A Systematic Review of the Effectiveness of Virtual Reality-Based Interventions on Pain and Range of Joint Movement Associated with Burn Injuries
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Search Strategy
2.3. Eligibility Criteria
- Type of participants: subjects with burns in any part of their body showing decreased range of joint movement and pain on rehabilitation. No age range or gender was limited.
- Type of intervention: virtual-reality interventions with or without additional or complementary treatment.
- Study type: randomized controlled trials, quasi-experimental studies, studies with experimental and control groups and clinical studies. The language of the studies was established as English or Spanish. Due to the specificity of the topic and the lack of related scientific production, the date of publication was not limited in the searches.
- Outcome measures: pain and range of joint movement.
- Meta-analyses, studies with less than two treatment sessions, study protocols, and qualitative descriptions.
- Studies with only one participant.
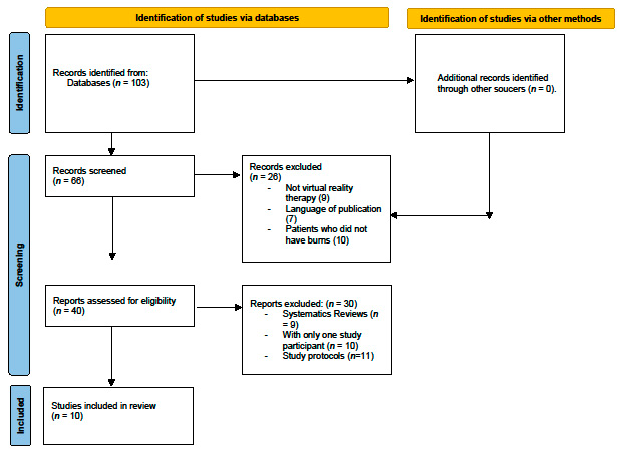
2.4. Selection of Studies
2.5. Methodological Quality Analysis
2.6. Risk of Bias Analysis
3. Results
3.1. Sociodemographic Characteristics
3.2. Methodology of the Studies
3.2.1. Interventions
3.2.2. Professionals
3.2.3. Outcome Measures and Assessment Tools
3.3. Results of the Studies
3.4. Methodological Quality of the Included Studies
3.5. Risk of Bias
4. Discussion
4.1. Virtual Reality and Pain
4.2. Virtual Reality and Range of Movement
4.3. Limitations of the Study
4.4. Implications for Clinical Practice
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Aldana, M.C.d.R.; Castellanos, L.F.; Osorio, L.Q.; Navarrete, N. Burns in the Colombian pediatric population: From ignorance to prevention. Pediatrics 2016, 49, 128–137. [Google Scholar] [CrossRef] [Green Version]
- Sánchez Correa, F.; Menchaca, P.; Gloria Rostion, C. Initial management of the burned child: What the general practitioner should know. Rev. Pediatr. Electron. 2014, 11. [Google Scholar]
- Lahoz Sánchez, M.P.; Marco Sanz, C. Role of the occupational therapist in the treatment of the burn patient: A bibliographic review: The role of the occupational therapist in burn treatment: A bibliographic review. TOG 2019, 16, 60–68. Available online: https://www.revistatog.es/ojs/index.php/tog/article/view/11 (accessed on 14 March 2022).
- Chouza-Ínsua, M.; Vázquez, M.E.A. Kinesitherapy in the rehabilitation of the burn patient. Proy. Lumbre Multidiscip. J. Acute Cutan. Insuffic. 2013, 41–46. Available online: https://dialnet.unirioja.es/servlet/articulo?codigo=4332594 (accessed on 2 May 2022).
- Jimenez, I.F.; García, E.M.; González, F.S. Burns in childhood. Assessment and treatment. Bol. Pediatr. 2011, 41, 99–105. [Google Scholar]
- Arriagada, C. Multidisciplinary management of severe burns. Clin. Condes Med. J. 2016, 27, 38–41. [Google Scholar]
- WHO: World Health Organization. Available online: https://www.who.int/es/news-room/fact-sheets/detail/burns (accessed on 30 April 2022).
- Scapin, S.; Echevarria-Guanilo, M.E.; Junior, P.R.B.F.; Gonçalves, N.; Rocha, P.K.; Coimbra, R. Virtual Reality in the treatment of burn patients: A systematic review. Burns 2018, 44, 1403–1416. [Google Scholar] [CrossRef]
- Shahrbanian, S.; Ma, X.; Aghaei, N.; Korner-Bitensky, N.; Moshiri, K.; Simmonds, M.J. Use of virtual reality (immersive vs. non immersive) for pain management in children and adults: A systematic review of evidence from randomized controlled trials. Eur. J. Exp. Biol. 2012, 2, 1408–1422. [Google Scholar]
- Killç, A.; Brown, A.; Aras, I.; Hare, J.; Hughes, L.D.; Mccracken, L.M. Using Virtual Technology for Fear of Medical Procedures: A Systematic Review of the Effectiveness of Virtual Reality-Based Interventions. Ann. Behav. Med. 2021, 55, 1062–1079. [Google Scholar] [CrossRef] [PubMed]
- Ali, R.R.; Selim, A.O.; Ghafar, M.A.A.; Abdelraouf, O.R.; Ali, O.I. Virtual reality as a pain distractor during physical rehabilitation in pediatric burns. Burns 2022, 48, 303–308. [Google Scholar] [CrossRef]
- Adamovich, S.V.; Fluet, G.G.; Tunik, E.; Merians, A.S. Sensorimotor training in virtual reality: A review. NeuroRehabilitation 2009, 25, 29–44. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pereira, E.M.; Rueda, F.M.; Diego, I.A.; De La Cuerda, R.C.; De Mauro, A.; Page, J.M. Use of virtual reality systems as a proprioception method in cerebral palsy: Clinical practice guideline. Neurology 2014, 29, 550–559. [Google Scholar]
- Peñasco-Martin, B.; de los Reyes-Guzman, A.; Gil-Agudo, Á.; Bernal-Sahún, A.; Perez-Aguilar, B.; de la Peña-Gonzalez, A.I. Application of virtual reality in the motor aspects of neurorehabilitation. Rev. Neurol. 2010, 51, 481–488. [Google Scholar] [PubMed]
- Pardo, G.D.; Garcia, I.M. Virtual reality-based intervention program for pediatric burns. Annu. Clin. Health Psychol. 2013, 9, 49–51. [Google Scholar]
- Hoffman, H.G.; Patterson, D.R.; Carrougher, G.J.; Sharar, S.R. Effectiveness of virtual reality-based pain control with multiple treatments. Clin. J. Pain 2001, 17, 229–235. [Google Scholar] [CrossRef]
- Fa Kamel, F.; Maged, M. Effects of Virtual Reality and Task-Oriented Training on Hand Function and Activity Performance in Pediatric Hand Burns: A Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2021, 102, 1059–1066. [Google Scholar] [CrossRef]
- Malloy, K.M.; Milling, L.S. The effectiveness of virtual reality distraction for pain reduction: A systematic review. Clin. Psychol. Rev. 2010, 30, 1011–1018. [Google Scholar] [CrossRef]
- Morris, L.D.; Louw, Q.A.; Grimmer-Somers, K. The effectiveness of virtual reality on reducing pain and anxiety in burn injury patients: A systematic review. Clin. J. Pain 2009, 25, 815–826. [Google Scholar] [CrossRef] [PubMed]
- Yohannan, S.K.; Tufaro, P.A.; Hunter, H.; Orleman, L.; Palmatier, S.; Sang, C.; Gorga, D.I.; Yurt, R.W. The utilization of Nintendo® Wii™ during burn rehabilitation: A pilot study. J. Burn. Care Res. 2012, 33, 36–45. [Google Scholar] [CrossRef] [PubMed]
- Eijlers, R.; Utens, E.M.W.J.; Staals, L.M.; de Nijs, P.F.A.; Berghmans, J.; Wijnen, R.M.H.; Hillegers, M.H.J.; Dierckx, B.; Legerstee, J.S. Systematic Review and Meta-analysis of Virtual Reality in Paediatrics: Effects on Pain and Anxiety. Anesth. Analg. 2019, 129, 1344–1353. [Google Scholar] [CrossRef]
- PEDro Scale. Available online: https://pedro.org.au/spanish/resources/pedro-scale/ (accessed on 21 March 2021).
- Higgins, J.P.T.; Altman, D.G.; Sterne, J.A.C. Chapter 8: Assessing risk of bias in included studies. In Cochrane Handbook of Systematic Review of Interventions; Version 510; Higgins, J.P.T., Green, S., Eds.; The Cochrane Collaboration: London, UK, 2011; Available online: http://handbook-5-1.cochrane.org/ (accessed on 14 April 2021).
- Lozano, E.I.; Potterton, J.L. The use of Xbox KinectTM in a Paediatric Burns Unit. South Afr. J. Physiother. 2018, 74, 1–7. [Google Scholar]
- Soltani, M.; Drever, S.A.; Hoffman, H.G.; Sharar, S.R.; Wiechman, S.A.; Jensen, M.P.; Patterson, D.R. Virtual reality analgesia for burn joint flexibility: A randomized controlled trial. Rehabil. Psychol. 2018, 63, 487. [Google Scholar] [CrossRef]
- Carrougher, G.J.; Hoffman, H.G.; Nakamura, D.; Lezotte, D.; Soltani, M.; Leahy, L.; Engrav, L.H.; Patterson, D.R. The effect of virtual reality on pain and range of motion in adults with burn injuries. J. Burn. Care Res. 2009, 30, 785–791. [Google Scholar] [CrossRef] [PubMed]
- Faber, A.W.; Patterson, D.R.; Bremer, M. Repeated use of immersive virtual reality therapy to control pain during wound dressing changes in pediatric and adult burn patients. J. Burn. Care Res. 2013, 34, 563–568. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hoffman, H.G.; Rodriguez, R.A.; Gonzalez, M.; Bernardy, M.; Peña, R.; Beck, W.; Patterson, D.R.; Meyer, W.J.I. Immersive virtual reality as an adjunctive non-opioid analgesic for pre-dominantly Latin American children with large severe burn wounds during burn wound cleaning in the intensive care unit: A pilot study. Front. Hum. Neurosci. 2019, 13, 262. [Google Scholar] [CrossRef] [Green Version]
- Schmitt, Y.S.; Hoffman, H.G.; Blough, D.K.; Patterson, D.R.; Jensen, M.P.; Soltani, M.; Carrougher, G.J.; Nakamura, D.; Sharar, S.R. A randomized, controlled trial of immersive virtual reality analgesia, during physical therapy for pediatric burns. Burns 2011, 37, 61–68. [Google Scholar] [CrossRef] [Green Version]
- Lee, S.Y.; Cha, J.Y.; Yoo, J.W.; Nazareno, M.; Cho, Y.S.; Joo, S.Y.; Seo, C.H. Effect of the Application of Virtual Reality on Pain Reduction and Cerebral Blood Flow in Robot-Assisted Gait Training in Burn Patients. J. Clin. Med. 2022, 11, 3762. [Google Scholar] [CrossRef]
- Radwan, N.L.; Ibrahim, M.M.; Mahmoud, W.S. Effect of Wii-habilitation on spatiotemporal parameters and upper limb function post-burn in children. Burns 2021, 47, 828–837. [Google Scholar] [CrossRef]
- Tadín, M.A. Comparative analysis of the various types of burns seen in the emergency department. RqR Community Nurs. Rev. Seapa 2018, 68, 10. [Google Scholar]
- Castellanos Ruiz, J.; Pinzón Bernal, M.Y. Physiotherapeutic management of pain in burn patients in the three phases of recovery: Systematic review. J. Span. Pain Soc. 2016, 23, 202–210. [Google Scholar]
- Diaz, E.; Fernandez, S.; Rivera, C. ViRtualízate: Un programa de Realidad Virtual (RV) para personas mayores. Calidad 2019, 21, 7–13. [Google Scholar]
- Sharar, S.R.; Carrougher, G.J.; Nakamura, D.; Hoffman, H.G.; Blough, D.K.; Patterson, D.R. Factors influencing the efficacy of virtual reality distraction analgesia during postburn physical therapy: Preliminary results from 3 ongoing studies. Arch. Phys. Med. Rehabil. 2007, 88, S43–S49. [Google Scholar] [CrossRef] [PubMed]
- Maani, C.V.; Hoffman, H.G.; Morrow, M.; Maiers, A.; Gaylord, K.; McGhee, L.L.; DeSocio, P.A. Virtual reality pain control during burn wound debridement of combat-related burn injuries using robot-like arm mounted VR goggles. J. Trauma 2011, 71, S125. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, M.; Ko, M.; Oh, S.-W.; Lee, J.-Y.; Ham, Y.; Yi, H.; Choi, Y.; Ha, D.; Shin, J.-H. Effects of virtual reality-based planar motion exercises on upper extremity function, range of motion, and health-related quality of life: A multicenter, single-blinded, randomized, controlled pilot study. J. Neuroeng. Rehabil. 2019, 16, 122. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cuervo, C.C.; Alonso, P.S. Use of methods versus pain during venipuncture in children. Nure Inv. 2016, 13, 7. [Google Scholar]
- Hoyos, K.C.; López, G.C.; Maldonado, J.G.; Esquivel, F.R.; Villalobos, G.T. Clinical use of virtual reality for distraction and reduction of postoperative pain in adult patients. Rev. Tesis Psicológica 2015, 10, 38–50. [Google Scholar]
- Crespo, M.D.M.I.; Martí, L.S. Effectiveness of immersive virtual reality in pain management of the burn patient: A systematic review. J. MOVE Ther. Sci. 2020, 2, 160–171. [Google Scholar]
- Morris, L.D.; Louw, Q.A.; Crous, L.C. Feasibility and potential effect of a low-cost virtual reality system on reducing pain and anxiety in adult burn injury patients during physiotherapy in a developing country. Burns 2012, 36, 659–664. [Google Scholar] [CrossRef]
- Martin Ruiz-Berdejo, A. Effectiveness of A Brief Intervention Program with Virtual Reality for Anxiety Reduction in Preoperative General Surgery Patients. 2016. Available online: file:///C:/Users/MDPI/Downloads/ALBA%20MART%C3%8DN_TFG.pdf(accessed on 2 May 2022).
- Jofré Pasinetti, N.; Rodríguez, G.; Alvarado, Y.; Fernández, J.; Guerrero, R.A. The use of immersive virtual reality in motor therapies. In XIX Workshop of Researchers in Computer Science; WICC 2017; ITBA: Buenos Aires, Argentina, 2017. [Google Scholar]
- Gomez, M.; Maria, A. Uso de la Realidad Virtual para Disminuir el Dolor en los Procedimientos Invasivos en la Hospitalizacion Pediatrica: Revision Bibliografica. 2021. Available online: http://hdl.handle.net/10854/6734 (accessed on 2 May 2022).
- Mantovani, F.; Castelnuovo, G.; Gaggioli, A.; Riva, G. Virtual reality training for health-care professionals. Cyberpsychol. Behav. 2003, 6, 389–395. [Google Scholar] [CrossRef] [Green Version]
| Database | Syntax Adopted |
|---|---|
| PubMed | “Virtual Reality AND therapy AND pain AND burn patients AND range of motion” |
| Cochrane | “Virtual Reality AND therapy AND pain AND burn patients AND range of motion” |
| Dialnet | “Realidad Virtual AND terapia AND dolor AND quemados AND rango de movimiento” |
| Scopus | “Virtual Reality AND therapy AND pain AND burn patients AND range of motion” |
| Science Direct | “Virtual Reality AND therapy AND pain AND burn patients AND range of motion” |
| Author | Country and Location | Age, Mean (SD), Median | Type of Study | Sample Size | Type of Intervention | Dose of Treatment | Outcome Measures/ Assessment Tools | Results |
|---|---|---|---|---|---|---|---|---|
| Yohannan et al. (2012) [20] | America Inc., Redmond, WA, USA | 20–78 GE = mean 42.1 GC = mean 32.1 | Comparative study | n = 28 (5 were eliminated) EG = 11 CG = 12 | EG = active ROM therapy and Wii exercises. CG = therapy for active range of motion adapted by the therapist. | 3 consecutive 15 min sessions of standardized therapy followed by an additional 15 min of Wii play. | Subjective assessment questionnaires developed. VAS goniometer. | The Wii group experienced less pain (× 0.97, p 0.07) than the control group (× 0.97, p 0.07) over time. Overall, trends with anxiety (× 0.1 l, p 0.77), AROM (× 0.55, p 0.81), function (× 0.38, p 0.43) and enjoyment (× 0.09, p 0.73) favoured the Wii group. |
| Lozano et al. (2018) [26] | Soweto (Gauteng) South Africa | 5–9, mean 7 | Control group and experimental group study | n = 66 CG = 35 XboxG = 31 | XboxG = standard physiotherapy treatment and an Xbox Kinect. 1 or 2 times a day. CG = standard standard physiotherapy. | 30 to 45 min treatment sessions performed at least 1 or 2 times a day. | Goniometer. activity scale for kids (ASK) Wong–Baker modified enjoyment rating scale (FACES) | The addition of Xbox Kinect in the treatment was effective in achieving higher AROM between discharge and follow-up (p < 0.01). |
| Radwan et al. (2020) [27] | Al-Kharj City, Riyadh, KSA. Saudi Arabia | 7–12 GE = 9.52 ± 1.72 GC = 10.23 ± 1.75 | Control group and experimental group study | n = 50 EG = 25 (3 excluded and 1 did not participate) EG = 21 CG = 25 (1 excluded and 1 did not attend) CG = 23 | EG = 30 min of traditional physical therapy treatment followed by 30 min of Wii training. Approved games were bowling, baseball and tennis. CG = a conventional physical therapy program to maintain normal ROM. | 30 min sessions of traditional therapy followed by 30 min of Wii therapy. | JTHFT | The study group significantly improved hand-to-head (p = 0.001, p < 0.001), hand-to-mouth (p = 0.001) and hand-to-shoulder (p < 0.001, p = 0.0018) movements compared to the control group. |
| Kamel et al. (2021) [17] | Cairo, Egypt | 7–14, mean 10,70 | RCT | n = 50 XboxG = 17 GTOT = 16 CG = 17 | XboxG = conventional rehabilitation plus therapeutic games on Xbox. TOTG = conventional rehabilitation by increasing the time of the activity and modifying the time spent in the materials used. CG = conventional rehabilitation. | 50 min sessions, 3 days a week for 8 weeks with motion detection games and interactive video games with the Xbox. | JTHFT DHI COPM Goniometer. | There were no significant changes in JTHFT performance and COMP performance, ROM, grip strength, and lateral and toe pinch strength between the Xbox group and the TOTG [p > 0.05]. |
| Soltani et al. (2018) [25] | Seattle, WA, USA | 15–66, mean 36 | RCT | n = 39 | Active ROM exercises while playing in virtual reality with the SnowWorld game. | Average treatment duration was approximately 3 min. | GRS Goniometer. Subjective evaluations. | No significant effect of VR on peak ROM was found when compared to order (No VR M = 59.0 ± 44.8 degrees; VR M ± 58.9 ± 43.6 degrees), t(37) p = 0.94 NS. Pain discomfort was also significantly lower during RV than during no RV (no RV M = 52.7 [SD = 28.8]; RV M = 29.3 [SD = 24.7], t (36) = 5.18, p < 0.001; SD = 27.44. |
| Carrougher et al. (2009) [26] | Seattle, WA, USA | 21–57, mean 35 | RCT and prospective study. | n = 41 (2 were withdrawn) n = 39 | Virtual-reality therapy with the SnowWorld game plus physiotherapy and pharmacological therapy. | Ten-minute sessions of exercises with and without virtual reality. Total duration not specified. | GRS Goniometer. | VR reduced all GRS pain scores (worst pain, time spent thinking about pain, and pain discomfort) by 27, 37, and 37%. (worst pain, time spent thinking about pain, and pain discomfort by 27%, 37%, and 31%, respectively). The mean improvement in ROM was slightly slightly greater with the VR condition; however, this difference did not reach clinical or statistical significance (p = 0.243). |
| Faber et al. (2013) [27] | Netherlands. | 8–57, mean 27.7. | Comparative study | n = 289 (253 excluded) n = 36 | Virtual-reality therapy with the SnowWorld game. | Seven virtual-reality sessions performed during wound care of the participants. | VAT Subjective valuations. | VR reduced the amount of reported pain by more than one dressing change/wound debridement session per patient. |
| Hoffman et al. (2019) [28] | Galveston, TX, USA | 6–17, mean 12. | Pilot study | n = 62 (14 excluded) n = 48 | Virtual-reality therapy with SnowWorld game and nursing care. | Five min virtual-reality sessions alternated with another 5 min of treatment without virtual reality. | GRS Surveys to assess the user’s presence in the virtual world. PSC-C | VR significantly reduced the “worst pain” indices. during No VR = 8.52 (SD = 1.75) vs. during VR yes = 5.10 (SD = 3.27), t (47) = 7.11, p < 0.001 |
| Schmitt et al. (2011) [29] | Seattle, WA, USA | 6–19, mean 12.0 ± 3.9, | RCT | n = 54 | Virtual-reality therapy with the SnowWorld game more physiotherapy to increase range of motion. | Sessions of 6 to 20 min divided into two consecutive parts of identical duration (3–10 min each) over 5 days | GRS Subjective assessments. Goniometer. | The GRS assessments of cognitive pain (44% reduction), affective pain (32% reduction), and sensory pain (27% reduction) were significantly lower (p < 0.05) with the adjunctive virtual-reality treatment than with the control. Immersive VR did not result in a significant increase in maximal range of joint motion compared to the control condition (p = 0.21). However, there was a significant increase in maximal range of motion (mean increase of 6.8 degrees, p = 0.03) in the second treatment condition. |
| Lee et al. (2022) [30] | Korea. (Asia Oriental) | Mean 57.55 ± 7.55 | Interventional (clinical trial) | n = 33 | Robot-assisted gait training (RAGT) in burn patients by analysing the cerebral blood flow (CBF) in the prefrontal cortex. | RAGT: 30 min sessions, 10 times for 2 weeks, from Monday to Friday. 15 min sessions of VR application, with a 2 min break, and 15 min session without VR. | Functional near-infrared spectroscopy (fNIRS). Visual analogue scale (VAS). | The mean VAS pain scores were significantly lower (p < 0.05) in the experimental condition than in the control condition. Oxyhaemoglobin in the prefrontal lobe significantly increased when RAGT was performed with VR. The results of the analyses conducted on HbO2 in the PFC indicated a significant VR-related PFC activation during RAGT, as compared with the results in the control condition. |
| Criteria | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Studies | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Total | Score Interpretation |
| Yohannan et al. [20] | Y | Y | N | Y | N | N | Y | Y | Y | Y | Y | 7 | Good |
| Lozano et al. [24] | Y | N | N | Y | N | N | N | Y | N | Y | Y | 5 | Average |
| Radwan et al. [31] | Y | Y | N | Y | N | N | N | Y | Y | Y | Y | 6 | Good |
| Kamel et al. [17] | Y | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8 | Good |
| Yoltani et al. [25] | Y | Y | N | Y | N | N | N | Y | Y | Y | Y | 6 | Good |
| Carrougher et al. [26] | Y | Y | N | Y | N | N | N | Y | Y | Y | Y | 6 | Good |
| Faber et al. [27] | Y | N | N | N | N | N | N | Y | Y | Y | Y | 4 | Average |
| Hoffman et al. [28] | Y | N | N | Y | N | N | N | Y | Y | Y | Y | 5 | Average |
| Schmitt et al. [29] | Y | N | N | Y | N | N | N | Y | Y | Y | Y | 5 | Average |
| Lee et al. [30] | Y | N | N | Y | N | N | N | Y | Y | Y | Y | 5 | Average |
| Criteria | |||||||
|---|---|---|---|---|---|---|---|
| Studies | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| Yohannan et al. [20] | ? | ? | - | - | + | + | + |
| Lozano et al. [24] | - | - | - | - | + | + | + |
| Radwan et al. [31] | + | - | ? | ? | + | + | + |
| Kamel et al. [17] | + | + | - | +? | + | + | + |
| Soltani et al. [25] | ? | ? | - | ? | - | + | + |
| Carrougher et al. [26] | ? | ? | - | - | + | + | + |
| Faber et al. [27] | - | ? | - | - | + | + | + |
| Hoffman et al. [28] | ? | ? | - | ? | + | + | + |
| Schmitt et al. [29] | ? | ? | - | - | + | + | + |
| Lee et al. [30] | - | - | - | - | + | + | + |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Garrido-Ardila, E.M.; Santos-Domínguez, M.; Rodríguez-Mansilla, J.; Torres-Piles, S.T.; Rodríguez-Domínguez, M.T.; González-Sánchez, B.; Jiménez-Palomares, M. A Systematic Review of the Effectiveness of Virtual Reality-Based Interventions on Pain and Range of Joint Movement Associated with Burn Injuries. J. Pers. Med. 2022, 12, 1269. https://doi.org/10.3390/jpm12081269
Garrido-Ardila EM, Santos-Domínguez M, Rodríguez-Mansilla J, Torres-Piles ST, Rodríguez-Domínguez MT, González-Sánchez B, Jiménez-Palomares M. A Systematic Review of the Effectiveness of Virtual Reality-Based Interventions on Pain and Range of Joint Movement Associated with Burn Injuries. Journal of Personalized Medicine. 2022; 12(8):1269. https://doi.org/10.3390/jpm12081269
Chicago/Turabian StyleGarrido-Ardila, Elisa María, María Santos-Domínguez, Juan Rodríguez-Mansilla, Silvia Teresa Torres-Piles, María Trinidad Rodríguez-Domínguez, Blanca González-Sánchez, and María Jiménez-Palomares. 2022. "A Systematic Review of the Effectiveness of Virtual Reality-Based Interventions on Pain and Range of Joint Movement Associated with Burn Injuries" Journal of Personalized Medicine 12, no. 8: 1269. https://doi.org/10.3390/jpm12081269
APA StyleGarrido-Ardila, E. M., Santos-Domínguez, M., Rodríguez-Mansilla, J., Torres-Piles, S. T., Rodríguez-Domínguez, M. T., González-Sánchez, B., & Jiménez-Palomares, M. (2022). A Systematic Review of the Effectiveness of Virtual Reality-Based Interventions on Pain and Range of Joint Movement Associated with Burn Injuries. Journal of Personalized Medicine, 12(8), 1269. https://doi.org/10.3390/jpm12081269









