Single-Level Anterior Cervical Discectomy and Interbody Fusion: A Comparison between Porous Tantalum and Polyetheretherketone Cages
Abstract
:1. Introduction
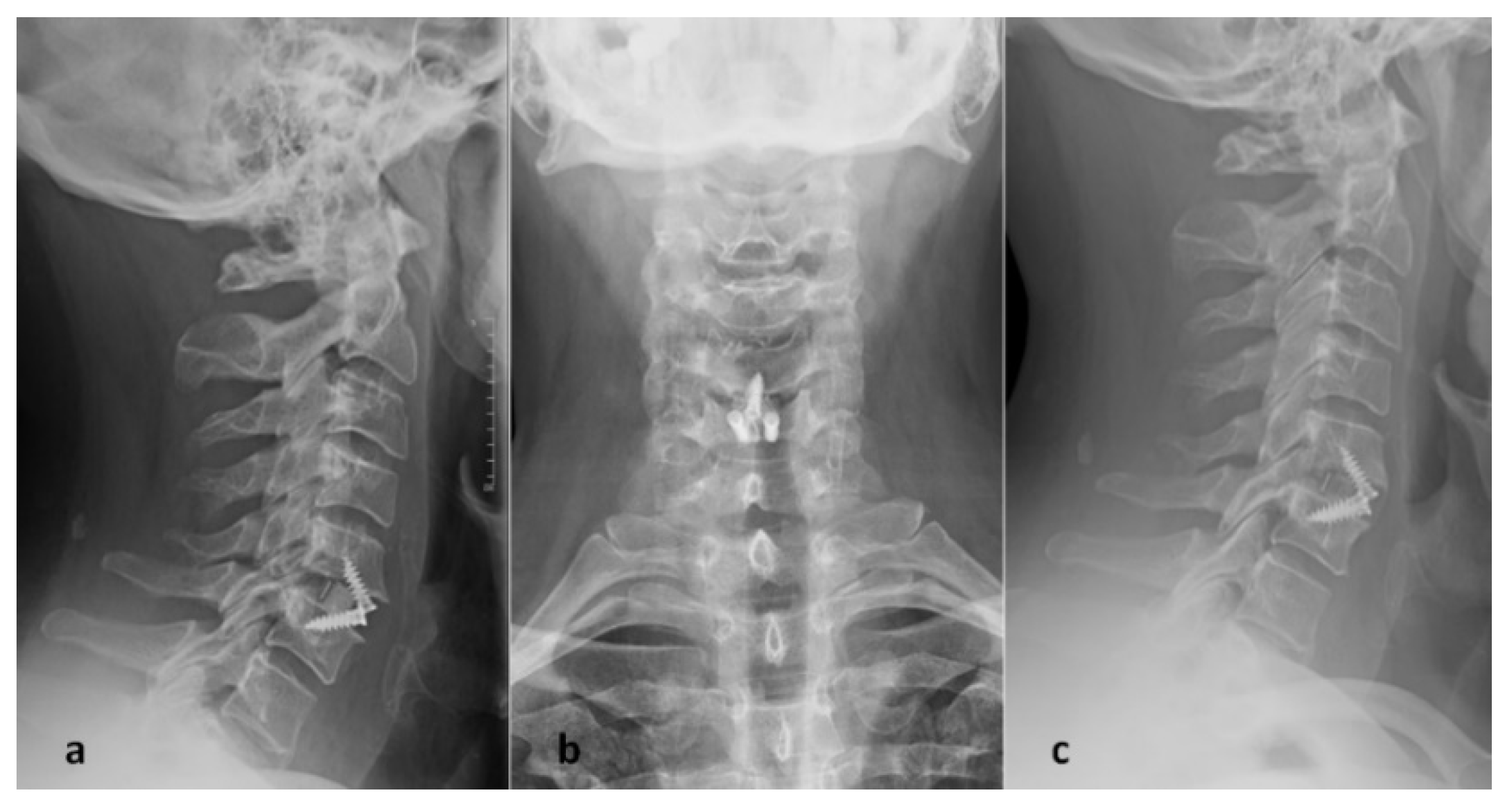
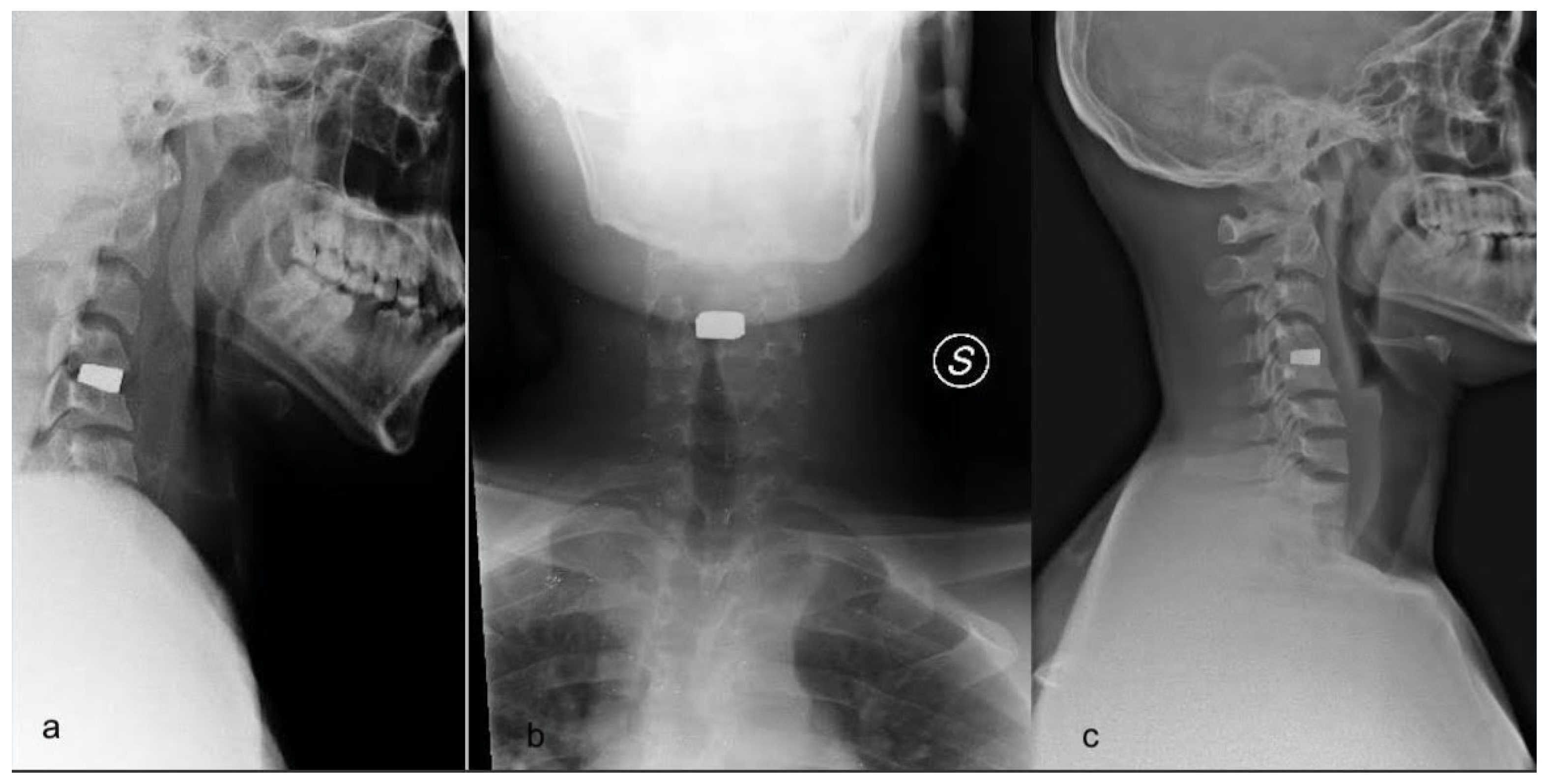
2. Materials and Methods
2.1. Patient Selection
2.2. Operative Techniques
2.3. Post-Operative Management
2.4. Clinical and Radiological Data
2.5. Statistical Analysis
3. Results
3.1. Demographic and Operative Data
3.2. Clinical Outcome
3.3. Radiographic Outcome
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Samartzis, D.; Shen, F.H.; Goldberg, E.J.; An, H.S. Is autograft the gold standard in achieving radiographic fusion in one-level anterior cervical discectomy and fusion with rigid anterior plate fixation? Spine 2005, 30, 1756–1761. [Google Scholar] [CrossRef] [PubMed]
- Yue, W.M.; Brodner, W.; Highland, T.R. Long-term results after anterior cervical discectomy and fusion with allograft and plating: A 5- to 11-year radiologic and clinical follow-up study. Spine 2005, 30, 2138–2144. [Google Scholar] [CrossRef] [PubMed]
- Bobyn, J.D.; Stackpool, G.J.; Hacking, S.A.; Tanzer, M.; Krygier, J.J. Characteristics of bone ingrowth and interface mechanics of a new porous tantalum biomaterial. J. Bone Jt. Surg. Br. Vol. 1999, 81, 907–914. [Google Scholar] [CrossRef]
- Cohen, R. A porous tantalum trabecular metal: Basic science. Am. J. Orthop. 2002, 31, 216–217. [Google Scholar]
- Levine, B.R.; Sporer, S.; Poggie, R.A.; Della Valle, C.J.; Jacobs, J.J. Experimental and clinical performance of porous tantalum in orthopedic surgery. Biomaterials 2006, 27, 4671–4681. [Google Scholar] [CrossRef]
- Levi, A.D.; Choi, W.G.; Keller, P.J.; Heiserman, J.E.; Sonntag, V.K.; Dickman, C.A. The radiographic and imaging characteristics of porous tantalum implants within the human cervical spine. Spine 1998, 23, 1245–1250. [Google Scholar] [CrossRef]
- Papacci, F.; Rigante, L.; Fernandez, E.; Meglio, M.; Montano, N. Anterior cervical discectomy and interbody fusion with porous tantalum implant. Results in a series with long-term follow-up. J. Clin. Neurosci. 2016, 33, 159–162. [Google Scholar] [CrossRef]
- Fernandez-Fairen, M.; Alvarado, E.; Torres, A. Eleven-Year Follow-Up of Two Cohorts of Patients Comparing Stand-Alone Porous Tantalum Cage Versus Autologous Bone Graft and Plating in Anterior Cervical Fusions. World Neurosurg. 2019, 122, e156–e167. [Google Scholar] [CrossRef]
- Kurtz, S. PEEK Biomaterials Handbook; Elsevier Inc.: Amsterdam, The Netherlands, 2012. [Google Scholar]
- AlOtaibi, N.; Naudi, K.; Conway, D.; Ayoub, A. The current state of PEEK implant osseointegration and future perspectives: A systematic review. Eur. Cells Mater. 2020, 40, 1–20. [Google Scholar] [CrossRef]
- Gercek, E.; Arlet, V.; Delisle, J.; Marchesi, D. Subsidence of stand-alone cervical cages in anterior interbody fusion: Warning. Eur. Spine J. 2003, 12, 513–516. [Google Scholar] [CrossRef] [Green Version]
- Cho, H.J.; Hur, J.W.; Lee, J.B.; Han, J.S.; Cho, T.H.; Park, J.Y. Cervical Stand-Alone Polyetheretherketone Cage versus Zero-Profile Anchored Spacer in Single-Level Anterior Cervical Discectomy and Fusion: Minimum 2-Year Assessment of Radiographic and Clinical Outcome. J. Korean Neurosurg. Soc. 2015, 58, 119–124. [Google Scholar] [CrossRef] [PubMed]
- Bridwell, K.H.; Lenke, L.G.; McEnery, K.W.; Baldus, C.; Blanke, K. Anterior fresh frozen structural allografts in the thoracic and lumbar spine. Do they work if combined with posterior fusion and instrumentation in adult patients with kyphosis or anterior column defects? Spine 1995, 20, 1410–1418. [Google Scholar] [CrossRef] [PubMed]
- Silber, J.S.; Anderson, D.G.; Daffner, S.D.; Brislin, B.T.; Leland, J.M.; Hilibrand, A.S.; Vaccaro, A.R.; Albert, T.J. Donor site morbidity after anterior iliac crest bone harvest for single-level anterior cervical discectomy and fusion. Spine 2003, 28, 134–139. [Google Scholar] [CrossRef] [PubMed]
- Xiao, S.; Liang, Z.; Wei, W.; Ning, J. Zero-profile anchored cage reduces risk of postoperative dysphagia compared with cage with plate fixation after anterior cervical discectomy and fusion. Eur. Spine J. 2017, 26, 975–984. [Google Scholar] [CrossRef]
- Karikari, I.O.; Jain, D.; Owens, T.R.; Gottfried, O.; Hodges, T.R.; Nimjee, S.M.; Bagley, C.A. Impact of subsidence on clinical outcomes and radiographic fusion rates in anterior cervical discectomy and fusion: A systematic review. Clin. Spine Surg. 2014, 27, 1–10. [Google Scholar] [CrossRef]
- Yoo, M.; Kim, W.H.; Hyun, S.J.; Kim, K.J.; Jahng, T.A.; Kim, H.J. Comparison between Two Different Cervical Interbody Fusion Cages in One Level Stand-alone ACDF: Carbon Fiber Composite Frame Cage Versus Polyetheretherketone Cage. Korean J. Spine 2014, 11, 127–135. [Google Scholar] [CrossRef] [Green Version]
- Kwon, O.I.; Son, D.W.; Lee, S.W.; Song, G.S. Comparison of Radiologic Outcomes of Different Methods in Single-Level Anterior Cervical Discectomy and Fusion. Korean J. Spine 2016, 13, 91–96. [Google Scholar] [CrossRef]
- Niu, C.C.; Liao, J.C.; Chen, W.J.; Chen, L.H. Outcomes of interbody fusion cages used in 1 and 2-levels anterior cervical discectomy and fusion: Titanium cages versus polyetheretherketone (PEEK) cages. Clin. Spine Surg. 2010, 23, 310–316. [Google Scholar] [CrossRef]
- Cabraja, M.; Oezdemir, S.; Koeppen, D.; Kroppenstedt, S. Anterior cervical discectomy and fusion: Comparison of titanium and polyetheretherketone cages. BMC Musculoskelet. Disord. 2012, 13, 172. [Google Scholar] [CrossRef] [Green Version]
- Katzer, A.; Marquardt, H.; Westendorf, J.; Wening, J.V.; von Foerster, G. Polyetheretherketone-cytotoxicity and mutagenicity in vitro. Biomaterials 2002, 23, 1749–1759. [Google Scholar] [CrossRef]
- Toth, J.M.; Wang, M.; Estes, B.T.; Scifert, J.L.; Seim, H.B.; Turner, A.S. Polyetheretherketone as a biomaterial for spinal applications. Biomaterials 2006, 27, 324–334. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, W.J.; Jiang, L.S.; Liang, Y.; Dai, L.Y. Cage subsidence does not, but cervical lordosis improvement does affect the long-term results of anterior cervical fusion with stand-alone cage for degenerative cervical disc disease: A retrospective study. Eur. Spine J. 2012, 21, 1374–1382. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Demetriades, A.K.; Tessitore, E. External cervical orthosis (hard collar) after ACDF: Have we moved forward? Acta Neurochir. 2020, 162, 327–328. [Google Scholar] [CrossRef] [PubMed]
| Variable | Tantalum | PEEK | p-Value |
|---|---|---|---|
| N° of patients | 38 | 31 | - |
| Sex (male:female) | 15:23 | 14:17 | 0.634 |
| Age (years) | 41 ± 6.3 | 50 ± 10.5 | <0.001 |
| Smoke (yes:no) | 16:22 | 14:17 | 0.101 |
| Follow-up (days) | 616.7 ± 93 | 544.3 ± 114.5 | 0.016 |
| Operative time | 100.4 ± 25.2 | 78.9 ± 19.2 | <0.001 |
| Length of stay | 2.2 ± 0.4 | 2.2 ± 0.5 | 0.588 |
| Location | - | - | 0.101 |
| C3C4 | 0 | 2 | - |
| C4C5 | 7 | 5 | - |
| C5C6 | 17 | 20 | - |
| C6C7 | 14 | 3 | - |
| C7D1 | 0 | 1 | - |
| Tantalum | PEEK | p-Value | |
|---|---|---|---|
| NDI | |||
| pre-operative | 24.6 ± 5.3 | 27.9 ± 9.9 | 0.09 |
| at follow-up | 12.7 ± 4.4 | 9.6 ± 8.8 | 0.04 |
| pre-FU | 11.8 ± 5.9 | 18.4 ± 9.9 | 0.002 |
| VAS | |||
| pre-operative | 6.9 ± 1.4 | 7.8 ± 1.7 | 0.014 |
| at follow-up | 2.4 ± 1.1 | 2.6 ± 2 | 0.926 |
| pre-FU | 4.5 ± 1.6 | 5.2 ± 2.2 | 0.193 |
| SF-36 | |||
| pre-operative | 37.3 ± 6.8 | 43 ± 19.3 | 0.411 |
| at FU | 48.5 ± 5.3 | 64.7 ± 20.7 | <0.001 |
| pre-FU | −11.1 ± 7.1 | −21.7 ± 19.2 | 0.049 |
| Tantalum | PEEK | p-Value | |
|---|---|---|---|
| Cobb-c (degree) | |||
| pre-operative | 7.9 ± 2.1 | 8 ± 6.7 | 0.08 |
| at follow-up | 9.8 ± 2.5 | 11.9 ± 7.5 | 0.918 |
| pre-FU | −1.8 ± 1.4 | −4 ± 1.9 | <0.001 |
| Cobb-s (degree) | |||
| pre-operative | 0.6 ± 1 | 2.5 ± 2.8 | <0.001 |
| at follow-up | 2.9 ± 0.9 | 6.9 ± 2.9 | <0.001 |
| pre-FU | −2.2 ± 0.8 | −4.3 ± 2.2 | <0.001 |
| Subsidence (Number of patients) | 5 | 7 | 0.304 |
| Fusion-Bridwell classification (Number of patients) | - | - | 0.018 |
| I | 19 | 26 | - |
| II | 13 | 5 | - |
| III | 5 | 0 | - |
| IV | 1 | 0 | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mazzucchi, E.; La Rocca, G.; Perna, A.; Pignotti, F.; Galieri, G.; De Santis, V.; Rinaldi, P.; Tamburrelli, F.C.; Sabatino, G. Single-Level Anterior Cervical Discectomy and Interbody Fusion: A Comparison between Porous Tantalum and Polyetheretherketone Cages. J. Pers. Med. 2022, 12, 986. https://doi.org/10.3390/jpm12060986
Mazzucchi E, La Rocca G, Perna A, Pignotti F, Galieri G, De Santis V, Rinaldi P, Tamburrelli FC, Sabatino G. Single-Level Anterior Cervical Discectomy and Interbody Fusion: A Comparison between Porous Tantalum and Polyetheretherketone Cages. Journal of Personalized Medicine. 2022; 12(6):986. https://doi.org/10.3390/jpm12060986
Chicago/Turabian StyleMazzucchi, Edoardo, Giuseppe La Rocca, Andrea Perna, Fabrizio Pignotti, Gianluca Galieri, Vincenzo De Santis, Pierluigi Rinaldi, Francesco Ciro Tamburrelli, and Giovanni Sabatino. 2022. "Single-Level Anterior Cervical Discectomy and Interbody Fusion: A Comparison between Porous Tantalum and Polyetheretherketone Cages" Journal of Personalized Medicine 12, no. 6: 986. https://doi.org/10.3390/jpm12060986
APA StyleMazzucchi, E., La Rocca, G., Perna, A., Pignotti, F., Galieri, G., De Santis, V., Rinaldi, P., Tamburrelli, F. C., & Sabatino, G. (2022). Single-Level Anterior Cervical Discectomy and Interbody Fusion: A Comparison between Porous Tantalum and Polyetheretherketone Cages. Journal of Personalized Medicine, 12(6), 986. https://doi.org/10.3390/jpm12060986








