Physical Activity and Sedentary Time in Korean Adults before and during the COVID-19 Pandemic Using Data from the Korea National Health and Nutritional Examination Survey
Abstract
:1. Introduction
2. Materials and Methods
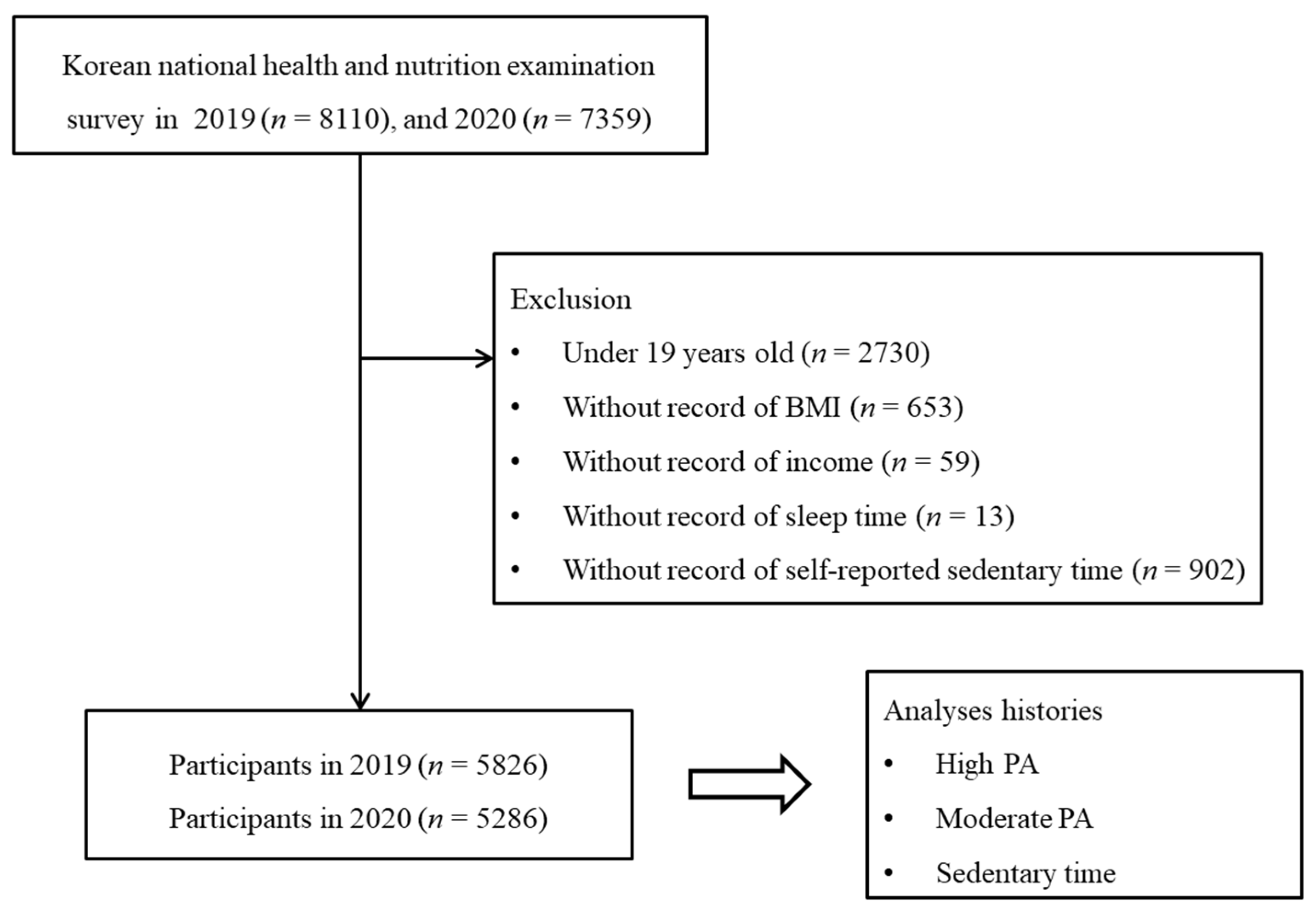
2.1. Study Population and Data Collection
2.2. Survey
2.2.1. Exposure
2.2.2. Outcome
2.2.3. Covariate
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lavie, C.J.; Ozemek, C.; Carbone, S.; Katzmarzyk, P.T.; Blair, S.N. Sedentary Behavior, Exercise, and Cardiovascular Health. Circ. Res. 2019, 124, 799–815. [Google Scholar] [CrossRef] [PubMed]
- Ozemek, C.; Laddu, D.R.; Lavie, C.J.; Claeys, H.; Kaminsky, L.A.; Ross, R.; Wisloff, U.; Arena, R.; Blair, S.N. An Update on the Role of Cardiorespiratory Fitness, Structured Exercise and Lifestyle Physical Activity in Preventing Cardiovascular Disease and Health Risk. Prog. Cardiovasc. Dis. 2018, 61, 484–490. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- AbdelBasset, W.K. Stay Home: Role of Physical Exercise Training in Elderly Individuals’ Ability to Face the COVID-19 Infection. J. Immunol. Res. 2020, 2020, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Carek, P.J.; Laibstain, S.E.; Carek, S.M. Exercise for the Treatment of Depression and Anxiety. Int. J. Psychiatry Med. 2011, 41, 15–28. [Google Scholar] [CrossRef]
- Wu, X.Y.; Han, L.H.; Zhang, J.H.; Luo, S.; Hu, J.W.; Sun, K. The influence of physical activity, sedentary behavior on health-related quality of life among the general population of children and adolescents: A systematic review. PLoS ONE 2017, 12, e0187668. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dempsey, P.C.; Matthews, C.E.; Dashti, S.G.; Doherty, A.R.; Bergouignan, A.; van Roekel, E.H.; Dunstan, D.W.; Wareham, N.J.; Yates, T.E.; Wijndaele, K.; et al. Sedentary Behavior and Chronic Disease: Mechanisms and Future Directions. J. Phys. Act. Health 2020, 17, 52–61. [Google Scholar] [CrossRef]
- Zhang, X.; Li, X.; Sun, Z.; He, Y.; Xu, W.; Campbell, H.; Dunlop, M.G.; Timofeeva, M.; Theodoratou, E. Physical activity and COVID-19: An observational and Mendelian randomisation study. J. Glob. Health 2020, 10, 020514. [Google Scholar] [CrossRef]
- Chen, P.; Mao, L.; Nassis, G.P.; Harmer, P.; Ainsworth, B.E.; Li, F. Coronavirus disease (COVID-19): The need to maintain regular physical activity while taking precautions. J. Sport Health Sci. 2020, 9, 103–104. [Google Scholar] [CrossRef]
- Rossi, L.; Behme, N.; Breuer, C. Physical Activity of Children and Adolescents during the COVID-19 Pandemic—A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 11440. [Google Scholar] [CrossRef]
- Delbressine, J.; Machado, F.; Goërtz, Y.; Van Herck, M.; Meys, R.; Houben-Wilke, S.; Burtin, C.; Franssen, F.; Spies, Y.; Vijlbrief, H.; et al. The Impact of Post-COVID-19 Syndrome on Self-Reported Physical Activity. Int. J. Environ. Res. Public Health 2021, 18, 6017. [Google Scholar] [CrossRef] [PubMed]
- Zaccagni, L.; Toselli, S.; Barbieri, D. Physical Activity during COVID-19 Lockdown in Italy: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 6416. [Google Scholar] [CrossRef] [PubMed]
- Dunton, G.F.; Do, B.; Wang, S.D. Early effects of the COVID-19 pandemic on physical activity and sedentary behavior in children living in the U.S. BMC Public Health 2020, 20, 1351. [Google Scholar] [CrossRef] [PubMed]
- Schuch, F.B.; Bulzing, R.A.; Meyer, J.; Vancampfort, D.; Firth, J.; Stubbs, B.; Grabovac, I.; Willeit, P.; Tavares, V.D.O.; Calegaro, V.C.; et al. Associations of moderate to vigorous physical activity and sedentary behavior with depressive and anxiety symptoms in self-isolating people during the COVID-19 pandemic: A cross-sectional survey in Brazil. Psychiatry Res. 2020, 292, 113339. [Google Scholar] [CrossRef]
- Korea National Health and Nutrition Examination Survey. Available online: https://knhanes.kdca.go.kr/knhanes/main.do (accessed on 2 January 2022).
- Headquarters Cdc. Coronavirus (COVID-19), Republic of Korea. 2022. Available online: http://ncov.mohw.go.kr/en/guidelineList.do?brdId=18&brdGubun=181&dataGubun=&ncvContSeq=&contSeq=&board_id=&gubun= (accessed on 2 January 2022).
- Kweon, S.; Kim, Y.; Jang, M.-J.; Kim, Y.; Kim, K.; Choi, S.; Chun, C.; Khang, Y.-H.; Oh, K. Data Resource Profile: The Korea National Health and Nutrition Examination Survey (KNHANES). Int. J. Epidemiol. 2014, 43, 69–77. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- An, K.-Y. Physical activity level in Korean adults: The Korea National Health and Nutrition Examination Survey 2017. Epidemiol. Health 2019, 41, e2019047. [Google Scholar] [CrossRef]
- Lee, J.; Lee, C.; Min, J.; Kang, D.W.; Kim, J.Y.; Yang, H.I.; Park, J.; Lee, M.K.; Lee, M.Y.; Park, I.; et al. Development of the Korean Global Physical Activity Questionnaire: Reliability and validity study. Global Health Promotion. 2020, 27, 44–55. [Google Scholar] [CrossRef]
- An, S.; Park, S. Association of Physical Activity and Sedentary Behavior With the Risk of Colorectal Cancer. J. Korean Med. Sci. 2022, 37, e158. [Google Scholar] [CrossRef]
- Hah, J.H.; Sim, S.; An, S.-Y.; Sung, M.-W.; Choi, H.G. Evaluation of the prevalence of and factors associated with laryngeal diseases among the general population. Laryngoscope 2015, 125, 2536–2542. [Google Scholar] [CrossRef]
- Min, C.; Kim, H.-J.; Park, I.-S.; Park, B.; Kim, J.-H.; Sim, S.; Choi, H.G. The association between sleep duration, sleep quality, and food consumption in adolescents: A cross-sectional study using the Korea Youth Risk Behavior Web-based Survey. BMJ Open 2018, 8, e022848. [Google Scholar] [CrossRef]
- Castañeda-Babarro, A.; Arbillaga-Etxarri, A.; Gutiérrez-Santamaría, B.; Coca, A. Physical Activity Change during COVID-19 Confinement. Int. J. Environ. Res. Public Health 2020, 17, 6878. [Google Scholar] [CrossRef]
- Lesser, I.A.; Nienhuis, C.P. The Impact of COVID-19 on Physical Activity Behavior and Well-Being of Canadians. Int. J. Environ. Res. Public Health 2020, 17, 3899. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Larrad, A.; Mañas, A.; Labayen, I.; González-Gross, M.; Espin, A.; Aznar, S.; Serrano-Sánchez, J.A.; Vera-Garcia, F.J.; González-Lamuño, D.; Ara, I.; et al. Impact of COVID-19 Confinement on Physical Activity and Sedentary Behaviour in Spanish University Students: Role of Gender. Int. J. Environ. Res. Public Health 2021, 18, 369. [Google Scholar] [CrossRef] [PubMed]
- Sharma, N.; Vaish, H. Impact of COVID-19 on mental health and physical load on women professionals: An online cross-sectional survey. Health Care Women Int. 2020, 41, 1255–1272. [Google Scholar] [CrossRef] [PubMed]
- Navas-Martín, M.; López-Bueno, J.A.; Oteiza, I.; Cuerdo-Vilches, T. Routines, Time Dedication and Habit Changes in Spanish Homes during the COVID-19 Lockdown. A Large Cross-Sectional Survey. Int. J. Environ. Res. Public Health 2021, 18, 12176. [Google Scholar] [CrossRef]
- Meyer, J.; McDowell, C.; Lansing, J.; Brower, C.; Smith, L.; Tully, M.; Herring, M. Changes in Physical Activity and Sedentary Behavior in Response to COVID-19 and Their Associations with Mental Health in 3052 US Adults. Int. J. Environ. Res. Public Health 2020, 17, 6469. [Google Scholar] [CrossRef]
- Carvalho, V.O.; Gois, C.O. COVID-19 pandemic and home-based physical activity. J. Allergy Clin. Immunol. Pr. 2020, 8, 2833–2834. [Google Scholar] [CrossRef]
- Chaabene, H.; Prieske, O.; Herz, M.; Moran, J.; Höhne, J.; Kliegl, R.; Ramirez-Campillo, R.; Behm, D.; Hortobágyi, T.; Granacher, U. Home-based exercise programmes improve physical fitness of healthy older adults: A PRISMA-compliant systematic review and meta-analysis with relevance for COVID-19. Ageing Res. Rev. 2021, 67, 101265. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.Y.; Kim, D.W. Does the Clinical Spectrum of Coronavirus Disease 2019 (COVID-19) Show Regional Differences? Clin. Exp. Otorhinolaryngol. 2020, 13, 83–84. [Google Scholar] [CrossRef] [PubMed]
- Park, J.-H.; Jang, W.; Kim, S.-W.; Lee, J.; Lim, Y.-S.; Cho, C.-G.; Park, S.-W.; Kim, B.H. The Clinical Manifestations and Chest Computed Tomography Findings of Coronavirus Disease 2019 (COVID-19) Patients in China: A Proportion Meta-Analysis. Clin. Exp. Otorhinolaryngol. 2020, 13, 95–105. [Google Scholar] [CrossRef]
| Characteristics | Year | p-Value * | ||
|---|---|---|---|---|
| 2019 | 2020 | |||
| Age (yrs, mean, SD) | 51.3 (16.7) | 51.0 (16.9) | 0.551 | |
| Age groups (yrs, n, %) | 0.942 | |||
| 19–39 | 1596 (27.4) | 1497 (28.3) | ||
| 40–59 | 2190 (37.6) | 1913 (36.2) | ||
| ≥60 | 2040 (35.0) | 1876 (35.5) | ||
| Sex (n, %) | 0.400 | |||
| Males | 2587 (49.7) | 2398 (45.4) | ||
| Females | 3239 (50.3) | 2888 (54.6) | ||
| Income (mean, SD) | 3.2 (1.4) | 3.3 (1.3) | 0.446 | |
| Income group (n, %) | 0.861 | |||
| 1 (lowest) | 841 (10.8) | 662 (10.0) | ||
| 2 | 1056 (16.1) | 931 (15.1) | ||
| 3 | 1178 (21.4) | 1110 (21.6) | ||
| 4 | 1343 (25.1) | 1265 (25.5) | ||
| 5 (highest) | 1408 (26.6) | 1318 (27.9) | ||
| Employment (n, %) | 0.356 | |||
| Unemployed | 2266 (34.9) | 2073 (36.1) | ||
| Employed | 3560 (65.1) | 3213 (63.9) | ||
| Educational status (n, %) | 0.281 | |||
| Elementary school or under, unknown | 1038 (12.2) | 850 (10.7) | ||
| Junior high school | 549 (7.7) | 512 (7.6) | ||
| High school | 1961 (35.8) | 1878 (38.9) | ||
| College or over | 2278 (44.2) | 2046 (42.8) | ||
| House type (n, %) | 0.710 | |||
| Detached house | 1777 (27.4) | 1676 (27.3) | ||
| Condominium | 3216 (57.3) | 2964 (64.3) | ||
| Raw houses | 784 (14.5) | 618 (11.9) | ||
| Others | 49 (9.8) | 28 (8.4) | ||
| Marriage status (n, %) | 0.049 * | |||
| Married | 4017 (66.7) | 3459 (63.3) | ||
| Unmarried | 783 (13.0) | 709 (19.0) | ||
| Unknown | 1026 (23.3) | 1118 (26.7) | ||
| Body mass index (mean, SD) | 23.9 (3.6) | 24.2 (3.8) | <0.001 * | |
| Smoking status (n, %) | 0.521 | |||
| Nonsmoker | 3465 (56.6) | 3160 (56.5) | ||
| Past smoker | 1346 (23.1) | 1231 (24.1) | ||
| Current smoker | 1015 (20.3) | 895 (19.4) | ||
| Alcohol consumption (n, %) | 0.115 | |||
| Nonconsumer | 2660 (41.8) | 2541 (43.7) | ||
| 1 to 5 times/mo | 1931 (36.4) | 1667 (33.8) | ||
| ≥2 times/week | 1235 (21.8) | 1078 (22.4) | ||
| Sleep duration (mean, SD) | 6.8 (1.3) | 6.8 (1.4) | 0.874 | |
| Hypertension (n, %) | 1449 (20.2) | 1288 (19.7) | 0.691 | |
| Dyslipidemia (n, %) | 1137 (16.6) | 1155 (18.0) | 0.117 | |
| Stroke (n, %) | 137 (1.9) | 114 (1.6) | 0.242 | |
| Ischemic heart disease (n, %) | 179 (2.5) | 173 (2.2) | 0.458 | |
| Osteoarthritis (n, %) | 661 (8.4) | 599 (8.2) | 0.813 | |
| Rheumatoid arthritis (n, %) | 117 (1.8) | 91 (1.2) | 0.031 * | |
| Diabetes mellitus (n, %) | 559 (7.8) | 557 (8.5) | 0.341 | |
| Chronic kidney disease (n, %) | 24 (0.4) | 99 (1.6) | <0.001 * | |
| Gout (n, %) | 102 (2.0) | 100 (1.9) | 0.694 | |
| High PA (n, %) | 0.814 | |||
| ≥75 min/wk | 438 (9.1) | 396 (8.9) | ||
| <75 min/wk | 5388 (90.9) | 4890 (91.1) | ||
| Moderate PA (n, %) | 0.097 | |||
| ≥150 min/wk | 818 (14.9) | 837 (16.7) | ||
| <150 min/wk | 5008 (85.1) | 4449 (83.3) | ||
| Sedentary time (n, %) | 0.071 | |||
| ≥240 min/d | 21 (0.3) | 39 (0.7) | ||
| ≥120 min/d and <240 min/d | 482 (7.9) | 394 (7.5) | ||
| <120 min/d | 5323 (91.8) | 4853 (91.8) | ||
| Characteristics | Odds Ratios for ≥75 min/wk of High PA in 2020 Compared to 2019 | ||||
|---|---|---|---|---|---|
| Crude | p-Value * | Adjusted † | p-Value * | ||
| Total participants (n = 11,112) | 0.98 (0.80–1.20) | 0.814 | 0.96 (0.79–1.18) | 0.696 | |
| Age | |||||
| 19–39 years old (n = 3093) | 0.93 (0.72–1.21) | 0.586 | 0.93 (0.71–1.23) | 0.629 | |
| 40–59 years old (n = 4103) | 1.00 (0.76–1.32) | 0.983 | 1.03 (0.77–1.37) | 0.860 | |
| ≥60 years old (n = 3916) | 1.11 (0.71–1.73) | 0.649 | 1.03 (0.66–1.60) | 0.913 | |
| Sex | |||||
| Males (n = 4985) | 0.88 (0.70–1.11) | 0.270 | 0.87 (0.69–1.10) | 0.241 | |
| Females (n = 6127) | 1.22 (0.90–1.66) | 0.191 | 1.21 (0.89–1.64) | 0.218 | |
| Characteristics | Odds Ratios for ≥150 min/wk of Moderate PA in 2020 Compared to 2019 | ||||
|---|---|---|---|---|---|
| Crude | p-Value * | Adjusted † | p-Value * | ||
| Total participants (n = 11,112) | 1.15 (0.97–1.36) | 0.100 | 1.12 (0.94–1.32) | 0.201 | |
| Age | |||||
| 19–39 years old (n = 3093) | 1.21 (0.97–1.51) | 0.084 | 1.23 (0.97–1.55) | 0.085 | |
| 40–59 years old (n = 4103) | 1.01 (0.79–1.28) | 0.971 | 1.01 (0.79–1.28) | 0.971 | |
| ≥60 years old (n = 3916) | 1.33 (1.00–1.77) | 0.050 | 1.23 (0.92–1.66) | 0.160 | |
| Sex | |||||
| Males (n = 4985) | 1.02 (0.85–1.24) | 0.813 | 1.01 (0.84–1.22) | 0.915 | |
| Females (n = 6127) | 1.36 (1.07–1.74) | 0.013 * | 1.29 (1.01–1.65) | 0.042 * | |
| Characteristics | Odds Ratios for ≥120 min/d of Sedentary Time in 2020 Compared to 2019 | ||||
|---|---|---|---|---|---|
| Crude | p-Value * | Adjusted † | p-Value * | ||
| Total participants (n = 11,112) | 0.39 (0.18–0.84) | 0.017 * | 0.35 (0.17–0.72) | 0.005 * | |
| Age | |||||
| 19–39 years old (n = 3093) | 0.18 (0.03–0.96) | 0.045 * | 0.13 (0.02–0.89) | 0.038 * | |
| 40–59 years old (n = 4103) | 0.35 (0.12–1.04) | 0.059 | 0.35 (0.11–1.08) | 0.067 | |
| ≥60 years old (n = 3916) | 0.59 (0.26–1.34) | 0.203 | 0.52 (0.23–1.21) | 0.131 | |
| Sex | |||||
| Males (n = 4985) | 0.67 (0.23–1.96) | 0.461 | 0.74 (0.26–2.14) | 0.582 | |
| Females (n = 6127) | 0.24 (0.09–0.65) | 0.005 * | 0.20 (0.07–0.53) | 0.001 * | |
| Characteristics | Sex | p-Value * | ||
|---|---|---|---|---|
| Males | Females | |||
| High PA (n, %) | <0.001 * | |||
| ≥75 min/wk | 298 (13.7) | 140 (4.6) | ||
| <75 min/wk | 2289 (86.3) | 3099 (95.4) | ||
| Moderate PA (n, %) | <0.001 * | |||
| ≥150 min/wk | 484 (19.5) | 334 (10.3) | ||
| <150 min/wk | 2103 (80.5) | 2905 (89.7) | ||
| Sedentary time (n, %) | 0.325 | |||
| ≥240 min/d | 2378 (92.3) | 2945 (91.2) | ||
| ≥120 min/d and <240 min/d | 196 (7.4) | 286 (8.5) | ||
| <120 min/d | 13 (0.3) | 08 (0.2) | ||
| Characteristics | Sex | p-Value * | ||
|---|---|---|---|---|
| Males | Females | |||
| High PA (n, %) | <0.001 * | |||
| ≥75 min/wk | 259 (12.2) | 137 (5.5) | ||
| <75 min/wk | 2139 (87.8) | 2751 (94.5) | ||
| Moderate PA (n, %) | <0.001 * | |||
| ≥150 min/wk | 475 (19.8) | 362 (13.6) | ||
| <150 min/wk | 1923 (80.2) | 2526 (86.4) | ||
| Sedentary time (n, %) | 0.026 * | |||
| ≥240 min/d | 2183 (91.8) | 2670 (91.8) | ||
| ≥120 min/d and <240 min/d | 204 (7.9) | 190 (7.5) | ||
| <120 min/d | 11 (0.3) | 28 (0.7) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.Y.; Yoo, D.M.; Kwon, M.J.; Kim, J.H.; Kim, J.-H.; Bang, W.J.; Choi, H.G. Physical Activity and Sedentary Time in Korean Adults before and during the COVID-19 Pandemic Using Data from the Korea National Health and Nutritional Examination Survey. J. Pers. Med. 2022, 12, 1217. https://doi.org/10.3390/jpm12081217
Kim SY, Yoo DM, Kwon MJ, Kim JH, Kim J-H, Bang WJ, Choi HG. Physical Activity and Sedentary Time in Korean Adults before and during the COVID-19 Pandemic Using Data from the Korea National Health and Nutritional Examination Survey. Journal of Personalized Medicine. 2022; 12(8):1217. https://doi.org/10.3390/jpm12081217
Chicago/Turabian StyleKim, So Young, Dae Myoung Yoo, Mi Jung Kwon, Ji Hee Kim, Joo-Hee Kim, Woo Jin Bang, and Hyo Geun Choi. 2022. "Physical Activity and Sedentary Time in Korean Adults before and during the COVID-19 Pandemic Using Data from the Korea National Health and Nutritional Examination Survey" Journal of Personalized Medicine 12, no. 8: 1217. https://doi.org/10.3390/jpm12081217
APA StyleKim, S. Y., Yoo, D. M., Kwon, M. J., Kim, J. H., Kim, J.-H., Bang, W. J., & Choi, H. G. (2022). Physical Activity and Sedentary Time in Korean Adults before and during the COVID-19 Pandemic Using Data from the Korea National Health and Nutritional Examination Survey. Journal of Personalized Medicine, 12(8), 1217. https://doi.org/10.3390/jpm12081217







