Predicting Loss of Efficacy after Non-Medical Switching: Correlation between Circulating TNF-α Levels and SB4 in Etanercept to SB4 Switchers and Naïve Patients with Rheumatic Disease
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Laboratory Evaluation
2.3. Detection of Drug Levels
2.4. Activity Disease Status Evaluation
2.5. Health Assessment Questionnaire
2.6. Statistical Analysis
3. Results
3.1. Patients’ Characteristics
3.2. Longitudinal Evaluation of Clinical and Laboratory Biomarkers, Disease Activity, and Quality of Life
3.3. Comparison of Clinical and Laboratory Biomarkers, Disease Activity, and Quality of Life in ETN/SB4 Switcher Responders and Non-Responders and in Naïve Patients
- -
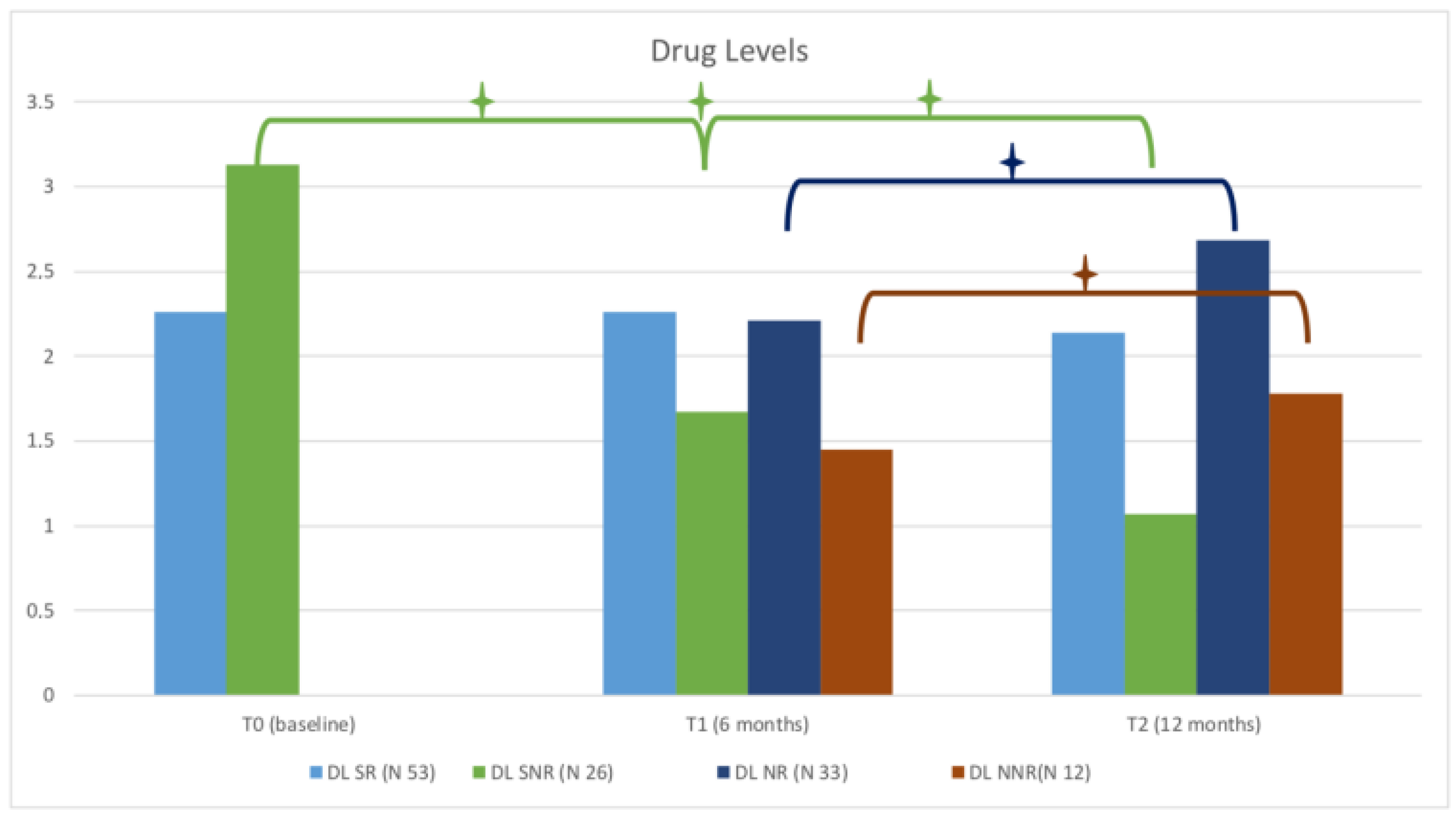
- DLs were higher in SNR at baseline (3.13 ± 0.2 mg/dL vs. 2.26 ± 0.11 mg/dL p < 0.0001) but became lower than SR value at 6 months (T1) (1.67 ± 0.16 mg/dL vs. 2.26 ± 0.1 mg/dL, p = 0.069) and at 12 months (T2) (1.07 ± 0.09 vs. 2.14 0.1 mg/dL, p < 0.0001), due to the decrease in DLs at follow-up in this cohort.
- -
- MRP in SNR was higher at T1 and at T2 (p < 0.0001).
- -
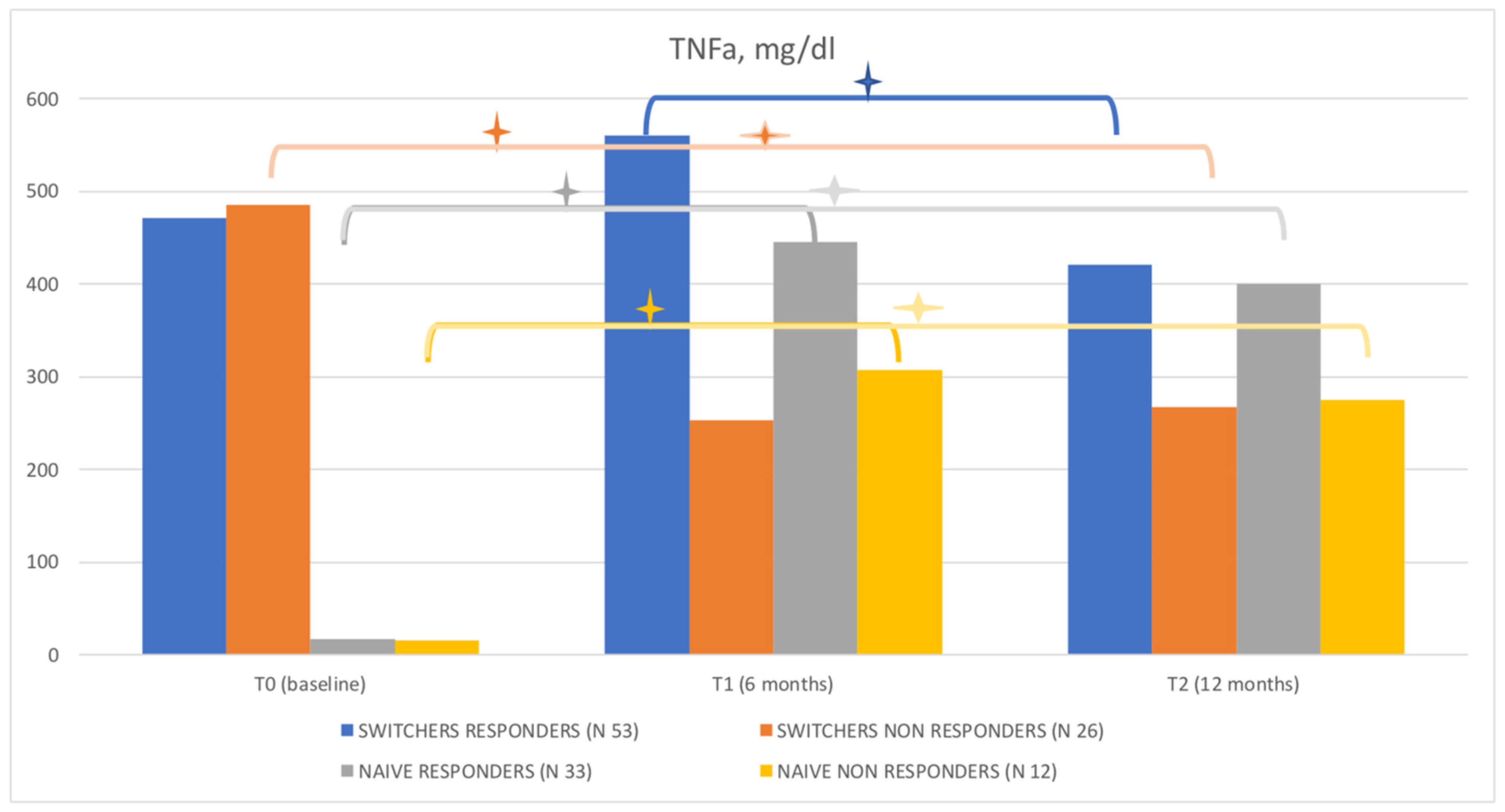
- TNF-α was higher in SR than in SNR at T1 and T2 (559.6 ± 26.25 mg/dL vs. 253 ± 34.75 mg/dL, p < 0.0001, and 420.5 ± 27.62 mg/dL vs. 266.8 ± 24.67 mg/dL, p = 0.0002, respectively).
- -
- IL-6 was higher in SR at T2 (p < 0.0001).
- -
- DL were lower in NNR at T1 (1.45 ± 0.41mg/dL vs. 2.21 ± 0.14, p < 0.0006) and T2 (1.78 ± 0.17 mg/dL ± 2.68 ± 0.2 mg/dL, p < 0.0047).
- -
- MRP was higher in NNR at T2 (p < 0.018).
- -
- TNFα was lower in NNR than in NR at T1 (307.6 ± 59.18 mg/dL vs. 445 ± 23.9 mg/dL vs. p = 0.032) and T2 (275.3 ± 49.17 mg/dL vs. 399.9 ± 24.5 mg/dL, p < 0.017).
- -
- IL-6 was higher in NNR at T1 (p < 0.01) and T2 (p < 0.0046).
3.4. Predictability of the Biomarkers in Switcher and Naïve Patients
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- European Medicines Agency (EMA). Biosimilars in EU. Information Guide for Healthcare Professionals. Available online: https://www.ema.europa.eu/en/news/new-guide-biosimilar-medicines-healthcare-professionals (accessed on 1 January 2022).
- US Food and Drug Administration. Biosimilars. Available online: https://www.fda.gov/Drugs/DevelopmentApprovalProcess/HowDrugsareDevelopedandAp-proved/ApprovalApplications/TherapeuticBiologicApplications/Biosimilars/ (accessed on 1 January 2022).
- Schulze-Koops, H.; Skapenko, A. Biosimilars in rheumatology: A review of the evidence and their place in the treatment algorithm. Rheumatology 2017, 56, iv30–iv48. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Cohen, H.P.; Blauvelt, A.; Rifkin, R.M.; Danese, S.; Gokhale, S.B.; Woollett, G. Switching Reference Medicines to Biosimilars: A Systematic Literature Review of Clinical Outcomes. Drugs 2018, 78, 463–478. [Google Scholar] [CrossRef]
- Ruff, L.; Rezk, M.F.; Uhlig, T.; Gommers, J.W. Budget impact analysis of an etanercept biosimilar for the treatment of rheumatoid arthritis in Europe. Value Health 2015, 18, A639. [Google Scholar] [CrossRef][Green Version]
- Considerations for Physicians on Switching Decisions Regarding Biosimilars. European Biopharmaceutical Enterprises; Euro-pean Federation of Pharmaceutical Industries and Associations; International Federation of Pharmaceutical Manufacturers and Associations. Available online: https://www.ebe-biopharma.eu/wpcon-tent/uploads/2017/04/considerations-forswitching-decisions_biosimilars-and-rbps-finalbranded-1.pdf (accessed on 3 April 2018).
- McKinnon, R.A.; Cook, M.; Liauw, W.; Marabani, M.; Marschner, I.C.; Packer, N.H.; Prins, J.B. Biosimilarity and Interchangeability: Principles and Evidence: A Systematic Review. BioDrugs 2018, 32, 27–52. [Google Scholar] [CrossRef] [PubMed]
- Gibofsky, A.; Skup, M.; Yang, M.; Mittal, M.; Macaulay, D.; Ganguli, A. Short-term costs associated with non-medical switching in autoimmune conditions. Clin. Exp. Rheumatol. 2018, 37, 97–105. [Google Scholar]
- Tarallo, M.; Onishchenko, K.; Alexopoulos, S.T. Costs associated with non-medical switching from originator to biosimilar etanercept in patients with rheumatoid arthritis in the UK. J. Med. Econ. 2019, 22, 1162–1170. [Google Scholar] [CrossRef]
- European Medicines Agency. Enbrel, Summary of Product Characteristics. Available online: www.ema.europa.eu/en/documents/product-information/enbrel-epar-product-information_en.pdf (accessed on 12 March 2020).
- European Medicines Agency. Benepali, Summary of Product Characteristics. Available online: https://www.ema.europa.eu/en/documents/product-information/benepali-epar-product-information_en.pdf (accessed on 12 March 2020).
- Lee, Y.J.; Shin, D.; Kim, Y.; Kang, J.W.; Gauliard, A.; Fuhr, R. A randomized phase l pharmacokinetic study comparing SB4 and etanercept reference product (Enbrel®) in healthy subjects. Br. J. Clin. Pharmacol. 2016, 82, 64–73. [Google Scholar] [CrossRef]
- Emery, P.; Vencovsky, J.; Sylwestrzak, A.; Leszczyński, P.; Porawska, W.; Baranauskaite, A.; Tseluyko, V.; Zhdan, V.M.; Stasiuk, B.; Milasiene, R.; et al. A phase III randomised, double-blind, parallel-group study comparing SB4 with etanercept reference product in patients with active rheumatoid arthritis despite methotrexate therapy. Ann. Rheum. Dis. 2015, 76, 51–57. [Google Scholar] [CrossRef]
- Cantini, F.; Benucci, M. Focus on biosimilar etanercept—Bioequivalence and interchangeability. Biol. Targets Ther. 2018, 12, 87–95. [Google Scholar] [CrossRef]
- Numan, S.; Faccin, F. Non-medical Switching from Originator Tumor Necrosis Factor Inhibitors to Their Biosimilars: Systematic Review of Randomized Controlled Trials and Real-World Studies. Adv. Ther. 2018, 35, 1295–1332. [Google Scholar] [CrossRef]
- Jamnitski, A.; Krieckaert, C.L.; Nurmohamed, M.T.; Hart, M.H.; Dijkmans, B.; Aarden, L.; Voskuyl, A.; Wolbink, G.J. Patients non-responding to etanercept obtain lower etanercept concentrations compared with responding patients. Ann. Rheum. Dis. 2011, 71, 88–91. [Google Scholar] [CrossRef]
- Deng, Y.; Hu, L.; Qiang, W.; Cheng, Z.; Wang, L.; Wang, X. TNF-α level affects etanercept clearance: TNF-α concentration as a new correction factor of allometric scaling to predict individual etanercept clearances in patients with ankylosing spondylitis. Clin. Exp. Pharmacol. Physiol. 2018, 45, 643–651. [Google Scholar] [CrossRef]
- Emery, P.; Vencovsky, J.; Sylwestrzak, A.; Leszczyński, P.; Porawska, W.; Stasiuk, B.; Hilt, J.; Mosterova, Z.; Cheong, S.Y.; Ghil, J. Long-term efficacy and safety in patients with rheumatoid arthritis continuing on SB4 or switching from reference etanercept to SB4. Ann. Rheum. Dis. 2017, 76, 1986–1991. [Google Scholar] [CrossRef]
- Emery, P.; Vencovský, J.; Sylwestrzak, A.; Leszczyński, P.; Porawska, W.; Baranauskaite, A.; Tseluyko, V.; Zhdan, V.M.; Stasiuk, B.; Milasiene, R.; et al. 52-week results of the phase 3 randomized study comparing SB4 with reference etanercept in patients with active rheumatoid arthritis. Rheumatology 2017, 56, 2093–2101. [Google Scholar] [CrossRef]
- Meacci, F.; Manfredi, M.; Infantino, M.; Grossi, V.; Benucci, M. Anti Etanercept and anti SB4 antibodies detection: Impact of the assay method. Ann. Rheum. Dis. 2016, 75, e39. [Google Scholar] [CrossRef]
- Krieckaert, C.L.; Nurmohamed, M.T.; Wolbink, G.J. Methotrexate reduces immunogenicity in adalimumab treated rheumatoid arthritis patients in a dose dependent manner. Ann. Rheum. Dis. 2012, 71, 1914–1915. [Google Scholar] [CrossRef] [PubMed]
- Burmester, G.-R.; Kivitz, A.J.; Kupper, H.; Arulmani, U.; Florentinus, S.; Goss, S.L.; Rathmann, S.S.; Fleischmann, R.M. Efficacy and safety of ascending methotrexate dose in combination with adalimumab: The randomised CONCERTO trial. Ann. Rheum. Dis. 2014, 74, 1037–1044. [Google Scholar] [CrossRef]
- Horiuchi, T.; Mitoma, H.; Harashima, S.-I.; Tsukamoto, H.; Shimoda, T. Transmembrane TNF-: Structure, function and interaction with anti-TNF agents. Rheumatology 2010, 49, 1215–1228. [Google Scholar] [CrossRef] [PubMed]
- Cho, I.H.; Lee, N.; Song, D.; Jung, S.Y.; Bou-Assaf, G.; Sosic, Z.; Zhang, W.; Lyubarskaya, Y. Evaluation of the structural, physicochemical, and biological characteristics of SB4, a biosimilar of etanercept. mAbs 2016, 8, 1136–1155. [Google Scholar] [CrossRef] [PubMed]
- European Medicines Agency. Human Medicines European Public Assessment Report (EPAR): Benepali [Internet]; European Medicines Agency: London, UK, 2016; Available online: http://www.ema.europa.eu/ema/ (accessed on 29 April 2016).
- Di-Paola, M.L.J.; Stephens, E.J. Development of biosimilars: Analysis of etanercept glycosylation as a case study. J. Bioanal. Biomed. 2013, 5, 180–186. [Google Scholar]
- Borza, B.; Szigeti, M.; Szekrenyes, A.; Hajba, L.; Guttman, A. Glycosimilarity assessment of biotherapeutics 1: Quantitative comparison of the N-glycosylation of the innovator and a biosimilar version of etanercept. J. Pharm. Biomed. Anal. 2018, 153, 182–185. [Google Scholar] [CrossRef] [PubMed]
- Obry, A.; Lequerré, T.; Hardouin, J.; Boyer, O.; Fardellone, P.; Philippe, P.; Le Loët, X.; Cosette, P.; Vittecoq, O. Identification of S100A9 as Biomarker of Responsiveness to the Methotrexate/Etanercept Combination in Rheumatoid Arthritis Using a Proteomic Approach. PLoS ONE 2014, 9, e115800. [Google Scholar] [CrossRef] [PubMed]
- Bandinelli, F.; Benucci, M.; Salaffi, F.; Manetti, M.; Infantino, M.; Damiani, A.; Manfredi, M.; Grossi, V.; Matucci, A.; Li Gobbi, F.; et al. Do new and old biomarkers of early undifferentiated arthritis correlate with Arthritis Impact Measurement Scales? Clin. Exp. Rheumatol. 2021, 39, 79–83. [Google Scholar] [CrossRef] [PubMed]
| Number of Patients (N) | Age (aa) | Female/Male Ratio | Duration of Disease (aa) | Duration of Treatment (aa) | |
|---|---|---|---|---|---|
| Switchers | |||||
| All | 79 | 59.21 (±13.20) | 45/34 | 9.11 (±3.75) | 8.04 (±2.70) |
| RA | 27 | 60.33 (±13.78) | 20/7 | 9.44 (±3.64) | 8.11 (±2.19) |
| AS | 24 | 58.08 (±13.04) | 6/18 | 9.62 (±4.27) | 8.70 (±2.12) |
| PsA | 28 | 59.11 (±13.15) | 19/9 | 8.36 (±3.38) | 7.43 (±2.8) |
| Naïve | |||||
| All | 45 | 60.42 (±15.62) | 32/13 | 3.33 (±2.56) | n.a. |
| RA | 14 | 67.43 (±13.40) | 12/2 | 4.79 (±3.15) | n.a. |
| AS | 12 | 49.33 (±17.12) | 8/ 4 | 2.42 (±0.67) | n.a. |
| PsA | 19 | 62.26 (±12.8) | 12/7 | 2.84 (±2.09) | n.a. |
| Number of Patients (N) | Baseline (T0) | 6 Months (T1) | 12 Months (T2) |
|---|---|---|---|
| Switcher Responders (53) | |||
| DAPSA (19) | 2.20 (±1.79) | 3.27 (±1.47) | 3.84 (±0.94) |
| DAS28 (16) | 2.23 (±1.18) | 1.85 (±0.76) | 2.04 (±0.40) |
| ASDAS (18) | 2.71 (±1.21) | 1.10 (±0.37) | 1.41 (±0.20) |
| Switcher non-responders (26) | |||
| DAPSA (10) | 1.59 (±1.20) | 5.20 (±0.42) | 6.08 (±1.72) |
| DAS28 (10) | 2.09 (±0.81) | 3.25 (±0.91) | 4.19 (±0.55) |
| ASDAS (6) | 1.82 (±0.72) | 2.52 (±0.42) | 3.15 (±0.56) |
| Naïve responders (33) | |||
| DAPSA (16) | 9.91 (±7.60) | 3.69 (±0.88) | 3.97 (±0.13) |
| DAS28 (9) | 4.33 (±0.99) | 2.25 (±0.18) | 2.98 (±0.60) |
| ASDAS (8) | 6.36 (±4.76 | 1.30 (±0.00) | 1.26 (±0.41) |
| Naïve non-responders (12) | |||
| DAPSA (3) | 11.1 (±7.16) | 6.27 (±1.61) | 8.43 (±0.51) |
| DAS28 (5) | 5.09 (±1.61) | 3.70 (±1.40) | 4.15 (±1.39) |
| ASDAS (4) | 3.65 (±0.24) | 3.72 (±0.17) | 4.47 (±0.39) |
| T0 (Baseline) | T1 (6 Months) | T2 (12 Months) | p-Value T0–T1 | p-Value T1–T2 | p-Value T0–T2 | |
|---|---|---|---|---|---|---|
| Switcher responders (N 53) | ||||||
| ERS, mm/h | 22.47 (±1.8) | 20.3 (±2) | 18.36 (±1.66) | n.s. | n.s. | n.s. |
| CRP, mg/dL | 0.47 (± 0.44) | 0.61 (±0.1) | 0.47 (±0.04) | n.s. | n.s. | n.s. |
| HAQ | 0.53 (±0.01) | 0.59 (±0.03) | 0.51 (±0.009) | n.s. | 0.0038 | n.s. |
| MRP, ng/mL | 2.25 (±0.09) | 1.91 (±0.09) | 2.09 (±0.1) | <0.0007 | n.s. | n.s. |
| TNF-a, mg/dL | 471 (± 26.18) | 559.6 (±26.25) | 420.5 (±27.62) | n.s. | 0.0018 | n.s. |
| IL 6, pg/mL | 3.71 (±0.2) | 3.9 (±0.3) | 5.32 (±0.7) | n.s. | n.s. | n.s. |
| Drug levels mg/dL | 2.26 (±0.1) | 2.26 (±0.1) | 2.14 (±0.1) | n.s. | n.s. | n.s. |
| Switcher non-responders (N 26) | ||||||
| ERS, mm/h | 19.96 (±2.1) | 30.9 (±3.8) | 29.88 (±3.28) | 0.028 | n.s. | n.s. |
| CRP, mg/dL | 0.40 (±0.07) | 1.10 (±0.18) | 1.55 (±0.15) | 0.001 | n.s. | <0.0001 |
| HAQ | 1.58 (±0.9) | 0.95 (±0.06) | 1.41 (±0.05) | n.s. | n.s. | n.s. |
| MRP, ng/mL | 2.18 (±0.14) | 2.22 (±0.1) | 2.88 (±0.19) | n.s. | 0.002 | 0.002 |
| TNFa, mg/dL | 485 (±33.9) | 253 (±34.75) | 266.8 (±24.67) | <0.0001 | n.s. | <0.0001 |
| IL 6, pg/mL | 3.28 (±0.18) | 3.36 (±0.16) | 4.96 (±0.79) | n.s. | n.s. | n.s. |
| Drug levels, mg/dL | 3.13 (±0.2) | 1.67 (±0.16) | 1.07 (±0.09) | <0.0001 | 0.02 | <0.0001 |
| Naïve responders (N 33) | ||||||
| ERS, mm/h | 26.06 (±2.38) | 19.36 (±2.1) | 17.1 (±1.4) | n.s. | n.s. | 0.01 |
| CRP, mg/dL | 1.51 (±0.25) | 0.49 (±0.06) | 0.46 (±0.05) | <0.0001 | n.s. | <0.0001 |
| HAQ | 1.37 (±0.07) | 0.54 (±0.02) | 0.52 (±0.01) | <0.0001 | n.s. | <0.0001 |
| MRP, ng/mL | 2.18 (±0.13) | 2.12 (±0.1) | 2.04 (±0.11) | n.s. | n.s. | n.s. |
| TNFa, mg/dL | 16.66(±0.49) | 445 (±23.9) | 399.9 (±24.5) | <0.0001 | n.s. | <0.0001 |
| IL 6, pg/mL | 5.64 (±0.59) | 3.91 (±0.42) | 4.03 (±0.51) | <0.0001 | n.s. | <0.0001 |
| Drug levels, mg/dL | n.e. | 2.21 (±0.14) | 2.68 (± 0.2) | n.e. | 0.032 | n.e. |
| Naïve non-responders (N 12) | ||||||
| ESR, mm/h | 33.42 (±5.72) | 27.3 (±5.75) | 29.75 (±4.09) | n.s. | n.s. | n.s. |
| CRP, mg/dL | 2.21 (±0.87) | 1.05 (±0.62) | 0.85 (±0.25) | n.s. | n.s. | n.s. |
| HAQ | 1.43 (±0.11) | 1.18 (±0.09) | 1.18 (±0.09) | n.s. | n.s. | n.s. |
| MRP, ng/mL | 2.41 (±0.25) | 2.15 (±0.1) | 2.42 (±0.19) | n.s. | n.s. | n.s. |
| TNFa, mg/dL | 15.28 (±1.05) | 307.6 (±59.18) | 275.3 (±49.17) | <0.0001 | n.s. | <0.0001 |
| IL 6, pg/mL | 6.59 (±1.76) | 5.63 (±1.86) | 4.85 (±0.81) | n.s. | n.s. | n.s. |
| Drug levels, mg/dL | n.e. | 1.45 (±0.41) | 1.78 (±0.17) | n.e. | 0.024 | n.e |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Benucci, M.; Damiani, A.; Bandinelli, F.; Russo, E.; Li Gobbi, F.; Grossi, V.; Amedei, A.; Infantino, M.; Manfredi, M. Predicting Loss of Efficacy after Non-Medical Switching: Correlation between Circulating TNF-α Levels and SB4 in Etanercept to SB4 Switchers and Naïve Patients with Rheumatic Disease. J. Pers. Med. 2022, 12, 1174. https://doi.org/10.3390/jpm12071174
Benucci M, Damiani A, Bandinelli F, Russo E, Li Gobbi F, Grossi V, Amedei A, Infantino M, Manfredi M. Predicting Loss of Efficacy after Non-Medical Switching: Correlation between Circulating TNF-α Levels and SB4 in Etanercept to SB4 Switchers and Naïve Patients with Rheumatic Disease. Journal of Personalized Medicine. 2022; 12(7):1174. https://doi.org/10.3390/jpm12071174
Chicago/Turabian StyleBenucci, Maurizio, Arianna Damiani, Francesca Bandinelli, Edda Russo, Francesca Li Gobbi, Valentina Grossi, Amedeo Amedei, Maria Infantino, and Mariangela Manfredi. 2022. "Predicting Loss of Efficacy after Non-Medical Switching: Correlation between Circulating TNF-α Levels and SB4 in Etanercept to SB4 Switchers and Naïve Patients with Rheumatic Disease" Journal of Personalized Medicine 12, no. 7: 1174. https://doi.org/10.3390/jpm12071174
APA StyleBenucci, M., Damiani, A., Bandinelli, F., Russo, E., Li Gobbi, F., Grossi, V., Amedei, A., Infantino, M., & Manfredi, M. (2022). Predicting Loss of Efficacy after Non-Medical Switching: Correlation between Circulating TNF-α Levels and SB4 in Etanercept to SB4 Switchers and Naïve Patients with Rheumatic Disease. Journal of Personalized Medicine, 12(7), 1174. https://doi.org/10.3390/jpm12071174








