A TKA Insert with A Lateral Flat Articular Surface Maximizes External and Internal Tibial Orientations without Anterior Lift-Off Relative to Low- and Ultracongruent Surfaces
Abstract
:1. Introduction
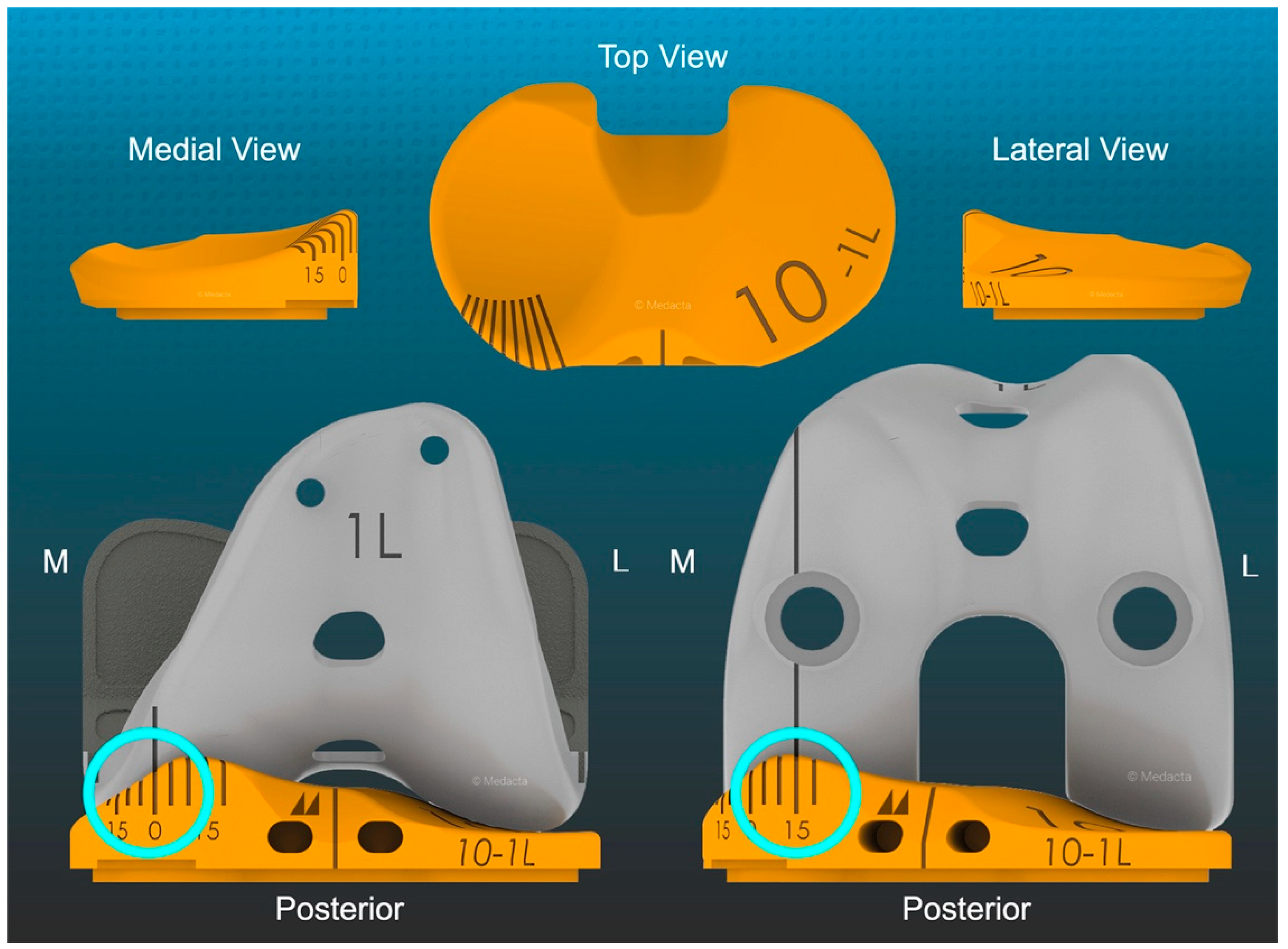
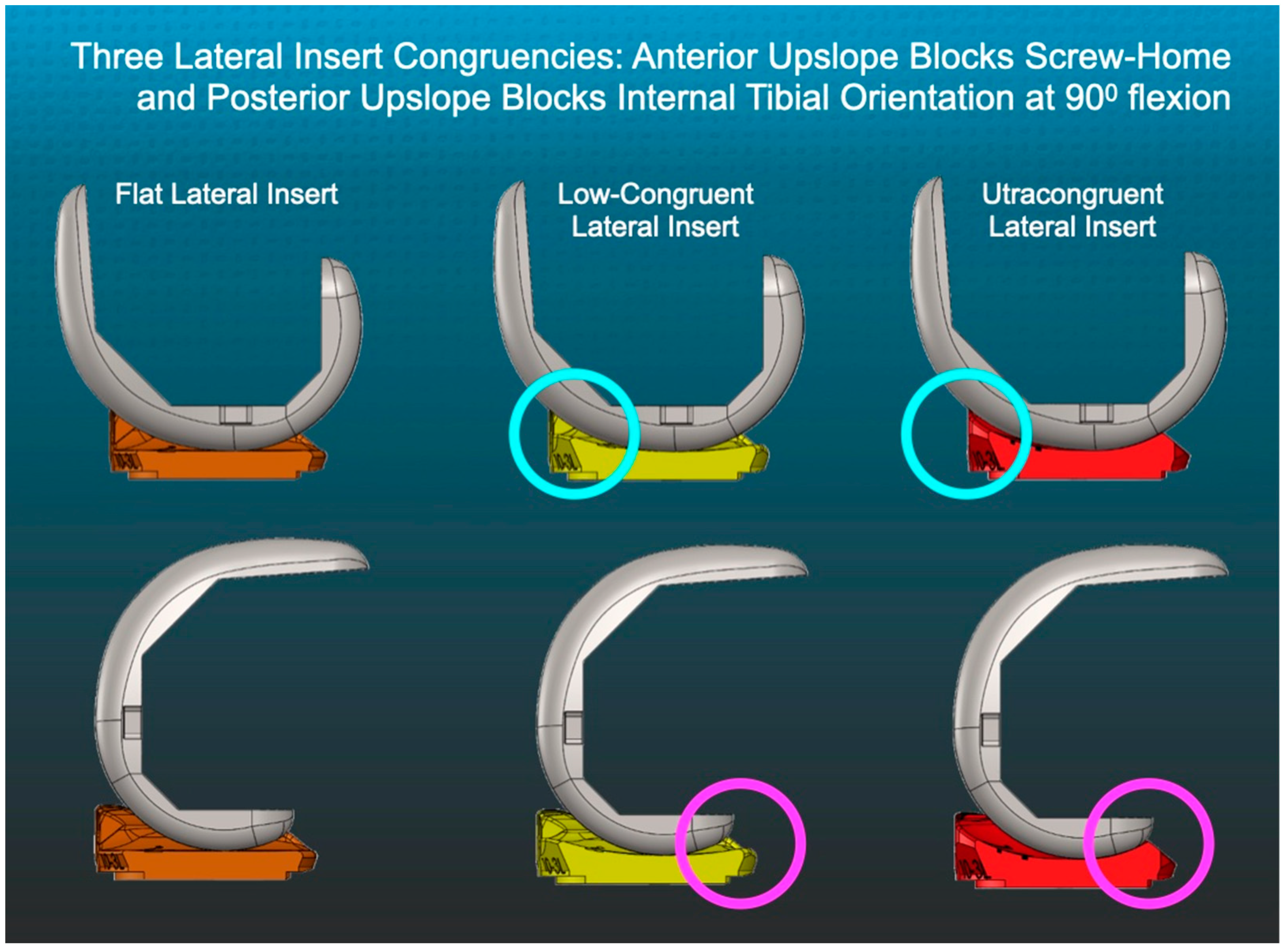
2. Materials and Methods
2.1. Overview of Unrestricted Caliper-Verified KA Technique and Accuracy Analysis of Component Placement
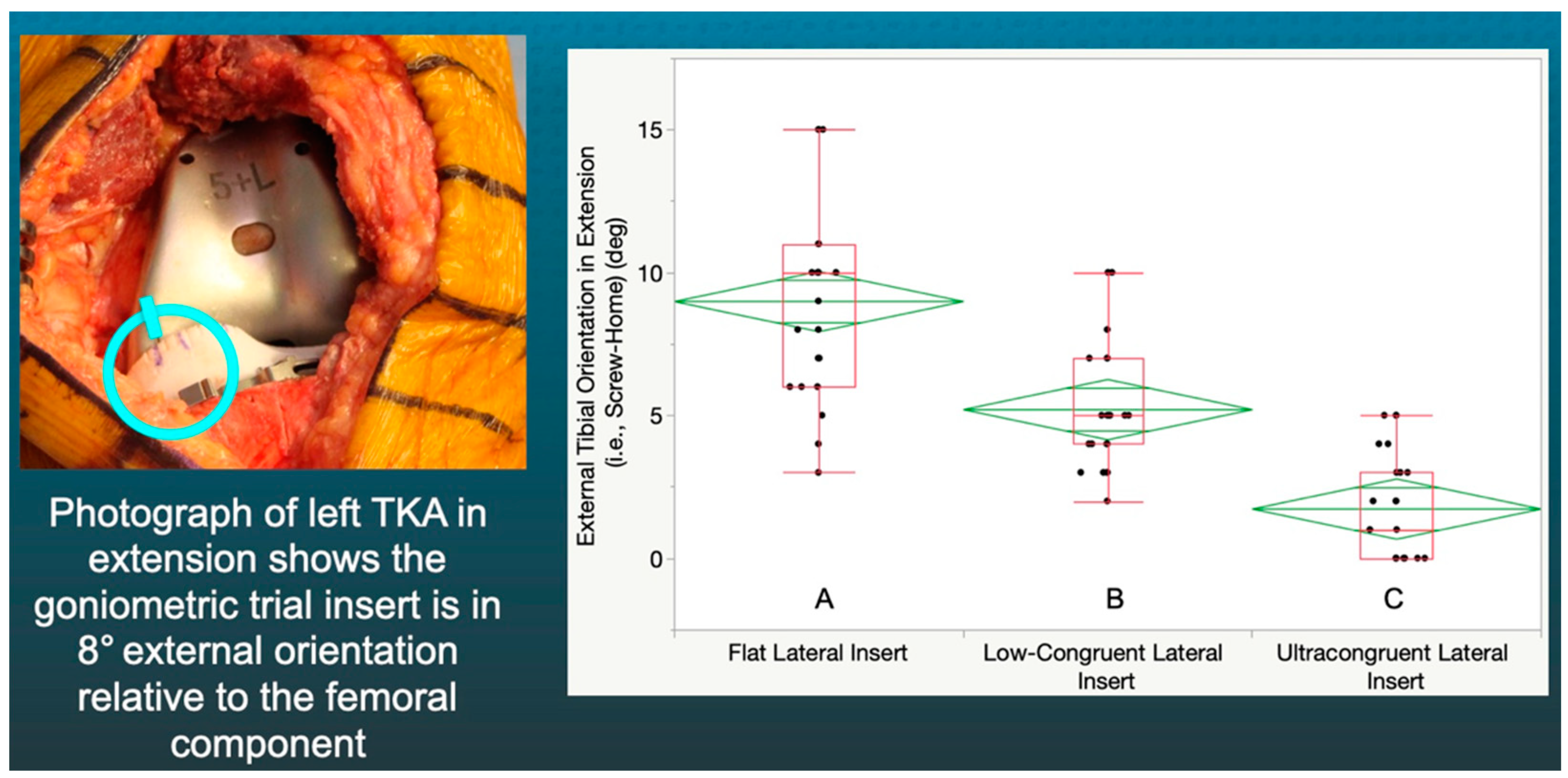
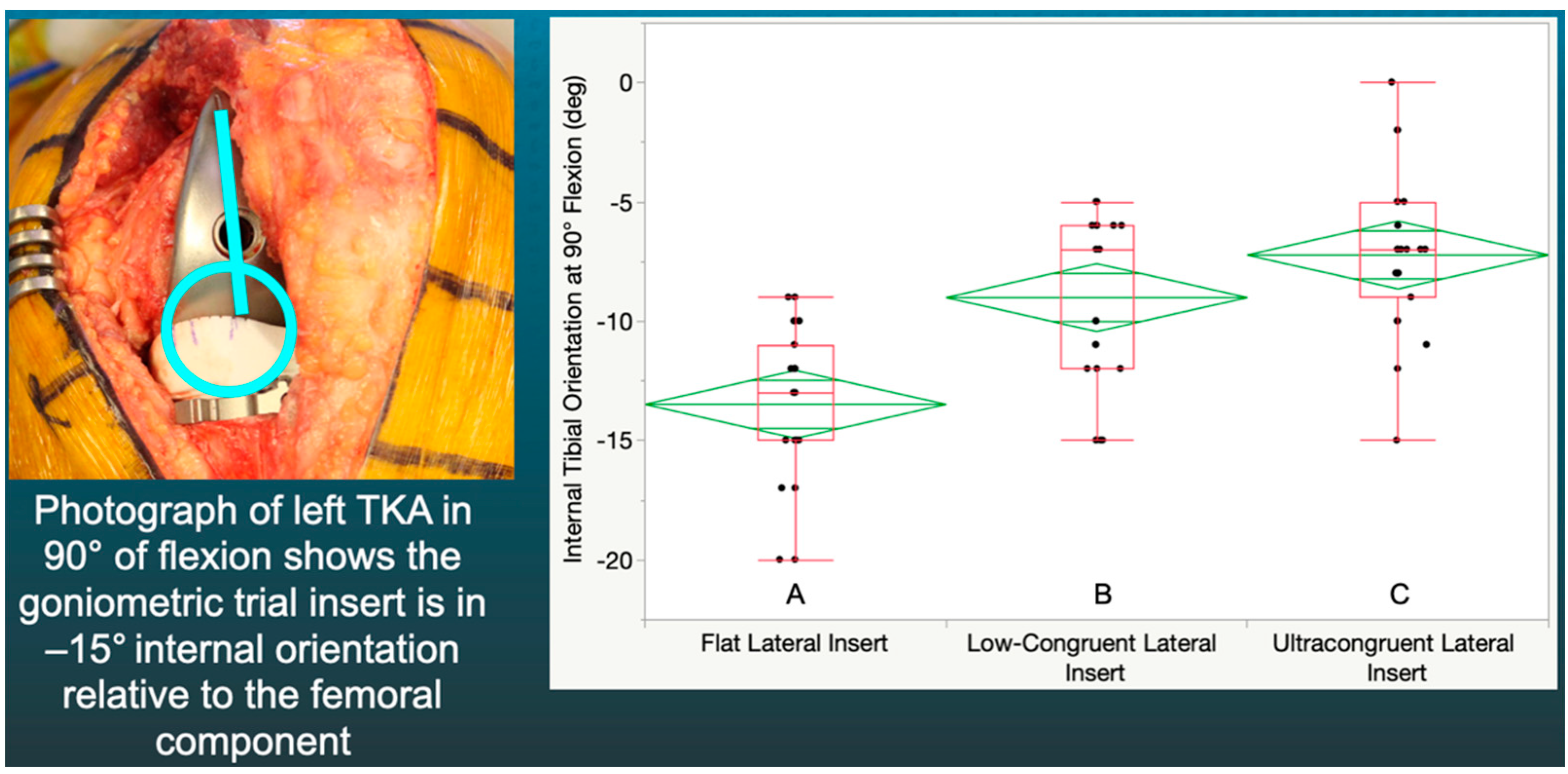
2.2. Method for Measuring the Orientation of the Tibia and Recording Anterior Lift-off of the Trial Insert
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Putame, G.; Terzini, M.; Rivera, F.; Kebbach, M.; Bader, R.; Bignardi, C. Kinematics and kinetics comparison of ultra-congruent versus medial-pivot designs for total knee arthroplasty by multibody analysis. Sci. Rep. 2022, 12, 3052. [Google Scholar] [CrossRef]
- Freeman, M.A.R.; Pinskerova, V. The Movement of the Knee Studied by Magnetic Resonance Imaging. Clin. Orthop. Relat. Res. 2003, 410, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Freeman, M.; Pinskerova, V. The movement of the normal tibio-femoral joint. J. Biomech. 2005, 38, 197–208. [Google Scholar] [CrossRef] [PubMed]
- Pinskerova, V.; Samuelson, K.M.; Stammers, J.; Maruthainar, K.; Sosna, A.; Freeman, M.A.R. The knee in full flexion. J. Bone Jt. Surgery. Br. Vol. 2009, 91, 830–834. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- French, S.R.; Munir, S.; Brighton, R. A Single Surgeon Series Comparing the Outcomes of a Cruciate Retaining and Medially Stabilized Total Knee Arthroplasty Using Kinematic Alignment Principles. J. Arthroplast. 2020, 35, 422–428. [Google Scholar] [CrossRef]
- Gray, H.A.; Guan, S.; Young, T.J.; Dowsey, M.M.; Choong, P.F.; Pandy, M.G. Comparison of posterior--stabilized, cruciate--retaining, and medial--stabilized knee implant motion during gait. J. Orthop. Res. 2020, 38, 1753–1768. [Google Scholar] [CrossRef] [PubMed]
- Schütz, P.; Taylor, W.R.; Postolka, B.; Fucentese, S.F.; Koch, P.P.; Freeman, M.A.; Pinskerova, V.; List, R. Kinematic Evaluation of the GMK Sphere Implant during Gait Activities: A Dynamic Videofluoroscopy Study. J. Orthop. Res. 2019, 37, 2337–2347. [Google Scholar] [CrossRef] [Green Version]
- Scott, D.F.; Gray, C.G. Outcomes are Better with a Medial-Stabilized vs a Posterior-Stabilized Total Knee Implanted With Kinematic Alignment. J. Arthroplast. 2022, 37, S852–S858. [Google Scholar] [CrossRef]
- Nedopil, A.J.; Howell, S.M.; Hull, M.L. More passive internal tibial rotation with posterior cruciate ligament retention than with excision in a medial pivot TKA implanted with unrestricted caliper verified kinematic alignment. Knee Surg. Sports Traumatol. Arthrosc. 2021, 1–9. [Google Scholar] [CrossRef]
- Nedopil, A.J.; Thadani, P.J.; McCoy, T.H.; Howell, S.M.; Hull, M.L. Adjusting Insert Thickness and Tibial Slope Do Not Correct Internal Tibial Rotation Loss Caused by PCL Resection: In Vitro Study of a Medial Constraint TKA Implanted with Unrestricted Calipered Kinematic Alignment. J. Knee Surg. 2021. [Google Scholar] [CrossRef]
- Fukubayashi, T.; Torzilli, P.A.; Sherman, M.F.; Warren, R.F. An in vitro biomechanical evaluation of anterior-posterior motion of the knee. Tibial displacement, rotation, and torque. J. Bone Jt. Surg. 1982, 64, 258–264. [Google Scholar] [CrossRef]
- Li, G.; Gill, T.J.; DeFrate, L.E.; Zayontz, S.; Glatt, V.; Zarins, B. Biomechanical consequences of PCL deficiency in the knee under simulated muscle loads—an in vitro experimental study. J. Orthop. Res. 2002, 20, 887–892. [Google Scholar] [CrossRef]
- Nedopil, A.J.; Shekhar, A.; Howell, S.M.; Hull, M.L. An insert with less than spherical medial congruency causes a loss of passive internal rotation after calipered kinematically aligned TKA. Arch. Orthop. Trauma. Surg. 2021, 141, 2287–2294. [Google Scholar] [CrossRef] [PubMed]
- Howell, S.M.; Nedopil, A.J.; Hull, M.L. Negligible effect of surgeon experience on the accuracy and time to perform unrestricted caliper verified kinematically aligned TKA with manual instruments. Knee Surg. Sports Traumatol. Arthrosc. 2022, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Nedopil, A.J.; Dhaliwal, A.; Howell, S.M.; Hull, M.L. A Surgeon That Switched to Unrestricted Kinematic Alignment with Manual Instruments Has a Short Learning Curve and Comparable Resection Accuracy and Outcomes to Those of an Experienced Surgeon. J. Pers. Med. 2022, 12, 1152. [Google Scholar] [CrossRef]
- Howell, S.M.; Shelton, T.J.; Gill, M.; Hull, M.L. A cruciate-retaining implant can treat both knees of most windswept deformities when performed with calipered kinematically aligned TKA. Knee Surg. Sports Traumatol. Arthrosc. 2020, 29, 437–445. [Google Scholar] [CrossRef]
- Nam, D.; Lin, K.M.; Howell, S.M.; Hull, M.L. Femoral bone and cartilage wear is predictable at 0° and 90° in the osteoarthritic knee treated with total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 2975–2981. [Google Scholar] [CrossRef]
- Nedopil, A.J.; Howell, S.M.; Hull, M.L. Deviations in femoral joint lines using calipered kinematically aligned TKA from virtually planned joint lines are small and do not affect clinical outcomes. Knee Surg. Sports Traumatol. Arthrosc. 2019, 28, 3118–3127. [Google Scholar] [CrossRef] [PubMed]
- Nedopil, A.J.; Singh, A.K.; Howell, S.M.; Hull, M.L. Does Calipered Kinematically Aligned TKA Restore Native Left to Right Symmetry of the Lower Limb and Improve Function? J. Arthroplast. 2018, 33, 398–406. [Google Scholar] [CrossRef]
- Nedopil, A.J.; Howell, S.; Hull, M.L. Does Malrotation of the Tibial and Femoral Components Compromise Function in Kinematically Aligned Total Knee Arthroplasty? Orthop. Clin. N. Am. 2016, 47, 41–50. [Google Scholar] [CrossRef]
- Howell, S.M.; Gill, M.; Shelton, T.J.; Nedopil, A.J. Reoperations are few and confined to the most valgus phenotypes 4 years after unrestricted calipered kinematically aligned TKA. Knee Surg. Sports Traumatol. Arthrosc. 2021, 30, 948–957. [Google Scholar] [CrossRef] [PubMed]
- Roth, J.D.; Howell, S.M.; Hull, M.L. Kinematically aligned total knee arthroplasty limits high tibial forces, differences in tibial forces between compartments, and abnormal tibial contact kinematics during passive flexion. Knee Surg. Sports Traumatol. Arthrosc. 2017, 26, 1589–1601. [Google Scholar] [CrossRef] [PubMed]
- Shelton, T.J.; Howell, S.M.; Hull, M.L. Is There a Force Target That Predicts Early Patient-reported Outcomes After Kinematically Aligned TKA? Clin. Orthop. Relat. Res. 2018, 477, 1200–1207. [Google Scholar] [CrossRef]
- Shelton, T.; Nedopil, A.J.; Howell, S.M.; Hull, M.L. Do varus or valgus outliers have higher forces in the medial or lateral compartments than those which are in-range after a kinematically aligned total knee arthroplasty? Bone Jt. J. 2017, 99, 1319–1328. [Google Scholar] [CrossRef]
- Johnson, J.M.; Mahfouz, M.R.; Midillioğlu, M.R.; Nedopil, A.J.; Howell, S.M. Three-dimensional analysis of the tibial resection plane relative to the arthritic tibial plateau in total knee arthroplasty. J. Exp. Orthop. 2017, 4, 27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nedopil, A.J.; Zamora, T.; Shelton, T.; Howell, S.M.; Hull, M. A Best-Fit of an Anatomic Tibial Baseplate Closely Parallels the Flexion-Extension Plane and Covers a High Percentage of the Proximal Tibia. J. Knee Surg. 2020, 34, 1486–1494. [Google Scholar] [CrossRef] [PubMed]
- Roth, J.D.; Howell, S.M.; Hull, M.L. Native Knee Laxities at 0°, 45°, and 90° of Flexion and Their Relationship to the Goal of the Gap-Balancing Alignment Method of Total Knee Arthroplasty. J. Bone Jt. Surg. 2015, 97, 1678–1684. [Google Scholar] [CrossRef] [PubMed]
- Indrayan, A. Methods of Clinical Epidemiology. In Springer Series on Epidemiology and Public Health; Springer: Berlin/Heidelberg, Germany, 2013; p. 24. [Google Scholar]
- Zhang, L.-K.; Wang, X.-M.; Niu, Y.-Z.; Liu, H.-X.; Wang, F. Relationship between Patellar Tracking and the “Screw-home” Mechanism of Tibiofemoral Joint. Orthop. Surg. 2016, 8, 490–495. [Google Scholar] [CrossRef]
- Freedman, B.R.; Brindle, T.J.; Sheehan, F.T. Re-evaluating the functional implications of the Q-angle and its relationship to in-vivo patellofemoral kinematics. Clin. Biomech. 2014, 29, 1139–1145. [Google Scholar] [CrossRef] [Green Version]
- Wada, K.; Hamada, D.; Takasago, T.; Nitta, A.; Goto, T.; Tonogai, I.; Tsuruo, Y.; Sairyo, K. Native rotational knee kinematics is restored after lateral UKA but not after medial UKA. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 3438–3443. [Google Scholar] [CrossRef]
- Scott, R.D.; Chmell, M.J. Balancing the Posterior Cruciate Ligament During Cruciate-Retaining Fixed and Mobile-Bearing Total Knee Arthroplasty: Description of the Pull-Out Lift-Off and Slide-Back Tests. J. Arthroplast. 2008, 23, 605–608. [Google Scholar] [CrossRef] [PubMed]
- Kayani, B.; Konan, S.; Horriat, S.; Ibrahim, M.S.; Haddad, F.S. Posterior cruciate ligament resection in total knee arthroplasty: The effect on flexion-extension gaps, mediolateral laxity, and fixed flexion deformity. Bone Jt. J. 2019, 101, 1230–1237. [Google Scholar] [CrossRef] [PubMed]
- Scott, G.; Imam, M.A.; Eifert, A.; Freeman, M.; Pinskerova, V.; Field, R.; Skinner, J.; Banks, S.A. Can a total knee arthroplasty be both rotationally unconstrained and anteroposteriorly stabilised? A pulsed fluoroscopic investigation. Bone Jt. Res. 2016, 5, 80–86. [Google Scholar] [CrossRef] [PubMed]
| Preoperative Characteristics | Values ± SD (Range) |
|---|---|
| Age | 68 ± 10 years (48 to 89) |
| Sex | 9 females, 14 males |
| Body mass index | 30 ± 5 kg/m2 (22 to 42) |
| Extension | 7 ± 7° (0 to 24°) |
| Flexion | 112 ± 8° (90 to 130°) |
| The compartment in which osteoarthritis predominated | 74% medial, 22% lateral, 4% patellofemoral |
| Radiographic knee deformity (+varus, –valgus) | −1 ± 7° (14 to −17) |
| Kellgren–Lawrence classification | 10% II, 50% III, 40% IV |
| Oxford Knee Score (48 is best, 0 is worst) | 19 ± 6 points (7 to 28) |
| Knee Society Score (100 is best, 0 is worst) | 35 ± 17 points (0 to 73) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nedopil, A.J.; Howell, S.M.; Hull, M.L. A TKA Insert with A Lateral Flat Articular Surface Maximizes External and Internal Tibial Orientations without Anterior Lift-Off Relative to Low- and Ultracongruent Surfaces. J. Pers. Med. 2022, 12, 1274. https://doi.org/10.3390/jpm12081274
Nedopil AJ, Howell SM, Hull ML. A TKA Insert with A Lateral Flat Articular Surface Maximizes External and Internal Tibial Orientations without Anterior Lift-Off Relative to Low- and Ultracongruent Surfaces. Journal of Personalized Medicine. 2022; 12(8):1274. https://doi.org/10.3390/jpm12081274
Chicago/Turabian StyleNedopil, Alexander J., Stephen M. Howell, and Maury L. Hull. 2022. "A TKA Insert with A Lateral Flat Articular Surface Maximizes External and Internal Tibial Orientations without Anterior Lift-Off Relative to Low- and Ultracongruent Surfaces" Journal of Personalized Medicine 12, no. 8: 1274. https://doi.org/10.3390/jpm12081274
APA StyleNedopil, A. J., Howell, S. M., & Hull, M. L. (2022). A TKA Insert with A Lateral Flat Articular Surface Maximizes External and Internal Tibial Orientations without Anterior Lift-Off Relative to Low- and Ultracongruent Surfaces. Journal of Personalized Medicine, 12(8), 1274. https://doi.org/10.3390/jpm12081274








