An Algorithm for Elective Amputation Combined with Targeted Muscle Reinnervation in Complex Regional Pain Syndrome—A Perspective
Abstract
1. Introduction
2. Background
2.1. CRPS and Amputation
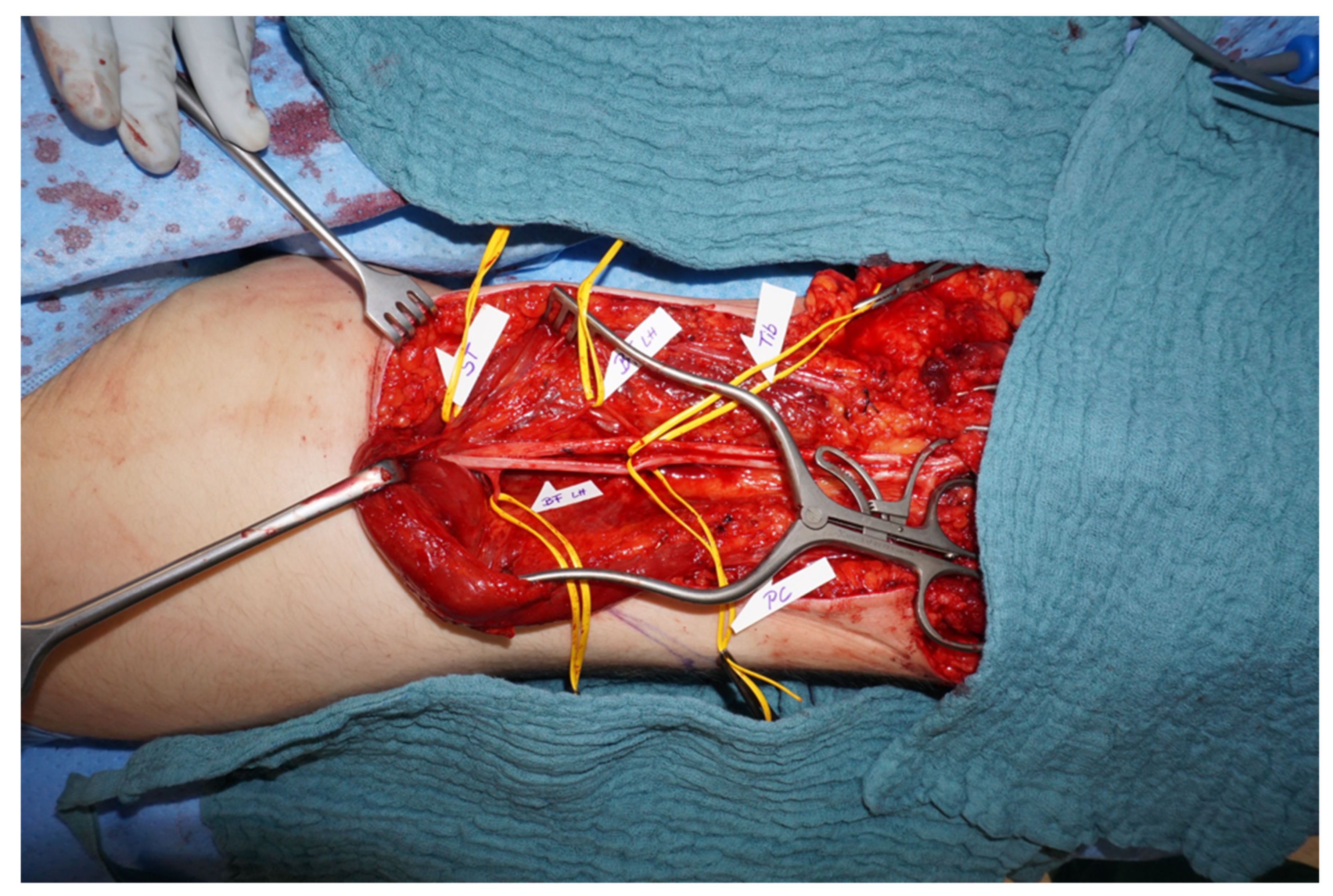
2.2. Targeted Muscle Reinnervation
2.3. Multidisciplinary Board
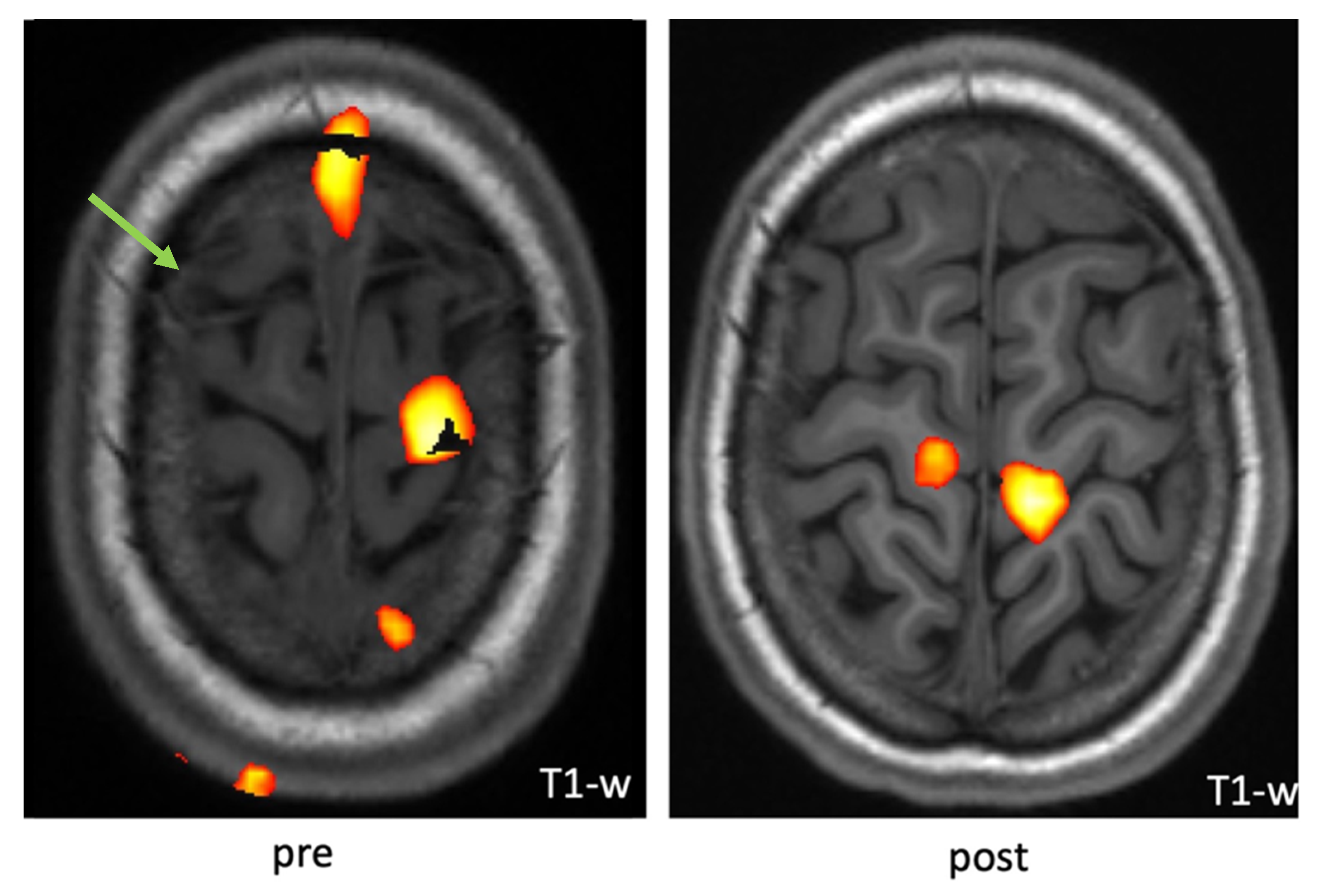
2.4. Functional Magnetic Resonance Imaging (fMRI)
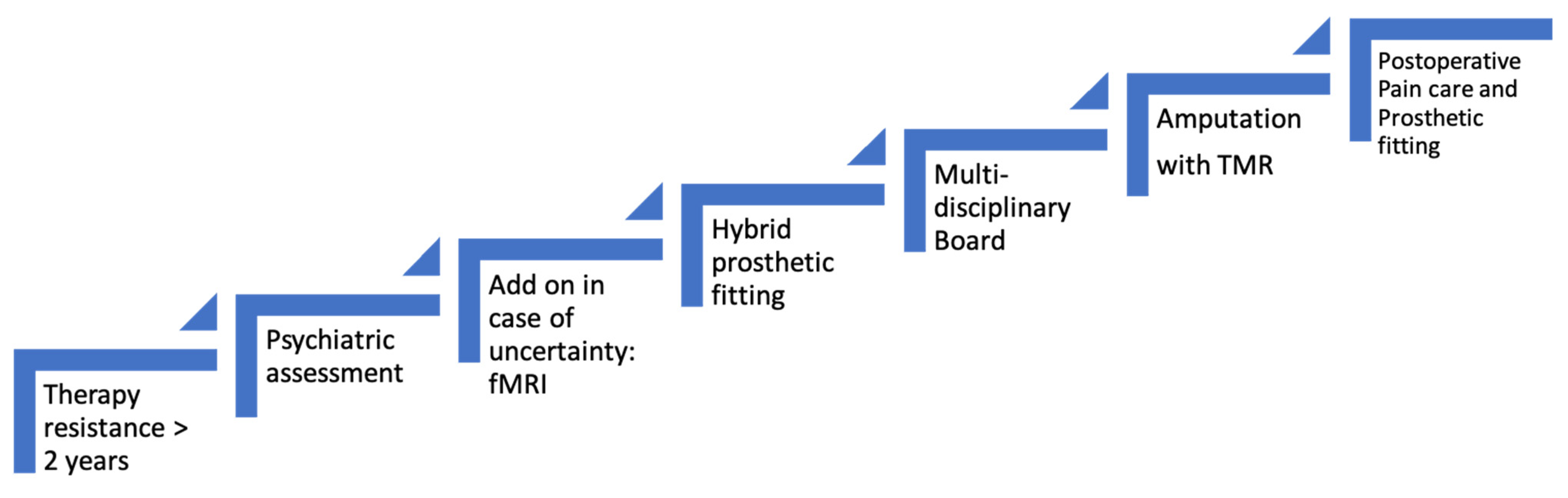
3. Advanced Algorithm for Amputation
4. Algorithm Demonstration
5. Challenges and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CRPS | complex regional pain syndrome |
| fMRI | functional magnetic resonance imaging |
| PTSD | post-traumatic stress disorder |
| TMR | targeted muscle reinnervation |
References
- Taylor, S.-S.; Noor, N.; Urits, I.; Paladini, A.; Sadhu, M.S.; Gibb, C.; Carlson, T.; Myrcik, D.; Varrassi, G.; Viswanath, O. Complex Regional Pain Syndrome: A Comprehensive Review. Pain Ther. 2021, 10, 875–892. [Google Scholar] [CrossRef] [PubMed]
- Geertzen, J.H.B.; Scheper, J.; Schrier, E.; Dijkstra, P.U. Outcomes of amputation due to long-standing therapy-resistant complex regional pain syndrome type I. J. Rehabil. Med. 2020, 52, jrm00087. [Google Scholar] [CrossRef] [PubMed]
- Schrier, E.; Dijkstra, P.U.; Zeebregts, C.J.; Wolff, A.P.; Geertzen, J.H.B. Decision making process for amputation in case of therapy resistant complex regional pain syndrome type-I in a Dutch specialist centre. Med. Hypotheses 2018, 121, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Aman, M.; Festin, C.; Sporer, M.E.; Gstoettner, C.; Prahm, C.; Bergmeister, K.D.; Aszmann, O.C. Bionic reconstruction: Restoration of extremity function with osseointegrated and mind-controlled prostheses. Wien. Klin. Wochenschr. 2019, 131, 599–607. [Google Scholar] [CrossRef] [PubMed]
- Ayyaswamy, B.; Saeed, B.; Anand, A.; Chan, L.; Shetty, V. Quality of life after amputation in patients with advanced complex regional pain syndrome: A systematic review. Efort Open Rev. 2019, 4, 533–540. [Google Scholar] [CrossRef] [PubMed]
- De Boer, K.S.; Schmitz, R.F.; Van Luijt, P.A.; Arendzen, J.H. Case Report: Functional Status After Transfemoral Amputation in Three Patients With Complex Regional Pain Syndrome. J. Prosthet. Orthot. 2007, 19, 91–93. [Google Scholar] [CrossRef]
- Dielissen, P.W.; Claassen, A.T.; Veldman, P.H.; Goris, R.J. Amputation for reflex sympathetic dystrophy. J. Bone Jt. Surg. Br. 1995, 77, 270–273. [Google Scholar] [CrossRef][Green Version]
- Bodde, M.I.; Schrier, E.; Krans, H.K.; Geertzen, J.H.; Dijkstra, P.U. Resilience in patients with amputation because of Complex Regional Pain Syndrome type I. Disabil. Rehabil. 2014, 36, 838–843. [Google Scholar] [CrossRef]
- Kuiken, T. Targeted reinnervation for improved prosthetic function. Phys. Med. Rehabil. Clin. N. Am. 2006, 17, 1–13. [Google Scholar] [CrossRef]
- Aman, M.; Sporer, M.E.; Gstoettner, C.; Prahm, C.; Hofer, C.; Mayr, W.; Farina, D.; Aszmann, O.C. Bionic hand as artificial organ: Current status and future perspectives. Artif. Organs 2019, 43, 109–118. [Google Scholar] [CrossRef]
- Stoehr, J.R.; Sood, R.; Jordan, S.W.; Dumanian, G.A. Targeted muscle reinnervation at the time of amputation in the management of complex regional pain syndrome of the lower extremity. Microsurgery 2020, 40, 852–858. [Google Scholar] [CrossRef]
- Bergmeister, K.D.; Salminger, S.; Aszmann, O.C. Targeted Muscle Reinnervation for Prosthetic Control. Hand Clin. 2021, 37, 415–424. [Google Scholar] [CrossRef]
- Kuiken, T.A.; Barlow, A.K.; Hargrove, L.; Dumanian, G.A. Targeted Muscle Reinnervation for the Upper and Lower Extremity. Tech. Orthop. 2017, 32, 109–116. [Google Scholar] [CrossRef]
- Bowen, J.B.; Ruter, D.; Wee, C.; West, J.; Valerio, I.L. Targeted Muscle Reinnervation Technique in Below-Knee Amputation. Plast. Reconstr. Surg. 2019, 143, 309–312. [Google Scholar] [CrossRef]
- Bergmeister, K.D.; Aman, M.; Muceli, S.; Vujaklija, I.; Manzano-Szalai, K.; Unger, E.; Byrne, R.A.; Scheinecker, C.; Riedl, O.; Salminger, S.; et al. Peripheral nerve transfers change target muscle structure and function. Sci. Adv. 2019, 5, eaau2956. [Google Scholar] [CrossRef]
- Bergmeister, K.D.; Vujaklija, I.; Muceli, S.; Sturma, A.; Hruby, L.A.; Prahm, C.; Riedl, O.; Salminger, S.; Manzano-Szalai, K.; Aman, M.; et al. Broadband Prosthetic Interfaces: Combining Nerve Transfers and Implantable Multichannel EMG Technology to Decode Spinal Motor Neuron Activity. Front. Neurosci. 2017, 11, 421. [Google Scholar] [CrossRef]
- Flor, H. Phantom-limb pain: Characteristics, causes, and treatment. Lancet Neurol. 2002, 1, 182–189. [Google Scholar] [CrossRef]
- Li, R.; Hettinger, P.C.; Machol, J.A.; Liu, X.; Stephenson, J.B.; Pawela, C.P.; Yan, J.-G.; Matloub, H.S.; Hyde, J.S. Cortical plasticity induced by different degrees of peripheral nerve injuries: A rat functional magnetic resonance imaging study under 9.4 Tesla. J. Brachial Plex. Peripher. Nerve Inj. 2013, 8, 4. [Google Scholar] [CrossRef]
- Ephraim, P.L.; Wegener, S.T.; MacKenzie, E.J.; Dillingham, T.R.; Pezzin, L.E. Phantom pain, residual limb pain, and back pain in amputees: Results of a national survey. Arch. Phys. Med. Rehabil. 2005, 86, 1910–1919. [Google Scholar] [CrossRef]
- Kooijman, C.M.; Dijkstra, P.U.; Geertzen, J.H.B.; Elzinga, A.; van der Schans, C.P. Phantom pain and phantom sensations in upper limb amputees: An epidemiological study. Pain 2000, 87, 33–41. [Google Scholar] [CrossRef]
- Richardson, C.; Glenn, S.; Nurmikko, T.; Horgan, M. Incidence of phantom phenomena including phantom limb pain 6 months after major lower limb amputation in patients with peripheral vascular disease. Clin. J. Pain 2006, 22, 353–358. [Google Scholar] [CrossRef]
- Midbari, A.; Suzan, E.; Adler, T.; Melamed, E.; Norman, D.; Vulfsons, S.; Eisenberg, E. Amputation in patients with complex regional pain syndrome: A comparative study between amputees and non-amputees with intractable disease. Bone Jt. J. 2016, 98-B, 548–554. [Google Scholar] [CrossRef]
- Dumanian, G.A.; Potter, B.K.; Mioton, L.M.; Ko, J.H.; Cheesborough, J.E.; Souza, J.M.; Ertl, W.J.; Tintle, S.M.; Nanos, G.P.; Valerio, I.L.; et al. Targeted Muscle Reinnervation Treats Neuroma and Phantom Pain in Major Limb Amputees: A Randomized Clinical Trial. Ann. Surg. 2019, 270, 238–246. [Google Scholar] [CrossRef]
- Harden, N.R.; Bruehl, S.; Perez, R.S.G.M.; Birklein, F.; Marinus, J.; Maihofner, C.; Lubenow, T.; Buvanendran, A.; Mackey, S.; Graciosa, J.; et al. Validation of proposed diagnostic criteria (the “Budapest Criteria”) for Complex Regional Pain Syndrome. Pain 2010, 150, 268–274. [Google Scholar] [CrossRef]
- Kotsougiani-Fischer, D.; Fischer, S.; Warszawski, J.; Gruetzner, P.A.; Reiter, G.; Hirche, C.; Kneser, U. Multidisciplinary team meetings for patients with complex extremity defects: A retrospective analysis of treatment recommendations and prognostic factors for non-implementation. BMC Surg. 2021, 21, 168. [Google Scholar] [CrossRef]
- Hilti, L.M.; Hänggi, J.; Vitacco, D.A.; Kraemer, B.; Palla, A.; Luechinger, R.; Jäncke, L.; Brugger, P. The desire for healthy limb amputation: Structural brain correlates and clinical features of xenomelia. Brain J. Neurol. 2013, 136 Pt 1, 318–329. [Google Scholar] [CrossRef]
- Gandola, M.; Zapparoli, L.; Saetta, G.; Reverberi, C.; Salvato, G.; Squarza, S.A.C.; Invernizzi, P.; Sberna, M.; Brugger, P.; Bottini, G.; et al. Brain Abnormalities in Individuals with a Desire for a Healthy Limb Amputation: Somatosensory, Motoric or Both? A Task-Based fMRI Verdict. Brain Sci. 2021, 11, 1248. [Google Scholar] [CrossRef]
- Strauss, S.; Barby, S.; Härtner, J.; Neumann, N.; Moseley, G.L.; Lotze, M. Modifications in fMRI Representation of Mental Rotation Following a 6 Week Graded Motor Imagery Training in Chronic CRPS Patients. J. Pain 2021, 22, 680–691. [Google Scholar] [CrossRef]
- Henderson, J. Updated guidelines on complex regional pain syndrome in adults✰. J. Plast. Reconstr. Aesthetic Surg. 2019, 72, 1–3. [Google Scholar] [CrossRef]
- Hruby, L.A.; Sturma, A.; Mayer, J.A.; Pittermann, A.; Salminger, S.; Aszmann, O.C. Algorithm for bionic hand reconstruction in patients with global brachial plexopathies. J. Neurosurg. 2017, 127, 1163–1171. [Google Scholar] [CrossRef]

| Level of Amputation. | Nerve | Targeted Muscle Motor Branch |
|---|---|---|
| Glenohumeral Amputation | Musculocutaneous | Clavicular part—pectoralis major |
| Ulnar | Pectoralis minor | |
| Median | Sternocostal part—pectoralis major | |
| Radial | Abdominal part—pectoralis major Latissimus dorsi | |
| Deep radial branch | Infraspinatus | |
| Above Elbow Amputation | Musculocutaneous | long head biceps brachii |
| Ulnar | Short head biceps brachii | |
| Median | Brachialis | |
| Radial | Long head/medial head triceps brachii | |
| Deep branch of the radial nerve | Lateral head triceps brachii | |
| Deep branch of the radial nerve | Brachioradialis | |
| Below Elbow Amputation | Median | Flexor digitorum superficialis |
| Ulnar | Flexor carpi ulnaris | |
| Superficial branch of the radial nerve | Anterior interosseus nerve | |
| Above Knee Amputation | Tibial | Semitendinosus |
| Peroneal | Biceps femoris | |
| Posterior cutaneous nerve | Biceps femoris | |
| Saphenous | Vastus medialis | |
| Below Knee Amputation | Posterior tibial nerve | Medial or lateral gastrocnemius |
| Deep peroneal nerve | Tibialis anterior, peroneal mm. | |
| Superficial peroneal nerve | Peroneal mm. | |
| Saphenous nerve | Medial gastrocnemius | |
| Sural nerve | Tibialis posterior |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aman, M.; Biglari, B.; Thielen, M.; Boecker, A.H.; Stolle, A.; Schwarz, D.; Gazyakan, E.; Kneser, U.; Harhaus, L. An Algorithm for Elective Amputation Combined with Targeted Muscle Reinnervation in Complex Regional Pain Syndrome—A Perspective. J. Pers. Med. 2022, 12, 1169. https://doi.org/10.3390/jpm12071169
Aman M, Biglari B, Thielen M, Boecker AH, Stolle A, Schwarz D, Gazyakan E, Kneser U, Harhaus L. An Algorithm for Elective Amputation Combined with Targeted Muscle Reinnervation in Complex Regional Pain Syndrome—A Perspective. Journal of Personalized Medicine. 2022; 12(7):1169. https://doi.org/10.3390/jpm12071169
Chicago/Turabian StyleAman, Martin, Bahram Biglari, Mirjam Thielen, Arne H. Boecker, Annette Stolle, Daniel Schwarz, Emre Gazyakan, Ulrich Kneser, and Leila Harhaus. 2022. "An Algorithm for Elective Amputation Combined with Targeted Muscle Reinnervation in Complex Regional Pain Syndrome—A Perspective" Journal of Personalized Medicine 12, no. 7: 1169. https://doi.org/10.3390/jpm12071169
APA StyleAman, M., Biglari, B., Thielen, M., Boecker, A. H., Stolle, A., Schwarz, D., Gazyakan, E., Kneser, U., & Harhaus, L. (2022). An Algorithm for Elective Amputation Combined with Targeted Muscle Reinnervation in Complex Regional Pain Syndrome—A Perspective. Journal of Personalized Medicine, 12(7), 1169. https://doi.org/10.3390/jpm12071169








