Comparison of Surgical Outcomes of Hysterectomy by Vaginal Natural Orifice Transluminal Endoscopic Surgery (vNOTES) versus Single-Port Access (SPA) Surgery
Abstract
:1. Introduction
2. Materials and Methods
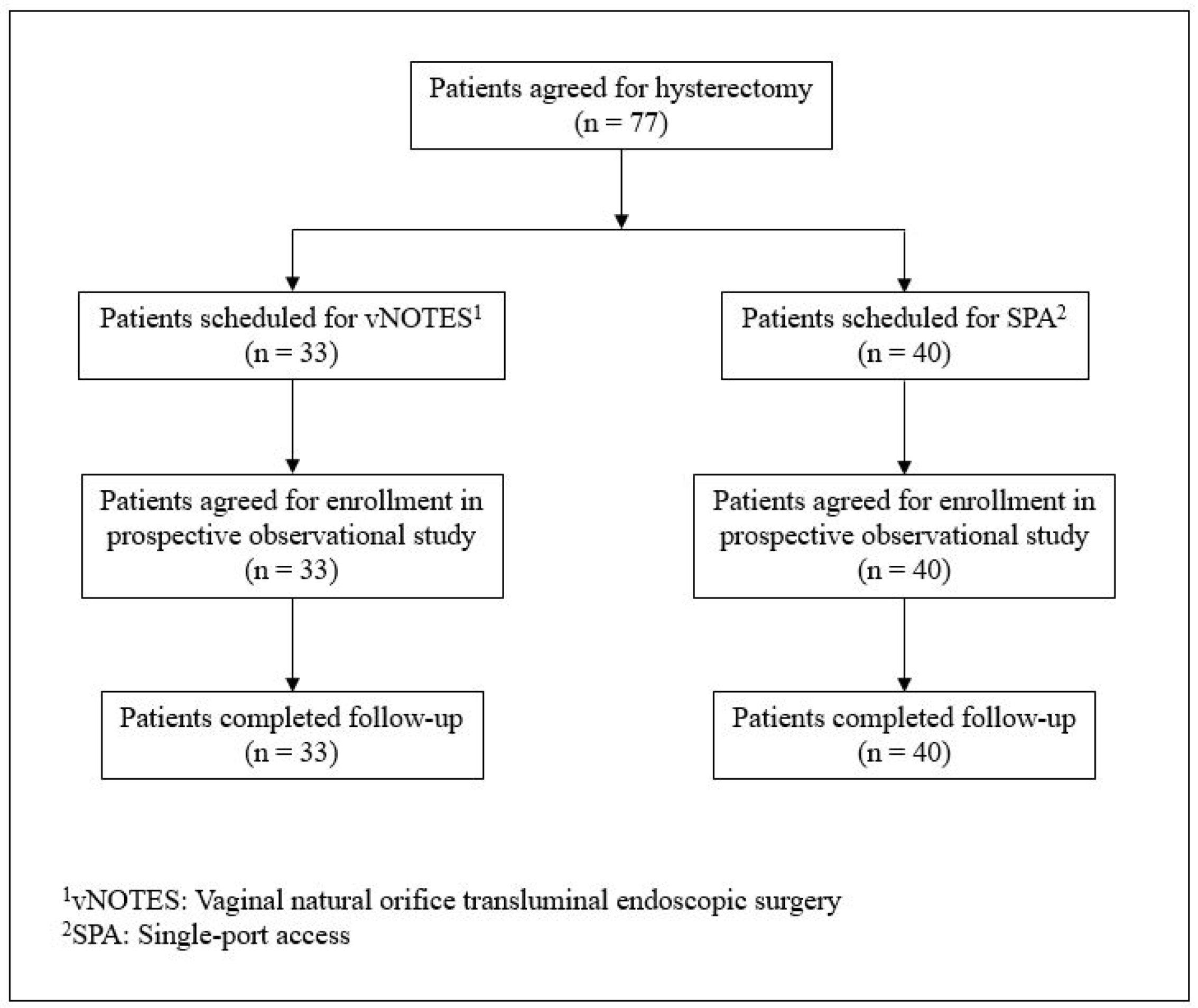
2.1. Patients
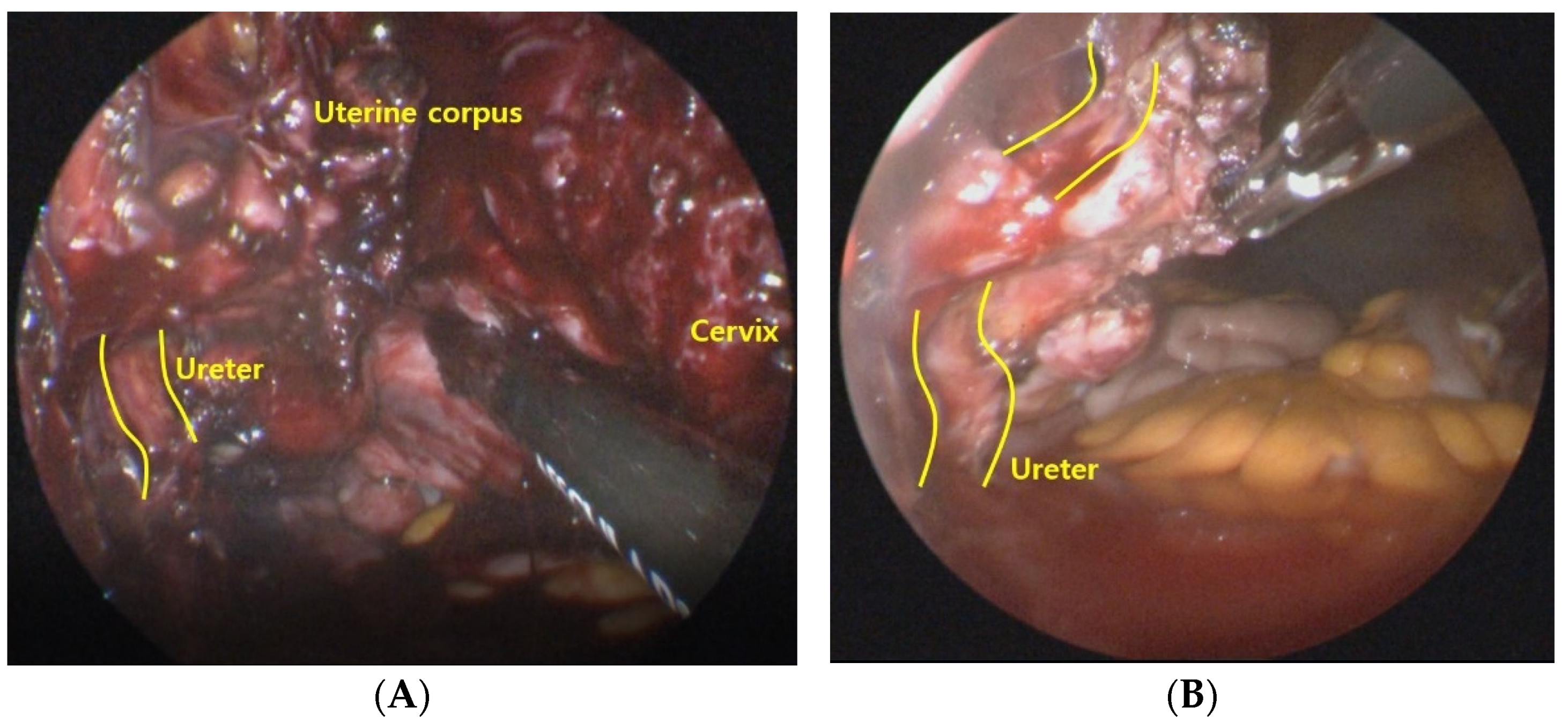
2.2. Operative Techniques
2.3. Data
2.4. Statistical Analyses
2.5. Ethics Approval
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bucher, P.; Pugin, F.; Buchs, N.C.; Ostermann, S.; Morel, P. Randomized clinical trial of laparoendoscopic single-site versus conventional laparoscopic cholecystectomy. Br. J. Surg. 2011, 98, 1695–1702. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.Y.; Kim, T.J.; Kim, C.J.; Park, H.S.; Choi, C.H.; Lee, J.W.; Lee, J.H.; Bae, D.S.; Kim, B.G. Single port access laparoscopic adnexal surgery versus conventional laparoscopic adnexal surgery: A comparison of peri-operative outcomes. Eur. J. Obstet. Gynecol. Reprod. Biol. 2010, 151, 181–184. [Google Scholar] [CrossRef] [PubMed]
- Fader, A.N.; Rojas-Espaillat, L.; Ibeanu, O.; Grumbine, F.C.; Escobar, P.F. Laparoendoscopic single-site surgery (LESS) in gynecology: A multi-institutional evaluation. Am. J. Obstet. Gynecol. 2010, 203, 501.e1–501.e6. [Google Scholar] [CrossRef]
- Fagotti, A.; Bottoni, C.; Vizzielli, G.; Gueli Alletti, S.; Scambia, G.; Marana, E.; Fanfani, F. Postoperative pain after conventional laparoscopy and laparoendoscopic single site surgery (LESS) for benign adnexal disease: A randomized trial. Fertil. Steril. 2011, 96, 255–259.e2. [Google Scholar] [CrossRef]
- Kalloo, A.N.; Singh, V.K.; Jagannath, S.B.; Niiyama, H.; Hill, S.L.; Vaughn, C.A.; Magee, C.A.; Kantsevoy, S.V. Flexible transgastric peritoneoscopy: A novel approach to diagnostic and therapeutic interventions in the peritoneal cavity. Gastrointest. Endosc. 2004, 60, 114–117. [Google Scholar] [CrossRef]
- Ahn, K.H.; Song, J.Y.; Kim, S.H.; Lee, K.W.; Kim, T. Transvaginal single-port natural orifice transluminal endoscopic surgery for benign uterine adnexal pathologies. J. Minim. Invasive Gynecol. 2012, 19, 631–635. [Google Scholar] [CrossRef]
- Lowenstein, L.; Baekelandt, J.; Paz, Y.; Lauterbach, R.; Matanes, E. Transvaginal Natural Orifice Transluminal Endoscopic Hysterectomy and Apical Suspension of the Vaginal Cuff to the Uterosacral Ligament. J. Minim. Invasive Gynecol. 2019, 26, 1015. [Google Scholar] [CrossRef] [PubMed]
- Baekelandt, J.F.; De Mulder, P.A.; Le Roy, I.; Mathieu, C.; Laenen, A.; Enzlin, P.; Weyers, S.; Mol, B.; Bosteels, J. Hysterectomy by transvaginal natural orifice transluminal endoscopic surgery versus laparoscopy as a day-care procedure: A randomised controlled trial. BJOG 2019, 126, 105–113. [Google Scholar] [CrossRef] [Green Version]
- Lowenstein, L.; Matanes, E.; Lauterbach, R.; Mor, O.; Burke, Y.Z.; Weiner, Z.; Baekelandt, J. Feasibility and Learning Curve of Transvaginal Natural Orifice Transluminal Endoscopic Surgery for Hysterectomy and Uterosacral Ligament Suspension in Apical Compartment Prolapse. Female Pelvic Med. Reconstr. Surg. 2021, 27, e171–e176. [Google Scholar] [CrossRef]
- Goldenberg, M.; Burke, Y.Z.; Matanes, E.; Lowenstein, L. Transvaginal Natural Orifice Transluminal Endoscopic Surgery (vNOTES) for prophylactic bilateral salpingo-oophorectomy. Surg. Oncol. 2020, 35, 79–80. [Google Scholar] [CrossRef]
- Coomber, R.S.; Sodergren, M.H.; Clark, J.; Teare, J.; Yang, G.Z.; Darzi, A. Natural orifice translumenal endoscopic surgery applications in clinical practice. World J. Gastrointest. Endosc. 2012, 4, 65–74. [Google Scholar] [CrossRef] [Green Version]
- Basol, G.; Cora, A.O.; Gundogdu, E.C.; Mat, E.; Yildiz, G.; Kuru, B.; Uzun, N.D.; Uzel, K.; Usta, T.; Kale, A. Hysterectomy via transvaginal natural orifice transluminal endoscopic surgery versus single-port laparoscopy: Comparison of early outcomes. J. Obstet. Gynaecol. Res. 2021, 47, 3288–3296. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.S.; Kim, S.Y.; Hur, M.H.; Oh, K.Y. Natural orifice transluminal endoscopic surgery-assisted versus single-port laparoscopic-assisted vaginal hysterectomy: A case-matched study. J. Minim. Invasive Gynecol. 2014, 21, 624–631. [Google Scholar] [CrossRef]
- Kim, M.S.; Noh, J.J.; Kim, T.J. Hysterectomy and Adnexal Procedures by Vaginal Natural Orifice Transluminal Endoscopic Surgery (VNH): Initial Findings From a Korean Surgeon. Front. Med. 2020, 7, 583147. [Google Scholar] [CrossRef] [PubMed]
- Noh, J.J.; Kim, T.H.; Kim, C.J.; Kim, T.J. Incisional hernia after 2498 single-port access (SPA) gynecologic surgery over a 10-year period. Sci. Rep. 2020, 10, 17388. [Google Scholar] [CrossRef] [PubMed]
- Michener, C.M.; Lampert, E.; Yao, M.; Harnegie, M.P.; Chalif, J.; Chambers, L.M. Meta-analysis of Laparoendoscopic Single-site and Vaginal Natural Orifice Transluminal Endoscopic Hysterectomy Compared with Multiport Hysterectomy: Real Benefits or Diminishing Returns? J. Minim. Invasive Gynecol. 2021, 28, 698–709.e1. [Google Scholar] [CrossRef]
- Al Wattar, B.H.; Vashisht, A.; Saridogan, E. Vaginal natural orifice transluminal endoscopic gynaecological surgery: Is it time to accept it as routine practice? BJOG 2021, 128, 1792. [Google Scholar] [CrossRef]
- Tinelli, A.; Tsin, D.A.; Forgione, A.; Zorron, R.; Dapri, G.; Malvasi, A.; Benhidjeb, T.; Sparic, R.; Nezhat, F. Exploring the umbilical and vaginal port during minimally invasive surgery. J. Turk. Ger. Gynecol. Assoc. 2017, 18, 143–147. [Google Scholar]
- Daniels, J. Reducing post-laparoscopy shoulder pain: Are simple strategies enough? BJOG 2018, 125, 1478. [Google Scholar] [CrossRef] [Green Version]
- Lee, C.L.; Wu, K.Y.; Su, H.; Wu, P.J.; Han, C.M.; Yen, C.F. Hysterectomy by transvaginal natural orifice transluminal endoscopic surgery (NOTES): A series of 137 patients. J. Minim. Invasive Gynecol. 2014, 21, 818–824. [Google Scholar] [CrossRef]
- Baekelandt, J. Total Vaginal NOTES Hysterectomy: A New Approach to Hysterectomy. J. Minim. Invasive Gynecol. 2015, 22, 1088–1094. [Google Scholar] [CrossRef] [PubMed]
- Bingener, J.; Sloan, J.A.; Ghosh, K.; McConico, A.; Mariani, A. Qualitative and quantitative analysis of women’s perceptions of transvaginal surgery. Surg. Endosc. 2012, 26, 998–1004. [Google Scholar] [CrossRef] [PubMed]
- Gerntke, C.I.; Kersten, J.F.; Schon, G.; Mann, O.; Stark, M.; Benhidjeb, T. Women’s Perception of Transvaginal Natural Orifice Transluminal Endoscopic Surgery (NOTES): Results of a Survey of Female Medical Staff and Literature Review. Surg. Innov. 2016, 23, 201–211. [Google Scholar] [CrossRef] [PubMed]
| vNOTES (n = 33) | SPA (n = 40) | p-Value | |
|---|---|---|---|
| Age (years) | 48.0 ± 4.1 | 47.5 ± 4.7 | 0.615 |
| Parity 0 1 2 3 | 2 (6.1%) 7 (21.2%) 22 (66.7%) 2 (6.1%) | 5 (12.5%) 11 (27.5%) 23 (57.5%) 1 (2.5%) | 0.598 |
| Menopause No Yes | 30 (90.9%) 3 (9.1%) | 38 (95.0%) 2 (5.0%) | 0.823 |
| BMIa (kg/m2) | 22.4 (21.1, 24.2) | 23.8 (21.3, 26.0) | 0.091 |
| History of vaginal delivery No Yes | 2 (6.5%) 29 (93.5%) | 19 (54.3%) 16 (45.7%) | < 0.001 |
| History of previous abdominal surgery Appendectomy, laparotomy Appendectomy, laparoscopy Cholecystectomy, laparotomy Cholecystectomy, laparoscopy Myomectomy, laparoscopy Myomectomy, laparotomy Salpingectomy, laparoscopy HIFU a | 1 (3.0%) 3 (9.1%) 0 0 2 (6.1%) 0 1 (3.0%) 0 | 0 2 (5.0%) 1 (2.5%) 1 (2.5%) 1 (2.5%) 1 (2.5%) 2 (5.0%) 1 (2.5%) | 0.480 |
| Size of the uterus (cm) Length Anterior-posterior (AP) | 10.2 ± 2.1 6.9 ± 1.9 | 10.9 ± 2.5 8.0 ± 2.7 | 0.245 0.084 |
| vNOTES (n = 33) | SPA (n = 40) | p-Value | |
|---|---|---|---|
| Operationa SPA-TLH, US SPA-TLH, BS SPA-TLH, USO, US SPA-TLH, BSO vNOTES-H, US vNOTES-H, BS vNOTES-H, USO, US vNOTES-H, BSO | 0 0 0 0 1 (3.0%) 25 (75.8%) 2 (6.0%) 5 (15.2%) | 2 (5.0%) 23 (27.5%) 7 (17.5%) 8 (20.0%) 0 0 0 0 | N/A |
| Estimated blood loss (ml) | 150 (50, 200) | 100 (90, 200) | 0.446 |
| Hemoglobin changes (g/dL) b | −1.3 (−2.1, −0.8) | −1.7 (−2.6, −1.0) | 0.136 |
| Post-operative hospital stay (days) 1 2 3 | 1 (3.0%) 29 (87.9%) 3 (9.1%) | 0 39 (97.5%) 1 (2.5%) | 0.243 |
| Post-operative diagnosis Uterine leiomyoma Adenomyosis Others | 23 (69.7%) 5 (15.2%) 5 (15.2%) | 26 (65.0%) 11 (27.5%) 3 (7.5%) | 0.250 |
| Median uterine weight (g) | 317.9 ± 161.1 | 408.8 ± 252.3 | 0.095 |
| Conversion of surgical methods | 0 | 0 | |
| Pain score (Visual Analog Scale) Post-operative 12 h Post-operative 24 h | 2.1 ± 2.4 1.9 ± 2.4 | 3.4 ± 2.7 2.8 ± 1.6 | 0.033 0.070 |
| Rescue analgesics requested on PODa1 None NSAIDsa Meperidine | 28 4 1 | 32 7 1 | 0.811 |
| Immediate post-operative complications | 0 | 0 | |
| Delayed post-operative complications | 1 | 0 |
| vNOTES (n = 33) | SPA (n = 40) | p-Value | |
|---|---|---|---|
| Completion of port installation | 18.0 (14.0, 20.0) | 5.0 (3.5, 5.5) | < 0.001 |
| Uterine artery ligation a Right Left | N/A N/A | 5.0 (3.0, 11.0) 5.5 (2.5, 10.5) | N/A N/A |
| Adnexal surgery Right Left | 5.0 (2.5, 7.5) 3.0 (2.0, 5.0) | 3.0 (1.5, 4.5) 4.5 (2.0, 6.0) | 0.134 0.479 |
| Vesicovaginal space dissection | N/A | 5.8 ± 2.7 | N/A |
| Colpotomy | N/A | 5.0 (3.5, 9.0) | N/A |
| Vaginal closure | 6.0 (4.0, 8.0) | 12.5 (10.0, 16.0) | <0.001 |
| Bleeding control | 4.0 (2.5, 7.0) | 4.0 (1.0, 9.5) | 0.863 |
| Abdominal wound closure | N/A | 13.0 (10.0, 16.0) | N/A |
| Total | 64.0 (46.0, 82.0) | 82.0 (68.5, 121.0) | <0.001 |
| Information | |
|---|---|
| Age | 48 |
| Chief complaint | Heavy menstrual bleeding, dysmenorrhea |
| Parity | Term delivery: 3 Preterm delivery: 0 Abortion: 1 Number of vaginal delivery: 3 |
| Menopausal status | Pre-menopausal |
| Medical/operative history | None |
| Pre-operative ultrasonography findings | Size of the uterus: 9.23 cm × 6.48 cm (length x anterior-posterior) Number of leiomyoma: 1 Size of leiomyoma: 6.83 cm (longest diameter) Location of leiomyoma: posterior wall Fallopian tubes and ovaries: unremarkable |
| Operative information | Operation name: vNOTESa-hysterectomy and bilateral salpingectomy Operation time Completion of port installation: 20 min Cold knife morcellation: 15 min Bilateral salpingectomy: 8 min Bleeding control: 7 min Vaginal closure: 6 min Total: 76 min |
| Intra-operative events | None |
| Events during hospitalization | None |
| Pre-operative hemoglobin levels (g/dl) | 13.9 |
| Post-operative hemoglobin levels (g/dl) | 10.0 |
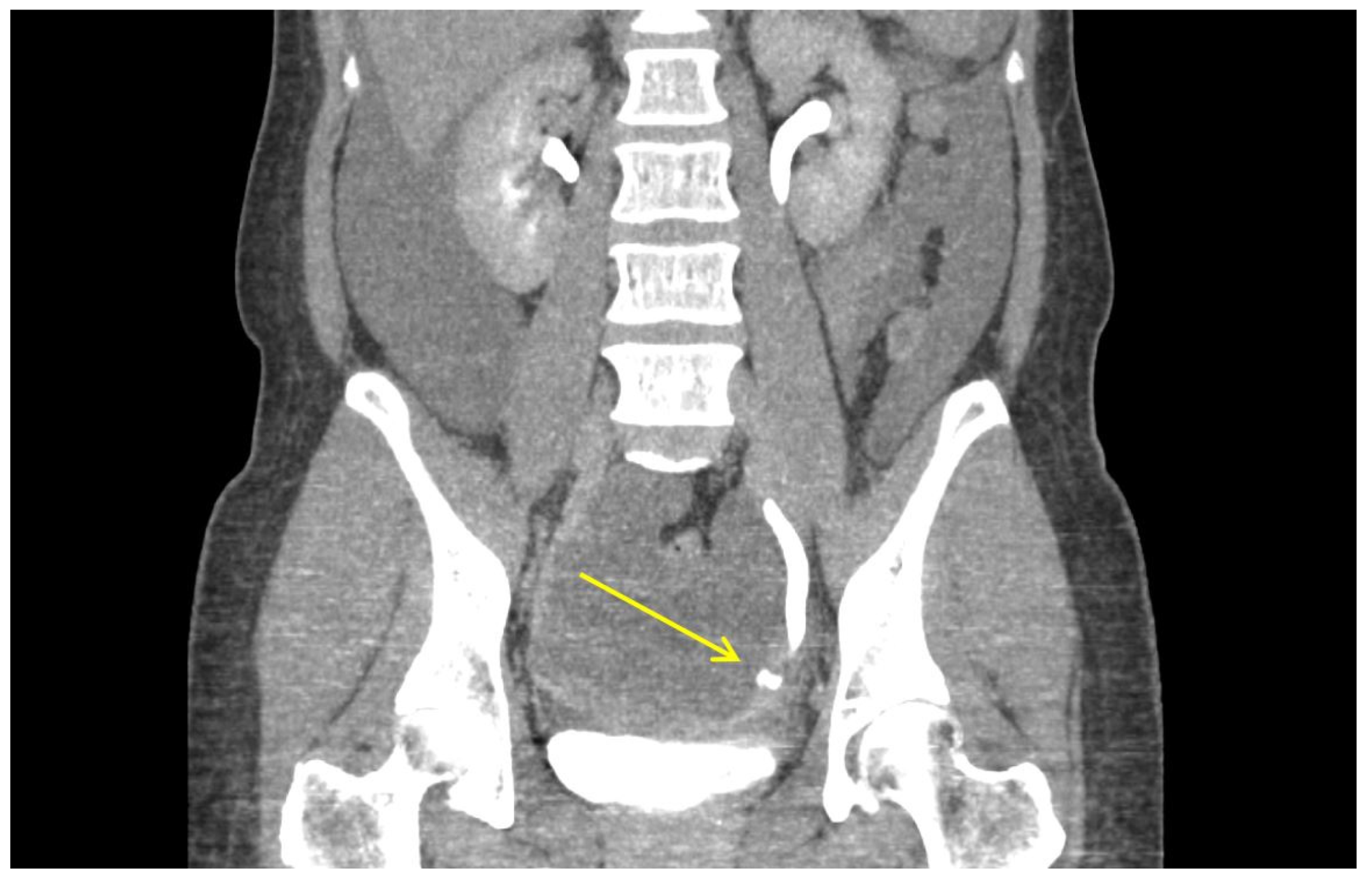
| Post-operative urography CT a findings | Profuse amount of fluid collection in the abdominal cavity. Contrast leakage at left distal ureter during the excretory phase. No hydronephrosis in both ureters. Mild peritoneal thickening, suggestive of peritonitis. Otherwise unremarkable. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Noh, J.J.; Kim, M.-S.; Kang, J.-H.; Jung, J.-H.; Chang, C.-S.; Jeon, J.; Kim, T.-J. Comparison of Surgical Outcomes of Hysterectomy by Vaginal Natural Orifice Transluminal Endoscopic Surgery (vNOTES) versus Single-Port Access (SPA) Surgery. J. Pers. Med. 2022, 12, 875. https://doi.org/10.3390/jpm12060875
Noh JJ, Kim M-S, Kang J-H, Jung J-H, Chang C-S, Jeon J, Kim T-J. Comparison of Surgical Outcomes of Hysterectomy by Vaginal Natural Orifice Transluminal Endoscopic Surgery (vNOTES) versus Single-Port Access (SPA) Surgery. Journal of Personalized Medicine. 2022; 12(6):875. https://doi.org/10.3390/jpm12060875
Chicago/Turabian StyleNoh, Joseph J., Myeong-Seon Kim, Jun-Hyeok Kang, Ji-Hee Jung, Chi-Son Chang, Jungeun Jeon, and Tae-Joong Kim. 2022. "Comparison of Surgical Outcomes of Hysterectomy by Vaginal Natural Orifice Transluminal Endoscopic Surgery (vNOTES) versus Single-Port Access (SPA) Surgery" Journal of Personalized Medicine 12, no. 6: 875. https://doi.org/10.3390/jpm12060875
APA StyleNoh, J. J., Kim, M.-S., Kang, J.-H., Jung, J.-H., Chang, C.-S., Jeon, J., & Kim, T.-J. (2022). Comparison of Surgical Outcomes of Hysterectomy by Vaginal Natural Orifice Transluminal Endoscopic Surgery (vNOTES) versus Single-Port Access (SPA) Surgery. Journal of Personalized Medicine, 12(6), 875. https://doi.org/10.3390/jpm12060875






