The COVID-19 Pandemic as an Impulse for the Development of Telemedicine in Primary Care in Poland
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Souza, M.; Fioretti, A.; Vincentin, A.; Botelho, R.; Vasconcellos, C. Effectiveness of telemedicine in response to the COVID-19 pandemic. Rev. Assoc. Médica Bras. 2021, 67, 1427–1431. [Google Scholar] [CrossRef] [PubMed]
- Laub, N.; Agarwal, A.; Shi, C.; Sjamsu, A.; Chaiyachati, K. Delivering Urgent Care Using Telemedicine: Insights from Experienced Clinicians at Academic Medical Centers. J. Gen. Intern. Med. 2021, 37, 707–713. [Google Scholar] [CrossRef] [PubMed]
- Mahmoud, M.; Daboos, M.; Gouda, S.; Othman, A.; Abdelmaboud, M.; Hussein, M.; Akl, M. Telemedicine (virtual clinic) effectively delivers the required healthcare service for pediatric ambulatory surgical patients during the current era of COVID-19 pandemic: A mixed descriptive study. J. Pediatr. Surg. 2022, 57, 630–636. [Google Scholar] [CrossRef] [PubMed]
- Strehle, E.; Shabde, N. One hundred years of telemedicine: Does this new technology have a place in pediatrics? Arch. Dis. Child. 2006, 91, 956–959. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bashshur, R. On the Definition and Evaluation of Telemedicine. Telemed. J. 1995, 1, 19–30. [Google Scholar] [CrossRef]
- Ryu, S. Telemedicine: Opportunities and Developments in the Member States: Report on the Second Global Survey on eHealth 2009 (Global Observatory for eHealth Series, Volume 2). Healthc. Inform. Res. 2012, 18, 153. Available online: https://apps.who.int/iris/handle/10665/44497 (accessed on 14 April 2022). [CrossRef]
- Glinkowski, W. (Ed.) Advances in International Telemedicine and eHealth. In Around the World, 1st ed.; MediPage: Warsaw, Poland, 2006; p. 171. Available online: https://www.researchgate.net/publication/273764498_ADVANCES_IN_INTERNATIONAL_TELEMEDICINE_AND_eHEALTH (accessed on 14 April 2022).
- Jacennik, B.; Wysocki, P.; Langrand, C.; Jankowska, A.K.; Sadowska, M.; Glinkowski, W. Regulacje prawne i wytyczne dobrych praktyk dla świadczenia telekonsultacji—na przykładzie Polski. In Interdyscyplinarne Wyzwania Nauk o Zdrowiu; Medical University of Bialystok: Bialystok, Poland, 2021; pp. 27–56. Available online: https://www.umb.edu.pl/photo/pliki/WNoZ_jednostki/wnoz-z-zintegrowanej-opieki-medycznej/monografie/interdyscyplinarne-wyzwania-nauk-o-zdrowiu-skompresowany.pdf (accessed on 14 April 2022).
- Sahni, M.; Choudhry, J.; Mittal, A.; Bhogal, G. Remote Musculoskeletal Consultations: A Survey of General Practitioner Registrars’ Level of Confidence, Acceptability, and Management. Cureus 2021, 13, e15084. [Google Scholar] [CrossRef]
- Byrne, M. Telehealth and the COVID-19 Pandemic. J. PeriAnesthesia Nurs. 2020, 35, 548–551. [Google Scholar] [CrossRef]
- Haque, S. Telehealth Beyond COVID-19. Psychiatr. Serv. 2021, 72, 100–103. [Google Scholar] [CrossRef]
- Moore, M.; Munroe, D. COVID-19 Brings About Rapid Changes in the Telehealth Landscape. Telemed. E-Health 2021, 27, 382–384. [Google Scholar] [CrossRef]
- Sclafani, A.; Shomorony, A.; Stewart, M.; Grunstein, E.; Overdevest, J. Telemedicine lessons learned during the COVID-19 pandemic: The augmented outpatient otolaryngology teleconsultation. Am. J. Otolaryngol. 2021, 42, 102960. [Google Scholar] [CrossRef] [PubMed]
- Regulation of the Minister of Health of 12 August 2020 on the Organizational Standard of Teleconsultations in Primary Health Care. Available online: https://isap.sejm.gov.pl/isap.nsf/DocDetails.xsp?id=WDU20200001395 (accessed on 14 April 2022).
- Kamecka, K.; Rybarczyk-Szwajkowska, A.; Staszewska, A.; Engelseth, P.; Kozlowski, R. Process of Posthospital Care Involving Telemedicine Solutions for Patients after Total Hip Arthroplasty. Int. J. Environ. Res. Public Health 2021, 18, 10135. [Google Scholar] [CrossRef] [PubMed]
- Kellish, A.S.; Hakim, A.; Shahi, A.; Gutowski, C.J.; Kleiner, M.T. The Delivery of Orthopaedic Care midst COVID-19 and Social Distancing. Arch. Bone Jt. Surg. 2021, 9, 371–378. [Google Scholar] [PubMed]
- Drake, C.; Lian, T.; Cameron, B.; Medynskaya, K.; Bosworth, H.; Shah, K. Understanding Telemedicine’s “New Normal”: Variations in Telemedicine Use by Specialty Line and Patient Demographics. Telemed. E-Health 2022, 28, 51–59. [Google Scholar] [CrossRef]
- Cadilhac, D.; Prvu Bettger, J. Health Policy and Health Services Delivery in the Era of COVID-19. Stroke 2021, 52, 2177–2179. [Google Scholar] [CrossRef]
- Wang, E.; Real, I.; David-Wang, A.; Rubio, D.A.; Gaston, C.L.; Quintos, A.J.; Dimayuga, C.; Dacanay, E. Lessons Learned: Patient Communication During the Pandemic. Malays. Orthop. J. 2021, 15, 12–15. [Google Scholar]
- Chin, B.; Nashi, N.; Lin, S.; Yik, K.; Tan, G.; Kagda, F. Telemedicine use in orthopaedics: Experience during the COVID-19 pandemic. J. Telemed. Telecare 2021, 28, 373–379. [Google Scholar] [CrossRef]
- Greif, D.; Shallop, B.; Rizzo, M.; Cade, W.; Letter, M.; Muñoz, J.; Baraga, M.; Kaplan, L. Telehealth in an Orthopedic Sports Medicine Clinic: The First 100 Patients. Telemed. E-Health 2021, 27, 1275–1281. [Google Scholar] [CrossRef]
- Lops, K. Cross-border Telemedicine. Master Health Economics, Policy and Law. 2011. Available online: http://hdl.handle.net/2105/9020 (accessed on 14 April 2022).
- Flaga-Gieruszyńska, K.; Kożybska, M.; Osman, T.; Radlińska, I.; Zabielska, P.; Karakiewicz-Krawczyk, K.; Jurczak, A.; Karakiewicz, B. Telemedicine services in the work of a doctor, dentist, nurse and midwife—Analysis of legal regulations in Poland and the possibility of their implementation on the example of selected European countries. Ann. Agric. Environ. Med. 2020, 27, 680–688. [Google Scholar] [CrossRef]
- Ordinance No. 132/2020/DSOZ of the President of the National Health Fund. Available online: https://www.nfz.gov.pl/zarzadzenia-prezesa/zarzadzenia-prezesa-nfz/zarzadzenie-nr-1322020dsoz,7225.html (accessed on 14 April 2022).
- Ramaswamy, A.; Yu, M.; Drangsholt, S.; Ng, E.; Culligan, P.; Schlegel, P.; Hu, J. Patient Satisfaction With Telemedicine During the COVID-19 Pandemic: Retrospective Cohort Study. J. Med. Internet Res. 2020, 22, e20786. [Google Scholar] [CrossRef]
- Kabala, A.; Nowacka, A.; Pawłowska, E. POZ w Polsce Struktura, Zadania, Funkcje; PZWL Wydawnictwo Lekarskie: Warsaw, Poland, 2017; pp. 9–58. [Google Scholar]
- Ustawa z Dnia 27 Października 2017 r. o Podstawowej Opiece Zdrowotnej. Available online: https://isap.sejm.gov.pl/isap.nsf/download.xsp/WDU20170002217/T/D20172217L.pdf (accessed on 14 April 2022).
- Furlepa, K.; Tenderenda, A.; Kozłowski, R.; Marczak, M.; Wierzba, W.; Śliwczyński, A. Recommendations for the Development of Telemedicine in Poland Based on the Analysis of Barriers and Selected Telemedicine Solutions. Int. J. Environ. Res. Public Health 2022, 19, 1221. [Google Scholar] [CrossRef] [PubMed]
- Wróbel, K.; Milewska, A.J.; Marczak, M.; Kozłowski, R. The Impact of the COVID-19 Pandemic on the Composition of Dietary Supplements and Functional Foods Notified in Poland. Int. J. Environ. Res. Public Health 2021, 18, 11751. [Google Scholar] [CrossRef] [PubMed]
- OECD/European Observatory on Health Systems and Policies. Country Health Profiles 2021. Available online: https://www.oecd.org/health/country-health-profiles-eu.htm (accessed on 14 April 2022).
- WHO European Centre for Primary Health Care: Annual Report of Activities 2018. 2019. Available online: https://www.euro.who.int/en/health-topics/Health-systems/primary-health-care/publications/2019/who-european-centre-for-primary-health-care-annual-report-of-activities-2018-2019 (accessed on 14 April 2022).
- Glinkowski, W.; Karlinska, M.; Karlinski, M.; Krupinski, E. Telemedicine and eHealth in Poland from 1995 to 2015. Adv. Clin. Exp. Med. 2018, 27, 277–282. [Google Scholar] [CrossRef] [PubMed]
- Ordinance No. 112/2021/DSOZ of the President of the National Health Fund of 24 June 2021, Amending the Ordinance on the Conditions for the Conclusion and Implementation of Contracts for the Provision of Healthcare Services in Primary Care. Available online: https://www.nfz.gov.pl/zarzadzenia-prezesa/zarzadzenia-prezesa-nfz/zarzadzenie-nr-1122021dsoz,7375.html (accessed on 14 April 2022).
- Bali, S.; Singh, A.J. Mobile phone consultation for community health care in rural north India. J. Telemed. Telecare 2007, 13, 421–424. [Google Scholar] [CrossRef] [PubMed]
- Day, K.; Hunter, I.; Rao, V.; Russell, G.; Roskvist, R.; Moir, F.; Gill, E.; van der Werf, B. Survey protocol for exploring video and phone use in Aotearoa New Zealand general practice: Considerations for future telehealth. BMJ Health Care Inform. 2021, 28, e100309. [Google Scholar] [CrossRef] [PubMed]
- Garcia Bermudez, I.; Gonzalez Manso, M.; Sanchez Sanchez, E.; Rodriguez Hita, A.; Rubio Rubio, M.; Suarez Fernandez, C. Usefulness and acceptance of telephone monitoring by a virtual assistant for patients with COVID-19 following discharge. Rev. Clin. Esp. 2021, 221, 464–467. [Google Scholar] [CrossRef]
- Gomes-de Almeida, S.; Marabujo, T.; do Carmo-Goncalves, M. Telemedicine satisfaction of primary care patients during COVID-19 pandemics. Semergen 2021, 47, 248–255. [Google Scholar] [CrossRef]
- Ordinance No. 39/2020/DSOZ of the President of the National Health Fund of 18 March 2020, Amending the Ordinance on the Conditions for the Conclusion and Implementation of Contracts for the Provision of Healthcare Services in the Primary Care. Available online: https://www.nfz.gov.pl/zarzadzenia-prezesa/zarzadzenia-prezesa-nfz/zarzadzenie-nr-392020dsoz,7150.html (accessed on 11 July 2022).
- Manocchia, A. Telehealth: Enhancing Care through Technology. Rhode Isl. Med. J. 2020, 103, 18–20. [Google Scholar]
- Stefanakis, M.; Batalik, L.; Papathanasiou, J.; Dipla, L.; Antoniou, V.; Pepera, G. Exercise-based cardiac rehabilitation programs in the era of COVID-19: A critical review. Rev. Cardiovasc. Med. 2021, 22, 1143. [Google Scholar] [CrossRef]
- Rogalska, A.; Syrkiewicz-Świtała, M. The role of e-health in the COVID-19 pandemic. In Zdrowie i Style Życia: Ekonomiczne, Społeczne i Zdrowotne Skutki Pandemii; Nowak, W., Szalonka, K., Eds.; Wydział Prawa, Administracji i Ekonomii Uniwersytetu Wrocławskiego: Wrocław, Poland, 2021; pp. 203–215. [Google Scholar]
- Gawinski, L.; Burzynska, M.; Kamecka, K.; Kozlowski, R. Practical Aspects of the Use of Telematic Systems in the Diagnosis of Acute Coronary Syndrome in Poland. Medicina 2022, 58, 554. [Google Scholar] [CrossRef]
- Haleem, A.; Javaid, M.; Singh, R.; Suman, R. Telemedicine for healthcare: Capabilities, features, barriers, and applications. Sens. Int. 2021, 2, 100117. [Google Scholar] [CrossRef] [PubMed]
- Moghadas, A.; Jamshidi, M.; Shaderam, M. Telemedicine in healthcare system. In Proceedings of the World Automation Congress 2008, Waikoloa, HI, USA, 28 September–2 October 2008; pp. 1–6. [Google Scholar]
- Ordinance of the Minister of Health of 5 March 2021. Amending the Ordinance on the Organizational Standard of Teleconsultation in Primary Care. Available online: https://isap.sejm.gov.pl/isap.nsf/DocDetails.xsp?id=WDU20210000427 (accessed on 5 July 2022).
- Weingart, S.; Hamrick, H.; Tutkus, S.; Carbo, A.; Sands, D.; Tess, A.; Davis, R.; Bates, D.; Phillips, R. Medication safety messages for patients via the web portal: The MedCheck intervention. Int. J. Med. Inform. 2008, 77, 161–168. [Google Scholar] [CrossRef] [PubMed]
- Galligioni, E.; Piras, E.; Galvagni, M.; Eccher, C.; Caramatti, S.; Zanolli, D.; Santi, J.; Berloffa, F.; Dianti, M.; Maines, F.; et al. Integrating mHealth in Oncology: Experience in the Province of Trento. J. Med. Internet Res. 2015, 17, e114. [Google Scholar] [CrossRef] [PubMed]
- Lim, E.; Chen, C.; Tan, E. Remote Prescription During Pandemic: Challenges and Solutions. Arch. Med. Res. 2021, 52, 450–452. [Google Scholar] [CrossRef]
- McMaster, T.; Wright, T.; Mori, K.; Stelmach, W.; To, H. Current and future use of telemedicine in surgical clinics during and beyond COVID-19: A narrative review. Ann. Med. Surg. 2021, 66, 102378. [Google Scholar] [CrossRef]
- Sasangohar, F.; Bradshaw, M.; Carlson, M.; Flack, J.; Fowler, J.; Freeland, D.; Head, J.; Marder, K.; Orme, W.; Weinstein, B.; et al. Adapting an Outpatient Psychiatric Clinic to Telehealth During the COVID-19 Pandemic: A Practice Perspective. J. Med. Internet Res. 2020, 22, e22523. [Google Scholar] [CrossRef]
- Drake, C.; Yu, J.; Lurie, N.; Kraemer, K.; Polsky, D.; Chaiyachati, K. Policies to Improve Substance Use Disorder Treatment With Telehealth During the COVID-19 Pandemic and Beyond. J. Addict. Med. 2020, 14, e139–e141. [Google Scholar] [CrossRef]
- McElroy, J.; Day, T.; Becevic, M. The Influence of Telehealth for Better Health Across Communities. Prev. Chronic Dis. 2020, 17, e64. [Google Scholar] [CrossRef]
- Atherly, A.; Van Den Broek-Altenburg, E.; Hart, V.; Gleason, K.; Carney, J. Consumer Reported Care Deferrals Due to the COVID-19 Pandemic, and the Role and Potential of Telemedicine: Cross-Sectional Analysis. JMIR Public Health Surveill. 2020, 6, e21607. [Google Scholar] [CrossRef]
- Bruce, C.; Harrison, P.; Nisar, T.; Giammattei, C.; Tan, N.; Bliven, C.; Shallcross, J.; Khleif, A.; Tran, N.; Kelkar, S.; et al. Assessing the Impact of Patient-Facing Mobile Health Technology on Patient Outcomes: Retrospective Observational Cohort Study. JMIR Mhealth Uhealth 2020, 8, e19333. [Google Scholar] [CrossRef]
- Kirby, D.; Fried, J.; Buchalter, D.; Moses, M.; Hurly, E.; Cardone, D.; Yang, S.; Virk, M.; Rokito, A.; Jazrawi, L.; et al. Patient and Physician Satisfaction with Telehealth during the COVID-19 Pandemic: Sports Medicine Perspective. Telemed. E-Health 2021, 27, 1151–1159. [Google Scholar] [CrossRef] [PubMed]
- Dobrusin, A.; Hawa, F.; Gladshteyn, M.; Corsello, P.; Harlen, K.; Walsh, C.; Alaparthi, L.; Weinstein, M.; Baig, N.; Sousa, A.; et al. Gastroenterologists and Patients Report High Satisfaction Rates with Telehealth Services during the Novel Coronavirus 2019 Pandemic. Clin. Gastroenterol. Hepatol. 2020, 18, 2393–2397.e2. [Google Scholar] [CrossRef] [PubMed]
- Keswani, A.; Brooks, J.; Khoury, P. The Future of Telehealth in Allergy and Immunology Training. J. Allergy Clin. Immunol. Pract. 2020, 8, 2135–2141. [Google Scholar] [CrossRef]
- Piera-Jiménez, J.; Etzelmueller, A.; Kolovos, S.; Folkvord, F.; Lupiáñez-Villanueva, F. Guided Internet-Based Cognitive Behavioral Therapy for Depression: Implementation Cost-Effectiveness Study. J. Med. Internet Res. 2021, 23, e27410. [Google Scholar] [CrossRef]
- Schopow, N.; Osterhoff, G.; von Dercks, N.; Girrbach, F.; Josten, C.; Stehr, S.; Hepp, P. Central COVID-19 Coordination Centers in Germany: Description, Economic Evaluation, and Systematic Review. JMIR Public Health Surveill. 2021, 7, e33509. [Google Scholar] [CrossRef] [PubMed]
- Tchero, H.; Kangambega, P.; Briatte, C.; Brunet-Houdard, S.; Retali, G.; Rusch, E. Clinical Effectiveness of Telemedicine in Diabetes Mellitus: A Meta-Analysis of 42 Randomized Controlled Trials. Telemed. E-Health 2019, 25, 569–583. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, S.F.; Sium, S.M.A.; Anwar, S. Research and Management of Rare Diseases in the COVID-19 Pandemic Era: Challenges and Countermeasures. Front. Public Health 2021, 9, 640282. [Google Scholar] [CrossRef] [PubMed]
- Carrillo de Albornoz, S.; Sia, K.L.; Harris, A. The effectiveness of teleconsultations in primary care: Systematic review. Fam. Pract. 2022, 39, 168–182. [Google Scholar] [CrossRef]
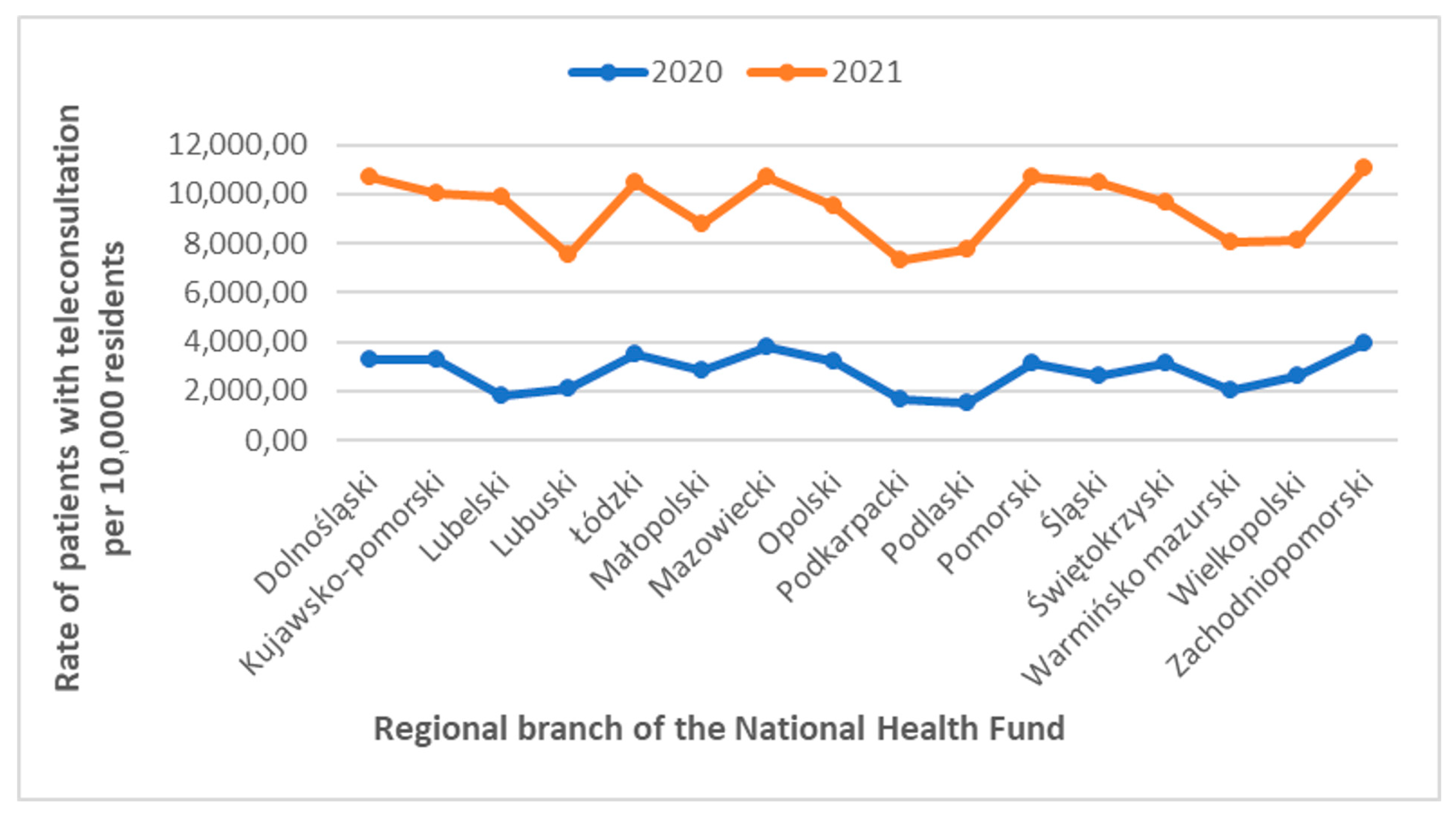
| Name of the National Health Fund Regional Branch | Number of Residents | The PCT Incidence/10,000 Residents | Increase of the PCT per National Health Fund Regional Branch (%) | ||
|---|---|---|---|---|---|
| 2020 | 2021 | 2020 | 2021 | ||
| Dolnośląski | 2,900,163 | 2,891,321 | 3299.22 | 10,681.39 | 323.8 |
| Kujawsko-Pomorski | 2,072,373 | 2,061,942 | 3289.73 | 10,026.96 | 304.8 |
| Lubelski | 2,108,270 | 2,095,258 | 1844.61 | 9856.08 | 534.3 |
| Lubuski | 1,011,592 | 1,007,145 | 2103.17 | 7540.91 | 358.5 |
| Łódzki | 2,454,779 | 2,437,970 | 3464.65 | 10,460.21 | 301.9 |
| Małopolski | 3,410,901 | 3,410,441 | 2805.13 | 8783.99 | 313.1 |
| Mazowiecki | 5,423,168 | 5,425,028 | 3785.60 | 10,718.28 | 283.1 |
| Opolski | 982,626 | 976,774 | 3228.91 | 9523.29 | 294.9 |
| Podkarpacki | 2,127,164 | 2,121,229 | 1668.08 | 7331.97 | 439.5 |
| Podlaski | 1,178,353 | 1,173,286 | 1496.44 | 7761.24 | 518.6 |
| Pomorski | 2,343,928 | 2,346,671 | 3114.57 | 10,712.22 | 343.9 |
| Śląski | 4,517,635 | 4,492,330 | 2603.38 | 10,492.96 | 403.1 |
| Świętokrzyski | 1,233,961 | 1,224,626 | 3127.25 | 9630.50 | 308 |
| Warmińsko mazurski | 1,422,737 | 1,416,495 | 2031.49 | 8052.34 | 396.4 |
| Wielkopolski | 3,498,733 | 3,496,450 | 2633.84 | 8139.02 | 309 |
| Zachodniopomorski | 1,696,193 | 1,688,047 | 3959.53 | 11,084.99 | 280 |
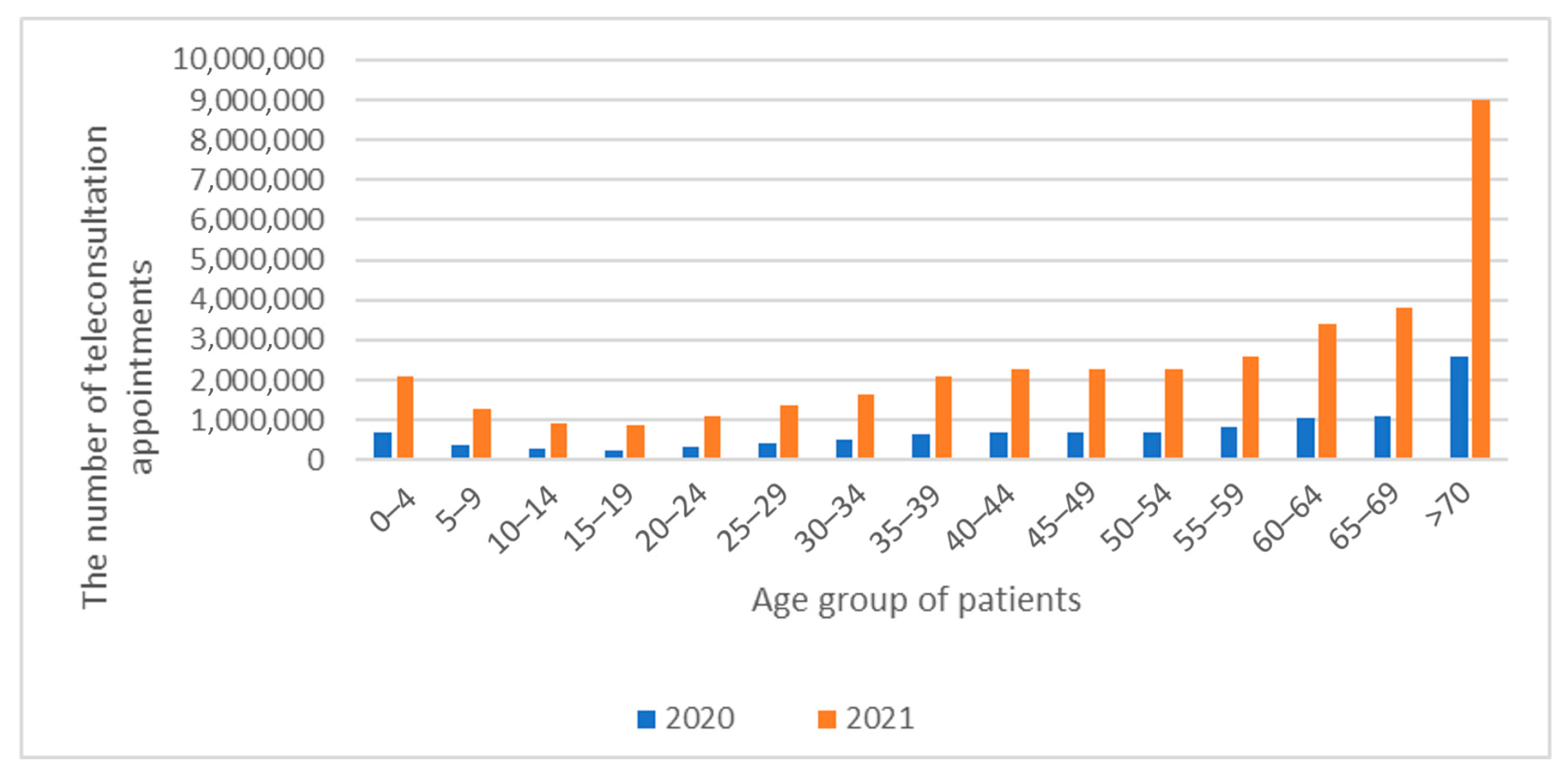
| Age Group | Population 2020 | Population 2021 | 2020 | 2021 | PCTs 2020 | PCTs 2021 | Rate 2020 | Rate 2021 |
|---|---|---|---|---|---|---|---|---|
| 0–4 | 1,911,494 | 1,876,822 | 6.09% | 5.7% | 677,058 | 2,104,353 | 3542.04 | 11,212.32 |
| 5–9 | 1,930,096 | 1,905,991 | 3.18% | 3.5% | 353,729 | 1,298,516 | 1832.70 | 6812.81 |
| 10–14 | 2,042,479 | 2,072,944 | 2.38% | 2.5% | 264,719 | 931,171 | 1296.07 | 4492.02 |
| 15–19 | 1,798,052 | 1,802,588 | 2.25% | 2.4% | 250,354 | 870,700 | 1392.36 | 4830.28 |
| 20–24 | 1,999,667 | 1,940,927 | 2.92% | 2.9% | 325,281 | 1,090,852 | 1626.68 | 5620.26 |
| 25–29 | 2,457,738 | 2,348,271 | 3.82% | 3.7% | 425,276 | 1,351,488 | 1730.36 | 5755.25 |
| 30–34 | 2,867,784 | 2,784,304 | 4.65% | 4.5% | 517,493 | 1,651,719 | 1804.50 | 5932.25 |
| 35–39 | 3,228,463 | 3,211,368 | 5.85% | 5.7% | 650,720 | 2,091,457 | 2015.57 | 6512.67 |
| 40–44 | 3,054,544 | 3,079,795 | 6.35% | 6.1% | 706,426 | 2,254,233 | 2312.71 | 7319.43 |
| 45–49 | 2,646,756 | 2,742,437 | 6.33% | 6.2% | 704,608 | 2,286,187 | 2662.16 | 8336.33 |
| 50–54 | 2,275,278 | 2,299,098 | 6.29% | 6.1% | 699,145 | 2,255,743 | 3072.79 | 9811.42 |
| 55–59 | 2,363,518 | 2,294,188 | 7.23% | 7.0% | 804,709 | 2,586,696 | 3404.71 | 11,275.00 |
| 60–64 | 2,719,848 | 2,628,254 | 9.31% | 9.2% | 1,035,921 | 3,420,617 | 3808.75 | 13,014.79 |
| 65–69 | 2,487,083 | 2,509,175 | 10.03% | 10.3% | 1,115,851 | 3,798,019 | 4486.59 | 15,136.52 |
| >70 | 4,571,373 | 4,666,062 | 23.30% | 24.4% | 2,591,857 | 9,009,907 | 5669.76 | 19,309.44 |
 | ||||||||
| Voivodeship | The Median Age in a Voivodeship 2020 | The Average Amount of PIT 2019 | The Average Amount of CIT 2019 | The Median Amount of PIT 2019 | The Median Amount of CIT 2019 | The Incidence of PCTs per 10,000 Residents in 2020 | The Incidence of PCTs per 10,000 Residents in 2021 |
|---|---|---|---|---|---|---|---|
| Dolnośląskie | 41.7 | 3608 | 167,128 | 3385 | 60,960 | 3299.22 | 10,681.39 |
| Kujawsko-Pomorskie | 42.3 | 2860 | 164,415 | 2655 | 86,730 | 3289.73 | 10,026.96 |
| Lubelskie | 41.7 | 2771 | 128,039 | 2501 | 92,028 | 1844.61 | 9856.08 |
| Lubuskie | 41.8 | 3122 | 66,918 | 3032 | 69,496 | 2103.17 | 7540.91 |
| Łódzkie | 41.6 | 3078 | 162,752 | 2844 | 128,357 | 3464.65 | 10,460.21 |
| Małopolskie | 43.3 | 3145 | 126,988 | 2953 | 118,355 | 2805.13 | 8783.99 |
| Mazowieckie | 40.4 | 3603 | 278,619 | 3008 | 128,451 | 3785.60 | 10,718.28 |
| Opolskie | 41.2 | 3204 | 129,224 | 3104 | 101,827 | 3228.91 | 9523.29 |
| Podkarpackie | 43.4 | 2818 | 130,746 | 2692 | 129,140 | 1668.08 | 7331.97 |
| Podlaskie | 40.7 | 2711 | 161,479 | 2612 | 120,793 | 1496.44 | 7761.24 |
| Pomorskie | 41.8 | 3526 | 118,704 | 3167 | 82,414 | 114.57 | 10,712.22 |
| Śląskie | 40.3 | 3890 | 143,754 | 3977 | 107,455 | 2603.38 | 10,492.96 |
| Świętokrzyskie | 43.0 | 2756 | 261,533 | 2752 | 173,287 | 3127.25 | 9630.50 |
| Warmińsko-Mazurskie | 43.0 | 2855 | 53,286 | 2716 | 36,408 | 2031.49 | 8052.34 |
| Wielkopolskie | 41.2 | 3065 | 193,677 | 2894 | 14,269 | 2633.84 | 8139.02 |
| Zachodniopomorskie | 40.5 | 3143 | 63,575 | 3023 | 46,432 | 3959.53 | 11,084.99 |
 | |||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Furlepa, K.; Śliwczyński, A.; Kamecka, K.; Kozłowski, R.; Gołębiak, I.; Cichońska-Rzeźnicka, D.; Marczak, M.; Glinkowski, W.M. The COVID-19 Pandemic as an Impulse for the Development of Telemedicine in Primary Care in Poland. J. Pers. Med. 2022, 12, 1165. https://doi.org/10.3390/jpm12071165
Furlepa K, Śliwczyński A, Kamecka K, Kozłowski R, Gołębiak I, Cichońska-Rzeźnicka D, Marczak M, Glinkowski WM. The COVID-19 Pandemic as an Impulse for the Development of Telemedicine in Primary Care in Poland. Journal of Personalized Medicine. 2022; 12(7):1165. https://doi.org/10.3390/jpm12071165
Chicago/Turabian StyleFurlepa, Kamila, Andrzej Śliwczyński, Karolina Kamecka, Remigiusz Kozłowski, Izabela Gołębiak, Dominika Cichońska-Rzeźnicka, Michał Marczak, and Wojciech Michał Glinkowski. 2022. "The COVID-19 Pandemic as an Impulse for the Development of Telemedicine in Primary Care in Poland" Journal of Personalized Medicine 12, no. 7: 1165. https://doi.org/10.3390/jpm12071165
APA StyleFurlepa, K., Śliwczyński, A., Kamecka, K., Kozłowski, R., Gołębiak, I., Cichońska-Rzeźnicka, D., Marczak, M., & Glinkowski, W. M. (2022). The COVID-19 Pandemic as an Impulse for the Development of Telemedicine in Primary Care in Poland. Journal of Personalized Medicine, 12(7), 1165. https://doi.org/10.3390/jpm12071165










