Personalized Management of Patients with Chronic Rhinosinusitis with Nasal Polyps in Clinical Practice: A Multidisciplinary Consensus Statement
Abstract
:1. Introduction
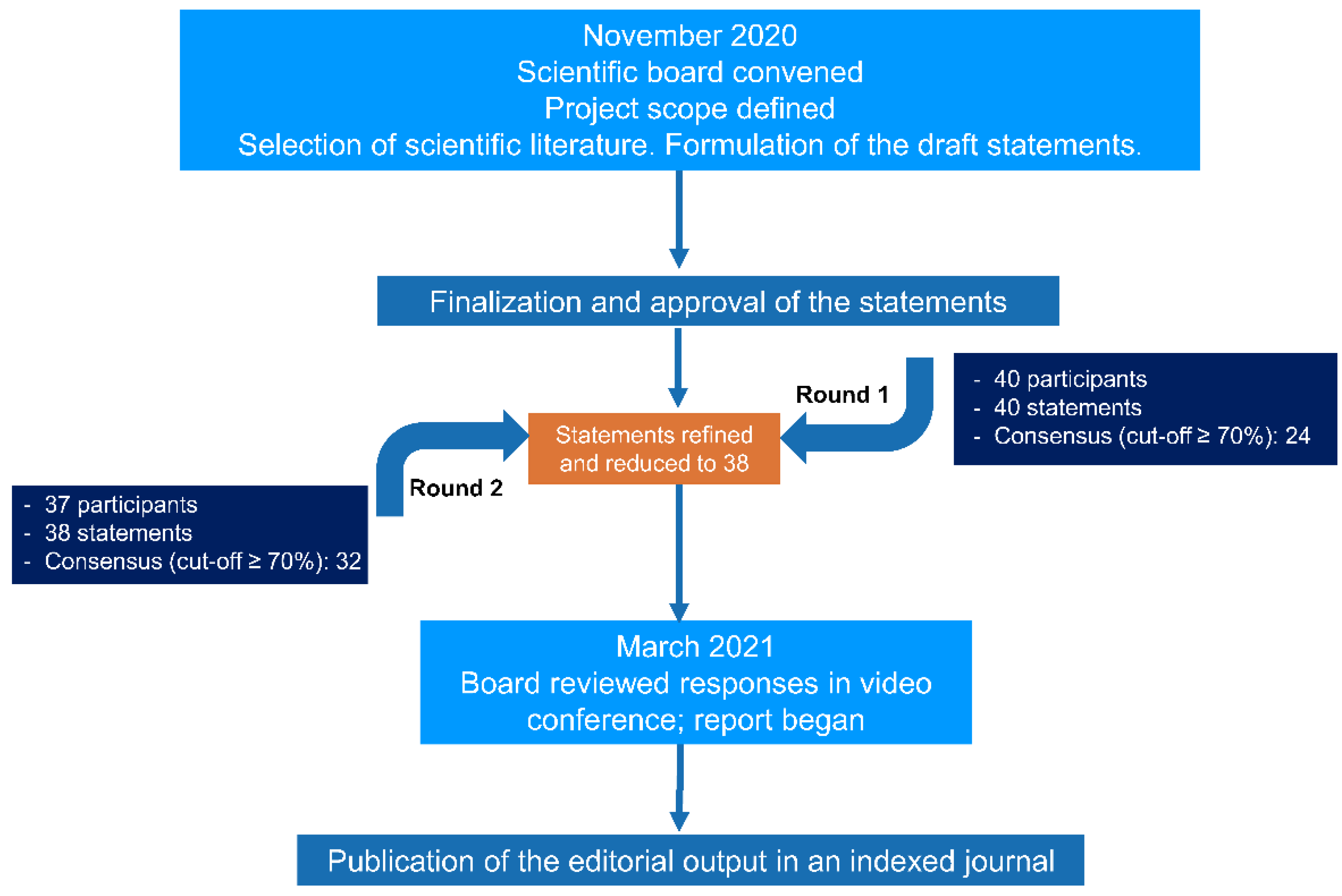
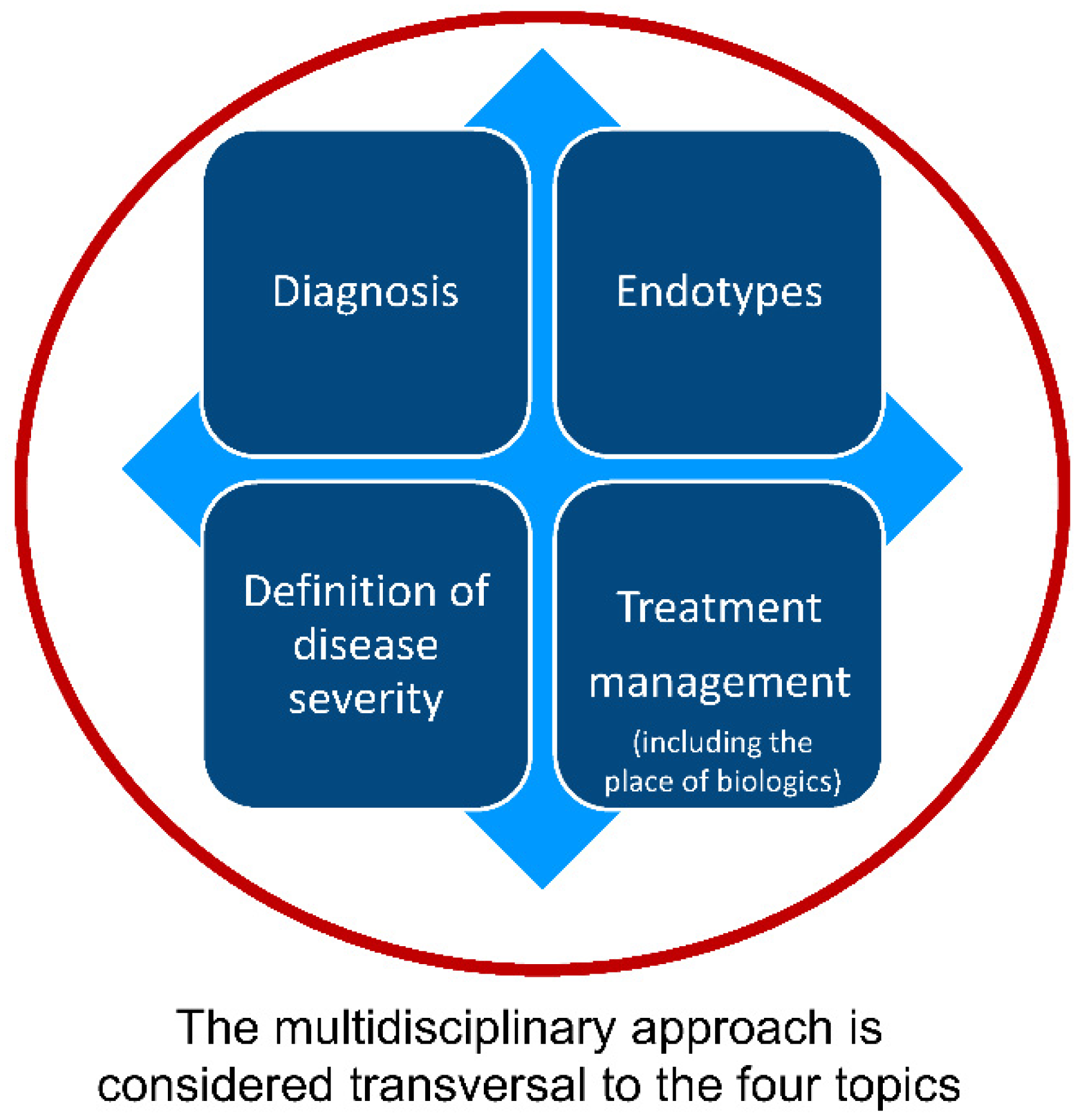
2. Materials and Methods
2.1. Design
2.2. Development of Consensus Statements
2.3. Ethics
2.4. Data Analysis
3. Results and Discussion
3.1. Diagnostic Work-Up (Statements 1–6)
3.1.1. Summary of Statements
3.1.2. Discussion
3.2. Endotyping (Statements 7–11)
3.2.1. Summary of Statements
3.2.2. Discussion
3.3. Disease Severity and Control (Statements 12–21)
3.3.1. Summary of Statements
3.3.2. Discussion
3.4. Management of Uncontrolled Severe CRSwNP with Biologics (Statements 22–35)
3.4.1. Summary of Statements
3.4.2. Use of Biologics in Patients Never Treated by Surgery
3.4.3. Supportive Role of Surgery during Treatment with Biologics
3.4.4. Use of Biologics in patients who have Undergone Multiple Surgeries
3.4.5. Evaluation of Response to Biologics
3.5. Open Questions to Be Addressed in Clinical Trials (Statements 36–38)
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Search Strategy
Appendix B. Members of the Panel of Experts and Their Specialty
References
- Fokkens, W.J.; Lund, V.J.; Hopkins, C.; Hellings, P.W.; Kern, R.; Reitsma, S.; Toppila-Salmi, S.; Bernal-Sprekelsen, M.; Mullol, J.; Alobid, I.; et al. European Position Paper on Rhinosinusitis and Nasal Polyps 2020. Rhinology 2020, 58, 1–464. [Google Scholar] [CrossRef]
- Bachert, C.; Marple, B.; Schlosser, R.J.; Hopkins, C.; Schleimer, R.P.; Lambrecht, B.N.; Broker, B.M.; Laidlaw, T.; Song, W.J. Adult chronic rhinosinusitis. Nat. Rev. Dis. Primers 2020, 6, 86. [Google Scholar] [CrossRef] [PubMed]
- Hastan, D.; Fokkens, W.J.; Bachert, C.; Newson, R.B.; Bislimovska, J.; Bockelbrink, A.; Bousquet, P.J.; Brozek, G.; Bruno, A.; Dahlen, S.E.; et al. Chronic rhinosinusitis in Europe--an underestimated disease. A GA(2)LEN study. Allergy 2011, 66, 1216–1223. [Google Scholar] [CrossRef] [PubMed]
- Palmer, J.N.; Messina, J.C.; Biletch, R.; Grosel, K.; Mahmoud, R.A. A cross-sectional, population-based survey of U.S. adults with symptoms of chronic rhinosinusitis. Allergy Asthma Proc. 2019, 40, 48–56. [Google Scholar] [CrossRef] [PubMed]
- Dietz de Loos, D.; Lourijsen, E.S.; Wildeman, M.A.M.; Freling, N.J.M.; Wolvers, M.D.J.; Reitsma, S.; Fokkens, W.J. Prevalence of chronic rhinosinusitis in the general population based on sinus radiology and symptomatology. J. Allergy Clin. Immunol. 2019, 143, 1207–1214. [Google Scholar] [CrossRef]
- Hirsch, A.G.; Stewart, W.F.; Sundaresan, A.S.; Young, A.J.; Kennedy, T.L.; Scott Greene, J.; Feng, W.; Tan, B.K.; Schleimer, R.P.; Kern, R.C.; et al. Nasal and sinus symptoms and chronic rhinosinusitis in a population-based sample. Allergy 2017, 72, 274–281. [Google Scholar] [CrossRef]
- Khan, A.; Vandeplas, G.; Huynh, T.M.T.; Joish, V.N.; Mannent, L.; Tomassen, P.; Van Zele, T.; Cardell, L.O.; Arebro, J.; Olze, H.; et al. The Global Allergy and Asthma European Network (GALEN rhinosinusitis cohort: A large European cross-sectional study of chronic rhinosinusitis patients with and without nasal polyps. Rhinology 2019, 57, 32–42. [Google Scholar] [CrossRef] [Green Version]
- Chen, S.; Zhou, A.; Emmanuel, B.; Thomas, K.; Guiang, H. Systematic literature review of the epidemiology and clinical burden of chronic rhinosinusitis with nasal polyposis. Curr. Med. Res. Opin. 2020, 36, 1897–1911. [Google Scholar] [CrossRef]
- Roland, L.T.; Smith, T.L.; Schlosser, R.J.; Soler, Z.M.; Peters, A.T.; Laidlaw, T.M.; Bleier, B.S.; Ramakrishnan, V.; Toskala, E.; Kennedy, D.W.; et al. Guidance for contemporary use of biologics in management of chronic rhinosinusitis with nasal polyps: Discussion from a National Institutes of Health-sponsored workshop. Int. Forum. Allergy Rhinol. 2020, 10, 1037–1042. [Google Scholar] [CrossRef]
- Bachert, C.; Han, J.K.; Wagenmann, M.; Hosemann, W.; Lee, S.E.; Backer, V.; Mullol, J.; Gevaert, P.; Klimek, L.; Prokopakis, E.; et al. EUFOREA expert board meeting on uncontrolled severe chronic rhinosinusitis with nasal polyps (CRSwNP) and biologics: Definitions and management. J. Allergy Clin. Immunol. 2021, 147, 29–36. [Google Scholar] [CrossRef]
- Bachert, C.; Zhang, N.; Hellings, P.W.; Bousquet, J. Endotype-driven care pathways in patients with chronic rhinosinusitis. J. Allergy Clin. Immunol. 2018, 141, 1543–1551. [Google Scholar] [CrossRef] [PubMed]
- van der Veen, J.; Seys, S.F.; Timmermans, M.; Levie, P.; Jorissen, M.; Fokkens, W.J.; Hellings, P.W. Real-life study showing uncontrolled rhinosinusitis after sinus surgery in a tertiary referral centre. Allergy 2017, 72, 282–290. [Google Scholar] [CrossRef] [PubMed]
- Fokkens, W.J.; Lund, V.; Bachert, C.; Mullol, J.; Bjermer, L.; Bousquet, J.; Canonica, G.W.; Deneyer, L.; Desrosiers, M.; Diamant, Z.; et al. EUFOREA consensus on biologics for CRSwNP with or without asthma. Allergy 2019, 74, 2312–2319. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hakansson, K.; Thomsen, S.F.; Konge, L.; Mortensen, J.; Backer, V.; von Buchwald, C. A comparative and descriptive study of asthma in chronic rhinosinusitis with nasal polyps. Am. J. Rhinol. Allergy 2014, 28, 383–387. [Google Scholar] [CrossRef]
- Bachert, C.; Zhang, N.; Cavaliere, C.; Weiping, W.; Gevaert, E.; Krysko, O. Biologics for chronic rhinosinusitis with nasal polyps. J. Allergy Clin. Immunol. 2020, 145, 725–739. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- European Medicines Agency. Dupixent (Dupilumab). Summary of Product Characteristics. 2021. Available online: https://www.ema.europa.eu/en/documents/product-information/dupixent-epar-product-information_en.pdf (accessed on 12 July 2021).
- European Medicines Agency. Xolair (Omalizumab). Summary of Product Characteristics. 2020. Available online: https://www.ema.europa.eu/en/documents/product-information/xolair-epar-product-information_en.pdf (accessed on 12 July 2021).
- Han, J.K.; Bachert, C.; Fokkens, W.; Desrosiers, M.; Wagenmann, M.; Lee, S.E.; Smith, S.G.; Martin, N.; Mayer, B.; Yancey, S.W.; et al. Mepolizumab for chronic rhinosinusitis with nasal polyps (SYNAPSE): A randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Respir. Med. 2021, 9, 1141–1153. [Google Scholar] [CrossRef]
- Canonica, G.W.; Harrison, T.W.; Chanez, P.; Menzella, F.; Louis, R.; Cosio, B.G.; Lugogo, N.L.; Mohan, A.; Burden, A.; Garcia Gil, E. Benralizumab improves symptoms of patients with severe, eosinophilic asthma with a diagnosis of nasal polyposis. Allergy 2022, 7, 150–161. [Google Scholar] [CrossRef]
- Bachert, C.; Marple, B.; Hosemann, W.; Cavaliere, C.; Wen, W.; Zhang, N. Endotypes of Chronic Rhinosinusitis with Nasal Polyps: Pathology and Possible Therapeutic Implications. J. Allergy Clin. Immunol. Pract. 2020, 8, 1514–1519. [Google Scholar] [CrossRef]
- Ciprandi, G.; Gelardi, M. Chronic rhinosinusitis with nasal polyposis: The role of personalized and integrated medicine. Monaldi. Arch. Chest. Dis. 2021, 91, 3. [Google Scholar] [CrossRef]
- Hasson, F.; Keeney, S.; McKenna, H. Research guidelines for the Delphi survey technique. J. Adv. Nurs. 2000, 32, 1008–1015. [Google Scholar]
- Vogel, C.; Zwolinsky, S.; Griffiths, C.; Hobbs, M.; Henderson, E.; Wilkins, E. A Delphi study to build consensus on the definition and use of big data in obesity research. Int. J. Obes. 2019, 43, 2573–2586. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bachert, C.; Han, J.K.; Desrosiers, M.; Hellings, P.W.; Amin, N.; Lee, S.E.; Mullol, J.; Greos, L.S.; Bosso, J.V.; Laidlaw, T.M.; et al. Efficacy and safety of dupilumab in patients with severe chronic rhinosinusitis with nasal polyps (LIBERTY NP SINUS-24 and LIBERTY NP SINUS-52): Results from two multicentre, randomised, double-blind, placebo-controlled, parallel-group phase 3 trials. Lancet 2019, 394, 1638–1650. [Google Scholar] [CrossRef] [Green Version]
- Gevaert, P.; Omachi, T.A.; Corren, J.; Mullol, J.; Han, J.; Lee, S.E.; Kaufman, D.; Ligueros-Saylan, M.; Howard, M.; Zhu, R.; et al. Efficacy and safety of omalizumab in nasal polyposis: 2 randomized phase 3 trials. J. Allergy Clin. Immunol. 2020, 146, 595–605. [Google Scholar] [CrossRef] [PubMed]
- De Corso, E.; Lucidi, D.; Battista, M.; Romanello, M.; De Vita, C.; Baroni, S.; Autilio, C.; Galli, J.; Paludetti, G. Prognostic value of nasal cytology and clinical factors in nasal polyps development in patients at risk: Can the beginning predict the end? Int. Forum. Allergy Rhinol. 2017, 7, 861–867. [Google Scholar] [CrossRef]
- Gelardi, M.; Iannuzzi, L.; Tafuri, S.; Passalacqua, G.; Quaranta, N. Allergic and non-allergic rhinitis: Relationship with nasal polyposis, asthma and family history. Acta Otorhinolaryngol. Ital. 2014, 34, 36–41. [Google Scholar]
- Latorre, M.; Bacci, E.; Seccia, V.; Bartoli, M.L.; Cardini, C.; Cianchetti, S.; Cristofani, L.; Di Franco, A.; Miccoli, M.; Puxeddu, I.; et al. Upper and lower airway inflammation in severe asthmatics: A guide for a precision biologic treatment. Ther. Adv. Respir. Dis. 2020, 14, 1753466620965151. [Google Scholar] [CrossRef]
- Philpott, C.M.; Erskine, S.; Hopkins, C.; Kumar, N.; Anari, S.; Kara, N.; Sunkaraneni, S.; Ray, J.; Clark, A.; Wilson, A.; et al. Prevalence of asthma, aspirin sensitivity and allergy in chronic rhinosinusitis: Data from the UK National Chronic Rhinosinusitis Epidemiology Study. Respir. Res. 2018, 19, 129. [Google Scholar] [CrossRef] [Green Version]
- Canonica, G.W.; Malvezzi, L.; Blasi, F.; Paggiaro, P.; Mantero, M.; Senna, G.; Heffler, E.; Severe Asthma Network, I. Chronic rhinosinusitis with nasal polyps impact in severe asthma patients: Evidences from the Severe Asthma Network Italy (SANI) registry. Respir. Med. 2020, 166, 105947. [Google Scholar] [CrossRef]
- Stevens, W.W.; Peters, A.T.; Hirsch, A.G.; Nordberg, C.M.; Schwartz, B.S.; Mercer, D.G.; Mahdavinia, M.; Grammer, L.C.; Hulse, K.E.; Kern, R.C.; et al. Clinical Characteristics of Patients with Chronic Rhinosinusitis with Nasal Polyps, Asthma, and Aspirin-Exacerbated Respiratory Disease. J. Allergy Clin. Immunol. Pract. 2017, 5, 1061–1070. [Google Scholar] [CrossRef]
- Orlandi, R.R.; Kingdom, T.T.; Hwang, P.H. International Consensus Statement on Allergy and Rhinology: Rhinosinusitis Executive Summary. Int. Forum. Allergy Rhinol. 2016, 6 (Suppl. 1), S3–S21. [Google Scholar] [CrossRef]
- Ho, J.; Alvarado, R.; Rimmer, J.; Sewell, W.A.; Harvey, R.J. Atopy in chronic rhinosinusitis: Impact on quality of life outcomes. Int. Forum. Allergy Rhinol. 2019, 9, 501–507. [Google Scholar] [CrossRef] [PubMed]
- Ramadan, H.H.; Fornelli, R.; Ortiz, A.O.; Rodman, S. Correlation of allergy and severity of sinus disease. Am. J. Rhinol. 1999, 13, 345–347. [Google Scholar] [CrossRef] [PubMed]
- Erbek, S.S.; Erbek, S.; Topal, O.; Cakmak, O. The role of allergy in the severity of nasal polyposis. Am. J. Rhinol. 2007, 21, 686–690. [Google Scholar] [CrossRef] [PubMed]
- Görgülü, O.; Ozdemir, S.; Canbolat, E.P.; Sayar, C.; Olgun, M.K.; Akbaş, Y. Analysis of the roles of smoking and allergy in nasal polyposis. Ann. Otol. Rhinol. Laryngol. 2012, 121, 615–619. [Google Scholar] [CrossRef]
- Pearlman, A.N.; Chandra, R.K.; Chang, D.; Conley, D.B.; Tripathi-Peters, A.; Grammer, L.C.; Schleimer, R.T.; Kern, R.C. Relationships between severity of chronic rhinosinusitis and nasal polyposis, asthma, and atopy. Am. J. Rhinol. Allergy 2009, 23, 145–148. [Google Scholar] [CrossRef] [Green Version]
- Groger, M.; Bernt, A.; Wolf, M.; Mack, B.; Pfrogner, E.; Becker, S.; Kramer, M.F. Eosinophils and mast cells: A comparison of nasal mucosa histology and cytology to markers in nasal discharge in patients with chronic sino-nasal diseases. Eur. Arch. Otorhinolaryngol. 2013, 270, 2667–2676. [Google Scholar] [CrossRef]
- She, W.; Yang, J.; Wang, C.; Zhang, L. Diagnostic Value of Nasal Cytology in Chronic Rhinosinusitis Assessed by a Liquid-based Cytological Technique. Am. J. Rhinol. Allergy 2018, 32, 181–187. [Google Scholar] [CrossRef]
- Zhu, Z.; Wang, W.; Zhang, X.; Wang, X.; Zha, Y.; Chen, Y.; Zhou, L.; Lv, W. Nasal fluid cytology and cytokine profiles of eosinophilic and non-eosinophilic chronic rhinosinusitis with nasal polyps. Rhinology 2020, 58, 314–322. [Google Scholar] [CrossRef]
- Gallo, S.; Bandi, F.; Preti, A.; Facco, C.; Ottini, G.; Di Candia, F.; Mozzanica, F.; Saderi, L.; Sessa, F.; Reguzzoni, M.; et al. Exploring the role of nasal cytology in chronic rhinosinusitis. Acta Otorhinolaryngol. Ital. 2020, 40, 368–376. [Google Scholar] [CrossRef]
- Heffler, E.; Landi, M.; Caruso, C.; Fichera, S.; Gani, F.; Guida, G.; Liuzzo, M.T.; Pistorio, M.P.; Pizzimenti, S.; Riccio, A.M.; et al. Nasal cytology: Methodology with application to clinical practice and research. Clin. Exp. Allergy 2018, 48, 1092–1106. [Google Scholar] [CrossRef]
- Akdis, C.A.; Bachert, C.; Cingi, C.; Dykewicz, M.S.; Hellings, P.W.; Naclerio, R.M.; Schleimer, R.P.; Ledford, D. Endotypes and phenotypes of chronic rhinosinusitis: A PRACTALL document of the European Academy of Allergy and Clinical Immunology and the American Academy of Allergy, Asthma & Immunology. J. Allergy Clin. Immunol. 2013, 131, 1479–1490. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cardell, L.O.; Stjarne, P.; Jonstam, K.; Bachert, C. Endotypes of chronic rhinosinusitis: Impact on management. J. Allergy Clin. Immunol. 2020, 145, 752–756. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tomassen, P.; Vandeplas, G.; Van Zele, T.; Cardell, L.O.; Arebro, J.; Olze, H.; Forster-Ruhrmann, U.; Kowalski, M.L.; Olszewska-Ziaber, A.; Holtappels, G.; et al. Inflammatory endotypes of chronic rhinosinusitis based on cluster analysis of biomarkers. J. Allergy Clin. Immunol. 2016, 137, 1449–1456. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Armengot, M.; Garin, L.; de Lamo, M.; Krause, F.; Carda, C. Cytological and tissue eosinophilia correlations in nasal polyposis. Am. J. Rhinol. Allergy 2010, 24, 413–415. [Google Scholar] [CrossRef] [PubMed]
- Scheerens, H.; Smith, A.; Li, O.; Honigberg, L.; Harris, J.M.; Holtappels, G.; Bachert, C. Elevated IgE M1 prime transcripts in nasal tissues in patients with nasal polyps and asthma. J. Allergy Clin. Immunol. 2019, 143, 805–807. [Google Scholar] [CrossRef] [Green Version]
- Bachert, C.; Bhattacharyya, N.; Desrosiers, M.; Khan, A.H. Burden of disease in chronic rhinosinusitis with nasal polyps. J. Asthma Allergy 2021, 14, 127–134. [Google Scholar] [CrossRef]
- Bachert, C.; Zhang, N.; Holtappels, G.; De Lobel, L.; van Cauwenberge, P.; Liu, S.; Lin, P.; Bousquet, J.; Van Steen, K. Presence of IL-5 protein and IgE antibodies to staphylococcal enterotoxins in nasal polyps is associated with comorbid asthma. J. Allergy Clin. Immunol. 2010, 126, 962–968. [Google Scholar] [CrossRef] [Green Version]
- Flora, M.; Perrotta, F.; Nicolai, A.; Maffucci, R.; Pratillo, A.; Mollica, M.; Bianco, A.; Calabrese, C. Staphylococcus Aureus in chronic airway diseases: An overview. Respir. Med. 2019, 155, 66–71. [Google Scholar] [CrossRef]
- Gevaert, P.; Calus, L.; Van Zele, T.; Blomme, K.; De Ruyck, N.; Bauters, W.; Hellings, P.; Brusselle, G.; De Bacquer, D.; van Cauwenberge, P.; et al. Omalizumab is effective in allergic and nonallergic patients with nasal polyps and asthma. J. Allergy Clin. Immunol. 2013, 131, 110–116. [Google Scholar] [CrossRef]
- Rha, M.S.; Kim, S.W.; Chang, D.Y.; Lee, J.K.; Kim, J.; Park, S.H.; Khalmuratova, R.; Lim, H.S.; Eun, K.M.; Hong, S.N.; et al. Superantigen-related TH2 CD4(+) T cells in nonasthmatic chronic rhinosinusitis with nasal polyps. J. Allergy Clin. Immunol. 2020, 145, 1378–1388. [Google Scholar] [CrossRef] [Green Version]
- Vickery, T.W.; Ramakrishnan, V.R.; Suh, J.D. The Role of Staphylococcus aureus in Patients with Chronic Sinusitis and Nasal Polyposis. Curr. Allergy Asthma Rep. 2019, 19, 21. [Google Scholar] [CrossRef] [PubMed]
- De Corso, E.; Settimi, S.; Tricarico, L.; Mele, D.A.; Mastrapasqua, R.F.; Di Cesare, T.; Salvati, A.; Trozzi, L.; De Vita, C.; Romanello, M.; et al. Predictors of disease control after endoscopic sinus surgery plus long-term local corticosteroids in CRSwNP. Am. J. Rhinol. Allergy 2021, 35, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Staudacher, A.G.; Peters, A.T.; Kato, A.; Stevens, W.W. Use of endotypes, phenotypes, and inflammatory markers to guide treatment decisions in chronic rhinosinusitis. Ann. Allergy Asthma Immunol. 2020, 124, 318–325. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gelardi, M.; Cassano, M.; Ciprandi, G. The clinical relevance of the clinical cytological grading in patients with chronic rhinosinusitis with nasal polyps. J. Allergy Clin. Immunol. 2020, 146, 462–463. [Google Scholar] [CrossRef]
- Gelardi, M.; Iannuzzi, L.; De Giosa, M.; Taliente, S.; De Candia, N.; Quaranta, N.; De Corso, E.; Seccia, V.; Ciprandi, G. Non-surgical management of chronic rhinosinusitis with nasal polyps based on clinical-cytological grading: A precision medicine-based approach. Acta Otorhinolaryngol. Ital. 2017, 37, 38–45. [Google Scholar] [CrossRef]
- Gelardi, M.; Porro, G.; Quaranta, V.; Quaranta, N.; Cassano, M.; Ciprandi, G.; Study Group On, C.I. Clinical-Cytological-Grading and phenotyping in patients with chronic rhinosinusitis with nasal polyps: The relevance in clinical practice. Monaldi. Arch. Chest Dis. 2020, 90, 2. [Google Scholar] [CrossRef]
- Gallo, S.; Russo, F.; Mozzanica, F.; Preti, A.; Bandi, F.; Costantino, C.; Gera, R.; Ottaviani, F.; Castelnuovo, P. Prognostic value of the Sinonasal Outcome Test 22 (SNOT-22) in chronic rhinosinusitis. Acta Otorhinolaryngol. Ital. 2020, 40, 113–121. [Google Scholar] [CrossRef]
- Gray, S.T.; Phillips, K.M.; Hoehle, L.P.; Caradonna, D.S.; Sedaghat, A.R. The 22-item Sino-Nasal Outcome Test accurately reflects patient-reported control of chronic rhinosinusitis symptomatology. Int. Forum. Allergy Rhinol. 2017, 7, 945–951. [Google Scholar] [CrossRef]
- Phillips, K.M.; Hoehle, L.P.; Bergmark, R.W.; Campbell, A.P.; Caradonna, D.S.; Gray, S.T.; Sedaghat, A.R. Chronic rhinosinusitis severity is associated with need for asthma-related systemic corticosteroids. Rhinology 2017, 55, 211–217. [Google Scholar] [CrossRef]
- Rudmik, L.; Soler, Z.M.; Mace, J.C.; DeConde, A.S.; Schlosser, R.J.; Smith, T.L. Using preoperative SNOT-22 score to inform patient decision for Endoscopic sinus surgery. Laryngoscope 2015, 125, 1517–1522. [Google Scholar] [CrossRef] [Green Version]
- Gray, S.T.; Phillips, K.M.; Hoehle, L.P.; Feng, A.L.; Yamasaki, A.; Caradonna, D.S.; Sedaghat, A.R. Utilization patterns of systemic corticosteroid use for chronic rhinosinusitis. Acta Otolaryngol. 2018, 138, 153–158. [Google Scholar] [CrossRef] [PubMed]
- Bourdin, A.; Adcock, I.; Berger, P.; Bonniaud, P.; Chanson, P.; Chenivesse, C.; de Blic, J.; Deschildre, A.; Devillier, P.; Devouassoux, G.; et al. How can we minimise the use of regular oral corticosteroids in asthma? Eur. Respir. Rev. 2020, 29, 190085. [Google Scholar] [CrossRef] [PubMed]
- Alanin, M.C.; Laidlaw, T.; Society, T.S.; Hopkins, C. The Burden of Non-steroidal anti-inflammatory exacerbated respiratory disease from the patient’s perspective—A qualitative analysis of posts from the Samter’s Society. Rhinology 2020, 58, 333–340. [Google Scholar] [CrossRef] [PubMed]
- Forster-Ruhrmann, U.; Stergioudi, D.; Pierchalla, G.; Fluhr, J.W.; Bergmann, K.C.; Olze, H. Omalizumab in patients with NSAIDs-exacerbated respiratory disease. Rhinology 2020, 58, 226–232. [Google Scholar] [CrossRef]
- Kowalski, M.L.; Agache, I.; Bavbek, S.; Bakirtas, A.; Blanca, M.; Bochenek, G.; Bonini, M.; Heffler, E.; Klimek, L.; Laidlaw, T.M.; et al. Diagnosis and management of NSAID-Exacerbated Respiratory Disease (N-ERD)-a EAACI position paper. Allergy 2019, 74, 28–39. [Google Scholar] [CrossRef] [Green Version]
- Laidlaw, T.M.; Mullol, J.; Fan, C.; Zhang, D.; Amin, N.; Khan, A.; Chao, J.; Mannent, L.P. Dupilumab improves nasal polyp burden and asthma control in patients with CRSwNP and AERD. J. Allergy Clin. Immunol. Pract. 2019, 7, 2462–2465. [Google Scholar] [CrossRef] [Green Version]
- Laulajainen-Hongisto, A.; Turpeinen, H.; Vento, S.I.; Numminen, J.; Sahlman, J.; Kauppi, P.; Virkkula, P.; Hytonen, M.; Toppila-Salmi, S. High Discontinuation Rates of Peroral ASA Treatment for CRSwNP: A Real-World Multicenter Study of 171 N-ERD Patients. J. Allergy Clin. Immunol. Pract. 2020, 8, 3565–3574. [Google Scholar] [CrossRef]
- Mustafa, S.S.; Vadamalai, K. Dupilumab increases aspirin tolerance in aspirin-exacerbated respiratory disease. Ann. Allergy Asthma Immunol. 2021, 126, 738–739. [Google Scholar] [CrossRef]
- Steiner, U.C.; Bischoff, S.; Valaperti, A.; Ikenberg, K.; Starzyk, J.; Bucher, S.; Bachmann, L.M.; Soyka, M.B. Endotypes of chronic rhinosinusitis with nasal polyps with and without NSAID aeuro" intolerance. Rhinology 2020, 58, 544–549. [Google Scholar] [CrossRef]
- Workman, A.D.; Bleier, B.S. Biologic therapies versus surgical management for aspirin-exacerbated respiratory disease: A review of preliminary data, efficacy, and cost. World J. Otorhinolaryngol. Head Neck Surg. 2020, 6, 230–234. [Google Scholar] [CrossRef]
- De Corso, E.; Bellocchi, G.; De Benedetto, M.; Lombardo, N.; Macchi, A.; Malvezzi, L.; Motta, G.; Pagella, F.; Vicini, C.; Passali, D. Biologics for severe uncontrolled chronic rhinosinusitis with nasal polyps: A change management approach. Consensus of the Joint Committee of Italian Society of Otorhinolaryngology on biologics in rhinology. Acta Otorhinolaryngol. Ital. 2022, 42, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Bachert, C.; Sousa, A.R.; Lund, V.J.; Scadding, G.K.; Gevaert, P.; Nasser, S.; Durham, S.R.; Cornet, M.E.; Kariyawasam, H.H.; Gilbert, J.; et al. Reduced need for surgery in severe nasal polyposis with mepolizumab: Randomized trial. J. Allergy Clin. Immunol. 2017, 140, 1024–1031. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bachert, C.; Zhang, L.; Gevaert, P. Current and future treatment options for adult chronic rhinosinusitis: Focus on nasal polyposis. J. Allergy Clin. Immunol. 2015, 136, 1431–1440. [Google Scholar] [CrossRef]
- Blaiss, M.S. Chronic rhinosinusitis with nasal polyps management in the age of biologics. Allergy Asthma Proc. 2020, 41, 413–419. [Google Scholar] [CrossRef] [PubMed]
- Franzese, C.B. The Role of Biologics in the Treatment of Nasal Polyps. Immunol. Allergy Clin. N. Am. 2020, 40, 295–302. [Google Scholar] [CrossRef]
- Heffler, E.; Malvezzi, L.; Pirola, F.; Zieba, N.; Paoletti, G.; Mercante, G.; Spriano, G.; Canonica, G.W. Treatable traits in chronic rhinosinusitis with nasal polyps. Curr. Opin. Allergy Clin. Immunol. 2019, 19, 373–378. [Google Scholar] [CrossRef]
- Mortuaire, G.; Gengler, I.; Carpentier, C.; Szymanski, C.; Chenivesse, C.; Lefevre, G. T helper 2 inflammatory markers are associated with recurrence in chronic rhinosinusitis with nasal polyps after endoscopic sinus surgery. Rhinology 2020, 58, 444–450. [Google Scholar] [CrossRef]
- Rudmik, L.; Smith, T.L. Olfactory improvement after endoscopic sinus surgery. Curr. Opin. Otolaryngol. Head Neck Surg. 2012, 20, 29–32. [Google Scholar] [CrossRef] [Green Version]
- Mansi, A.; Bui, R.; Chaaban, M.R. Oral Corticosteroid Regimens in the Management of Chronic Rhinosinusitis. Ear Nose Throat J. 2020, 101, 145561319876906. [Google Scholar] [CrossRef]
- Numata, T.; Nakayama, K.; Utsumi, H.; Kobayashi, K.; Yanagisawa, H.; Hashimoto, M.; Minagawa, S.; Ishikawa, T.; Hara, H.; Araya, J.; et al. Efficacy of mepolizumab for patients with severe asthma and eosinophilic chronic rhinosinusitis. BMC Pulm. Med. 2019, 19, 176. [Google Scholar] [CrossRef] [Green Version]
- Ruan, J.W.; Zhao, J.F.; Li, X.L.; Liao, B.; Pan, L.; Zhu, K.Z.; Feng, Q.M.; Liu, J.X.; Yu, Z.E.; Song, J.; et al. Characterizing the neutrophilic inflammation in chronic rhinosinusitis with nasal polyps. Front. Cell Dev. Biol. 2021, 9, 793073. [Google Scholar] [CrossRef] [PubMed]
| No. | Statements by Topic | Response Rate, n/N (%) | % of Replies ≥ 4 a,b | Strongly Disagree | Disagree | Partially Agree | Agree | Strongly Agree |
|---|---|---|---|---|---|---|---|---|
| 1 | In patients with CRSwNP, olfaction should be routinely assessed by means of the University of Pennsylvania Smell Identification Test (UPSIT) or Sniffin’ sticks | 37/37 (100.0) | 67.6 | 2.7% | 2.7% | 27.03% | 24.32% | 43.24% |
| 2 | All patients with CRSwNP symptoms should be evaluated in a multidisciplinary fashion to detect the presence of asthma | 36/37 (97.3) | 88.9 | 2.78% | 0.00% | 8.33% | 33.33% | 55.56% |
| 3 | All patients with moderate/severe asthma should be routinely evaluated by an ear, nose and throat (ENT) specialist to detect the presence of chronic rhinosinusitis and/or nasal polyposis | 36/37 (97.3) | 91.7 | 2.78% | 2.78% | 2.78% | 25.00% | 66.67% |
| 4 | A multidisciplinary approach enables early detection and management of patients, thus preventing possible worsening of the disease | 36/37 (97.3) | 94.4 | 2.78% | 0.00% | 2.78% | 36.11% | 58.33 |
| 5 | All patients with CRSwNP should be routinely evaluated by a specialist to detect the presence of concomitant atopy with sensitization to aeroallergens and/or drug hypersensitivity | 36/37 (97.3) | 94.4 | 2.78% | 0.00% | 2.78% | 44.44% | 50.00% |
| 6 | Nasal cytology with sampling of the inferior turbinate is a simple, inexpensive, non-invasive method for the cellular phenotyping of nasal polyposis, and is applicable to outpatient settings | 36/37 (97.3) | 75.0 | 5.56% | 2.78% | 16.67% | 30.56% | 44.44% |
| No. | Statements by Topic | Response Rate, n/N (%) | % of Replies ≥ 4 a,b | Strongly Disagree | Disagree | Partially Agree | Agree | Strongly Agree |
|---|---|---|---|---|---|---|---|---|
| 7 | Values greater than 10 eosinophils per high-powered field (EOS/HPF) in biopsy specimens are indicative of type 2 inflammation | 36/37 (97.3) | 83.3 | 2.78% | 0.00% | 13.89% | 72.22% | 11.11% |
| 8 | Eosinophil cut-off point of 250 cells/μL and/or IgE ≥ 100 kU/L, both suggested by EPOS 2020 [1], are indicative of a type 2 endotype | 36/37 (97.3) | 61.1 | 2.78% | 8.33% | 27.78% | 44.44% | 16.67% |
| 9 | IgE levels are one of the main drivers of type 2 inflammation in asthma and in CRSwNP | 36/37 (97.3) | 80.6 | 0.00% | 2.78% | 16.67% | 52.78% | 27.78% |
| 10 | IgE antibodies play a pathogenic role in CRSwNP, regardless of the patient’s atopic status | 36/37 (97.3) | 72.2 | 0.00% | 0.00% | 27.78% | 58.33% | 13.89% |
| 11 | Targeting IgE is a strategy that contributes to reducing type 2 inflammation in CRSwNP | 35/37 (94.6) | 71.4 | 0.00% | 0.00% | 28.57% | 54.29% | 17.14% |
| No. | Statements by Topic | Response Rate, n/N (%) | % of Replies ≥ 4 a,b | Strongly Disagree | Disagree | Partially Agree | Agree | Strongly Agree |
|---|---|---|---|---|---|---|---|---|
| 12 | In CRSwNP the Clinical-Cytological Grading (CCG) is a useful method for classifying the pathology’s degree of severity | 36/37 (97.3) | 50.0 | 5.56% | 13.89% | 30.56% | 36.11% | 13.89% |
| 13 | Total nasal polyp score ≥ 5 can be considered as one of the parameters for CRSwNP severity | 36/37 (97.3) | 94.4 | 2.78% | 0.00% | 2.78% | 55.56% | 38.89% |
| 14 | SNOT-22 ≥ 40 (confirmed by EPOS 2020 [1]) is related to CRSwNP severity | 36/37 (97.3) | 88.9 | 2.78% | 2.78% | 5.56% | 58.33% | 30.56% |
| 15 | OCS dosage of more than 1 g/year is a sign of CRSwNP severity | 36/37 (97.3) | 72.2 | 2.78% | 5.56% | 19.44% | 58.33% | 13.89% |
| 16 | SNOT-22 is the only validated available tool for the assessment of health-related quality of life in CRSwNP patients, and can be considered as a reliable outcome in response to treatment | 36/37 (97.3) | 77.8 | 0.00% | 0.00% | 22.22% | 55.56% | 22.22% |
| 17 | Total nasal polyp score reduction can be considered as a reliable outcome in response to treatment | 36/37 (97.3) | 88.9 | 2.78% | 0.00% | 8.33% | 61.11% | 27.78% |
| 18 | SNOT-22 and total nasal polyp score are more useful when used together in order to have a deeper insight into the patient’s burden caused by the pathology | 36/37 (97.3) | 88.9 | 5.56% | 0.00% | 5.56% | 44.44% | 44.44% |
| 19 | Reduction in systemic prednisone dosage of ≥50% is an indirect outcome in response to biologic treatment | 36/37 (97.3) | 80.6 | 2.78% | 0.00% | 16.67% | 61.11% | 19.44% |
| 20 | N-ERD patients are difficult to treat and frequently relapse, and should therefore be considered a candidate to treatment with biologics | 36/37 (97.3) | 91.7 | 2.78% | 0.00% | 5.56% | 61.11% | 30.56% |
| 21 | A total nasal polyp score ≥ 4/8, which is one of the criteria for severity suggested by the update of EUFOREA published January 2021 [10], might also be a criterion for eligibility for biologic treatment | 35/37 (94.6) | 71.4 | 2.86% | 5.71% | 20.00% | 57.14% | 14.29% |
| No. | Statements by Topic | Response Rate, n/N (%) | % of Replies ≥ 4 a,b | Strongly Disagree | Disagree | Partially Agree | Agree | Strongly Agree |
|---|---|---|---|---|---|---|---|---|
| 23 | Patients with severe CRSwNP not eligible for surgery should be treated with available biologics first line | 36/37 (97.3) | 69.4 | 0.00% | 11.11% | 19.44% | 27.78% | 41.67% |
| 24 | Patients with severe CRSwNP may be firstly treated by biologics first-line in the presence of predictors of poor surgical outcome (asthma, allergy, N-ERD, high type 2 biomarkers) | 36/37 (97.3) | 72.2 | 0.00% | 13.89% | 13.89% | 30.56% | 41.67% |
| 34 | In patients with high nasal endoscopic polyp scores, treating with biologics before surgery is a driver to reduce the load of inflammation | 36/37 (97.3) | 72.2 | 2.78% | 11.11% | 13.89% | 50.00% | 22.22% |
| No. | Statements by Topic | Response Rate, n/N (%) | % of Replies ≥ 4 a,b | Strongly Disagree | Disagree | Partially Agree | Agree | Strongly Agree |
|---|---|---|---|---|---|---|---|---|
| 33 | Functional endoscopic sinus surgery simultaneous to biologic treatment in CRSwNP patients with very high nasal polyps endoscopic scores may offer a better starting point compared with exclusive treatment with biologics | 36/37 (97.3) | 72.2 | 2.78% | 8.33% | 16.67% | 41.67% | 30.56% |
| 35 | Functional endoscopic sinus surgery could be a coadjuvant treatment in patients with a moderate response to biologics | 36/37 (97.3) | 77.8 | 0.00% | 5.56% | 16.67% | 61.11% | 16.67% |
| No. | Statements by Topic | Response Rate, n/N (%) | % of Replies ≥ 4 a,b | Strongly Disagree | Disagree | Partially Agree | Agree | Strongly Agree |
|---|---|---|---|---|---|---|---|---|
| 25 | Treatment with biologics is highly recommended in difficult-to-treat CRSwNP patients who have undergone multiple endoscopic sinus surgeries | 36/37 (97.3) | 86.1 | 2.78% | 0.00% | 11.11% | 22.22% | 63.89% |
| 26 | Patients with CRSwNP with a significantly impaired QoL who have undergone multiple appropriate surgery should be eligible for treatment with biologics whatever the nasal polyp score | 36/37 (97.3) | 72.2 | 2.78% | 8.33% | 16.67% | 47.22% | 25.00% |
| No. | Statements by Topic | Response Rate, n/N (%) | % of Replies ≥ 4 a,b | Strongly Disagree | Disagree | Partially Agree | Agree | Strongly Agree |
|---|---|---|---|---|---|---|---|---|
| 22 | There should always be clear evidence of type 2 inflammation to consider CRSwNP patients eligible for treatment with available biologics | 36/37 (97.3) | 91.7 | 2.78% | 0.00% | 5.56% | 30.56% | 61.11% |
| 27 | Biologics should be discontinued at 6 months of treatment in patients with poor or no response | 36/37 (97.3) | 86.1 | 0.00% | 0.00% | 13.89% | 63.89% | 22.22% |
| 28 | Biologics may offer more chance of olfaction recovery compared with revision surgery | 36/37 (97.3) | 83.3 | 0.00% | 2.78% | 13.89% | 50.00% | 33.33% |
| 29 | A reduction in polyp size, improvement in sense of smell, and improvement in QoL are criteria to define response to biologics, that should be based on specific cut-offs set by EUFOREA | 36/37 (97.3) | 97.2 | 2.78% | 0.00% | 0.00% | 61.11% | 36.11% |
| 30 | In case of discontinuation of a specific biologic, a washout time is not mandatory before starting with another one | 36/37 (97.3) | 66.7 | 0.00% | 8.33% | 25.00% | 44.44% | 22.22% |
| 31 | The lowest effective dose of systemic corticosteroids should be used in the short-term management of CRSwNP | 36/37 (97.3) | 86.1 | 2.78% | 2.78% | 8.33% | 58.33% | 27.78% |
| 32 | Biologics should be offered for the management of comorbid CRSwNP and asthma in order to reduce exposure to systemic corticosteroids | 36/37 (97.3) | 88.9 | 2.78% | 0.00% | 8.33% | 30.56% | 58.33% |
| No. | Statements by Topic | Response Rate, n/N (%) | % of Replies ≥ 4 a,b | Strongly Disagree | Disagree | Partially Agree | Agree | Strongly Agree |
|---|---|---|---|---|---|---|---|---|
| 36 c | Clinical predictors of poor disease control with standard of care (surgery plus local corticosteroids/OCS), to support the decision of whether or not to perform surgery | 36/37 (97.3) | 83.3 | 2.78% | 2.78% | 11.11% | 44.44% | 38.89% |
| 37 c | Accuracy of biomarkers (including nasal cytology) as markers of response to biologics | 36/37 (97.3) | 91.7 | 2.78% | 0.00% | 5.56% | 36.11% | 55.56% |
| 38 c | Clinical usefulness of the detection of Staphylococcus endotoxin-specific IgE at nasal level | 36/37 (97.3) | 58.3 | 0.00% | 8.33% | 33.33% | 38.89% | 19.44% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Corso, E.; Bilò, M.B.; Matucci, A.; Seccia, V.; Braido, F.; Gelardi, M.; Heffler, E.; Latorre, M.; Malvezzi, L.; Pelaia, G.; et al. Personalized Management of Patients with Chronic Rhinosinusitis with Nasal Polyps in Clinical Practice: A Multidisciplinary Consensus Statement. J. Pers. Med. 2022, 12, 846. https://doi.org/10.3390/jpm12050846
De Corso E, Bilò MB, Matucci A, Seccia V, Braido F, Gelardi M, Heffler E, Latorre M, Malvezzi L, Pelaia G, et al. Personalized Management of Patients with Chronic Rhinosinusitis with Nasal Polyps in Clinical Practice: A Multidisciplinary Consensus Statement. Journal of Personalized Medicine. 2022; 12(5):846. https://doi.org/10.3390/jpm12050846
Chicago/Turabian StyleDe Corso, Eugenio, Maria Beatrice Bilò, Andrea Matucci, Veronica Seccia, Fulvio Braido, Matteo Gelardi, Enrico Heffler, Manuela Latorre, Luca Malvezzi, Girolamo Pelaia, and et al. 2022. "Personalized Management of Patients with Chronic Rhinosinusitis with Nasal Polyps in Clinical Practice: A Multidisciplinary Consensus Statement" Journal of Personalized Medicine 12, no. 5: 846. https://doi.org/10.3390/jpm12050846
APA StyleDe Corso, E., Bilò, M. B., Matucci, A., Seccia, V., Braido, F., Gelardi, M., Heffler, E., Latorre, M., Malvezzi, L., Pelaia, G., Senna, G., Castelnuovo, P., & Canonica, G. W. (2022). Personalized Management of Patients with Chronic Rhinosinusitis with Nasal Polyps in Clinical Practice: A Multidisciplinary Consensus Statement. Journal of Personalized Medicine, 12(5), 846. https://doi.org/10.3390/jpm12050846












