Abstract
Background: Data to support the routine use of embolic protection devices for stroke prevention during transcatheter aortic valve replacement (TAVR) are controversial. Identifying patients at high risk for peri-procedural cerebrovascular events may facilitate effective patient selection for embolic protection devices during TAVR. Aim: To generate a risk score model for stratifying TAVR patients according to peri-procedural cerebrovascular events risk. Methods and results: A total of 8779 TAVR patients from 12 centers worldwide were included. Peri-procedural cerebrovascular events were defined as an ischemic stroke or a transient ischemic attack occurring ≤24 h from TAVR. The peri-procedural cerebrovascular events rate was 1.4% (n = 127), which was independently associated with 1-year mortality (hazards ratio (HR) 1.78, 95% confidence interval (CI) 1.06–2.98, p < 0.028). The TASK risk score parameters were history of stroke, use of a non-balloon expandable valve, chronic kidney disease, and peripheral vascular disease, and each parameter was assigned one point. Each one-point increment was associated with a significant increase in peri-procedural cerebrovascular events risk (OR 1.96, 95% CI 1.56–2.45, p < 0.001). The TASK score was dichotomized into very-low, low, intermediate, and high (0, 1, 2, 3–4 points, respectively). The high-risk TASK score group (OR 5.4, 95% CI 2.06–14.16, p = 0.001) was associated with a significantly higher risk of peri-procedural cerebrovascular events compared with the low TASK score group. Conclusions: The proposed novel TASK risk score may assist in the pre-procedural risk stratification of TAVR patients for peri-procedural cerebrovascular events.
1. Introduction
The application of transcatheter aortic valve replacement (TAVR) is expanding to include lower-risk patients. Although recent studies have shown that rates of stroke after TAVR are low (0.6–3.4%) [1,2], the significant morbidity and mortality associated with it render it a priority target for preventative measures [3]. Cerebrovascular protection during TAVR has emerged as a new approach for the prevention of peri-procedural strokes. The devices are designed to capture embolic debris released during the TAVR procedure, thereby providing protection during the procedure itself as well as in the period immediately following it. However, the lack of compelling evidence for clinical stroke event reduction, the high cost, and the additional procedural complexity of device utilization have limited the widespread adoption of such technologies.
Tools to identify TAVR candidates at high risk for peri-procedural stroke may be valuable in selecting patients who require cerebrovascular protection during TAVR. Furthermore, such stratification tools may facilitate the future evaluation of the clinical efficacy of embolic protection devices among patients with different levels of risk for peri-procedural cardiovascular events. Earlier studies had evaluated predictors for post-procedural stroke [4,5,6,7], but peri-procedural cerebrovascular events represent different pathophysiology factors than those of cerebrovascular events that occur later during follow-up (i.e., >24 h). Thus, such predictors may no longer be pertinent to predicting peri-procedural events and may not be relevant for the clinical assessment of patients prior to the procedure.
The aims of the current study are to identify predictors and to design a scoring system to stratify the risk of a TAVR-associated cerebrovascular event in order to assist in identifying patients at high risk for peri-procedural strokes who may benefit from embolic protection devices during TAVR.
2. Methods
The data that support the findings of this study are available from the corresponding author upon reasonable request.
The TASK (Transcatheter Aortic valve replacement in-hoSpital stroKe) study included consecutive TAVR patients from 12 high-volume TAVR centers in Europe and the Middle East that contributed their data (Table S1). All the study patients had undergone TAVR procedures between 2007 and 2018 after careful evaluation by each institutional heart team. All patients undergoing the TAVR procedure during the designated period were included in the analysis. Patients who underwent TAVR via a non-transfemoral approach and those in whom an embolic protection device was utilized were excluded. All centers used heparin during the TAVR procedure, with a target activated clotting time of >250 s.
The participating centers were required to fill out a case report form designed specifically for this study, which included information on demographics, past medical history, and medications. Low body weight was defined as a body mass index of ≤25 kg/m2 and ischemic heart disease as any prior acute coronary syndrome, coronary intervention, or bypass surgery. Chronic kidney disease was defined as a glomerular filtration rate of <60 mL/min/1.73 m2 based on the Modification of Diet in Renal Disease equation and peripheral vascular disease as any documented atherosclerotic disease in the carotid arteries, renal arteries, or any peripheral arteries. Outcome data were collected according to the Valve Academic Research Consortium-2 definitions [8] and included post-procedural complications with a special focus on ischemic stroke, transient ischemic attack, and hemorrhagic stroke, as well as the timing of their occurrence. Any inconsistencies in the data were resolved directly with local investigators and on-site data monitoring. All patients gave written informed consent to undergo a transcatheter aortic valve procedure. The inclusion of patients was approved in each center by a local ethics committee.
The primary endpoint of peri-procedural cerebrovascular events was defined as the composite of peri-procedural ischemic stroke or transient ischemic attack occurring earlier than 24 h post-procedure. Cerebrovascular events were defined according to the Valve Academic Research Consortium-2 definitions [8] and categorized as transient ischemic attack or ischemic stroke. “Transient ischemic attack” was defined as a sensorimotor deficit that lasted 24 h or less without associated evidence of cerebral infarction in imaging studies. “Ischemic stroke” was defined as an acute neurological dysfunction lasting at least 24 h with or without evidence of infarction in imaging studies. TAVR patients for whom there was no information on a stroke event or the timing of a stroke with respect to the TAVR procedure were excluded from the analysis.
3. Statistical Analysis
Continuous data were compared with Student’s t-test and one-way ANOVA. Categorical data were compared with the chi-square test or the Fisher exact test. To assess the prognostic impact of a peri-procedural cerebrovascular event, a multivariate Cox regression analysis adjusted for age, gender, ischemic heart disease, hypertension, diabetes mellitus, peripheral vascular disease, chronic kidney disease, ejection fraction, and previous stroke was performed. Odds ratios (ORs) are reported as absolute values and 95% confidence intervals (CIs).
Candidate parameters that were considered for the derivation of the TASK score included exclusively the pre-procedural parameters that are available to the physician prior to the procedure in order to identify pre-procedural predictors for stroke.
Univariate logistic binary regression modeling was used to evaluate the ORs for peri-procedural cerebrovascular events. The final components selected for inclusion in the TASK score were derived using a resampling-based procedure. The relative impact of each of the pre-procedural parameters in predicting stroke was determined and ranked. The frequency of each candidate parameter in a final model derived from 1 of 1000 bootstrapped samples served as an indication of the importance of that parameter (Appendix A).
Parameters identified as most important were included in a multivariable logistic regression and were inspected to confirm whether equal weight can be given to each parameter so that a TASK score can be created by counting the number of present parameters for an individual. The C statistic was used to assess the performance of the multivariable model (Appendix A).
The TASK score was designed by assigning a single point to each significant factor. The TASK score was further dichotomized into four risk groups: very-low, low, intermediate, and high (0, 1, 2, 3–4 points, respectively). The prognostic value of the TASK score was assessed using a receiver operating characteristics analysis, producing an area under the curve with 95% CIs. The predicted and observed incidence of peri-procedural cerebrovascular events was compared using the Hosmer–Lemeshow test to assess the goodness-of-fit of the model. The model was regarded as having no goodness-of-fit if p < 0.05. In order to assess the possible effects of a procedural learning curve on the incidence of peri-procedural cerebrovascular events and on the TASK risk score, we defined “early” and “late” periods according to procedures performed before or after the median procedure date, respectively, and performed an interaction analysis between these two time periods.
Given the low rates of peri-procedural cerebrovascular events, a separate validation cohort was not available.
Statistical significance was accepted for a two-sided p < 0.05. The statistical analyses were performed with IBM SPSS version 25.0 (Chicago, IL, USA) and with SAS Enterprise Guide version 7.1.
4. Results
A total of 8779 patients underwent TAVR during the study period, of whom 4546 (52%) were females. The median age of the cohort was 82 years (IQR 79–86 years). The baseline characteristics of the study population are summarized in Table 1. In total, 100% of patients in the cerebrovascular group had an event, while only 0.9% of the control group had an event. The 0.9% are events that occurred after the first 24 h of the procedure. The procedure was performed under conscious sedation in the majority of patients (69%). A self-expandable valve was utilized most frequently (57%), followed by a balloon expandable valve (37%) and a mechanically expandable valve (6%). Balloon pre-dilatation was performed in one-half of the cases.

Table 1.
Demographic, clinical, and procedural characteristics of the patients according to peri-procedural cerebrovascular events.
The in-hospital adverse events rate was low, with the total in-hospital cerebrovascular event rate of 2.3%, most of which were ischemic strokes (86%), followed by transient ischemic attacks (14%), and hemorrhagic strokes (0.1%). Life-threatening or major bleeding events occurred in 7% of the patients, and the in-hospital mortality rate was 1.2% (Table 1).
4.1. Peri-Procedural Cerebrovascular Events
Stroke events within 72 h occurred in 145 patients (1.7%): 127 events occurred <24 h post-procedure (1.4%), 12 events during the second post-procedural day (0.14%), and only 6 events on the third post-procedural day (0.07%).
Evaluating patients with peri-procedural cerebrovascular events <24 h post-TAVR, the univariate binary regression analysis identified several parameters associated with peri-procedural cerebrovascular events: chronic kidney disease (OR 2.16, 95% CI 1.36–3.43), the use of non-balloon expandable valves (OR 1.89, 95% CI 1.21–2.94), peripheral vascular disease (OR 1.76, 95% CI 1.19–2.62), and a previous stroke event (OR 1.60, 95% CI 0.91–2.8) (Table 1). Of note, common risk factors for stroke, such as older age, diabetes, and atrial fibrillation, were not associated with peri-procedural cerebrovascular events (Table 1).
A multivariate binary analysis comprised of 6131 patients with complete baseline information identified four independent predictors of peri-procedural cerebrovascular events: a previous stroke (OR 1.84, 95% CI 1.01–3.34), the use of non-balloon expandable valves (OR 2.06, 95% CI 1.29–3.30), chronic kidney disease (OR 2.14, 95% CI 1.31–3.51), and peripheral vascular disease (OR 1.82, 95% CI 1.19–2.80) (Figure 1, Table S2). These findings were substantiated by bootstrap analysis (Table S2). The final components selected for inclusion in the TASK score were derived using a resampling-based procedure.
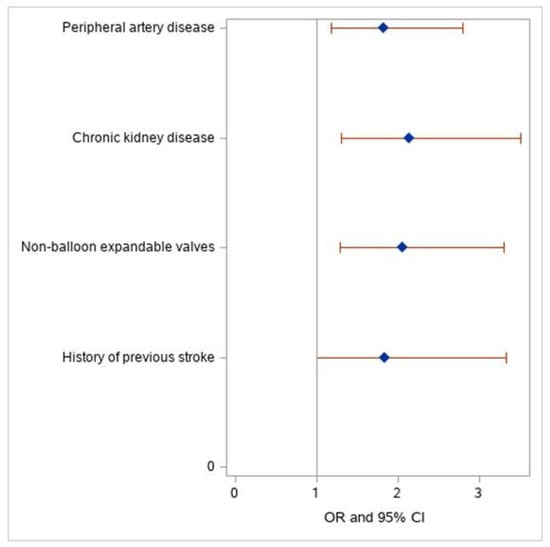
Figure 1.
Odds ratio with 95% confidence limits. Multivariate Cox regression analysis for independent predictors for peri-procedural cerebrovascular events. Forest plot graph demonstrating the odds ratio of the TASK score components for peri-procedural cerebrovascular events.
4.2. TASK Score Derivation and Validation
The TASK score was derived by assigning a single point to each of the selected components, and it ranged between 0–4, including previous stroke, the use of non-balloon expandable valves, chronic kidney disease, and peripheral vascular disease. All four variables had a statistically equivalent impact on stroke risk. The event rates were 0.7%, 0.8%, 2.1%, 3.4%, and 7.8% for each increment in the TASK score points of 0–4, respectively (Figure 2). Each one-point increment in the TASK risk score was associated with a significant increase in the risk of peri-procedural cerebrovascular events (OR 1.96, CI 1.56–2.45, p < 0.001) with a C statistic of 0.65 ± 0.03 (95% CI 0.60–0.71; Figure 3). The Hosmer–Lemeshow goodness-of-fit test demonstrated that the TASK model was well-calibrated, with a non-significant p-value of 0.84. Cross-validation of the TASK score using resampling-based metrics confirmed the robustness of the derivation model with a cross-validated C statistic of 0.641 and an optimism-corrected C statistic of 0.0038 (Table S3).
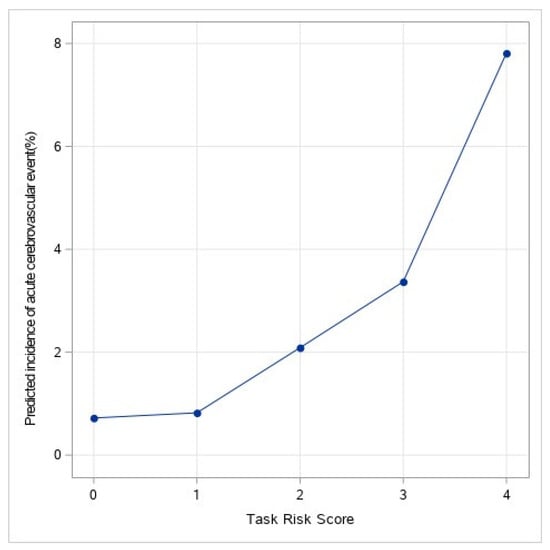
Figure 2.
Predicted incidence of acute cerebrovascular event (%). Predicted incidence of peri-procedural cerebrovascular event (%) according to the TASK score.
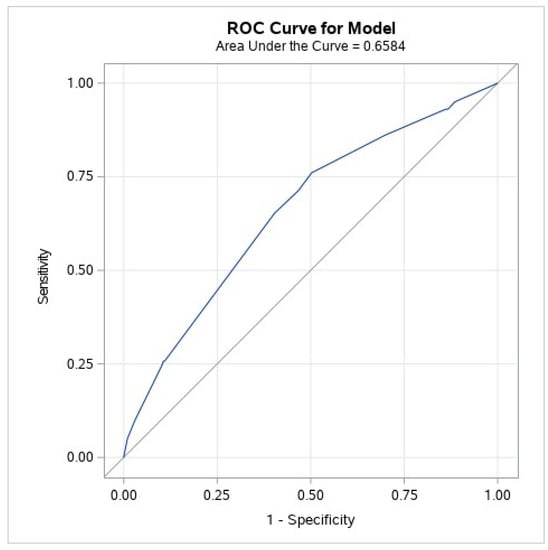
Figure 3.
ROC curve (original data). Receiver operator curve. The value of the TASK score was analyzed by receiver operator curve analysis for the prediction of peri-procedural cerebrovascular events (AUC: 0.65, 95% confidence interval 0.60–0.71).
An interaction analysis demonstrated that the association between the TASK score and peri-procedural cerebrovascular events was consistent in both the early and late study periods (HR 2.12 (1.61–4.79) for the early period vs. 1.51 (1.12–2.05) for the late period, p for interaction 0.106).
The TASK score was dichotomized into four mutually exclusive groups according to the predicted risk for peri-procedural cerebrovascular events, i.e., very-low, low, intermediate, and high (0, 1, 2, 3–4 points, respectively). Patients assigned to the low-risk group (one point) had a non-significant increase in the risk of peri-procedural cerebrovascular events compared with the very-low TASK score group (0 points) (OR 1.14 95% CI 0.42–3.06). However, patients in the intermediate-risk group (2 points) had a significant increase in the risk of peri-procedural cerebrovascular events compared with the very-low TASK score group (0 points) (OR 2.9, 95% CI 1.16–7.37) (Table 2). Moreover, patients in the high (3–4 points) TASK score group showed a significantly higher risk of peri-procedural cerebrovascular events compared with the very-low TASK score group, with an OR of 5.4 for the high TASK score (95% CI 2.06–14.16, p = 0.001) (Table 2).

Table 2.
TASK risk score *.
4.3. Prognostic Value of Peri-Procedural Cerebrovascular Events
A total of 1166 (14%) patients died within one year after undergoing a TAVR procedure. The Kaplan–Meier survival analysis demonstrated that patients who sustained peri-procedural cerebrovascular events had significantly higher 1-year mortality compared to patients who did not (p < 0.001) (Figure 4). The multivariate Cox regression analysis adjusted for age, gender, ischemic heart disease, hypertension, diabetes mellitus, peripheral vascular disease, chronic kidney disease, ejection fraction, and previous stroke found that peri-procedural cerebrovascular events were an independent risk factor for mortality, with an increased 1-year mortality risk compared to patients who did not undergo a stroke (HR 1.78, 95% CI 1.06–2.98, p < 0.028) (Table S4).
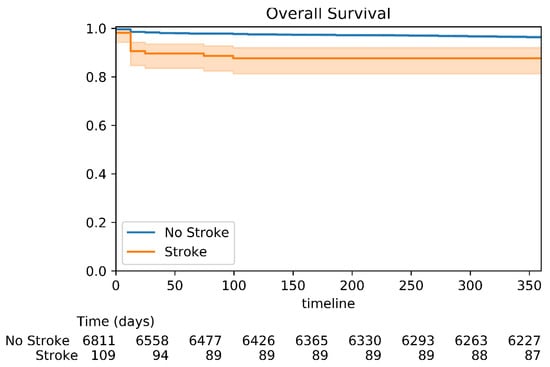
Figure 4.
Kaplan–Meier survival analysis for 1-year mortality. Kaplan–Meier survival analysis for 1-year mortality showing the probability of mortality at the 1-year follow-up according to the peri-procedural status. P-value log rank <0.001.
5. Discussion
The current study represents the first attempt to perform a multicenter, all-comer analysis to create a clinically relevant score for stratifying patients at high risk for peri-procedural cerebrovascular events during or after a TAVR procedure. The importance of the TASK score stems from the fact that although the rates of peri-procedural cerebrovascular events are low (1.4%), they are associated with increased mortality. The proposed TASK score utilizes exclusively the parameters that are known prior to the procedure to stratify patients into four distinct risk groups for peri-procedural cerebrovascular events. The TASK score may, therefore, be utilized during the pre-procedural evaluation process as guidance for the use of embolic protection devices in high-risk patients and may thus serve as a practical tool to reduce the risk of peri-procedural cerebrovascular events during TAVR or shortly thereafter.
The findings in this study, as well as those of prior studies [4,9,10], indicate that stroke after TAVR is an independent predictor of increased mortality and morbidity, such that patients who sustain an acute cerebrovascular event have a 6.5-fold increased risk of 30-day mortality [9]. Considering the expansion of TAVR to low-surgical-risk patients and younger populations, tools to identify patients at high risk for peri-procedural cerebrovascular events are essential in order to decrease the risk of disabling stroke.
A number of devices have been developed to prevent cerebrovascular embolization during the TAVR procedure [10]. Seeger and colleagues performed a retrospective analysis on the use of an embolic protection device in TAVR procedures and showed a decrease in stroke rates related to its utilization [11]. However, other randomized control trials and observational studies, including two separate meta-analyses [12,13] that evaluated several major randomized control trials [10,14,15,16,17,18], did not demonstrate a statistically significant decrease in clinically overt stroke rates with the use of embolic protection devices. Several studies have shown that embolic protection devices may decrease the formation of new brain lesions, as demonstrated in diffusion-weighted magnetic resonance imaging; however, none were associated with a reduction in clinical stroke events [10]. Therefore, embolic protection devices are used in a small minority (13%) of TAVR cases in the United States [19]. The available data, however, may support the need for a pre-procedural risk assessment tool and the use of protection devices in selected high-risk patients. The TASK score was developed to provide a simple tool to identify the patients at high risk for peri-procedural stroke, in which cerebrovascular protection may yield a high risk–benefit ratio. Furthermore, the TASK score may be utilized in the design of future clinical studies that evaluate the safety and efficacy of new embolic protection devices and contribute to the identification of a specific group of patients who will benefit most from such protection during the TAVR procedure.
Prior studies that evaluated clinical predictors of stroke after TAVR had assessed all stroke events, including those occurring late (>48 h following the procedure) [5,7]. Those studies identified parameters such as female gender, acute renal failure, chronic obstructive pulmonary disease, and low body weight as predictive factors [5,7]. Of note, those proposed predictors of stroke were not evaluated according to the timing of the event but rather to the occurrence of an event at any time during follow-up. However, as opposed to late events, the initial 24 hours after TAVR represent a unique period of vulnerability for acute cerebrovascular events. Stroke events occurring during this period account for the majority of cases [20], and they may have different pathophysiology, mainly attributable to procedural factors that are embolic in nature [21] and that result from device manipulation within the aortic arch and the calcified aortic valve. Such manipulations may lead to the dislodgement of micro-particles and the subsequent embolization of debris from an atheroma or from the valve itself [5]. Thus, the predictors of stroke following TAVR that were reported in earlier publications may not necessarily be relevant for predicting peri-procedural events.
Despite the increased risk of stroke and the different pathophysiology of peri-procedural stroke, few studies have explored the predictors of acute stroke by identifying technical procedural elements such as the balloon post-dilatation, the number of implantation attempts, and valve embolization [4,20]. However, none of these factors can be accounted for during a pre-procedural evaluation, and a more practical tool is needed in order to stratify patients according to the risk of acute stroke. Thus, the present analysis is focused upon pre-procedural parameters with potential impact on the likelihood of peri-procedural cerebrovascular events. We identified a history of stroke, the use of non-balloon expandable valves, chronic kidney disease, and peripheral vascular disease as predictors of peri-procedural stroke, and these parameters were incorporated into the new TASK score. One shared characteristic of all these factors is that they are available to the physician prior to the procedure, thereby enabling pre-procedural risk stratification. Importantly, the presence of all predictors (a TASK score = 4) was associated with a more-than-11-fold increased risk of peri-procedural cerebrovascular events compared with patients without those factors. The majority of the identified predictors are well-established predictors for stroke at any time after the procedure, i.e., peripheral artery disease, chronic kidney disease, and history of stroke. These predictors may increase the risk for stroke at any time but also during the peri-procedural period. The emergence of the use of non-balloon expandable transcatheter heart valves as a predictor for peri-procedural stroke may be related to increased rates of post-dilatation [22] or other maneuvers in the aortic arch. Of note, traditional risk factors for stroke (e.g., atrial fibrillation) were not associated with peri-procedural events, probably reflecting the homogeneity of age of this elderly group of patients and the different pathophysiologies involved in peri-procedural versus late stroke events.
6. Limitations
The present study has several limitations. The TASK score was designed to identify patients at high risk for peri-procedural cerebrovascular events in order to help clinicians identify, prior to the procedure, those patients who may benefit from the implementation of cerebrovascular protection. Therefore, procedural factors that may have a significant impact on the risk of acute stroke were not included in the present analysis despite the fact that they might influence the risk of stroke. Given the retrospective nature of the study and the variability in clinical practice among participating centers, there was no standardization in the evaluation of the patients who sustained a cerebrovascular event, no mandatory neurological evaluation by a neurologist, and no routine assessment of the modified Rankin scale. Additionally, not all patients underwent head computed tomography or brain magnetic resonance imaging. All the participating sites did, however, use the VARC-2 criteria to define cerebrovascular events. Finally, information on pre-procedural CTs was not available for all patients. Therefore, calcification severity or other CT parameters were not integrated into the model.
7. Conclusions
In conclusion, the TASK score represents a possible stratification tool for TAVR candidates according to the risk of cerebrovascular events during or immediately after the procedure. The score is comprised of clinical parameters readily available prior to undertaking the procedure. The utilization of the TASK score may serve as an additional tool for clinicians who are considering providing cerebrovascular protection during a TAVR procedure to a given patient.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jpm12071056/s1, Table S1: Participating centers and personnel; Table S2: Multivariate logistic regression analysis for the risk of peri-procedural cerebrovascular events; Table S3: C statistic, optimism-corrected C statistic, and cross-validated C statistic; Table S4: Multivariate Cox regression analysis for the risk of mortality at 1 year.
Author Contributions
Conceptualization, A.B., A.S. (Amit Segev), E.M. and I.M.B.; methodology: A.B., E.M. and I.M.B.; formal analysis, A.B., E.M. and I.M.B.; investigation, A.B., E.M. and I.M.B.; resources, A.B., A.S. (Amit Segev), E.M., A.S. (Alexander Sedaghat), A.F., M.S., R.K., A.L., J.M.D.L.T.H., L.S., D.M., N.V.R., A.G.Z., P.R., J.-M.S., A.S. (Arie Steinvil), F.M., K.O., G.I., D.-H.L., O.D.B., F.M., K.v.d.W., J.S., D.T. and I.M.B.; supervision, A.S. (Amit Segev), E.M. and I.M.B.; data curation, A.B., A.S. (Amit Segev), E.M., A.S. (Alexander Sedaghat), A.F., M.S., R.K., A.L., J.M.D.L.T.H., L.S., D.M., N.V.R., A.G.Z., P.R., J.-M.S., A.S. (Arie Steinvil), F.M., K.O., G.I., D.-H.L., O.D.B., F.M., K.v.d.W., J.S., D.T. and I.M.B.; supervision, A.S. (Amit Segev), E.M. and I.M.B. writing—original draft preparation, A.B.; writing—review and editing, A.S., E.M. and I.M.B.; visualization, A.B., A.S. (Amit Segev), E.M., A.S. (Alexander Sedaghat), A.F., M.S., R.K., A.L., J.M.D.L.T.H., L.S., D.M., N.V.R., A.G.Z., P.R., J.-M.S., A.S. (Arie Steinvil), F.M., K.O., G.I., D.-H.L., O.D.B., F.M., K.v.d.W., J.S., D.T. and I.M.B.; supervision, A.S. (Amit Segev), E.M. and I.M.B.; project administration, A.B., A.S. (Amit Segev), E.M., A.S. (Alexander Sedaghat), A.F., M.S., R.K., A.L., J.M.D.L.T.H., L.S., D.M., N.V.R., A.G.Z., P.R., J.-M.S., A.S. (Arie Steinvil), F.M., K.O., G.I., D.-H.L., O.D.B., F.M., K.v.d.W., J.S., D.T. and I.M.B.; supervision, A.S. (Amit Segev), E.M. and I.M.B.; funding acquisition, I.M.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The regional ethical review board at each site approved the trial protocol, and the trial was conducted according to the principles of the Declaration of Helsinki.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy issues.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| TAVR | transcatheter aortic valve replacement |
| TASK | Transcatheter Aortic valve replacement in-hoSpital stroKe study |
| OR | odds ratio |
| CI | confidence interval |
Appendix A
Appendix A.1. Statistical Analysis
Categorical variables are reported as frequencies and percentages and continuous variables as means and standard deviations. Continuous data were compared with Student’s t-test and one-way ANOVA. Categorical data were compared with the chi-square test or the Fisher exact test. To assess the prognostic impact of a peri-procedural cerebrovascular event, a multivariate Cox regression analysis adjusted for age, gender, ischemic heart disease, hypertension, diabetes mellitus, peripheral vascular disease, chronic renal disease, ejection fraction, and previous stroke was performed. Odds ratios (ORs) are reported as absolute values and 95% confidence intervals (CIs).
Appendix A.2. TASK Score Derivation
Candidate parameters that were considered for the derivation of the TASK score included exclusively the pre-procedural parameters that are available to the physician prior to the procedure in order to identify pre-procedural predictors for stroke.
Univariate logistic binary regression modeling was used to evaluate the OR for peri-procedural cerebrovascular events. The final components selected for inclusion in the TASK score were derived using a resampling-based procedure, which aims to incorporate model uncertainty and, thus, enhance model stability, which is the robustness of the selected model to small perturbations of the dataset [23]. The relative impact of each of the pre-procedural parameters in predicting stroke was determined and ranked. The frequency of each candidate parameter in a final model derived from 1 of 1000 bootstrapped samples served as an indication of the importance of that parameter. In each of the bootstrapped samples (drawn with replacement from the dataset), a stepwise selection procedure was used, where the final model was chosen based on optimizing the Schwarz Bayesian information criterion. The factors selected in at least 20% of samples were identified as most important (Figure A1). This resampling-based approach was implemented using the GLMSELECT procedure in SAS software, which supports a variety of model selection models. While the procedure fits an ordinary regression model, as discussed by Cohen et al. [24], a selection of good predictors for a logistic model may be identified by running the procedure against a binary target.

Figure A1.
GLMSELECT Effect Selection in at Least 20% of the samples for Post CVA in 24 hours.
Parameters identified as most important were included in a multivariable logistic regression and inspected to confirm whether equal weight can be given to each parameter so that a TASK score can be created by counting the number of present parameters for an individual. The C statistic was used to assess the performance of the multivariable model, including the final factors (Appendix A).
Resampling-based metrics were utilized to preclude optimistic estimation of the C statistic due to the overfitting of the models [25]: the optimism-corrected C statistic and the cross-validated C statistic. The optimism-corrected C statistic was derived by resampling the original data to produce 200 datasets. The predictive model was fitted to each of the 200 data sets in turn. Each fitted model was then applied to both the resampled dataset from which it was generated and to the original dataset. The C statistics of both methods were calculated, and the delta C statistic was calculated. The average of these 200 samples formed an estimate of optimism.
The TASK score was designed by assigning a single point to each significant factor. The TASK score was further dichotomized into four risk groups: low, intermediate, high, and very high (0, 1, 2, 3–4 points, respectively). The prognostic value of the TASK score was assessed using a receiver operating characteristics (ROC) analysis, producing an area under the curve with 95% CIs. The predicted and observed incidences of peri-procedural cerebrovascular events were compared using the Hosmer–Lemeshow test to assess the goodness-of-fit of the model. The model was regarded as having no goodness-of-fit if p < 0.05. In order to assess the possible effects of a procedural learning curve on the incidence of peri-procedural cerebrovascular events and on the TASK risk score, we defined “early” and “late” periods according to procedures performed before or after the median procedure date, respectively.
References
- Popma, J.J.; Deeb, G.M.; Yakubov, S.J.; Mumtaz, M.; Gada, H.; O’Hair, D.; Bajwa, T.; Heiser, J.C.; Merhi, W.; Kleiman, N.S.; et al. Transcatheter Aortic-Valve Replacement with a Self-Expanding Valve in Low-Risk Patients. N. Engl. J. Med. 2019, 380, 1706–1715. [Google Scholar] [CrossRef]
- Mack, M.J.; Leon, M.B.; Thourani, V.H.; Makkar, R.; Kodali, S.K.; Russo, M.; Kapadia, S.R.; Malaisrie, S.C.; Cohen, D.J.; Pibarot, P.; et al. Transcatheter Aortic-Valve Replacement with a Balloon-Expandable Valve in Low-Risk Patients. N. Engl. J. Med. 2019, 380, 1695–1705. [Google Scholar] [CrossRef] [PubMed]
- Eggebrecht, H.; Schmermund, A.; Voigtländer, T.; Kahlert, P.; Erbel, R.; Mehta, R.H. Risk of stroke after transcatheter aortic valve implantation (TAVI): A meta-analysis of 10,037 published patients. EuroIntervention 2012, 8, 129–138. [Google Scholar] [CrossRef] [PubMed]
- Kapadia, S.R.; Kodali, S.; Makkar, R.; Mehran, R.; Lazar, R.M.; Zivadinov, R.; Dwyer, M.G.; Jilaihawi, H.; Virmani, R.; Anwaruddin, S.; et al. Protection Against Cerebral Embolism During Transcatheter Aortic Valve Replacement. J. Am. Coll. Cardiol. 2017, 69, 367–377. [Google Scholar] [CrossRef] [PubMed]
- Stortecky, S.; Windecker, S.; Pilgrim, T.; Heg, D.; Buellesfeld, L.; Khattab, A.A.; Huber, C.; Gloekler, S.; Nietlispach, F.; Mattle, H.; et al. Cerebrovascular accidents complicating transcatheter aortic valve implantation: Frequency, timing and impact on outcomes. EuroIntervention 2012, 88, 62–70. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tay, E.L.W.; Gurvitch, R.; Wijesinghe, N.; Nietlispach, F.; Nielispach, F.; Wood, D.; Cheung, A.; Ye, J.; Lichtenstein, S.V.; Carere, R.; et al. A high-risk period for cerebrovascular events exists after transcatheter aortic valve implantation. JACC. Cardiovasc. Interv. 2011, 4, 1290–1297. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bosmans, J.; Bleiziffer, S.; Gerckens, U.; Wenaweser, P.; Brecker, S.; Tamburino, C.; Linke, A. The Incidence and Predictors of Early- and Mid-Term Clinically Relevant Neurological Events After Transcatheter Aortic Valve Replacement in Real-World Patients. J. Am. Coll. Cardiol. 2015, 66, 209–217. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kappetein, A.P.; Head, S.J.; Généreux, P.; Piazza, N.; van Mieghem, N.M.; Blackstone, E.H.; Brott, T.G.; Cohen, D.J.; Cutlip, D.E.; van Es, G.-A.; et al. Updated standardized endpoint definitions for transcatheter aortic valve implantation: The Valve Academic Research Consortium-2 consensus document†. Eur. Heart J. 2012, 33, 2403–2418. [Google Scholar] [CrossRef]
- Muralidharan, A.; Thiagarajan, K.; Van Ham, R.; Gleason, T.G.; Mulukutla, S.; Schindler, J.T.; Jeevanantham, V.; Thirumala, P.D. Meta-Analysis of Perioperative Stroke and Mortality in Transcatheter Aortic Valve Implantation. Am. J. Cardiol. 2016, 118, 1031–1045. [Google Scholar] [CrossRef]
- Nazif, T.M.; Moses, J.; Sharma, R.; Dhoble, A.; Rovin, J.; Brown, D.; Horwitz, P.; Makkar, R.; Stoler, R.; Forrest, J.; et al. Randomized Evaluation of TriGuard 3 Cerebral Embolic Protection After Transcatheter Aortic Valve Replacement: REFLECT II. JACC Cardiovasc. Interv. 2021, 14, 515–527. [Google Scholar] [CrossRef]
- Van Mieghem, N.M.; Van Gils, L.; Ahmad, H.; Van Kesteren, F.; Van Der Werf, H.W.; Brueren, G.; Storm, M.; Lenzen, M.; Daemen, J.; Van Den Heuvel, A.F.M.; et al. Filter-based cerebral embolic protection with transcatheter aortic valve implantation: The randomised MISTRAL-C trial. EuroIntervention 2016, 12, 499–507. [Google Scholar] [CrossRef] [PubMed]
- Haussig, S.; Mangner, N.; Dwyer, M.G.; Lehmkuhl, L.; Lücke, C.; Woitek, F.; Holzhey, D.M.; Mohr, F.W.; Gutberlet, M.; Zivadinov, R.; et al. Effect of a Cerebral Protection Device on Brain Lesions Following Transcatheter Aortic Valve Implantation in Patients With Severe Aortic Stenosis. JAMA 2016, 316, 592. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, Y.; Howard, J.P. Meta-Analysis of Usefulness of Cerebral Embolic Protection During Transcatheter Aortic Valve Implantation. Am. J. Cardiol. 2021, 146, 69–73. [Google Scholar] [CrossRef] [PubMed]
- Lansky, A.J.; Schofer, J.; Tchetche, D.; Stella, P.; Pietras, C.G.; Parise, H.; Abrams, K.; Forrest, J.K.; Cleman, M.; Reinöhl, J.; et al. A prospective randomized evaluation of the TriGuardTM HDH embolic deflection device during transcatheter aortic valve implantation: Results from the DEFLECT III trial. Eur. Heart J. 2015, 36, 2070–2078. [Google Scholar] [CrossRef] [PubMed]
- Sobieski, M.A., II; Pappas, P.S.; Tatooles, A.J.; Slaughter, M.S. Embol-X Intra-Aortic Filtration System: Capturing Particulate Emboli in the Cardiac Surgery Patient. J. Extra. Corpor. Technol. 2005, 37, 222. [Google Scholar]
- Gasior, T.; Mangner, N.; Bijoch, J.; Wojakowski, W. Cerebral embolic protection systems for transcatheter aortic valve replacement. J. Interv. Cardiol. 2018, 31, 891–898. [Google Scholar] [CrossRef] [Green Version]
- Kahlert, P.; Knipp, S.C.; Schlamann, M.; Thielmann, M.; Al-Rashid, F.; Weber, M.; Johansson, U.; Wendt, D.; Jakob, H.G.; Forsting, M.; et al. Silent and Apparent Cerebral Ischemia After Percutaneous Transfemoral Aortic Valve Implantation. Circulation 2010, 121, 870–878. [Google Scholar] [CrossRef] [Green Version]
- Nombela-Franco, L.; Webb, J.G.; de Jaegere, P.P.; Toggweiler, S.; Nuis, R.-J.; Dager, A.E.; Amat-Santos, I.J.; Cheung, A.; Ye, J.; Binder, R.K.; et al. Timing, Predictive Factors, and Prognostic Value of Cerebrovascular Events in a Large Cohort of Patients Undergoing Transcatheter Aortic Valve Implantation. Circulation 2012, 126, 3041–3053. [Google Scholar] [CrossRef]
- Butala, N.M.; Makkar, R.; Secemsky, E.A.; Gallup, D.; Marquis-Gravel, G.; Kosinski, A.S.; Vemulapalli, S.; Valle, J.A.; Bradley, S.M.; Chakravarty, T.; et al. Cerebral Embolic Protection and Outcomes of Transcatheter Aortic Valve Replacement: Results from the TVT Registry. Circulation 2021, 143, 2229–2240. [Google Scholar] [CrossRef]
- Giustino, G.; Sorrentino, S.; Mehran, R.; Faggioni, M.; Dangas, G. Cerebral Embolic Protection During TAVR: A Clinical Event Meta-Analysis. J. Am. Coll. Cardiol. 2017, 69, 465–466. [Google Scholar] [CrossRef]
- Armijo, G.; Nombela-Franco, L.; Tirado-Conte, G. Cerebrovascular Events After Transcatheter Aortic Valve Implantation. Front. Cardiovasc. Med. 2018, 5, 104. [Google Scholar] [CrossRef]
- Fink, N.; Segev, A.; Kornowski, R.; Finkelstein, A.; Assali, A.; Rozenbaum, Z.; Vaknin-Assa, H.; Halkin, A.; Fefer, P.; Ben-Shoshan, J.; et al. Balloon dilatation and outcome among patients undergoing trans-femoral aortic valve replacement. Int. J. Cardiol. 2017, 230, 537–541. [Google Scholar] [CrossRef] [PubMed]
- Heinze, G.; Wallisch, C.; Dunkler, D. Variable selection—A review and recommendations for the practicing statistician. Biom. J. 2018, 60, 431–449. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cohen, R.A. Introducing the GLMSELECT Procedure for Model Selection. In Proceedings of the Thirty-First Annual SAS Users Group International Conference, San Francisco, CA, USA, 26–29 March 2006. [Google Scholar]
- Smith, G.C.S.; Seaman, S.R.; Wood, A.M.; Royston, P.; White, I.R. Correcting for Optimistic Prediction in Small Data Sets. Am. J. Epidemiol. 2014, 180, 318–324. [Google Scholar] [CrossRef] [PubMed] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).