Quality of Life for Patients Receiving Elective Interventions for Abdominal Aortic Aneurysms
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Altobelli, E.; Rapacchietta, L.; Profeta, V.F.; Fagnano, R. Risk factors for abdominal aortic aneurysm in population-based studies: A systematic review and meta-analysis. Int. J. Environ. Res. Public Health 2018, 15, 2805. [Google Scholar] [CrossRef]
- Kent, K.C.; Zwolak, R.M.; Jaff, M.R.; Hollenbeck, S.T.; Thompson, R.W.; Schermerhorn, M.L.; Sicard, G.A.; Riles, T.S.; Cronenwett, J.L. Screening for abdominal aortic aneurysm: A consensus statement. J. Vasc. Surg. 2004, 39, 267–269. [Google Scholar] [CrossRef] [PubMed]
- Maceira-Rozas, M.; Atienza-Merino, G. Cribado de aneurisma de aorta abdominal en población de riesgo: Revisión sistemática. Angiología 2008, 60, 165–176. [Google Scholar] [CrossRef]
- Wanhainen, A.; Verzini, F.; Van Herzeele, I.; Allaire, E.; Bown, M.; Cohnert, T.; Dick, F.; van Herwaarden, J.; Karkos, C.; Koelemay, M.; et al. Editor’s Choice-European Society for Vascular Surgery (ESVS) 2019 Clinical Practice Guideliness on the Management of Abdominal Aorto-iliac Artery Aneurysms. Eur. J. Vasc. Endovassc. Surg. 2019, 57, 8–93. [Google Scholar] [CrossRef] [PubMed]
- Coughlin, P.A.; Jackson, D.; White, A.D.; Bailey, M.A.; Farrow, C.; Scott, D.J.A.; Howell, S.J. Meta-analysis of prospective trials determining the short-and-mid-term effect of elective open and endovascular repair of abdominal aortic aneurysms on quality of life. Br. J. Surg. 2013, 100, 448–455. [Google Scholar] [CrossRef] [PubMed]
- Schwartzmann Bonilla, L.S.; Olaizola Otonello, I.R.; Guerra, A.; Dergazarian, S.; Francolino, C.; Porley, G.; Ceretti Berchio, T.H. Validación de un instrumento para medir calidad de vida en hemodiálisis crónica: Perfil de impacto de la enfermedad. Rev. Med. Urug. 1999, 15, 103–109. [Google Scholar]
- Ferguson, N.D.; Fan, E.; Camporota, L.; Antonelli, M.; Anzueto, A.; Beale, R.; Brochard, L.; Brower, R.; Esteban, A.; Gattinoni, L.; et al. The Berlin definition of ARDS: An expanded rationale, justification, and supplementary material. Intensive Care Med. 2012, 38, 1573–1582. [Google Scholar] [CrossRef] [PubMed]
- Bagshaw, S.M.; George, C.; Dinu, I.; Bellomo, R. A multi-center evaluation of the RIFLE criteria for early acute kidney injury in critically ill patients. Nephrol. Dial. Transplant. 2008, 23, 1203–1210. [Google Scholar] [CrossRef] [PubMed]
- Alonso, J. Manual de puntuación de la versión española del Cuestionario SF-36. Barc. Inst. Munic. D’investig. Mèd. (IMIM). 2000. Available online: https://ginvestigaciontmo.files.wordpress.com/2018/07/sf-36-cuestionario.pdf (accessed on 7 May 2022).
- Noel, A.A.; Gloviczki, P.; Cherry, K.J., Jr.; Bower, T.C.; Panneton, J.M.; Mozes, G.I.; Harmsen, W.S.; Jenkins, G.D.; Hallett, J.W. Ruptured abdominal aortic aneurysms: The excessive mortality rate of conventional repair. J. Vasc. Surg. 2001, 34, 41–46. [Google Scholar] [CrossRef] [PubMed]
- Majd, P.; Ahmad, W.; Galas, N.; Brunkwall, J.S. Patients older than 80 years can reach their normal life expectancy after abdominal aortic aneurysm repair: A comparison between endovascular aneurysm repair and open surgery. J. Endovasc. Ther. 2018, 25, 247–251. [Google Scholar] [CrossRef] [PubMed]
- Aaronson, N.K.; Muller, M.; Cohen, P.D.; Essink-Bot, M.L.; Fekkes, M.; Sanderman, R.; Sprangers, M.A.; Te Velde, A.; Verrips, E. Translation, validation, and norming of the Dutch language version of the SF-36 Health Survey in community and chronic disease populations. J. Clin. Epidemiol. 1998, 51, 1055–1068. [Google Scholar] [CrossRef]
- Ramírez, J.; Pozo, M.E. Aneurisma de la aorta abdominal: Controversias y tendencias en su diagnóstico y manejo. Rev. Colomb. De Cirugía 2010, 25, 323–331. [Google Scholar]
- Vallejo, P.P.; Vargas, D.A. Caracterización de Pacientes y Resultados de la Reparación Endovascular de Aneurismas de Aorta Abdominal. Clínica General del Norte, Periodo 2015–2016. 2017. Available online: https://repository.unilibre.edu.co/bitstream/handle/10901/10724/1.114.817.014.pdf?sequence=1&isAllowed=y (accessed on 7 May 2022).
- Barrena-Blázquez, S.; Díez-Alonso, M.; Riera del Moral, L.F.; Sanchez-Coll, S.; Alvarez-Mon, M.; Ortega, M.A.; Ruiz-Grande, F. Association of Age and Surgical Technique with the Quality of Life of Male Patients Treated for Abdominal Aorta Aneurysms: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 6580. [Google Scholar] [CrossRef]
- Hill, A.B.; Palerme, L.P.; Brandys, T.; Lewis, R.; Steinmetz, O.K. Health-related quality of life in survivors of open ruptured abdominal aortic aneurysm repair: A matched, controlled cohort study. J. Vasc. Surg. 2007, 46, 223–229. [Google Scholar] [CrossRef] [PubMed]
- Hayes, V.; Morris, J.; Wolfe, C.; Morgan, M. The SF-36 health survey questionnaire: Is it suitable for use with older adults? Age Ageing 1995, 24, 120–125. [Google Scholar] [CrossRef] [PubMed]
- Ware, J.; Snow, K.K.; Kosinski, M.; Gandek, B. SF-36 Health Survey. Manual and Interpretation Guide; Boston Health Institute, New England Medical Center: Boston, MA, USA, 1993; pp. 10.16–10.17. [Google Scholar]
- Vilagut, G.; Ferrer, M.; Rajmil, L.; Rebollo, P.; Permanyer-Miralda, G.; Quintana, J.M.; Alonso, J. El Cuestionario de Salud SF-36 español: Una década de experiencia y nuevos desarrollos. Gac. Sanit. 2005, 19, 135–150. [Google Scholar] [CrossRef]
- Barrena-Blázquez, S.; Díez-Alonso, M.; Riera del Moral, L.F.; Sanchez Coll, S.; Alvarez-Mon, M.; Ortega, M.A.; Ruiz Grande, F. Quality of Life of Patients Treated for Abdominal Aortic Aneurysm: Open Surgery and Endoprosthesis. J. Clin. Med. 2022, 11, 2195. [Google Scholar] [CrossRef] [PubMed]
| AAR (n = 109) | EVAR (n = 69) | p-Value | |
|---|---|---|---|
| AGE (mean ± SD) | 71 (7) | 76 (7) | 0.09 |
| Diabetes | 19 (17.4%) | 9 (13%) | 0.49 |
| Intermittent claudication | 3 (2.7%) | 1 (1.7%) | 0.56 |
| Lerich’s syndrome | 1 (1%) | 0 | -- |
| Ischemic heart disease | 11 (10%) | 11 (15.9%) | 0.34 |
| ACVA | 2 (1.8%) | 5 (7.2%) | 0.25 |
| EPOC | 9 (9.6%) | 8 (11.5%) | 0.38 |
| Chronic renal failure | 16 (14.6%) | 7 (10.1%) | 0.27 |
| Hyperuricemia | 5 (4.5%) | 0 | -- |
| Hypothyroidism | 4 (3.6%) | 2 (2.8%) | 0.69 |
| Prostate Pathology | 16 (14.2%) | 7 (10.1%) | 0.47 |
| SIZE OF THE ANEURISM | |||
| 40–56 mm | 41 (44%) | 30 (43.8%) | 0.08 |
| 57–73 mm | 28 (30%) | 38 (55%) | |
| 73–90 mm | 10 (10.7%) | 1 (1.6%) | |
| >90 mm | 14 (15%) | 0 | |
| EARLY POSTOPERATIVE COMPLICATIONS | |||
| Paralytic ileus | 13 (11.9%) | 0 | -- |
| Acute Renal Failure | 11 (10%) | 0 | -- |
| Respiratory distress | 8 (7.3%) | 0 | -- |
| Haemorrhagic shock | 6 (5.5%) | 1 (1.4%) | 0.14 |
| Bronchopneumonia | 4 (3.6%) | 0 | -- |
| Femoral pseudoaneurysm | 0 | 1 (1.4%) | -- |
| Paresis in LL | 0 | 1 (1.4%) | -- |
| Total (*) | 30 (27.5%) | 2 (2.8%) | 0.001 |
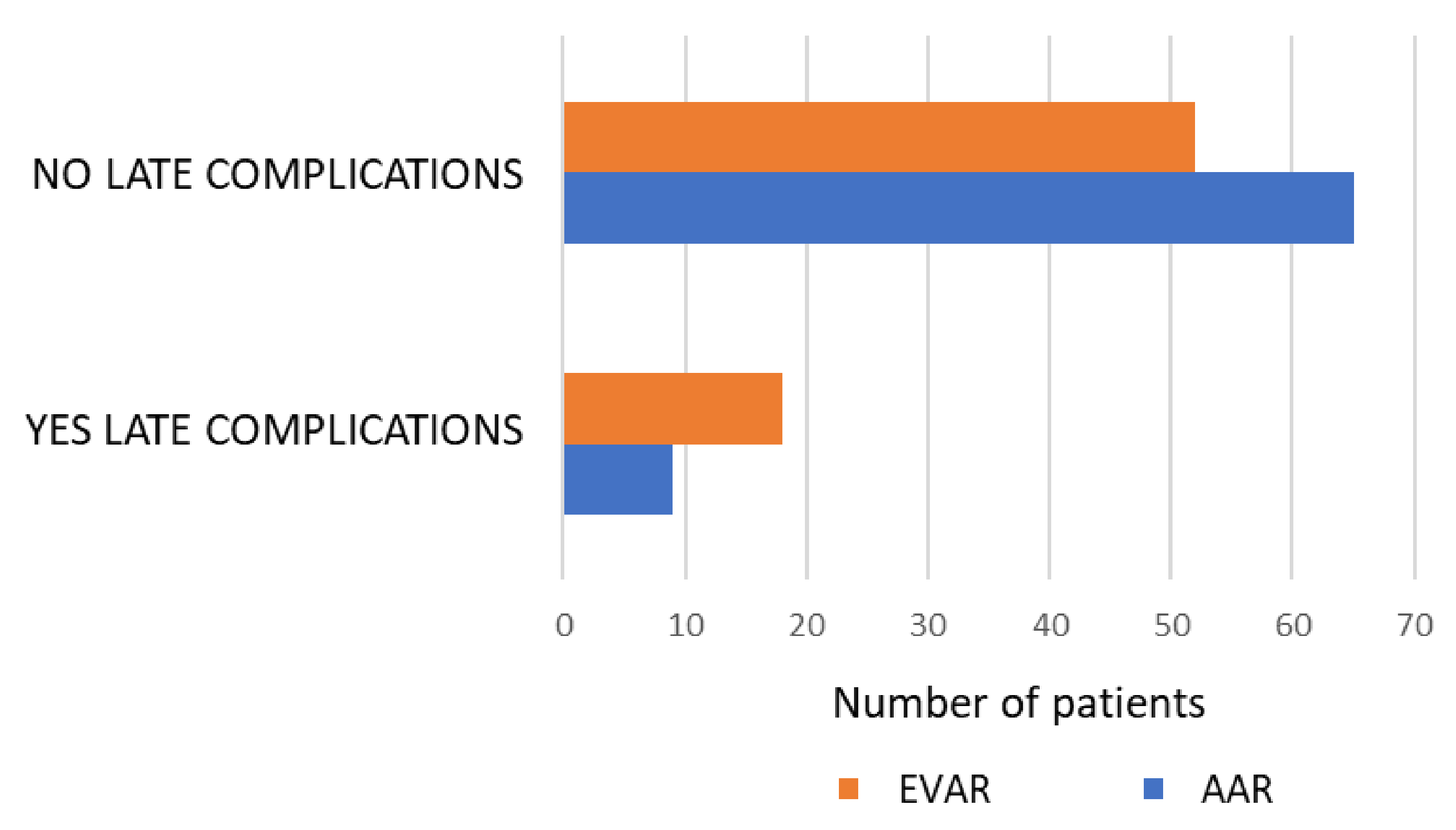
| LATE POSTOPERATIVE COMPLICATIONS | |||
| Eventration | 6(5.4%) | 0 | -- |
| Ischemic Colitis | 1(0.9%) | 0 | -- |
| Peritonitis | 1(0.9%) | 0 | -- |
| Surgical wound dehiscence | 1(0.9%) | 0 | -- |
| Stent leak | 0 | 7 (10.1%) | -- |
| Iliac stenosis | 0 | 2 (2.8%) | -- |
| Lower limb thrombosis | 0 | 3 (4.3%) | -- |
| Acute lower limb ischemia | 0 | 2 (2.8%) | -- |
| Thrombophlebitis in Lower Limb | 0 | 1 (1.4%) | -- |
| Iliac pseudoaneurysm | 0 | 1 (1.4%) | -- |
| EVAR branch thrombosis | 0 | 1 (1.4%) | -- |
| Lower limb paraesthesia | 0 | 1 (1.4%) | -- |
| Total (*) | 9 (8.2%) | 18 (26%) | 0.013 |
| HOSPITAL STAY days (mean) | 10 (7) | 4.14 (4) | 0.001 |
| %N Answer | Cronbach’s Alpha | Correlation Person | Mean | SD | Percentile 5 | Rank | Maximum | Minimum | Percentile 25 | Percentile 75 | Percentage with Maximum Score | Percentage with Minimum Score | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Physical Function | 0 | 0.88 | 0.88–0.54 | 76.2 | 22 | 80 | 100 | 100 (14) | 0 (2) | 70 | 95 | 9.3 | 1.3 |
| Physical Role | 0 | 0.88 | 0.78–0.54 | 74.3 | 37 | 100 | 100 | 100 (90) | 0 (19) | 50 | 100 | 59.6 | 13.9 |
| Body Ache | 0 | 0.75 | 0.60–0.89 | 81.7 | 23.5 | 90 | 100 | 100 (71) | 0 (1) | 70 | 100 | 47.7 | 0.7 |
| General Health | 0 | 0.70 | 0.82–0.56 | 60.8 | 18.7 | 65 | 85 | 100 (2) | 15 (2) | 45 | 75 | 1.3 | 1.3 |
| Vitality | 0 | 0.80 | 0.82–0.44 | 64.8 | 21.1 | 70 | 95 | 100 (4) | 5 (1) | 50 | 80 | 2.6 | 0.7 |
| Social Function | 0 | 0.86 | 0.93–0.76 | 80 | 25 | 87 | 100 | 100 (66) | 0 (2) | 75 | 100 | 43.7 | 1.3 |
| Emotional Role | 0 | 0.88 | 0.84–0.60 | 59.2 | 15.4 | 66 | 100 | 100 (1) | 0 (2) | 66 | 66 | 0.7 | 1.3 |
| Mental Health | 0 | 0.87 | 0.81–0.64 | 73.3 | 21.5 | 80 | 80 | 100 (17) | 20 (6) | 60 | 88 | 11.3 | 4.0 |
| (n = 151) | Physical Health | Mental Health |
|---|---|---|
| Mean | 35.9582 | 34.9354 |
| SD | 10.24146 | 8.24213 |
| Median | 39.7917 | 36.2500 |
| Minimum | 4.79 | 8.50 |
| Maximum | 48.75 | 48.75 |
| Physical Function | Role Physical | Body Ache | General Health | Vitality | Social Function | Role Emotional | Mental Health | ||
|---|---|---|---|---|---|---|---|---|---|
| AAR (n = 93) | Mean | 80.05 | 74.46 | 82.47 | 63.01 | 67.90 | 81.99 | 58.42 | 75.48 |
| SD | 21.23 | 37.76 | 22.58 | 20.82 | 22.20 | 25.76 | 16.04 | 23,46 | |
| Median (Rank) | 85 (100) | 100 (100) | 90 (100) | 65 (85) | 75 (100) | 100 (100) | 66.67 (100) | 80 (80) | |
| EVAR (n = 58) | Mean | 69.05 | 71.55 | 80.52 | 56.47 | 58.62 | 75.65 | 59.77 | 68.83 |
| SD | 22.48 | 38.74 | 24.95 | 14.23 | 18.77 | 25.15 | 14.98 | 18.21 | |
| Median (Rank) | 75 (100) | 100 (100) | 90 (100) | 57.5 (55) | 60 (80) | 87.5 (100) | 66.67 (67) | 72 (80) | |
| p value | 0.001 | 0.623 | 0.704 | 0.037 | 0.003 | 0.023 | 0.562 | 0.006 |
| Physical Health | Mental Health | ||
|---|---|---|---|
| AAR (n = 93) | Median | 41.45 | 38.05 |
| IQR | 43.46 | 40.25 | |
| EVAR (n = 58) | Median | 38.48 | 34.06 |
| IQR | 40.01 | 25.88 | |
| p value (*) | 0.032 | 0.003 | |
| Total (n = 151) | Median | 39.79 | 36.25 |
| IQR | 43.96 | 40.25 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barrena-Blázquez, S.; Díez-Alonso, M.; Riera del Moral, L.F.; Coll, S.S.; García-Honduvilla, N.; Alvarez-Mon, M.; Ortega, M.A.; Ruiz-Grande, F. Quality of Life for Patients Receiving Elective Interventions for Abdominal Aortic Aneurysms. J. Pers. Med. 2022, 12, 910. https://doi.org/10.3390/jpm12060910
Barrena-Blázquez S, Díez-Alonso M, Riera del Moral LF, Coll SS, García-Honduvilla N, Alvarez-Mon M, Ortega MA, Ruiz-Grande F. Quality of Life for Patients Receiving Elective Interventions for Abdominal Aortic Aneurysms. Journal of Personalized Medicine. 2022; 12(6):910. https://doi.org/10.3390/jpm12060910
Chicago/Turabian StyleBarrena-Blázquez, Silvestra, Manuel Díez-Alonso, Luis Felipe Riera del Moral, Salvador Sanchez Coll, Natalio García-Honduvilla, Melchor Alvarez-Mon, Miguel A. Ortega, and Fernando Ruiz-Grande. 2022. "Quality of Life for Patients Receiving Elective Interventions for Abdominal Aortic Aneurysms" Journal of Personalized Medicine 12, no. 6: 910. https://doi.org/10.3390/jpm12060910
APA StyleBarrena-Blázquez, S., Díez-Alonso, M., Riera del Moral, L. F., Coll, S. S., García-Honduvilla, N., Alvarez-Mon, M., Ortega, M. A., & Ruiz-Grande, F. (2022). Quality of Life for Patients Receiving Elective Interventions for Abdominal Aortic Aneurysms. Journal of Personalized Medicine, 12(6), 910. https://doi.org/10.3390/jpm12060910









