C.; Blasio, G. Genotyping panel to assess Hand-Foot Syndrome in T2DM and cancer patients who receive concurrent Platin derivates and Biguanides. WCRJ 2020, 7, e1748. [Google Scholar]
- İnci, H.; İnci, F. Complementary and alternative medicine awareness in cancer patients receiving chemotherapy. WCRJ 2020, 7, e1752. [Google Scholar]
- Yang, H.; Yang, X.; Liu, H.; Long, H.; Hu, H.; Wang, Q.; Huang, R.; Shan, D.; Li, K.; Lai, W. Placebo modulation in orthodontic pain: A single-blind functional magnetic resonance study. Radiol. Med. 2021, 126, 1356–1365. [Google Scholar] [CrossRef]
- Burns, J.; Catanzano, T.M.; Schaefer, P.W.; Agarwal, V.; Kim, D.; Goiffon, R.J.; Jordan, S.G. Structured Reports and Radiology Residents: Friends or Foes? Acad. Radiol. 2020, 29, S43–S47. [Google Scholar] [CrossRef] [PubMed]
- Acgme. Diagnostic Radiology Milestones. 2019 The Accreditation Council for Graduate Medical Education. Available online: https://www.acgme.org/Portals/0/PDFs/Milestones/DiagnosticRadiologyMile-stones2.0.pdf?ver=2020-03-10-151835-740 (accessed on 6 June 2022).
- Shin, N.; Choi, J.A.; Choi, J.M.; Cho, E.S.; Kim, J.H.; Chung, J.J.; Yu, J.S. Sclerotic changes of cavernous hemangioma in the cirrhotic liver: Long-term follow-up using dynamic contrast-enhanced computed tomography. Radiol. Med. 2020, 125, 1225–1232. [Google Scholar] [CrossRef]
- Gabelloni, M.; Di Nasso, M.; Morganti, R.; Faggioni, L.; Masi, G.; Falcone, A.; Neri, E. Application of the ESR iGuide clinical decision support system to the imaging pathway of patients with hepatocellular carcinoma and cholangiocarcinoma: Preliminary findings. Radiol. Med. 2020, 125, 531–537. [Google Scholar] [CrossRef] [PubMed]
- Barabino, M.; Gurgitano, M.; Fochesato, C.; Angileri, S.A.; Franceschelli, G.; Santambrogio, R.; Mariani, N.M.; Opocher, E.; Carrafiello, G. LI-RADS to categorize liver nodules in patients at risk of HCC: Tool or a gadget in daily practice? Radiol. Med. 2021, 126, 5–13. [Google Scholar] [CrossRef] [PubMed]
- Schicchi, N.; Fogante, M.; Palumbo, P.; Agliata, G.; Esposto Pirani, P.; Di Cesare, E.; Giovagnoni, A. The sub-millisievert era in CTCA: The technical basis of the new radiation dose approach. Radiol. Med. 2020, 125, 1024–1039. [Google Scholar] [CrossRef] [PubMed]
- Rega, D.; Pace, U.; Scala, D.; Chiodini, P.; Granata, V.; Fares Bucci, A.; Pecori, B.; Delrio, P. Treatment of splenic flexure colon cancer: A comparison of three different surgical procedures: Experience of a high volume cancer center. Sci. Rep. 2019, 9, 10953. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fornell-Perez, R.; Vivas-Escalona, V.; Aranda-Sanchez, J.; Gonzalez-Dominguez, M.C.; Rubio-Garcia, J.; Aleman-Flores, P.; Lozano-Rodriguez, A.; Porcel-de-Peralta, G.; Loro-Ferrer, J.F. Primary and post-chemoradiotherapy MRI detection of extramural venous invasion in rectal cancer: The role of diffusion-weighted imaging. Radiol. Med. 2020, 125, 522–530. [Google Scholar] [CrossRef]
- Danti, G.; Berti, V.; Abenavoli, E.; Briganti, V.; Linguanti, F.; Mungai, F.; Pradella, S.; Miele, V. Diagnostic imaging of typical lung carcinoids: Relationship between MDCT, (111)In-Octreoscan and (18)F-FDG-PET imaging features with Ki-67 index. Radiol. Med. 2020, 125, 715–729. [Google Scholar] [CrossRef]
- Koc, A.; Sezgin, O.S.; Kayipmaz, S. Comparing different planimetric methods on volumetric estimations by using cone beam computed tomography. Radiol. Med. 2020, 125, 398–405. [Google Scholar] [CrossRef]
- Neri, E.; Miele, V.; Coppola, F.; Grassi, R. Use of CT and artificial intelligence in suspected or COVID-19 positive patients: Statement of the Italian Society of Medical and Interventional Radiology. Radiol. Med. 2020, 125, 505–508. [Google Scholar] [CrossRef]
- Farchione, A.; Larici, A.R.; Masciocchi, C.; Cicchetti, G.; Congedo, M.T.; Franchi, P.; Gatta, R.; Lo Cicero, S.; Valentini, V.; Bonomo, L.; et al. Exploring technical issues in personalized medicine: NSCLC survival prediction by quantitative image analysis-usefulness of density correction of volumetric CT data. Radiol. Med. 2020, 125, 625–635. [Google Scholar] [CrossRef]
- Hu, H.T.; Shan, Q.Y.; Chen, S.L.; Li, B.; Feng, S.T.; Xu, E.J.; Li, X.; Long, J.Y.; Xie, X.Y.; Lu, M.D.; et al. CT-based radiomics for preoperative prediction of early recurrent hepatocellular carcinoma: Technical reproducibility of acquisition and scanners. Radiol. Med. 2020, 125, 697–705. [Google Scholar] [CrossRef]
- Granata, V.; Fusco, R.; Avallone, A.; De Stefano, A.; Ottaiano, A.; Sbordone, C.; Brunese, L.; Izzo, F.; Petrillo, A. Radiomics-Derived Data by Contrast Enhanced Magnetic Resonance in RAS Mutations Detection in Colorectal Liver Metastases. Cancers 2021, 13, 453. [Google Scholar] [CrossRef] [PubMed]
- Granata, V.; Fusco, R.; Risi, C.; Ottaiano, A.; Avallone, A.; De Stefano, A.; Grimm, R.; Grassi, R.; Brunese, L.; Izzo, F.; et al. Diffusion-Weighted MRI and Diffusion Kurtosis Imaging to Detect RAS Mutation in Colorectal Liver Metastasis. Cancers 2020, 12, 2420. [Google Scholar] [CrossRef] [PubMed]
- Granata, V.; Fusco, R.; De Muzio, F.; Cutolo, C.; Setola, S.V.; Dell’Aversana, F.; Belli, A.; Romano, C.; Ottaiano, A.; Nasti, G.; et al. Magnetic Resonance Features of Liver Mucinous Colorectal Metastases: What the Radiologist Should Know. J. Clin. Med. 2022, 11, 2221. [Google Scholar] [CrossRef] [PubMed]
- Cutolo, C.; Dell’Aversana, F.; Fusco, R.; Grazzini, G.; Chiti, G.; Simonetti, I.; Bruno, F.; Palumbo, P.; Pierpaoli, L.; Valeri, T.; et al. Combined Hepatocellular-Cholangiocarcinoma: What the Multidisciplinary Team Should Know. Diagnostics 2022, 12, 890. [Google Scholar] [CrossRef] [PubMed]
- Mildenberger, P. Strukturierte Befundung in der Radiologie: IT-Essentials [Structured reporting in radiology: IT essentials]. Radiologe 2021, 61, 995–998. [Google Scholar] [CrossRef]
- Ganeshan, D.; Duong, P.T.; Probyn, L.; Lenchik, L.; McArthur, T.A.; Retrouvey, M.; Ghobadi, E.H.; Desouches, S.L.; Pastel, D.; Francis, I.R. Structured Reporting in Radiology. Acad. Radiol. 2018, 25, 66–73. [Google Scholar] [CrossRef]
- Kohli, A.; Castillo, S.; Thakur, U.; Chhabra, A. Structured Reporting in Musculoskeletal Radiology. Semin. Musculoskelet. Radiol. 2021, 25, 641–645. [Google Scholar] [CrossRef]
- Radiological Society of North America Informatics Reporting. MR Brain Template. Available online: http://www.radreport.org/txt-mrrt/0000045 (accessed on 6 June 2022).
- Boland, G.W.; Duszak, R., Jr. Structured reporting and communication. J. Am. Coll. Radiol. 2015, 12, 1286–1288. [Google Scholar] [CrossRef]
- Nobel, J.M.; Kok, E.M.; Robben, S.G.F. Redefining the structure of structured reporting in radiology. Insights Imaging 2020, 11, 10. [Google Scholar] [CrossRef] [Green Version]
- Sun, J.; Li, H.; Gao, J.; Li, J.; Li, M.; Zhou, Z.; Peng, Y. Performance evaluation of a deep learning image reconstruction (DLIR) algorithm in “double low” chest CTA in children: A feasibility study. Radiol. Med. 2021, 126, 1181–1188. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Granata, V.; De Muzio, F.; Cutolo, C.; Dell’Aversana, F.; Grassi, F.; Grassi, R.; Simonetti, I.; Bruno, F.; Palumbo, P.; Chiti, G.; et al. Structured Reporting in Radiological Settings: Pitfalls and Perspectives. J. Pers. Med. 2022, 12, 1344. https://doi.org/10.3390/jpm12081344
Granata V, De Muzio F, Cutolo C, Dell’Aversana F, Grassi F, Grassi R, Simonetti I, Bruno F, Palumbo P, Chiti G, et al. Structured Reporting in Radiological Settings: Pitfalls and Perspectives. Journal of Personalized Medicine. 2022; 12(8):1344. https://doi.org/10.3390/jpm12081344
Chicago/Turabian StyleGranata, Vincenza, Federica De Muzio, Carmen Cutolo, Federica Dell’Aversana, Francesca Grassi, Roberta Grassi, Igino Simonetti, Federico Bruno, Pierpaolo Palumbo, Giuditta Chiti, and et al. 2022. "Structured Reporting in Radiological Settings: Pitfalls and Perspectives" Journal of Personalized Medicine 12, no. 8: 1344. https://doi.org/10.3390/jpm12081344
APA StyleGranata, V., De Muzio, F., Cutolo, C., Dell’Aversana, F., Grassi, F., Grassi, R., Simonetti, I., Bruno, F., Palumbo, P., Chiti, G., Danti, G., & Fusco, R. (2022). Structured Reporting in Radiological Settings: Pitfalls and Perspectives. Journal of Personalized Medicine, 12(8), 1344. https://doi.org/10.3390/jpm12081344






