High SUVmax Is an Independent Predictor of Higher Diagnostic Accuracy of ROSE in EBUS-TBNA for Patients with NSCLC
Abstract
:1. Introduction
2. Methods
2.1. Patient Selection and Study Design
2.2. Mediastinal Lymph Node Sampling
2.3. Statistical Analyses
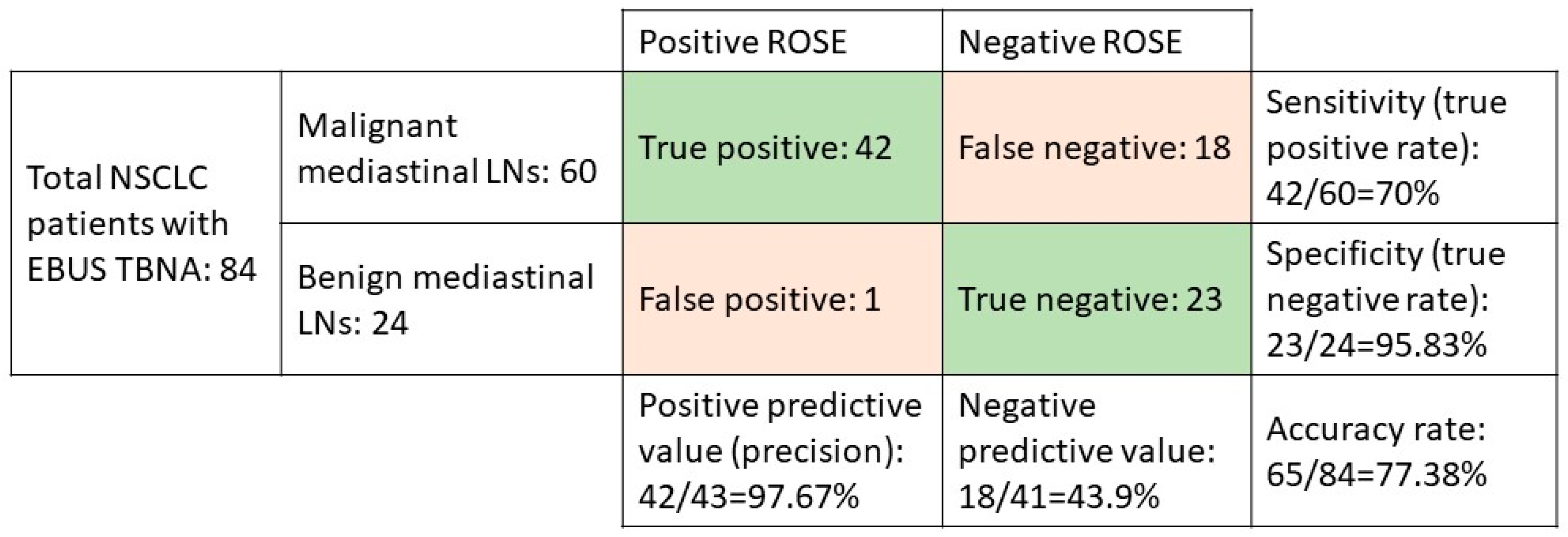
3. Results
3.1. Demographic Characteristics of the Enrolled Patients
3.2. Univariate and Multivariate Analysis of Predictive Factors of the Diagnostic Accuracy of ROSE in EBUS-TBNA in Non-Small-Cell Lung Cancer Patients with Malignant Mediastinal LNs
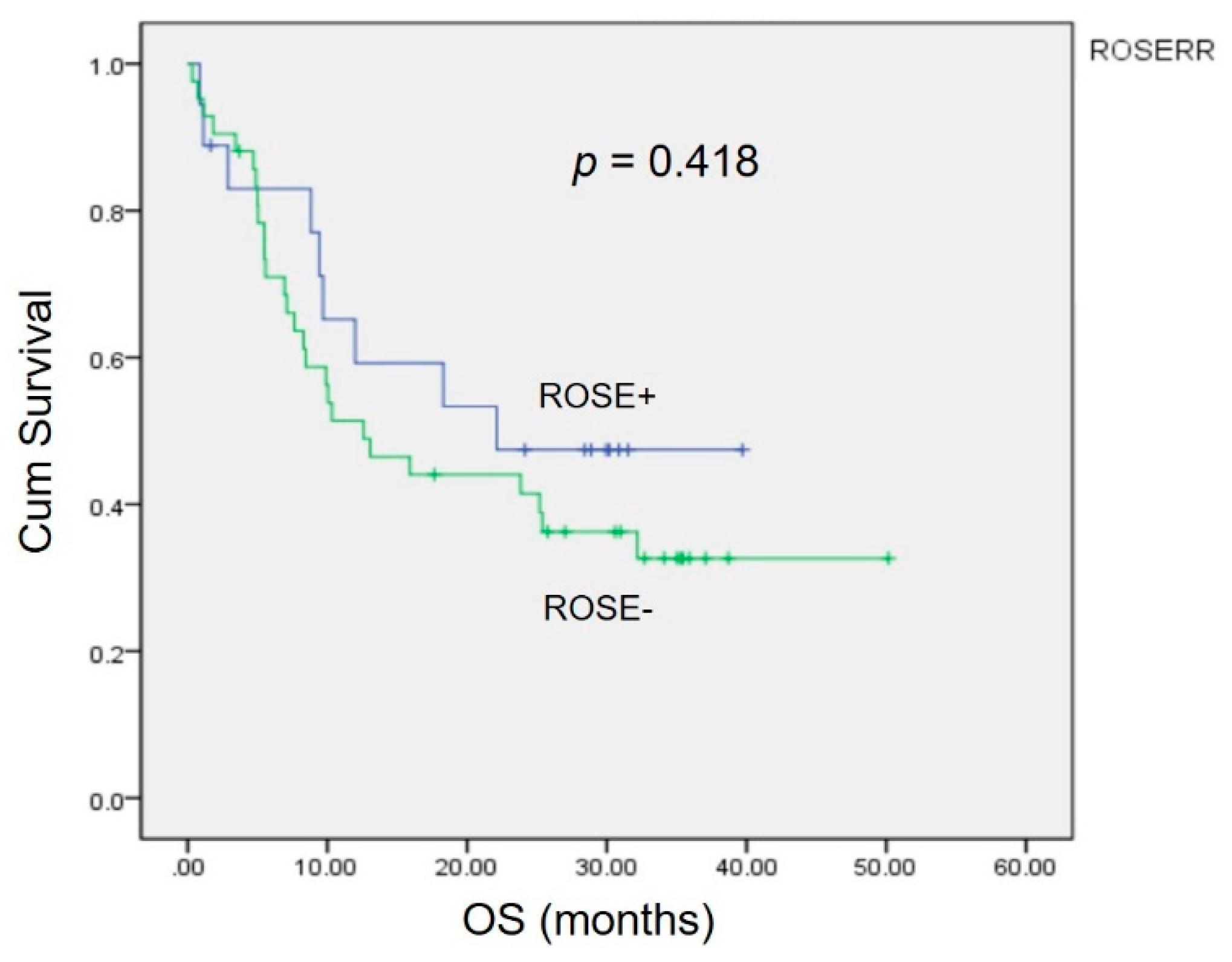
3.3. Survival Analysis
4. Discussion
4.1. The Role of ROSE in Clinical Practice
4.2. Predictive Factors of the Diagnostic Accuracy of ROSE in EBUS-TBNA
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhi, X.; Chen, J.; Xie, F.; Sun, J.; Herth, F.J.F. Diagnostic value of endobronchial ultrasound image features: A specialized review. Endosc. Ultrasound 2021, 10, 3–18. [Google Scholar] [PubMed]
- Kinsey, C.M.; Arenberg, D.A. Endobronchial ultrasound-guided transbronchial needle aspiration for non-small cell lung cancer staging. Am. J. Respir. Crit. Care Med. 2014, 189, 640–649. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Xie, F.; Mao, X.; Zheng, X.; Li, Y.; Zhu, L.; Sun, J. Determining factors of endobronchial ultrasound-guided transbronchial needle aspiration specimens for lung cancer subtyping and molecular testing. Endosc. Ultrasound 2019, 8, 404–411. [Google Scholar] [PubMed]
- Wahidi, M.M.; Herth, F.; Yasufuku, K.; Shepherd, R.W.; Yarmus, L.; Chawla, M.; Lamb, C.; Casey, K.R.; Patel, S.; Silvestri, G.A.; et al. Technical Aspects of Endobronchial Ultrasound-Guided Transbronchial Needle Aspiration: CHEST Guideline and Expert Panel Report. Chest 2016, 149, 816–835. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baram, D.; Garcia, R.B.; Richman, P.S. Impact of rapid on-site cytologic evaluation during transbronchial needle aspiration. Chest 2005, 128, 869–875. [Google Scholar] [CrossRef]
- Jain, D.; Allen, T.C.; Aisner, D.L.; Beasley, M.B.; Cagle, P.T.; Capelozzi, V.L.; Hariri, L.P.; Lantuejoul, S.; Miller, R.; Mino-Kenudson, M.; et al. Rapid On-Site Evaluation of Endobronchial Ultrasound-Guided Transbronchial Needle Aspirations for the Diagnosis of Lung Cancer: A Perspective From Members of the Pulmonary Pathology Society. Arch. Pathol. Lab. Med. 2018, 142, 253–262. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nakajima, T.; Yasufuku, K.; Saegusa, F.; Fujiwara, T.; Sakairi, Y.; Hiroshima, K.; Nakatani, Y.; Yoshino, I. Rapid on-site cytologic evaluation during endobronchial ultrasound-guided transbronchial needle aspiration for nodal staging in patients with lung cancer. Ann. Thorac. Surg. 2013, 95, 1695–1699. [Google Scholar] [CrossRef] [PubMed]
- Yarmus, L.; Akulian, J.; Gilbert, C.; Feller-Kopman, D.; Lee, H.J.; Zarogoulidis, P.; Lechtzin, N.; Ali, S.Z.; Sathiyamoorthy, V. Optimizing endobronchial ultrasound for molecular analysis. How many passes are needed? Ann. Am. Thorac. Soc. 2013, 10, 636–643. [Google Scholar] [CrossRef] [PubMed]
- Dyhdalo, K.S.; Booth, C.N.; Shorie, J.; Underwood, D.L.; Mazzone, P.; Brainard, J.A. Rapid on-site evaluation of endobronchial ultrasound-guided fine-needle aspirates: Correlation of adequacy assessment and final diagnosis in patients with bronchogenic carcinoma. J. Am. Soc. Cytopathol. 2014, 3, 199–205. [Google Scholar] [CrossRef]
- Shim, S.S.; Lee, K.S.; Kim, B.T.; Chung, M.J.; Lee, E.J.; Han, J.; Choi, J.Y.; Kwon, O.J.; Shim, Y.M.; Kim, S. Non-small cell lung cancer: Prospective comparison of integrated FDG PET/CT and CT alone for preoperative staging. Radiology 2005, 236, 1011–1019. [Google Scholar] [CrossRef]
- Kim, B.T.; Lee, K.S.; Shim, S.S.; Choi, J.Y.; Kwon, O.J.; Kim, H.; Shim, Y.M.; Kim, J.; Kim, S. Stage T1 non-small cell lung cancer: Preoperative mediastinal nodal staging with integrated FDG PET/CT--a prospective study. Radiology 2006, 241, 501–509. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.K.; Lee, K.S.; Kim, B.T.; Choi, J.Y.; Kim, H.; Kwon, O.J.; Shim, Y.M.; Yi, C.A.; Kim, H.Y.; Chung, M.J. Mediastinal nodal staging of nonsmall cell lung cancer using integrated 18F-FDG PET/CT in a tuberculosis-endemic country: Diagnostic efficacy in 674 patients. Cancer 2007, 109, 1068–1077. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.Y.; Zhao, H.; Zhang, J.; Wang, X.D.; Han, B.H. First 30 endobronchial ultrasound-guided transbronchial needle aspirations: A single institution’s early experience. Chin. Med. J. 2011, 124, 1818–1823. [Google Scholar] [PubMed]
- Casal, R.F.; Staerkel, G.A.; Ost, D.; Almeida, F.A.; Uzbeck, M.H.; Eapen, G.A.; Jimenez, C.A.; Nogueras-Gonzalez, G.M.; Sarkiss, M.; Morice, R.C. Randomized clinical trial of endobronchial ultrasound needle biopsy with and without aspiration. Chest 2012, 142, 568–573. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guo, H.; Liu, S.; Guo, J.; Li, B.; Li, W.; Lu, Z.; Sun, J.; Zhang, B.; Yu, J. Rapid on-site evaluation during endobronchial ultrasound-guided transbronchial needle aspiration for the diagnosis of hilar and mediastinal lymphadenopathy in patients with lung cancer. Cancer Lett. 2016, 371, 182–186. [Google Scholar] [CrossRef] [PubMed]
- van der Heijden, E.H.; Casal, R.F.; Trisolini, R.; Steinfort, D.P.; Hwangbo, B.; Nakajima, T.; Guldhammer-Skov, B.; Rossi, G.; Ferretti, M.; Herth, F.F.; et al. Guideline for the acquisition and preparation of conventional and endobronchial ultrasound-guided transbronchial needle aspiration specimens for the diagnosis and molecular testing of patients with known or suspected lung cancer. Respiration 2014, 88, 500–517. [Google Scholar] [CrossRef] [PubMed]
- Layfield, L.J.; Bentz, J.S.; Gopez, E.V. Immediate on-site interpretation of fine-needle aspiration smears: A cost and compensation analysis. Cancer 2001, 93, 319–322. [Google Scholar] [CrossRef]
- Louw, M.; Brundyn, K.; Schubert, P.T.; Wright, C.A.; Bolliger, C.T.; Diacon, A.H. Comparison of the quality of smears in transbronchial fine-needle aspirates using two staining methods for rapid on-site evaluation. Diagn. Cytopathol. 2012, 40, 777–781. [Google Scholar] [CrossRef] [PubMed]
- Moulla, Y.; Gradistanac, T.; Wittekind, C.; Eichfeld, U.; Gockel, I.; Dietrich, A. Predictive risk factors for lymph node metastasis in patients with resected non-small cell lung cancer: A case control study. J. Cardiothorac. Surg. 2019, 14, 11. [Google Scholar] [CrossRef]
- Koike, T.; Koike, T.; Yamato, Y.; Yoshiya, K.; Toyabe, S. Predictive risk factors for mediastinal lymph node metastasis in clinical stage IA non-small-cell lung cancer patients. J. Thorac. Oncol. 2012, 7, 1246–1251. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bao, F.; Yuan, P.; Yuan, X.; Lv, X.; Wang, Z.; Hu, J. Predictive risk factors for lymph node metastasis in patients with small size non-small cell lung cancer. J. Thorac. Dis. 2014, 6, 1697–1703. [Google Scholar]
- Roh, M.S.; Lee, J.I.; Choi, P.J.; Hong, Y.S. Relationship between micropapillary component and micrometastasis in the regional lymph nodes of patients with stage I lung adenocarcinoma. Histopathology 2004, 45, 580–586. [Google Scholar] [CrossRef] [PubMed]
- Russell, P.A.; Wainer, Z.; Wright, G.M.; Daniels, M.; Conron, M.; Williams, R.A. Does lung adenocarcinoma subtype predict patient survival?: A clinicopathologic study based on the new International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society international multidisciplinary lung adenocarcinoma classification. J. Thorac. Oncol. 2011, 6, 1496–1504. [Google Scholar]
- Liu, Y.; Xu, M.L.; Zhong, H.H.; Heng, W.J.; Wu, B.Q. EGFR mutations are more frequent in well-differentiated than in poor-differentiated lung adenocarcinomas. Pathol. Oncol. Res. 2008, 14, 373–379. [Google Scholar] [CrossRef] [PubMed]
- Yoon, H.Y.; Ryu, J.S.; Sim, Y.S.; Kim, D.; Lee, S.Y.; Choi, J.; Park, S.; Ryu, Y.J.; Lee, J.H.; Chang, J.H. Clinical significance of EGFR mutation types in lung adenocarcinoma: A multi-centre Korean study. PLoS ONE 2020, 15, e0228925. [Google Scholar] [CrossRef] [PubMed]
- Han, H.S.; Eom, D.W.; Kim, J.H.; Kim, K.H.; Shin, H.M.; An, J.Y.; Lee, K.M.; Choe, K.H.; Lee, K.H.; Kim, S.T.; et al. EGFR mutation status in primary lung adenocarcinomas and corresponding metastatic lesions: Discordance in pleural metastases. Clin. Lung Cancer 2011, 12, 380–386. [Google Scholar] [CrossRef] [PubMed]
- Tsao, M.S.; Sakurada, A.; Ding, K.; Aviel-Ronen, S.; Ludkovski, O.; Liu, N.; Le Maitre, A.; Gandara, D.; Johnson, D.H.; Rigas, J.R.; et al. Prognostic and predictive value of epidermal growth factor receptor tyrosine kinase domain mutation status and gene copy number for adjuvant chemotherapy in non-small cell lung cancer. J. Thorac. Oncol. 2011, 6, 139–147. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, M.W.; Wu, C.T.; Shih, J.Y.; Chang, Y.L.; Yang, P.C. Clinicopathologic characteristics and prognostic significance of EGFR and p53 mutations in surgically resected lung adenocarcinomas ≤ 2 cm in maximal dimension. J. Surg. Oncol. 2014, 110, 99–106. [Google Scholar] [CrossRef]
- Gundogdu, A.G.; Onder, S.; Firat, P.; Dogan, R. EGFR immunoexpression, RAS immunoexpression and their effects on survival in lung adenocarcinoma cases. J. Thorac. Dis. 2014, 6, 778–784. [Google Scholar] [PubMed]
- Kandathil, A.; Kay, F.U.; Butt, Y.M.; Wachsmann, J.W.; Subramaniam, R.M. Role of FDG PET/CT in the Eighth Edition of TNM Staging of Non-Small Cell Lung Cancer. Radiographics 2018, 38, 2134–2149. [Google Scholar] [CrossRef]
- Lee, S.M.; Park, C.M.; Paeng, J.C.; Im, H.J.; Goo, J.M.; Lee, H.J.; Kang, C.H.; Kim, Y.W.; Kim, J.I. Accuracy and predictive features of FDG-PET/CT and CT for diagnosis of lymph node metastasis of T1 non-small-cell lung cancer manifesting as a subsolid nodule. Eur. Radiol. 2012, 22, 1556–1563. [Google Scholar] [CrossRef] [PubMed]
| Correct Diagnosis of ROSE n = 42 (%) | Incorrect Diagnosis of ROSE n = 18 (%) | p-Value a | |
|---|---|---|---|
| Age | 65.5 ± 1.69 | 65.5 ± 2.38 | 1 |
| Gender | 0.678 | ||
| Male | 28 (66.67) | 13 (72.22) | |
| Female | 14 (33.33) | 5 (27.78) | |
| Smoking | 0.78 | ||
| Yes | 24 (57.14) | 11 (61.11) | |
| No | 18 (42.86) | 7 (38.89) | |
| Histology | 0.335 | ||
| Adenocarcinoma | 28 (66.67) | 5 (27.78) | |
| SCC | 7 (16.67) | 3 (16.67) | |
| PDA | 5 (11.9) | 4 (22.22) | |
| Clinical stage | 0.875 | ||
| IA | 1 (2.38) | 0 | |
| IB | 0 | 1 (5.56) | |
| IIB | 3 (7.14) | 0 | |
| IIIA | 9 (21.43) | 5 (27.78) | |
| IIIB | 8 (19.05) | 4 (22.22) | |
| IVA | 6 (14.29) | 5 (27.78) | |
| IVB | 15 (35.71) | 3 (16.67) | |
| Differentiation | 0.145 | ||
| Moderate | 15 (35.71) | 3 (16.67) | |
| Poor | 27 (64.29) | 15 (83.33) | |
| EGFR | 0.321 | ||
| Mutation | 11 (39.29) | 3 (23.08) | |
| Wild-type | 17 (60.71) | 10 (76.92) | |
| SUVmax of mediastinal LNs | 10.77 ± 0.75 | 6.45 ± 0.78 | 0.001 a |
| SUVmax of mediastinal LNs > 5 | <0.001 a | ||
| Yes | 37 (88.10) | 12 (66.67) | |
| No | 2 (4.76) | 4 (22.22) | |
| Mediastinal LN size (cm) | 24.55 ± 2.23 | 22.86 ± 4.13 | 0.698 |
| Mediastinal LN size > 1.5 cm | 0.027 a | ||
| Yes | 33 (78.57) | 9 (50) | |
| No | 9 (21.43) | 9 (50) | |
| Hounsfield units (HU) | 54.14 ± 2.81 | 53.18 ± 4.18 | 0.852 |
| ROSE slides | 6.62 ± 0.357 | 6.28 ± 0.497 | 0.594 |
| CEA (ng/mL) | 47.4 ± 26.39 | 29.46 ± 12.17 | 0.695 |
| Anti-SCC (ng/mL) | 2.94 ± 1.43 | 1.3 ± 0.37 | 0.515 |
| Final pathology of EBUS | 0.003 a | ||
| Correct | 30 (71.43) | 8 (50) | |
| Incorrect | 4 (9.52) | 8 (50) | |
| Operation time (min) | 50.4 ± 3.23 | 64 ± 6.42 | 0.04 a |
| Survival | 0.309 | ||
| Yes | 15 (35.71) | 9 (50) | |
| No | 27 (64.29) | 9 (50) |
| Univariant | p-Value a | Multi-Variant | p-Value | |||
|---|---|---|---|---|---|---|
| HR | CI (95%) | HR | CI (95%) | |||
| N2 LN size > 1.5 cm | 3.667 | 1.125–11.955 | 0.031 a | 1.867 | 0.278–12.537 | 0.521 |
| Pathology accuracy | 7.5 | 1.792–31.383 | 0.006 a | 1.548 | 0.171–13.986 | 0.697 |
| SUVmax > 5 | 41 | 4.596–365.734 | 0.001 a | 20.258 | 1.761–233.057 | 0.016 a |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, Y.-Y.; Huang, H.-Y.; Lin, C.-Y.; Chen, K.-L.; Huang, T.-W. High SUVmax Is an Independent Predictor of Higher Diagnostic Accuracy of ROSE in EBUS-TBNA for Patients with NSCLC. J. Pers. Med. 2022, 12, 451. https://doi.org/10.3390/jpm12030451
Chen Y-Y, Huang H-Y, Lin C-Y, Chen K-L, Huang T-W. High SUVmax Is an Independent Predictor of Higher Diagnostic Accuracy of ROSE in EBUS-TBNA for Patients with NSCLC. Journal of Personalized Medicine. 2022; 12(3):451. https://doi.org/10.3390/jpm12030451
Chicago/Turabian StyleChen, Ying-Yi, Hsin-Ya Huang, Chi-Yi Lin, Kuan-Liang Chen, and Tsai-Wang Huang. 2022. "High SUVmax Is an Independent Predictor of Higher Diagnostic Accuracy of ROSE in EBUS-TBNA for Patients with NSCLC" Journal of Personalized Medicine 12, no. 3: 451. https://doi.org/10.3390/jpm12030451
APA StyleChen, Y.-Y., Huang, H.-Y., Lin, C.-Y., Chen, K.-L., & Huang, T.-W. (2022). High SUVmax Is an Independent Predictor of Higher Diagnostic Accuracy of ROSE in EBUS-TBNA for Patients with NSCLC. Journal of Personalized Medicine, 12(3), 451. https://doi.org/10.3390/jpm12030451






