Correlation Comparison and Personalized Utility of Field Walking Tests in Assessing the Exercise Capacity of Patients with Chronic Obstructive Pulmonary Disease: A Randomized Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Participants
2.3. Cardiopulmonary Exercise Test
2.4. Six-Minute Walk Test
2.5. Incremental Shuttle Walking Test
2.6. Sample Size Calculation
2.7. Statistical Analysis
3. Results
3.1. Participants
3.2. Correlation of CPET with ISWT and 6MWT
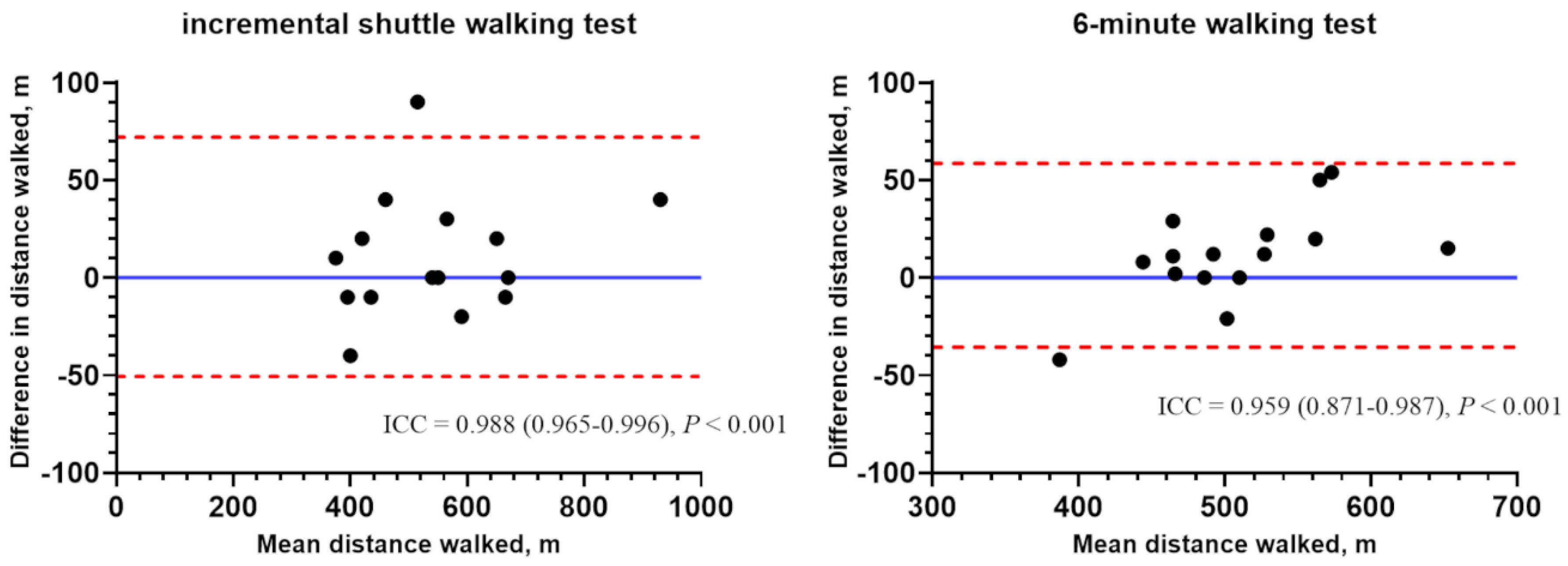
3.3. Reliability of ISWT and 6MWT
3.4. Correlation Analysis of ISWT and 6MWT
3.5. Clinical Parameters of Each Exercise Test
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Celli, B.R.; Cote, C.G.; Marin, J.M.; Casanova, C.; Montes de Oca, M.; Mendez, R.A.; Pinto Plata, V.; Cabral, H.J. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N. Engl. J. Med. 2004, 350, 1005–1012. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Global Strategy for Prevention, Diagnosis and Management of COPD: 2022 Report. Available online: https://goldcopd.org/2022-gold-reports-2/ (accessed on 3 February 2022).
- Holland, A.E.; Spruit, M.A.; Troosters, T.; Puhan, M.A.; Pepin, V.; Saey, D.; McCormack, M.C.; Carlin, B.W.; Sciurba, F.C.; Pitta, F.; et al. An official European Respiratory Society/American Thoracic Society technical standard: Field walking tests in chronic respiratory disease. Eur. Respir. J. 2014, 44, 1428–1446. [Google Scholar] [CrossRef] [PubMed]
- Guazzi, M.; Arena, R.; Halle, M.; Piepoli, M.F.; Myers, J.; Lavie, C.J. 2016 focused update: Clinical recommendations for cardiopulmonary exercise testing data assessment in specific patient populations. Eur. Heart J. 2018, 39, 1144–1161. [Google Scholar] [CrossRef] [PubMed]
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: Guidelines for the six-minute walk test. Am. J. Respir. Crit. Care Med. 2002, 166, 111–117. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.J.; Morgan, M.D.; Scott, S.; Walters, D.; Hardman, A.E. Development of a shuttle walking test of disability in patients with chronic airways obstruction. Thorax 1992, 47, 1019–1024. [Google Scholar] [CrossRef] [Green Version]
- Singh, S.J.; Puhan, M.A.; Andrianopoulos, V.; Hernandes, N.A.; Mitchell, K.E.; Hill, C.J.; Lee, A.L.; Camillo, C.A.; Troosters, T.; Spruit, M.A.; et al. An official systematic review of the European Respiratory Society/American Thoracic Society: Measurement properties of field walking tests in chronic respiratory disease. Eur. Respir. J. 2014, 44, 1447–1478. [Google Scholar] [CrossRef] [PubMed]
- Morales, F.J.; Montemayor, T.; Martinez, A. Shuttle versus six-minute walk test in the prediction of outcome in chronic heart failure. Int. J. Cardiol. 2000, 76, 101–105. [Google Scholar] [CrossRef]
- Beaver, W.L.; Wasserman, K.; Whipp, B.J. A new method for detecting anaerobic threshold by gas exchange. J. Appl. Physiol. (1985) 1986, 60, 2020–2027. [Google Scholar] [CrossRef]
- Reinhard, U.; Müller, P.H.; Schmulling, R.M. Determination of anaerobic threshold by the ventilation equivalent in normal individuals. Respiration 1979, 38, 36–42. [Google Scholar] [CrossRef]
- Chae, G.; Ko, E.J.; Lee, S.W.; Kim, H.J.; Kwak, S.G.; Park, D.; Ra, S.W. Stronger correlation of peak oxygen uptake with distance of incremental shuttle walk test than 6-min walk test in patients with COPD: A systematic review and meta-analysis. BMC Pulm. Med. 2022, 22, 102. [Google Scholar] [CrossRef]
- Parreira, V.F.; Janaudis-Ferreira, T.; Evans, R.A.; Mathur, S.; Goldstein, R.S.; Brooks, D. Measurement properties of the incremental shuttle walk test. a systematic review. Chest 2014, 145, 1357–1369. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Diedenhofen, B.; Musch, J. cocor: A comprehensive solution for the statistical comparison of correlations. PLoS ONE 2015, 10, e0121945. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Turner, S.E.; Eastwood, P.R.; Cecins, N.M.; Hillman, D.R.; Jenkins, S.C. Physiologic responses to incremental and self-paced exercise in COPD: A comparison of three tests. Chest 2004, 126, 766–773. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.J.; Morgan, M.D.; Hardman, A.E.; Rowe, C.; Bardsley, P.A. Comparison of oxygen uptake during a conventional treadmill test and the shuttle walking test in chronic airflow limitation. Eur. Respir. J. 1994, 7, 2016–2020. [Google Scholar] [PubMed]
- Onorati, P.; Antonucci, R.; Valli, G.; Berton, E.; De Marco, F.; Serra, P.; Palange, P. Non-invasive evaluation of gas exchange during a shuttle walking test vs. a 6-min walking test to assess exercise tolerance in COPD patients. Eur. J. Appl. Physiol. 2003, 89, 331–336. [Google Scholar] [CrossRef]
- Arizono, S.-I.; Kitagawa, C.; Tanaka, T.; Oike, T.; Rikitomi, N.; Takahashi, T.; Moji, K.; Senju, H. Validity of incremental shuttle walking test as a measure of exercise tolerance in chronic obstructive pulmonary disease. J. Jpn. Soc. Respir. Care Rehabil. 2002, 11, 414–419. [Google Scholar]
- Arizono, S.; Ogawa, T.; Watanabe, F.; Homon, R.; Hirasawa, J.; Kondoh, Y.; Kimura, T.; Nishiyama, O.; Kato, K.; Senjyu, H.; et al. Prediction of peak VO2 using 6 minutes walk teat and incremental shuttle walking test in COPD patients. J. Jpn. Soc. Respir. Care Rehabil. 2008, 18, 160–165. [Google Scholar]
- Rejeski, W.J.; Foley, K.O.; Woodard, C.M.; Zaccaro, D.J.; Berry, M.J. Evaluating and understanding performance testing in COPD patients. J. Cardiopulm. Rehabil. Prev. 2000, 20, 79–88. [Google Scholar] [CrossRef]
- Chuang, M.L.; Lin, I.F.; Wasserman, K. The body weight-walking distance product as related to lung function, anaerobic threshold and peak VO2 in COPD patients. Respir. Med. 2001, 95, 618–626. [Google Scholar] [CrossRef] [Green Version]
- Oga, T.; Nishimura, K.; Tsukino, M.; Hajiro, T.; Ikeda, A.; Mishima, M. Relationship between different indices of exercise capacity and clinical measures in patients with chronic obstructive pulmonary disease. Heart Lung 2002, 31, 374–381. [Google Scholar] [CrossRef]
- Carter, R.; Holiday, D.B.; Nwasuruba, C.; Stocks, J.; Grothues, C.; Tiep, B. 6-minute walk work for assessment of functional capacity in patients with COPD. Chest 2003, 123, 1408–1415. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Starobin, D.; Kramer, M.R.; Yarmolovsky, A.; Bendayan, D.; Rosenberg, I.; Sulkes, J.; Fink, G. Assessment of functional capacity in patients with chronic obstructive pulmonary disease: Correlation between cardiopulmonary exercise, 6 minute walk and 15 step exercise oximetry test. Isr. Med. Assoc. J. 2006, 8, 460–463. [Google Scholar] [PubMed]
- Hill, K.; Jenkins, S.C.; Cecins, N.; Philippe, D.L.; Hillman, D.R.; Eastwood, P.R. Estimating maximum work rate during incremental cycle ergometry testing from six-minute walk distance in patients with chronic obstructive pulmonary disease. Arch. Phys. Med. Rehabil. 2008, 89, 1782–1787. [Google Scholar] [CrossRef] [PubMed]
- Diaz, O.; Morales, A.; Osses, R.; Klaassen, J.; Lisboa, C.; Saldias, F. Six-minute-walk test and maximum exercise test in cycloergometer in chronic obstructive pulmonary disease. Are the physiological demands equivalent? Arch. Bronconeumol. 2010, 46, 294–301. [Google Scholar] [CrossRef]
- Campo, L.A.; Chilingaryan, G.; Berg, K.; Paradis, B.; Mazer, B. Validity and reliability of the modified shuttle walk test in patients with chronic obstructive pulmonary disease. Arch. Phys. Med. Rehabil. 2006, 87, 918–922. [Google Scholar] [CrossRef]
- Eiser, N.; Willsher, D.; Dore, C.J. Reliability, repeatability and sensitivity to change of externally and self-paced walking tests in COPD patients. Respir. Med. 2003, 97, 407–414. [Google Scholar] [CrossRef] [Green Version]
- Guyatt, G.H.; Pugsley, S.O.; Sullivan, M.J.; Thompson, P.J.; Berman, L.; Jones, N.L.; Fallen, E.L.; Taylor, D.W. Effect of encouragement on walking test performance. Thorax 1984, 39, 818–822. [Google Scholar] [CrossRef] [Green Version]
- Guyatt, G.H.; Thompson, P.J.; Berman, L.B.; Sullivan, M.J.; Townsend, M.; Jones, N.L.; Pugsley, S.O. How should we measure function in patients with chronic heart and lung disease? J. Chronic Dis. 1985, 38, 517–524. [Google Scholar] [CrossRef]
- Iriberri, M.; Galdiz, J.B.; Gorostiza, A.; Ansola, P.; Jaca, C. Comparison of the distances covered during 3 and 6 min walking test. Respir. Med. 2002, 96, 812–816. [Google Scholar] [CrossRef] [Green Version]
- Kozu, R.; Jenkins, S.; Senjyu, H.; Mukae, H.; Sakamoto, N.; Kohno, S. Peak power estimated from 6-minute walk distance in Asian patients with idiopathic pulmonary fibrosis and chronic obstructive pulmonary disease. Respirology 2010, 15, 706–713. [Google Scholar] [CrossRef] [Green Version]
- Jorquera Guillen, M.A.; Salcedo Posadas, A.; Villa Asensi, J.R.; Giron Moreno, R.M.; Neira Rodriguez, M.A.; Sequeiros Gonzalez, A. Reproducibility of the walking test in patients with cystic fibrosis. An. Esp. Pediatr. 1999, 51, 475–478. [Google Scholar] [PubMed]
- Ziegler, B.; Rovedder, P.M.; Oliveira, C.L.; de Abreu e Silva, F.; de Tarso Roth Dalcin, P. Repeatability of the 6-minute walk test in adolescents and adults with cystic fibrosis. Respir. Care 2010, 55, 1020–1025. [Google Scholar] [PubMed]
- Eaton, T.; Young, P.; Milne, D.; Wells, A.U. Six-minute walk, maximal exercise tests: Reproducibility in fibrotic interstitial pneumonia. Am. J. Respir. Crit. Care Med. 2005, 171, 1150–1157. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, S.; Cecins, N.M. Six-minute walk test in pulmonary rehabilitation: Do all patients need a practice test? Respirology 2010, 15, 1192–1196. [Google Scholar] [CrossRef]
- American Thoracic, S.; American College of Chest, P. ATS/ACCP Statement on cardiopulmonary exercise testing. Am. J. Respir. Crit. Care Med. 2003, 167, 211–277. [Google Scholar]
- Neves, C.D.; Lacerda, A.C.; Lage, V.K.; Lima, L.P.; Fonseca, S.F.; de Avelar, N.C.; Teixeira, M.M.; Mendonca, V.A. Cardiorespiratory responses and prediction of peak oxygen uptake during the shuttle walking test in healthy sedentary adult men. PLoS ONE 2015, 10, e0117563. [Google Scholar] [CrossRef] [Green Version]
- Lima, L.P.; Leite, H.R.; Matos, M.A.; Neves, C.D.C.; Lage, V.; Silva, G.P.D.; Lopes, G.S.; Chaves, M.G.A.; Santos, J.N.V.; Camargos, A.C.R.; et al. Cardiorespiratory fitness assessment and prediction of peak oxygen consumption by Incremental Shuttle Walking Test in healthy women. PLoS ONE 2019, 14, e0211327. [Google Scholar] [CrossRef]
- Sillen, M.J.; Vercoulen, J.H.; van ‘t Hul, A.J.; Klijn, P.H.; Wouters, E.F.; van Ranst, D.; Peters, J.B.; van Keimpema, A.R.; Franssen, F.M.; Otten, H.J.; et al. Inaccuracy of estimating peak work rate from six-minute walk distance in patients with COPD. COPD J. Chronic Obstr. Pulm. Dis. 2012, 9, 281–288. [Google Scholar] [CrossRef]
- Ringbaek, T.; Martinez, G.; Brondum, E.; Thogersen, J.; Morgan, M.; Lange, P. Shuttle walking test as predictor of survival in chronic obstructive pulmonary disease patients enrolled in a rehabilitation program. J. Cardiopulm. Rehabil. Prev. 2010, 30, 409–414. [Google Scholar] [CrossRef]
- Hill, K.; Dolmage, T.E.; Woon, L.; Coutts, D.; Goldstein, R.; Brooks, D. Comparing peak and submaximal cardiorespiratory responses during field walking tests with incremental cycle ergometry in COPD. Respirology 2012, 17, 278–284. [Google Scholar] [CrossRef]
- Vonbank, K.; Marzluf, B.; Knotig, M.; Funk, G.C. Agreement between Cardiopulmonary Exercise Test and Modified 6-Min Walk Test in Determining Oxygen Uptake in COPD Patients with Different Severity Stages. Respiration 2020, 99, 225–230. [Google Scholar] [CrossRef] [PubMed]
- Pulz, C.; Diniz, R.V.; Alves, A.N.; Tebexreni, A.S.; Carvalho, A.C.; de Paola, A.A.; Almeida, D.R. Incremental shuttle and six-minute walking tests in the assessment of functional capacity in chronic heart failure. Can. J. Cardiol. 2008, 24, 131–135. [Google Scholar] [CrossRef] [Green Version]



| Total (n = 29) | Hospital 1 (UUH) (n = 15) | Hospital 2 (AMC) (n = 14) | p † | |
|---|---|---|---|---|
| Age (years) * | 67.0 (61.0–72.0) | 65.0 (61.0–71.0) | 67.5 (64.0–73.5) | 0.619 |
| Male gender | 28 (96.6%) | 15 (100.0%) | 13 (92.9%) | 0.483 |
| Body mass index (kg/m2) * | 23.7 (22.3–26.0) | 23.1 (22.1–26.7) | 24.3 (23.2–25.5) | 0.680 |
| Smoking history | 0.483 | |||
| Nonsmoker | 1 (3.4%) | 0 (0.0%) | 1 (7.1%) | |
| Current or ex-smoker | 28 (96.6%) | 15 (100.0%) | 13 (92.9%) | |
| Smoking amount (pack-years) | 35.0 (26.0–49.0) | 39.0 (30.0–50.0) | 34.0 (14.5–49.0) | 0.400 |
| Comorbidity | ||||
| DM | 3 (10.3%) | 3 (20.0%) | 0 (0.0%) | 0.224 |
| HTN | 7 (24.1%) | 3 (20.0%) | 4 (28.6%) | 0.682 |
| Pulmonary HTN | 1 (3.4%) | 1 (6.7%) | 0 (0.0%) | >0.999 |
| CAD | 1 (3.4%) | 0 (0.0%) | 1 (7.1%) | 0.483 |
| Arrhythmia | 1 (3.4%) | 0 (0.0%) | 1 (7.1%) | 0.483 |
| Lung cancer | 1 (3.4%) | 0 (0.0%) | 1 (7.1%) | 0.483 |
| Malignancy except lung | 4 (13.8%) | 2 (13.3%) | 2 (14.3%) | >0.999 |
| Any exacerbation in the past year | 7 (24.1%) | 6 (40.0%) | 1 (7.1%) | 0.080 |
| Inhalers | 0.041 | |||
| No use | 1 (3.4%) | 0 (0.0%) | 1 (7.1%) | |
| LAMA | 1 (3.4%) | 0 (0.0%) | 1 (7.1%) | |
| LAMA + LABA | 17 (58.6%) | 6 (40.0%) | 11 (78.5%) | |
| LABA + ICS | 2 (6.9%) | 2 (13.3%) | 0 (0.0%) | |
| LAMA + LABA + ICS | 8 (27.6%) | 7 (46.7%) | 1 (7.1%) | |
| mMRC | 1.0 (1.0–2.0) | 1.0 (1.0–1.0) | 1.5 (1.0–2.0) | 0.046 |
| CAT * | 7.0 (4.0–12.0) | 8.0 (5.0–12.0) | 6.5 (3.8–17.5) | 0.637 |
| Pulmonary function test | ||||
| FEV1 (L) * | 1.9 (1.4–2.3) | 2.1 (1.3–2.3) | 1.8 (1.4–2.2) | 0.409 |
| FEV1, % predicted | 66.5 (54.5–82.5) | 66.5 (53.9–82.7) | 67.9 (55.9–83.5) | 0.914 |
| FVC (L) * | 3.8 (3.3–4.3) | 3.8 (3.5–4.3) | 3.6 (3.1–4.3) | 0.362 |
| FVC, % predicted | 108.8 (94.7–117.4) | 108.8 (93.8–115.4) | 108.9 (95.0–119.5) | 0.914 |
| FEV1/FVC | 47.0 (38.5–59.5) | 47.0 (35.0–62.0) | 51.0 (42.3–59.0) | 0.780 |
| CPET | ||||
| Peak VO2 (mL/kg/min) | 17.8 (14.5–21.1) | 18.0 (14.0–23.8) | 17.6 (15.4–19.5) | 0.780 |
| MVV * | 73.0 (47.5–97.5) | 87.0 (46.0–99.0) | 72.0 (54.0–95.5) | 0.525 |
| Breathing reserve * | 19.0 (3.0–33.5) | 14.0 (2.0–21.0) | 29.2 (14.8–38.3) | 0.105 |
| Peak RQ | 1.3 (1.2–1.4) | 1.2 (1.1–1.4) | 1.4 (1.3–1.5) | 0.188 |
| O2 pulse | 10.0 (8.5–12.6) | 9.6 (7.4–13.1) | 10.3 (9.0–12.5) | 0.161 |
| Distance of ISWT (m) * | 483.5 ± 124.1 | 538.7 ± 143.7 | 424.3 ± 60.3 | 0.011 |
| Distance of 6MWT (m) * | 525.3 ± 62.5 | 502.5 ± 57.5 | 549.8 ± 60.2 | 0.040 |
| Total (n = 29) | Hospital 1 (n = 15) | Hospital 2 (n = 14) | p * | ||||
|---|---|---|---|---|---|---|---|
| r | p | r | p | r | p | ||
| Peak VO2~ISWT | 0.782 | <0.001 | 0.868 | <0.001 | 0.540 | 0.046 | 0.084 |
| Peak VO2~6MWT | 0.512 | 0.005 | 0.685 | 0.005 | 0.572 | 0.033 | 0.653 |
| p † | 0.043 | 0.029 | 0.883 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ko, E.J.; Lee, J.H.; Lee, H.Y.; Lee, S.H.; Lee, H.-J.; Chae, G.; Lee, S.W.; Ra, S.W. Correlation Comparison and Personalized Utility of Field Walking Tests in Assessing the Exercise Capacity of Patients with Chronic Obstructive Pulmonary Disease: A Randomized Controlled Trial. J. Pers. Med. 2022, 12, 901. https://doi.org/10.3390/jpm12060901
Ko EJ, Lee JH, Lee HY, Lee SH, Lee H-J, Chae G, Lee SW, Ra SW. Correlation Comparison and Personalized Utility of Field Walking Tests in Assessing the Exercise Capacity of Patients with Chronic Obstructive Pulmonary Disease: A Randomized Controlled Trial. Journal of Personalized Medicine. 2022; 12(6):901. https://doi.org/10.3390/jpm12060901
Chicago/Turabian StyleKo, Eun Jae, Jang Ho Lee, Hyang Yi Lee, Seong Ho Lee, Hack-Jae Lee, Ganghee Chae, Sei Won Lee, and Seung Won Ra. 2022. "Correlation Comparison and Personalized Utility of Field Walking Tests in Assessing the Exercise Capacity of Patients with Chronic Obstructive Pulmonary Disease: A Randomized Controlled Trial" Journal of Personalized Medicine 12, no. 6: 901. https://doi.org/10.3390/jpm12060901
APA StyleKo, E. J., Lee, J. H., Lee, H. Y., Lee, S. H., Lee, H.-J., Chae, G., Lee, S. W., & Ra, S. W. (2022). Correlation Comparison and Personalized Utility of Field Walking Tests in Assessing the Exercise Capacity of Patients with Chronic Obstructive Pulmonary Disease: A Randomized Controlled Trial. Journal of Personalized Medicine, 12(6), 901. https://doi.org/10.3390/jpm12060901






